Abstract
Steroid-resistant nephrotic syndrome (SRNS) is one of the major causes of end-stage renal disease (ESRD) in childhood and is mostly associated with focal segmental glomerulosclerosis (FSGS). More than 50 monogenic causes of SRNS or FSGS have been identified. Recently, the mutation detection rate in pediatric patients with SRNS has been reported to be approximately 30%. In this study, genotype-phenotype correlations in a cohort of 291 Korean pediatric patients with SRNS/FSGS were analyzed. The overall mutation detection rate was 43.6% (127 of 291 patients). WT1 was the most common causative gene (23.6%), followed by COQ6 (8.7%), NPHS1 (8.7%), NUP107 (7.1%), and COQ8B (6.3%). Mutations in COQ6, NUP107, and COQ8B were more frequently detected, and mutations in NPHS2 were less commonly detected in this cohort than in study cohorts from Western countries. The mutation detection rate was higher in patients with congenital onset, those who presented with proteinuria or chronic kidney disease/ESRD, and those who did not receive steroid treatment. Genetic diagnosis in patients with SRNS provides not only definitive diagnosis but also valuable information for decisions on treatment policy and prediction of prognosis. Therefore, further genotype-phenotype correlation studies are required.
1. Introduction
Childhood onset nephrotic syndrome (NS) generally responds well to conventional oral corticosteroid therapy, and steroid-sensitive NS has a benign long-term renal prognosis even though it shows frequent relapses. However, 10–20% of pediatric NS cases are steroid-resistant nephrotic syndrome (SRNS), which does not achieve remission by oral corticosteroid therapy. SRNS is one of the most common causes of end-stage renal disease (ESRD) in childhood, and the common pathological finding in SRNS is focal segmental glomerulosclerosis (FSGS) [1].
Furthermore, SRNS is highly heterogeneous both phenotypically and genetically and can occur at any age, manifesting as isolated proteinuria or fully developed NS. In addition, various kinds of syndromic diseases may manifest SRNS as a renal phenotype along with characteristic extrarenal phenotypes. To date, at least 50 monogenic causes of SRNS or FSGS have been identified, and novel causative genes are constantly being discovered [2].
Recent advances in next-generation sequencing (NGS) techniques make genetic diagnosis more feasible in SRNS patients. Recent large cohort studies [3,4,5,6] revealed genetic mutations in approximately 30% of pediatric patients with SRNS/FSGS. Benefits of genetic diagnosis in patients with SRNS include providing definitive diagnosis and valuable information for decisions on treatment policy and prediction of prognosis.
Genetic testing modalities currently used for SRNS include Sanger sequencing, targeted exome sequencing (TES) with gene panels, whole exome sequencing (WES) and whole-genome sequencing (WGS) [7,8,9,10,11]. Sanger sequencing can be effectively applied to test a single or few candidate genes using a gene-by-gene approach. Candidate genes can be easily identified clinically in patients with typical extrarenal phenotypes of syndromic diseases. In addition, one of the four candidate genes (NPHS1, NPHS2, WT1, and LAMB2) can be identified in more than 85% of patients with congenital onset [12,13]. Sanger sequencing is still regarded as the gold standard, and variants detected by NGS should be confirmed by Sanger sequencing [14]. In patients whose candidate genes are not identified clinically, gene-by-gene Sanger sequencing of more than 50 known candidate genes for SRNS is a time-consuming and costly test. Instead, TES with gene panels can provide a rapid and cost-effective test by sequencing a set of all known genes relevant to SRNS simultaneously. Notably, some patients with syndromic disorders manifest no or mild/atypical extrarenal phenotypes. In these cases, the suspected underlying genetic syndrome cannot be identified clinically, but TES is able to detect the disease-causing mutations [14]. However, TES cannot detect mutations in novel or phenocopying genes unless these genes are included in the panels. Another disadvantage of TES is rapidly outdated gene panels due to the continuous discovery of novel disease-causing genes. Despite these drawbacks, TES with gene panels is currently considered the most cost-effective approach for indication-driven mutation analysis [10,14].
Compared with TES gene panels, WES is an unbiased approach to genetic diagnosis by sequencing entire exons, i.e., all protein-coding regions of the genome. Therefore, WES can identify not only known gene mutations but also novel disease-causing genes. Current limitations of WES include issues with lower coverage of some exons, high costs and difficulty in handling enormous amounts of data [8,9,10,11,14]. A more complete per-base coverage can be provided by WGS, but the cost and interpretation issues are larger than in WES [8,9,14]. Currently, Sanger sequencing or TES is used as the first-line test for the genetic diagnosis of SRNS, and WES or WGS can be used when the first-line test shows negative results [8,9,10,11,14]. In this study, 127 patients had disease-causing mutations, including 80 (63.0%) patients diagnosed by Sanger sequencing, 40 (31.5%) by TES, and 4 (3.1%) by WES.
Like most genetic disorders, hereditary SRNS shows ethnic and geographic differences. However, there have been no large-scale genetic studies for pediatric patients with SRNS/FSGS in Korea. In this study, phenotype-genotype correlations were studied in a cohort of Korean pediatric patients with SRNS/FSGS.
2. Materials and Methods
2.1. Study Participants
This study was approved by the Institutional Review Board of Seoul National University Hospital (IRB No. 0812-002-264). Informed consent was obtained from all individual participants and/or their parents. All methods were carried out in accordance with the Declaration of Helsinki. Two hundred ninety-one pediatric patients with an onset age of renal symptoms ≤20 years were recruited from 20 major pediatric nephrology centers in Korea. All patients had persistent proteinuria (spot urine protein/creatinine ratio >0.2 mg/mg) or fully developed NS. Most patients showed resistance to conventional oral steroid therapy either at the initial presentation (initial steroid non-responders) or during follow-up (late steroid non-responders). Based on the KDIGO (Kidney Disease: Improving Global Outcomes) clinical practice guideline for management of glomerulonephritis [15], an initial non-responder is defined as “failure to achieve complete remission after 8 weeks of corticosteroid therapy”, and a late non-responder is defined as “persistent proteinuria during 4 or more weeks of corticosteroids following one or more remissions”. Some patients did not receive steroid treatment because they showed congenital onset, advanced stage of chronic kidney disease (CKD), or mild to moderate degree of proteinuria only at the initial presentation. Medical records of the patients were reviewed retrospectively.
2.2. Strategy of Mutational Studies
In most patients, screening of a single or few candidate genes using Sanger sequencing was performed first; (1) NPHS1, NPHS2, WT1, and LAMB2 for patients with congenital (disease onset within the first 3 months of life) or infantile (disease onset at age 4–12 months) NS [12,13]; (2) INF2, ACTN4, and TRPC6 for patients with a family history of autosomal dominant (AD) inheritance; (3) NPHS2 and NUP107 for patients with a family history of autosomal recessive (AR) inheritance; and (4) corresponding causative gene for patients with syndrome diseases. In patients suspected of mitochondrial cytopathy, especially MELAS (mitochondrial encephalopathy, lactic acidosis, and stroke-like episodes) syndrome, heteroplasmy of the 3243A > G variation in MT-TL1 was tested by polymerase chain reaction-restriction fragment length polymorphism (PCR-RFLP) using the ApaI restriction enzyme [16]. Then, TES or WES were performed for the remaining patients and those patients with negative results in the initial screening tests.
2.3. Targeted Exome Sequencing (TES) and Variant Calling
The gene panel for TES covered 57 genes known to be associated with SRNS or FSGS at that time (Supplementary Table S1). Genomic DNA was extracted from whole blood using QIAamp DNA mini kits (Qiagen, Valencia, CA, USA). The quality or quantity of DNA was checked using a Nanodrop 8000 ultraviolet–visible (UV–Vis) spectrometer (Thermo Scientific, Waltham, MA, USA) and Qubit 2.0 Fluorometer (Life Technologies, Grand Island, NY, USA). Genomic DNA was sheared by a Covaris S220 (Covaris, Woburn, MA, USA). Targeted exome capture was performed using a SureSelect XT customized kit (Agilent Technologies, Santa Clara, CA, USA). Sequencing was performed on the HiSeq 2500 platform with paired-end 100-bp reads (Illumina, San Diego, CA, USA).
Sequenced reads were aligned to the human reference genome (hg19) using the Burrows–Wheeler alignment (BWA) tool with the maximal exact match (MEM) algorithm (version 0.7.5) [17]. SAMtools (version 0.1.18) [18], Picard Tools (version 1.93, https://broadinstitute.github.io/picard/, accessed on 31 January 2020) and GATK (version 3.1-3) [19] were used for manipulating aligned sequenced data. Single nucleotide variants and InDels (insertions/deletions) were detected by UnifiedGenotyper in GATK. Various information, such as mutation nomenclature, dbSNP id, minor allele frequency of ExAC (the Exome Aggregation Consortium), and LJB23 databases, were annotated for each variant by ANNOVAR (Annotate Variation) [20]. Several filtering steps were applied to obtain candidates from germline variants; (1) variants with very low VAF (<5%), (2) variants with minor allele frequency (>1%) in the 1000GP3, and (3) variants in genes not related to the disease. Interpretation of variants followed the American College of Medical Genetics and Genomics (ACMG) guidelines, and variants classified as pathogenic or likely pathogenic were considered to be disease-causing mutations after confirmation by Sanger sequencing [21].
2.4. Whole-Exome Sequencing (WES) and Variant Calling
The procedures used for the preparation of genomic DNA, whole-exome capture using an Agilent V5 array, sequencing using the Illumina HiSeq 2500 platform (Illumina, San Diego, CA, USA), read alignment, variant calling, variant filtering and de novo variant calling have been described previously [22].
2.5. Statistical Analysis
To determine significant differences between groups with or without pathogenic variants, categorical variables were analyzed using the chi-square test or Fisher’s exact test, and continuous variables were compared using the t-test or Mann–Whitney U test. All values are reported as the median (interquartile range, IQR). The statistical analysis was performed using SPSS version 24.0 (SPSS, Armonk, NY, USA).
3. Results
3.1. Phenotypes
The clinical features of the patients are summarized in Table 1. A total of 291 unrelated pediatric patients (male:female = 162:129) with SRNS/FSGS were recruited for this study. The median onset age was 3.9 years (IQR 1.5–9.2 years), and the median duration of follow-up from the onset was 8.0 years (IQR 3.4–13.3 years). None of the patients were offspring of a consanguineous couple, and 48 (16.4%) patients had a family history of kidney disease.

Table 1.
Genotype-phenotype correlations in pediatric patients with steroid-resistant nephrotic syndrome or focal segmental glomerulosclerosis.
Regarding age of onset, 35 (12.2%) patients showed congenital onset, and 25 (8.6%) patients showed infantile onset. One hundred seventy-seven (60.8%) patients presented with NS, 93 (32.0%) patients with proteinuria, and 19 (6.5%) patients with CKD or ESRD. Conventional steroid therapy was administered to 206 patients, and 191 (92.7%) patients showed steroid resistance. In 83 patients, steroid therapy was not performed because they presented with congenital onset (n = 32), advanced stage of CKD (n = 29), or a mild to moderate degree of proteinuria only (n = 22). Kidney biopsy was performed in 236 patients and FSGS revealed in 165 (69.9%) patients, minimal change disease in 31 (13.1%) patients, and other lesions in 40 (16.9%) patients. During follow-up, 113 (38.8%) patients had maintained a normal estimated glomerular filtration rate (eGFR), 29 (10.0%) patients progressed to CKD stages 2–4, and 144 (49.5%) patients progressed to ESRD. Kidney transplantation was performed in 100 patients, including 71 patients with FSGS, nine of whom had recurrence of SRNS/FSGS in the graft kidney.
3.2. Genotypes
The overall detection rate of disease-causing mutations was 43.6% (127 of 291 patients): 80 (27.5%) patients by Sanger sequencing, three (1.0%) patients with MELAS syndrome by PCR-RFLP of the MT-TL1 gene, four (1.4%) patients by WES, and 40 (13.7%) patients by TES. Among 127 patients with disease-causing mutations, 59 (46.5%) patients had AD mutations, 58 (45.7%) patients had AR mutations, and 10 (7.9%) patients had X-linked or mitochondrial mutations.
WT1 was the most common causative gene (23.6%, 30 patients), followed by COQ6 (8.7%, 11 patients), NPHS1 (8.7%, 11 patients), NUP107 (7.1%, 9 patients), COQ8B (6.3%, 8 patients), MYH9 (4.7%, 6 patients), and INF2 (4.7%, 6 patients) (Table 2). There were 14 patients with mutations in phenocopy genes, including COL4A3–5 and WDR19 (Table 2). The genotypes and clinical features of patients with disease-causing mutations are summarized in Supplementary Table S2. In addition, variants of unknown significance (VUS) were detected by TES in 23 additional patients (Supplementary Table S3).

Table 2.
Mutation screening results.
3.3. Genotype-Phenotype Correlations
A comparison between patients with disease-causing mutations and patients without mutations is summarized in Table 1. The mutation detection rate was 77.1% in patients with congenital onset, which was significantly higher than that in patients with older disease onset (38.7%, p < 0.001). The rate was lower in patients presenting with NS than in patients presenting with proteinuria or CKD/ESRD (34.5% versus 57.1%, p < 0.001). Patients who did not receive steroid treatment showed a higher mutation detection rate than steroid non-responders (63.9% versus 37.7%, p < 0.001). None of the steroid responders and only one of 12 steroid late non-responders had mutations. Moreover, mutations were not detected in any of the patients with minimal change disease. Interestingly, the mutation detection rate showed a negative correlation with the current eGFR of the patients: 15.0% in patients with normal eGFR, 37.9% in patients with CKD stages 2–4, and 67.4% in patients with ESRD (Table 1 and Figure 1). The rate of progression to ESRD showed no significant difference between the mutation (+) and mutation (−) groups, and disease recurrence in the graft kidney was noted in the latter group only.
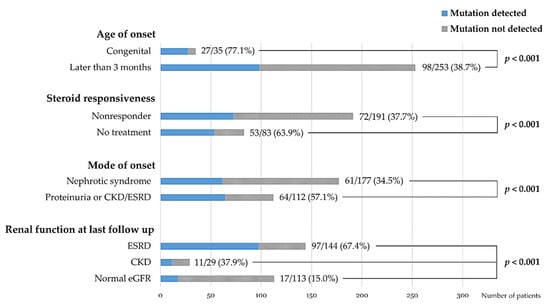
Figure 1.
Comparison of mutation detection rates among subgroups of patients according to onset age, steroid responsiveness, mode of onset, and renal functional outcome.
Comparison between patients with AD mutations and patients with AR mutations showed that most (11 of 12) patients with disease onset ≥13 years had AD mutations (Supplementary Table S4 and Figure 2). Other clinical parameters showed no significant difference between the two groups.
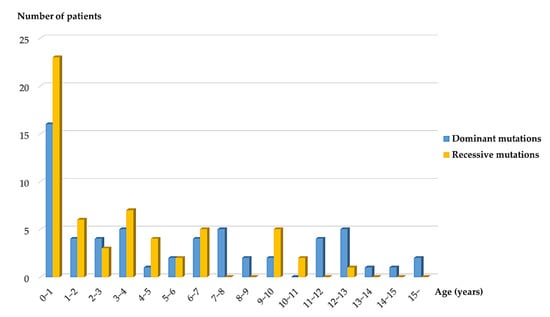
Figure 2.
Distribution of dominant and recessive mutations by onset age.
4. Discussion
In this work, of 291 Korean children with SRNS or FSGS, genetic mutations were identified in 127 patients (43.6%) in one of 26 causative genes. Thirty different novel mutations detected in 15 causative genes are described in Supplemental Table S2. The mutation detection rate was higher than the 23.6–30.3% reported by previous large cohort studies from Western and Asian countries (Table 3). Such differences cannot be explained clearly, but the size of the sample database, selection bias of the target patients, and differences in ethnicity may play some role.

Table 3.
Genetic studies in large cohorts of pediatric patients with steroid-resistant nephrotic syndrome.
One of the most striking differences in this study compared with studies from other countries was the low prevalence of NPHS2 mutations—1.4% of total patients and 3.1% of patients with mutations. In 2015, two large international cohort studies, the PodoNet Registry study [3] and the SRNS Study Group [4], using a panel of genes covering 31 and 27 candidate genes, respectively, were published. In these studies, NPHS2 was the most commonly mutated gene (49.8% and 33.7% of patients with mutations, respectively), and the sum of three major causative genes (NPHS2, NPHS1, and WT1) accounted for 81.9% and 74.8% of total mutations, respectively. In 2017, another study from the United Kingdom using WES with a focus on 53 genes was published [2]. In this study, the proportion of mutations in NPHS2 and the sum of three major causative genes (NPHS2, NPHS1, and WT1) were 24.5% and 61.3%, respectively. The difference between the studies published in 2015 and 2017 may be due, at least in part, to differences in the number of genes studied. An international study [23] using WES showed a low prevalence of NPHS2 and WT1 mutations because many enrolled individuals were screened for mutations in WT1 and NPHS2 before performing WES, and those who screened positive were excluded. Moreover, a Japanese study [6] showed that none of the 230 unrelated patients with proteinuria had NPHS2 mutations, and a Chinese study [5] showed that NPHS2 mutations were detected in 4 (3.3%) of 120 children with SRNS or isolated proteinuria, which accounted for 11.8% of 33 patients with disease-causing mutations. The lower prevalence of NPHS2 mutations in Asian countries, including Korea, may be due to the absence of common mutations, i.e., a founder effect [4,24,25]. Another interesting finding in this study is the higher prevalence of mutations in COQ6, COQ8B and NUP107, which was consistent with our previous studies [26,27,28]. An increased prevalence of COQ8B mutations was also found in a Chinese study [5], while an increased prevalence of NUP107 mutations was found in a Japanese study [6].
In this study, the mutation detection rate was higher in patients with congenital onset than in patients with other onset age groups (77.1% versus 38.7%, p < 0.001). Previous reports [4,12,13] have shown that the mutation detection rate is inversely related to age at disease onset in patients with SRNS. In a European study [12], the mutation detection rates of congenital and infantile NS were 84.8% and 44.1%, respectively (66.3% in the first year combined). Similarly, a previous study [13] from our group reported that the mutation detection rates of congenital and infantile NS were 93.9% and 20.2%, respectively (56.7% overall). In addition, a large international cohort study by the SRNS Study Group [4] reported the mutation detection rate by onset age as follows: onset in the first 3 months of life (69.4%), between 4 and 12 months old (49.7%), between 1 and 6 years old (25.3%), between 7 and 12 years old (17.8%), and between 13 and 18 years old (10.8%).
This study showed a higher mutation detection rate in patients who presented with proteinuria than in patients who presented with NS (57.0% versus 34.5%, p < 0.001). Similarly, in a Japanese study [6], the absence of edema was one of the risk factors for genetic mutations in pediatric patients with severe proteinuria. In this study, the mutation detection rate was higher in patients without steroid treatment than in patients with initial steroid non-responsiveness (63.9% versus 39.7%, p < 0.001). Most patients who did not receive steroid treatment in the present study presented with congenital onset, advanced stage CKD, or proteinuria, and these findings may contribute to the higher mutation detection rate. SRNS with AD mutations, except for WT1 mutations, typically presents later in life, in adolescence or adulthood [4,7]. This study also showed that 10 of 11 patients with disease onset over 13 years of age had AD mutations. Disease recurrence in the graft kidney was noted in the mutation (-) group only. The recurrence rate after transplantation in the mutation (−) group (25.8%, 8 of 31 patients) was lower than that in a previous report from a Korean tertiary center (50.0%, 18 of 36 idiopathic FSGS patients) [29].
Early genetic diagnosis can benefit patients with SRNS in many ways. First, patients do not have to waste their time and money on an accurate diagnosis, i.e., a ‘diagnostic odyssey’ [14,30]. Second, genetic diagnosis is essential for family counseling. Third, detection of certain mutations allows prediction and further screening of renal and extrarenal comorbidities and helps to avoid possible future complications, e.g., risk of Wilms’ tumor or gonadoblastoma in patients with WT1 mutations [31,32]. Fourth, patients can avoid invasive diagnostic procedures (e.g., a kidney biopsy) and ineffective, possibly harmful, drug therapy. Fifth, some rare mutations are potentially treatable with other therapeutic options, e.g., coenzyme Q10 supplementation for mutations involving the coenzyme Q10 biosynthesis pathway, such as COQ2, COQ6, COQ8B or PDSS2 mutations [33,34,35]. Finally, genetic diagnosis is important for preparing a kidney transplantation in terms of donor evaluation in family members with AD mutations as well as predicting the possibility of recurrence of FSGS in the graft kidney [3,36].
Ideally, genetic testing is recommended for all children with SRNS due to the relatively high overall mutation detection rate. If it is practically unfeasible, patients at high risk of genetic mutations should be selected. Commonly applied indications for genetic testing are as follows: (1) early age of onset (congenital or infantile); (2) a family history of SRNS or consanguinity; (3) presence of typical extrarenal manifestation of syndromic diseases; (4) progression to CKD or ESRD, and (5) preoperative evaluation for kidney transplantation [7,8,9,10,11].
Fourteen (11.0% of patients with disease-causing mutations) patients in this study had mutations in four phenocopying genes, including COL4A3–5 and WDR19. Because these cases manifested proteinuria or SRNS as the only evident clinical sign at disease onset or even later, they were clinically diagnosed with and treated for SRNS. A phenocopy is defined as “a phenotypic trait or disease that resembles the trait expressed by a particular genotype, but in an individual who is not a carrier of that genotype” [37]. In a recent study [23] in 300 families with SRNS using WES, 74 families (25%) had mutations in one of the known SRNS genes, and 11 families (3.7%) had mutations in genes that cause a phenocopy of SRNS. Landini et al. [38] studied 64 young patients diagnosed with SRNS, and the exome sequencing results were filtered in silico for 298 genes related to CKD, including but not limited to SRNS-related genes. They found disease-causing variants in podocytopathy genes typically associated with SRNS and FSGS in 19 patients (30%) as well as pathogenic mutations in phenocopy genes, including COL4A3–5 (Alport syndrome), CLCN5 (Dent disease), PAX2 (renal-coloboma syndrome), and GLA (Fabry disease), in 18 patients. In addition, they found distinct extrarenal phenotypes typical of the genetic diagnoses in all patients and/or first-degree relatives by post hoc thorough ‘reverse phenotyping’. These findings highlight that, even in the era of genomics, precise and thorough phenotyping by clinicians remains essential for an accurate genetic diagnosis, including selection of the appropriate genetic testing method and interpretation of results [14,39].
5. Conclusions
In conclusion, the overall mutation detection rate in this cohort of Korean pediatric patients with SRNS was 43.6%. Mutations in COQ6, NUP107, and COQ8B were more frequently detected, and mutations in NPHS2 were less commonly detected in this cohort compared to study cohorts from Western countries. The mutation detection rate was higher in patients with congenital onset, those who presented with proteinuria or CKD/ESRD, and those who did not receive steroid treatment. The worse the current renal function was, the higher the mutation detection rate. Genetic tests should be performed for pediatric patients with SRNS, especially for patients with younger onset age, presentation with proteinuria or progression to advanced CKD stages.
Supplementary Materials
The following are available online at https://www.mdpi.com/2077-0383/9/6/2013/s1: Table S1: Fifty-seven genes included in the targeted exome sequencing, Table S2: Genotypes and phenotypes of patients with disease-causing mutations, Table S3: Variants of unknown significance detected by targeted exome sequencing, Table S4: Comparison between patients with autosomal dominant (AD) mutations and patients with autosomal recessive (AR) mutations. References [22,24,33,34,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90] are cited in the Supplementary Materials.
Author Contributions
Conceptualization, E.P. and H.I.C.; Data curation, H.G.K.; Formal analysis, E.P.; Funding acquisition, H.G.K. and H.I.C.; Investigation, Y.H.A.; Methodology, W.-Y.P.; Resources, Y.S.P., J.H.L., S.H.K., M.H.C., H.C., K.H.Y., J.I.S. and I.-S.H.; Supervision, H.I.C.; Validation, C.L. and N.K.D.K.; Writing—original draft, E.P. and N.K.D.K.; Writing—review and editing, H.I.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by a grant from the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea, grant number HI18C0013 and was also supported by Research Resettlement Fund for the new faculty of Seoul National University.
Acknowledgments
The authors thank all the clinicians who referred their patients for genetic analysis: Kee Hyuk Kim, National Health Insurance System Ilsan Hospital, Gyunggi-Do; Kyung Mi Jang, College of Medicine, Yeungnam University, Daegu; Jun Ho Lee, CHA Bundang Medical Center, CHA University School of Medicine, Gyunggi-Do; Jung Won Lee, Ewha Womans University School of Medicine, Seoul; In Seok Lim, College of Medicine, Chung-Ang University, Seoul; Eun Mi Yang, Chonnam National University Hospital, Gwangju; Kyung Hee Han, Jeju University Hospital, Jeju, Korea.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Noone, D.G.; Iijima, K.; Parekh, R. Idiopathic nephrotic syndrome in children. Lancet 2018, 392, 61–74. [Google Scholar] [CrossRef]
- Bierzynska, A.; McCarthy, H.J.; Soderquest, K.; Sen, E.S.; Colby, E.; Ding, W.Y.; Nabhan, M.M.; Kerecuk, L.; Hegde, S.; Hughes, D.; et al. Genomic and clinical profiling of a national nephrotic syndrome cohort advocates a precision medicine approach to disease management. Kidney Int. 2017, 91, 937–947. [Google Scholar] [CrossRef] [PubMed]
- Trautmann, A.; Bodria, M.; Ozaltin, F.; Gheisari, A.; Melk, A.; Azocar, M.; Anarat, A.; Caliskan, S.; Emma, F.; Gellermann, J.; et al. Spectrum of steroid-resistant and congenital nephrotic syndrome in children: The PodoNet registry cohort. Clin. J. Am. Soc. Nephrol. 2015, 10, 592–600. [Google Scholar] [CrossRef] [PubMed]
- Sadowski, C.E.; Lovric, S.; Ashraf, S.; Pabst, W.L.; Gee, H.Y.; Kohl, S.; Engelmann, S.; Vega-Warner, V.; Fang, H.; Halbritter, J.; et al. A single-gene cause in 29.5% of cases of steroid-resistant nephrotic syndrome. J. Am. Soc. Nephrol. 2015, 26, 1279–1289. [Google Scholar] [CrossRef]
- Wang, F.; Zhang, Y.; Mao, J.; Yu, Z.; Yi, Z.; Yu, L.; Sun, J.; Wei, X.; Ding, F.; Zhang, H.; et al. Spectrum of mutations in Chinese children with steroid-resistant nephrotic syndrome. Pediatr. Nephrol. 2017, 32, 1181–1192. [Google Scholar] [CrossRef]
- Nagano, C.; Yamamura, T.; Horinouchi, T.; Aoto, Y.; Ishiko, S.; Sakakibara, N.; Shima, Y.; Nakanishi, K.; Nagase, H.; Iijima, K.; et al. Comprehensive genetic diagnosis of Japanese patients with severe proteinuria. Sci. Rep. 2020, 10, 270. [Google Scholar] [CrossRef]
- Hildebrandt, F.; Heeringa, S.F. Specific podocin mutations determine age of onset of nephrotic syndrome all the way into adult life. Kidney Int. 2009, 75, 669–671. [Google Scholar] [CrossRef]
- Harita, Y. Application of next-generation sequencing technology to diagnosis and treatment of focal segmental glomerulosclerosis. Clin. Exp. Nephrol. 2018, 22, 491–500. [Google Scholar] [CrossRef]
- Groopman, E.E.; Rasouly, H.M.; Gharavi, A.G. Genomic medicine for kidney disease. Nat. Rev. Nephrol. 2018, 14, 83–104. [Google Scholar] [CrossRef]
- Lovric, S.; Ashraf, S.; Tan, W.; Hildebrandt, F. Genetic testing in steroid-resistant nephrotic syndrome: When and how? Nephrol. Dial. Transplant. 2016, 31, 1802–1813. [Google Scholar] [CrossRef]
- Preston, R.; Stuart, H.M.; Lennon, R. Genetic testing in steroid-resistant nephrotic syndrome: Why, who, when and how? Pediatr. Nephrol. 2019, 34, 195–210. [Google Scholar] [CrossRef]
- Hinkes, B.G.; Mucha, B.; Vlangos, C.N.; Gbadegesin, R.; Liu, J.; Hasselbacher, K.; Hangan, D.; Ozaltin, F.; Zenker, M.; Hildebrandt, F.; et al. Nephrotic syndrome in the first year of life: Two thirds of cases are caused by mutations in 4 genes (NPHS1, NPHS2, WT1, and LAMB2). Pediatrics 2007, 119, e907–e919. [Google Scholar] [CrossRef]
- Lee, J.H.; Han, K.H.; Lee, H.; Kang, H.G.; Moon, K.C.; Shin, J.I.; Hahn, H.; Park, Y.S.; Pai, K.S.; Cho, B.S.; et al. Genetic basis of congenital and infantile nephrotic syndromes. Am. J. Kidney Dis. 2011, 58, 1042–1043. [Google Scholar] [CrossRef]
- Cheong, H.I. Genetic tests in children with steroid-resistant nephrotic syndrome. Kidney Res. Clin. Pract. 2020, 39, 7–16. [Google Scholar] [CrossRef]
- Kidney Disease: Improving Global Outcomes (KDIGO) CKD Work Group. KDIGO 2015 Clinical Practice Guideline for glomerulonephritis. Kidney Int. Suppl. 2012, 2, 139–274. [Google Scholar]
- Cheong, H.I.; Chae, J.H.; Kim, J.S.; Park, H.W.; Ha, I.S.; Hwang, Y.S.; Lee, H.S.; Choi, Y. Hereditary glomerulopathy associated with a mitochondrial tRNA(Leu) gene mutation. Pediatr. Nephrol. 1999, 13, 477–480. [Google Scholar] [CrossRef]
- Li, H.; Durbin, R. Fast and accurate short read alignment with Burrows-Wheeler transform. Bioinformatics 2009, 25, 1754–1760. [Google Scholar] [CrossRef]
- Li, H.; Handsaker, B.; Wysoker, A.; Fennell, T.; Ruan, J.; Homer, N.; Marth, G.; Abecasis, G.; Durbin, R.; 1000 Genome Project Data Processing Subgroup. The Sequence Alignment/Map format and SAMtools. Bioinformatics 2009, 25, 2078–2079. [Google Scholar] [CrossRef]
- McKenna, A.; Hanna, M.; Banks, E.; Sivachenko, A.; Cibulskis, K.; Kernytsky, A.; Garimella, K.; Altshuler, D.; Gabriel, S.; Daly, M.; et al. The genome analysis toolkit: A MapReduce framework for analyzing next-generation DNA sequencing data. Genome Res. 2010, 20, 1297–1303. [Google Scholar] [CrossRef]
- Wang, K.; Li, M.; Hakonarson, H. ANNOVAR: Functional annotation of genetic variants from high-throughput sequencing data. Nucleic Acids Res. 2010, 38, e164. [Google Scholar] [CrossRef]
- Richards, S.; Aziz, N.; Bale, S.; Bick, D.; Das, S.; Gastier-Foster, J.; Grody, W.W.; Hegde, M.; Lyon, E.; Spector, E.; et al. Standards and guidelines for the interpretation of sequence variants: A joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet. Med. 2015, 17, 405–424. [Google Scholar] [CrossRef]
- Kang, H.G.; Lee, M.; Lee, K.B.; Hughes, M.; Kwon, B.S.; Lee, S.; McNagny, K.M.; Ahn, Y.H.; Ko, J.M.; Ha, I.S.; et al. Loss of podocalyxin causes a novel syndromic type of congenital nephrotic syndrome. Exp. Mol. Med. 2017, 49, e414. [Google Scholar] [CrossRef]
- Warejko, J.K.; Tan, W.; Daga, A.; Schapiro, D.; Lawson, J.A.; Shril, S.; Lovric, S.; Ashraf, S.; Rao, J.; Hermle, T.; et al. Whole exome sequencing of patients with steroid-resistant nephrotic syndrome. Clin. J. Am. Soc. Nephrol. 2018, 13, 53–62. [Google Scholar] [CrossRef]
- Boute, N.; Gribouval, O.; Roselli, S.; Benessy, F.; Lee, H.; Fuchshuber, A.; Dahan, K.; Gubler, M.C.; Niaudet, P.; Antignac, C. NPHS2, encoding the glomerular protein podocin, is mutated in autosomal recessive steroid-resistant nephrotic syndrome. Nat. Genet. 2000, 24, 349–354. [Google Scholar] [CrossRef]
- Tsukaguchi, H.; Sudhakar, A.; Le, T.C.; Nguyen, T.; Yao, J.; Schwimmer, J.A.; Schachter, A.D.; Poch, E.; Abreu, P.F.; Appel, G.B.; et al. NPHS2 mutations in late-onset focal segmental glomerulosclerosis: R229Q is a common disease-associated allele. J. Clin. Investig. 2002, 110, 1659–1666. [Google Scholar] [CrossRef]
- Park, E.; Ahn, Y.H.; Kang, H.G.; Yoo, K.H.; Won, N.H.; Lee, K.B.; Moon, K.C.; Seong, M.W.; Gwon, T.R.; Park, S.S.; et al. COQ6 mutations in children with steroid-resistant focal segmental glomerulosclerosis and sensorineural hearing loss. Am. J. Kidney Dis. 2017, 70, 139–144. [Google Scholar] [CrossRef]
- Park, E.; Kang, H.G.; Choi, Y.H.; Lee, K.B.; Moon, K.C.; Jeong, H.J.; Nagata, M.; Cheong, H.I. Focal segmental glomerulosclerosis and medullary nephrocalcinosis in children with ADCK4 mutations. Pediatr. Nephrol. 2017, 32, 1547–1554. [Google Scholar] [CrossRef]
- Park, E.; Ahn, Y.H.; Kang, H.G.; Miyake, N.; Tsukaguchi, H.; Cheong, H.I. NUP107 mutations in children with steroid-resistant nephrotic syndrome. Nephrol. Dial. Transplant. 2017, 32, 1013–1017. [Google Scholar]
- Lee, S.E.; Min, S.I.; Kim, Y.S.; Ha, J.; Ha, I.S.; Cheong, H.I.; Kim, S.J.; Choi, Y.; Kang, H.G. Recurrence of idiopathic focal segmental glomerulosclerosis after kidney transplantation: Experience of a Korean tertiary center. Pediatr. Transplant. 2014, 18, 369–376. [Google Scholar] [CrossRef]
- Bergmann, C. Advances in renal genetic diagnosis. Cell Tissue Res. 2017, 369, 93–104. [Google Scholar] [CrossRef]
- Lipska, B.S.; Ranchin, B.; Iatropoulos, P.; Gellermann, J.; Melk, A.; Ozaltin, F.; Caridi, G.; Seeman, T.; Tory, K.; Jankauskiene, A.; et al. Genotype-phenotype associations in WT1 glomerulopathy. Kidney Int. 2014, 85, 1169–1178. [Google Scholar] [CrossRef] [PubMed]
- Ahn, Y.H.; Park, E.J.; Kang, H.G.; Kim, S.H.; Cho, H.Y.; Shin, J.I.; Lee, J.H.; Park, Y.S.; Kim, K.S.; Ha, I.S.; et al. Genotype-phenotype analysis of pediatric patients with WT1 glomerulopathy. Pediatr. Nephrol. 2017, 32, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Heeringa, S.F.; Chernin, G.; Chaki, M.; Zhou, W.; Sloan, A.J.; Ji, Z.; Xie, L.X.; Salviati, L.; Hurd, T.W.; Vega-Warner, V.; et al. COQ6 mutations in human patients produce nephrotic syndrome with sensorineural deafness. J. Clin. Investig. 2011, 121, 2013–2024. [Google Scholar] [CrossRef] [PubMed]
- Ashraf, S.; Gee, H.Y.; Woerner, S.; Xie, L.X.; Vega-Warner, V.; Lovric, S.; Fang, H.; Song, X.; Cattran, D.C.; Avila-Casado, C.; et al. ADCK4 mutations promote steroid-resistant nephrotic syndrome through CoQ10 biosynthesis disruption. J. Clin. Investig. 2013, 123, 5179–5189. [Google Scholar] [CrossRef] [PubMed]
- Montini, G.; Malaventura, C.; Salviati, L. Early coenzyme Q10 supplementation in primary coenzyme Q10 deficiency. N. Engl. J. Med. 2008, 358, 2849–2850. [Google Scholar] [CrossRef] [PubMed]
- Jungraithmayr, T.C.; Hofer, K.; Cochat, P.; Chernin, G.; Cortina, G.; Fargue, S.; Grimm, P.; Knueppel, T.; Kowarsch, A.; Neuhaus, T.; et al. Screening for NPHS2 mutations may help predict FSGS recurrence after transplantation. J. Am. Soc. Nephrol. 2011, 22, 579–585. [Google Scholar] [CrossRef][Green Version]
- National Cancer Institute. NCI Dictionary of Genetics Terms. Available online: https://www.cancer.gov/publications/dictionaries/genetics-dictionary/def/phenocopy (accessed on 27 February 2020).
- Landini, S.; Mazzinghi, B.; Becherucci, F.; Allinovi, M.; Provenzano, A.; Palazzo, V.; Ravaglia, F.; Artuso, R.; Bosi, E.; Stagi, S.; et al. Reverse phenotyping after whole-exome sequencing in steroid-resistant nephrotic syndrome. Clin. J. Am. Soc. Nephrol. 2020, 15, 89–100. [Google Scholar] [CrossRef]
- Schaefer, F. It’s in your genes: Exome sequencing enables precision diagnostics in proteinuric kidney diseases. Clin. J. Am. Soc. Nephrol. 2020, 15, 10–12. [Google Scholar] [CrossRef]
- Kaplan, J.M.; Kim, S.H.; North, K.N.; Rennke, H.; Correia, L.A.; Tong, H.Q.; Mathis, B.J.; Rodríguez-Pérez, J.C.; Allen, P.G.; Beggs, A.H.; et al. Mutations in ACTN4, encoding alpha-actinin-4, cause familial focal segmental glomerulosclerosis. Nat. Genet. 2000, 24, 251–256. [Google Scholar] [CrossRef]
- Kranz, C.; Denecke, J.; Lehle, L.; Sohlbach, K.; Jeske, S.; Meinhardt, F.; Rossi, R.; Gudowius, S.; Marquardt, T. Congenital disorder of glycosylation type Ik (CDG-Ik): A defect of mannosyltransferase I. Am. J. Hum. Genet. 2004, 74, 545–551. [Google Scholar] [CrossRef][Green Version]
- Gbadegesin, R.A.; Hall, G.; Adeyemo, A.; Hanke, N.; Tossidou, I.; Burchette, J.; Wu, G.; Homstad, A.; Sparks, M.A.; Gomez, J.; et al. Mutations in the gene that encodes the F-actin binding protein anillin cause FSGS. J. Am. Soc. Nephrol. 2014, 25, 1991–2002. [Google Scholar] [CrossRef] [PubMed]
- Genovese, G.; Friedman, D.J.; Ross, M.D.; Lecordier, L.; Uzureau, P.; Freedman, B.I.; Bowden, D.W.; Langefeld, C.D.; Oleksyk, T.K.; Uscinski Knob, A.L.; et al. Association of trypanolytic ApoL1 variants with kidney disease in African Americans. Science 2010, 329, 841–845. [Google Scholar] [CrossRef]
- Akilesh, S.; Suleiman, H.; Yu, H.; Stander, M.C.; Lavin, P.; Gbadegesin, R.; Antignac, C.; Pollak, M.; Kopp, J.B.; Winn, M.P.; et al. Arhgap24 inactivates Rac1 in mouse podocytes, and a mutant form is associated with familial focal segmental glomerulosclerosis. J. Clin. Investig. 2011, 121, 4127–4137. [Google Scholar] [CrossRef]
- Gee, H.Y.; Saisawat, P.; Ashraf, S.; Hurd, T.W.; Vega-Warner, V.; Fang, H.; Beck, B.B.; Gribouval, O.; Zhou, W.; Diaz, K.A.; et al. ARHGDIA mutations cause nephrotic syndrome via defective RHO GTPase signaling. J. Clin. Investig. 2013, 123, 3243–3253. [Google Scholar] [CrossRef]
- Dear, T.N.; Meier, N.T.; Hunn, M.; Boehm, T. Gene structure, chromosomal localization, and expression pattern of Capn12, a new member of the calpain large subunit gene family. Genomics 2000, 68, 152–160. [Google Scholar] [CrossRef]
- Karamatic Crew, V.; Burton, N.; Kagan, A.; Green, C.A.; Levene, C.; Flinter, F.; Brady, R.L.; Daniels, G.; Anstee, D.J. CD151, the first member of the tetraspanin (TM4) superfamily detected on erythrocytes, is essential for the correct assembly of human basement membranes in kidney and skin. Blood 2004, 104, 2217–2223. [Google Scholar] [CrossRef]
- Löwik, M.M.; Groenen, P.J.; Pronk, I.; Lilien, M.R.; Goldschmeding, R.; Dijkman, H.B.; Levtchenko, E.N.; Monnens, L.A.; van den Heuvel, L.P. Focal segmental glomerulosclerosis in a patient homozygous for a CD2AP mutation. Kidney Int. 2007, 72, 1198–1203. [Google Scholar] [CrossRef]
- Sethi, S.; Fervenza, F.C.; Zhang, Y.; Smith, R.J. Secondary focal and segmental glomerulosclerosis associated with single-nucleotide polymorphisms in the genes encoding complement factor H and C3. Am. J. Kidney Dis. 2012, 60, 316–321. [Google Scholar] [CrossRef]
- Voskarides, K.; Damianou, L.; Neocleous, V.; Zouvani, I.; Christodoulidou, S.; Hadjiconstantinou, V.; Ioannou, K.; Athanasiou, Y.; Patsias, C.; Alexopoulos, E.; et al. COL4A3/COL4A4 mutations producing focal segmental glomerulosclerosis and renal failure in thin basement membrane nephropathy. J. Am. Soc. Nephrol. 2007, 18, 3004–3016. [Google Scholar] [CrossRef]
- Slajpah, M.; Gorinsek, B.; Berginc, G.; Vizjak, A.; Ferluga, D.; Hvala, A.; Meglic, A.; Jaksa, I.; Furlan, P.; Gregoric, A.; et al. Sixteen novel mutations identified in COL4A3, COL4A4, and COL4A5 genes in Slovenian families with Alport syndrome and benign familial hematuria. Kidney Int. 2007, 71, 1287–1295. [Google Scholar] [CrossRef] [PubMed]
- Salviati, L.; Sacconi, S.; Murer, L.; Zacchello, G.; Franceschini, L.; Laverda, A.M.; Basso, G.; Quinzii, C.; Angelini, C.; Hirano, M.; et al. Infantile encephalomyopathy and nephropathy with CoQ10 deficiency: A CoQ10-responsive condition. Neurology 2005, 65, 606–608. [Google Scholar] [CrossRef] [PubMed]
- Ebarasi, L.; Ashraf, S.; Bierzynska, A.; Gee, H.Y.; McCarthy, H.J.; Lovric, S.; Sadowski, C.E.; Pabst, W.; Vega-Warner, V.; Fang, H.; et al. Defects of CRB2 cause steroid-resistant nephrotic syndrome. Am. J. Hum. Genet. 2015, 96, 153–161. [Google Scholar] [CrossRef] [PubMed]
- Ovunc, B.; Otto, E.A.; Vega-Warner, V.; Saisawat, P.; Ashraf, S.; Ramaswami, G.; Fathy, H.M.; Schoeb, D.; Chernin, G.; Lyons, R.H.; et al. Exome sequencing reveals cubilin mutation as a single-gene cause of proteinuria. J. Am. Soc. Nephrol. 2011, 22, 1815–1820. [Google Scholar] [CrossRef] [PubMed]
- Ozaltin, F.; Li, B.; Rauhauser, A.; An, S.W.; Soylemezoglu, O.; Gonul, I.I.; Taskiran, E.Z.; Ibsirlioglu, T.; Korkmaz, E.; Bilginer, Y.; et al. DGKE variants cause a glomerular microangiopathy that mimics membranoproliferative GN. J. Am. Soc. Nephrol. 2013, 24, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Izu, A.; Yanagida, H.; Sugimoto, K.; Fujita, S.; Sakata, N.; Wada, N.; Okada, M.; Takemura, T. Pathogenesis of focal segmental glomerular sclerosis in a girl with the partial deletion of chromosome 6p. Tohoku J. Exp. Med. 2011, 223, 187–192. [Google Scholar] [CrossRef]
- Gee, H.Y.; Ashraf, S.; Wan, X.; Vega-Warner, V.; Esteve-Rudd, J.; Lovric, S.; Fang, H.; Hurd, T.W.; Sadowski, C.E.; Allen, S.J.; et al. Mutations in EMP2 cause childhood-onset nephrotic syndrome. Am. J. Hum. Genet. 2014, 94, 884–890. [Google Scholar] [CrossRef]
- Castelletti, F.; Donadelli, R.; Banterla, F.; Hildebrandt, F.; Zipfel, P.F.; Bresin, E.; Otto, E.; Skerka, C.; Renieri, A.; Todeschini, M.; et al. Mutations in FN1 cause glomerulopathy with fibronectin deposits. Proc. Natl. Acad. Sci. USA 2008, 105, 2538–2543. [Google Scholar] [CrossRef]
- Moudgil, A.; Perriello, P.; Loechelt, B.; Przygodzki, R.; Fitzerald, W.; Kamani, N. Immunodysregulation, polyendocrinopathy, enteropathy, X-linked (IPEX) syndrome: An unusual cause of proteinuria in infancy. Pediatr. Nephrol. 2007, 22, 1799–1802. [Google Scholar] [CrossRef]
- Okamoto, K.; Tokunaga, K.; Doi, K.; Fujita, T.; Suzuki, H.; Katoh, T.; Watanabe, T.; Nishida, N.; Mabuchi, A.; Takahashi, A.; et al. Common variation in GPC5 is associated with acquired nephrotic syndrome. Nat. Genet. 2011, 43, 459–463. [Google Scholar] [CrossRef]
- Barua, M.; Brown, E.J.; Charoonratana, V.T.; Genovese, G.; Sun, H.; Pollak, M.R. Mutations in the INF2 gene account for a significant proportion of familial but not sporadic focal and segmental glomerulosclerosis. Kidney Int. 2013, 83, 316–322. [Google Scholar] [CrossRef]
- Has, C.; Spartà, G.; Kiritsi, D.; Weibel, L.; Moeller, A.; Vega-Warner, V.; Waters, A.; He, Y.; Anikster, Y.; Esser, P.; et al. Integrin α3 mutations with kidney, lung, and skin disease. N. Engl. J. Med. 2012, 366, 1508–1514. [Google Scholar] [CrossRef]
- Kambham, N.; Tanji, N.; Seigle, R.L.; Markowitz, G.S.; Pulkkinen, L.; Uitto, J.; D’Agati, V.D. Congenital focal segmental glomerulosclerosis associated with beta4 integrin mutation and epidermolysis bullosa. Am. J. Kidney Dis. 2000, 36, 190–196. [Google Scholar] [CrossRef]
- Gee, H.Y.; Zhang, F.; Ashraf, S.; Kohl, S.; Sadowski, C.E.; Vega-Warner, V.; Zhou, W.; Lovric, S.; Fang, H.; Nettleton, M.; et al. KANK deficiency leads to podocyte dysfunction and nephrotic syndrome. J. Clin. Investig. 2015, 125, 2375–2384. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, R.; Hoffman, M.; Cliften, P.; Seshan, S.; Liapis, H.; Jain, S. Targeted exome sequencing integrated with clinicopathological information reveals novel and rare mutations in atypical, suspected and unknown cases of Alport syndrome or proteinuria. PLoS ONE 2013, 8, e76360. [Google Scholar] [CrossRef]
- Zenker, M.; Aigner, T.; Wendler, O.; Tralau, T.; Müntefering, H.; Fenski, R.; Pitz, S.; Schumacher, V.; Royer-Pokora, B.; Wühl, E.; et al. Human laminin beta2 deficiency causes congenital nephrosis with mesangial sclerosis and distinct eye abnormalities. Hum. Mol. Genet. 2004, 13, 2625–2632. [Google Scholar] [CrossRef] [PubMed]
- Thong, K.M.; Xu, Y.; Cook, J.; Takou, A.; Wagner, B.; Kawar, B.; Ong, A.C. Cosegregation of focal segmental glomerulosclerosis in a family with familial partial lipodystrophy due to a mutation in LMNA. Nephron Clin. Pract. 2013, 124, 31–37. [Google Scholar] [CrossRef] [PubMed]
- Dreyer, S.D.; Zhou, G.; Baldini, A.; Winterpacht, A.; Zabel, B.; Cole, W.; Johnson, R.L.; Lee, B. Mutations in LMX1B cause abnormal skeletal patterning and renal dysplasia in nail patella syndrome. Nat. Genet. 1998, 19, 47–50. [Google Scholar] [CrossRef] [PubMed]
- Shohat, M.; Magal, N.; Shohat, T.; Chen, X.; Dagan, T.; Mimouni, A.; Danon, Y.; Lotan, R.; Ogur, G.; Sirin, A.; et al. Phenotype-genotype correlation in familial Mediterranean fever: Evidence for an association between Met694Val and amyloidosis. Eur. J. Hum. Genet. 1999, 7, 287–292. [Google Scholar] [CrossRef]
- Sanna-Cherchi, S.; Burgess, K.E.; Nees, S.N.; Caridi, G.; Weng, P.L.; Dagnino, M.; Bodria, M.; Carrea, A.; Allegretta, M.A.; Kim, H.R.; et al. Exome sequencing identified MYO1E and NEIL1 as candidate genes for human autosomal recessive steroid-resistant nephrotic syndrome. Kidney Int. 2011, 80, 389–396. [Google Scholar] [CrossRef]
- Brunelli, S.M.; Meyers, K.E.; Guttenberg, M.; Kaplan, P.; Kaplan, B.S. Cobalamin C deficiency complicated by an atypical glomerulopathy. Pediatr. Nephrol. 2002, 17, 800–803. [Google Scholar] [CrossRef]
- Yasukawa, T.; Suzuki, T.; Ueda, T.; Ohta, S.; Watanabe, K. Modification defect at anticodon wobble nucleotide of mitochondrial tRNAs(Leu)(UUR) with pathogenic mutations of mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes. J. Biol. Chem. 2000, 275, 4251–4257. [Google Scholar] [CrossRef] [PubMed]
- Scaglia, F.; Vogel, H.; Hawkins, E.P.; Vladutiu, G.D.; Liu, L.L.; Wong, L.J. Novel homoplasmic mutation in the mitochondrial tRNATyr gene associated with atypical mitochondrial cytopathy presenting with focal segmental glomerulosclerosis. Am. J. Med. Genet. A 2003, 123, 172–178. [Google Scholar] [CrossRef] [PubMed]
- Kopp, J.B.; Smith, M.W.; Nelson, G.W.; Johnson, R.C.; Freedman, B.I.; Bowden, D.W.; Oleksyk, T.; McKenzie, L.M.; Kajiyama, H.; Ahuja, T.S.; et al. MYH9 is a major-effect risk gene for focal segmental glomerulosclerosis. Nat. Genet. 2008, 40, 1175–1184. [Google Scholar] [CrossRef] [PubMed]
- Mele, C.; Iatropoulos, P.; Donadelli, R.; Calabria, A.; Maranta, R.; Cassis, P.; Buelli, S.; Tomasoni, S.; Piras, R.; Krendel, M.; et al. MYO1E mutations and childhood familial focal segmental glomerulosclerosis. N. Engl. J. Med. 2011, 365, 295–306. [Google Scholar] [CrossRef] [PubMed]
- Kestilä, M.; Lenkkeri, U.; Männikkö, M.; Lamerdin, J.; McCready, P.; Putaala, H.; Ruotsalainen, V.; Morita, T.; Nissinen, M.; Herva, R.; et al. Positionally cloned gene for a novel glomerular protein--nephrin--is mutated in congenital nephrotic syndrome. Mol. Cell 1998, 1, 575–582. [Google Scholar] [CrossRef]
- Miyake, N.; Tsukaguchi, H.; Koshimizu, E.; Shono, A.; Matsunaga, S.; Shiina, M.; Mimura, Y.; Imamura, S.; Hirose, T.; Okudela, K.; et al. Biallelic Mutations in Nuclear Pore Complex Subunit NUP107 Cause Early-Childhood-Onset Steroid-Resistant Nephrotic Syndrome. Am. J. Hum. Genet. 2015, 97, 555–566. [Google Scholar] [CrossRef]
- Esposito, T.; Lea, R.A.; Maher, B.H.; Moses, D.; Cox, H.C.; Magliocca, S.; Angius, A.; Nyholt, D.R.; Titus, T.; Kay, T.; et al. Unique X-linked familial FSGS with co-segregating heart block disorder is associated with a mutation in the NXF5 gene. Hum. Mol. Genet. 2013, 22, 3654–3666. [Google Scholar] [CrossRef] [PubMed]
- Kerti, A.; Csohány, R.; Wagner, L.; Jávorszky, E.; Maka, E.; Tory, K. NPHS2 homozygous p.R229Q variant: Potential modifier instead of causal effect in focal segmental glomerulosclerosis. Pediatr. Nephrol. 2013, 28, 2061–2064. [Google Scholar] [CrossRef]
- López, L.C.; Schuelke, M.; Quinzii, C.M.; Kanki, T.; Rodenburg, R.J.; Naini, A.; Dimauro, S.; Hirano, M. Leigh syndrome with nephropathy and CoQ10 deficiency due to decaprenyl diphosphate synthase subunit 2 (PDSS2) mutations. Am. J. Hum. Genet. 2006, 79, 1125–1129. [Google Scholar] [CrossRef]
- Gbadegesin, R.; Hinkes, B.G.; Hoskins, B.E.; Vlangos, C.N.; Heeringa, S.F.; Liu, J.; Loirat, C.; Ozaltin, F.; Hashmi, S.; Ulmer, F.; et al. Mutations in PLCE1 are a major cause of isolated diffuse mesangial sclerosis (IDMS). Nephrol. Dial. Transplant. 2008, 23, 1291–1297. [Google Scholar] [CrossRef]
- Ozaltin, F.; Ibsirlioglu, T.; Taskiran, E.Z.; Baydar, D.E.; Kaymaz, F.; Buyukcelik, M.; Kilic, B.D.; Balat, A.; Iatropoulos, P.; Asan, E.; et al. Disruption of PTPRO causes childhood-onset nephrotic syndrome. Am. J. Hum. Genet. 2011, 89, 139–147. [Google Scholar] [CrossRef] [PubMed]
- Berkovic, S.F.; Dibbens, L.M.; Oshlack, A.; Silver, J.D.; Katerelos, M.; Vears, D.F.; Lüllmann-Rauch, R.; Blanz, J.; Zhang, K.W.; Stankovich, J.; et al. Array-based gene discovery with three unrelated subjects shows SCARB2/LIMP-2 deficiency causes myoclonus epilepsy and glomerulosclerosis. Am. J. Hum. Genet. 2008, 82, 673–684. [Google Scholar] [CrossRef] [PubMed]
- Boerkoel, C.F.; Takashima, H.; John, J.; Yan, J.; Stankiewicz, P.; Rosenbarker, L.; André, J.L.; Bogdanovic, R.; Burguet, A.; Cockfield, S.; et al. Mutant chromatin remodeling protein SMARCAL1 causes Schimke immuno-osseous dysplasia. Nat. Genet. 2002, 30, 215–220. [Google Scholar] [CrossRef] [PubMed]
- Dai, S.; Wang, Z.; Pan, X.; Wang, W.; Chen, X.; Ren, H.; Hao, C.; Han, B.; Chen, N. Functional analysis of promoter mutations in the ACTN4 and SYNPO genes in focal segmental glomerulosclerosis. Nephrol. Dial. Transplant. 2010, 25, 824–835. [Google Scholar] [CrossRef][Green Version]
- Santín, S.; Ars, E.; Rossetti, S.; Salido, E.; Silva, I.; García-Maset, R.; Giménez, I.; Ruíz, P.; Mendizábal, S.; Luciano Nieto, J.; et al. TRPC6 mutational analysis in a large cohort of patients with focal segmental glomerulosclerosis. Nephrol. Dial. Transplant. 2009, 24, 3089–3096. [Google Scholar] [CrossRef]
- Huynh Cong, E.; Bizet, A.A.; Boyer, O.; Woerner, S.; Gribouval, O.; Filhol, E.; Arrondel, C.; Thomas, S.; Silbermann, F.; Canaud, G.; et al. A homozygous missense mutation in the ciliary gene TTC21B causes familial FSGS. J. Am. Soc. Nephrol. 2014, 25, 2435–2443. [Google Scholar] [CrossRef]
- Colin, E.; Huynh Cong, E.; Mollet, G.; Guichet, A.; Gribouval, O.; Arrondel, C.; Boyer, O.; Daniel, L.; Gubler, M.C.; Ekinci, Z.; et al. Loss-of-function mutations in WDR73 are responsible for microcephaly and steroid-resistant nephrotic syndrome: Galloway-Mowat syndrome. Am. J. Hum. Genet. 2014, 95, 637–648. [Google Scholar] [CrossRef]
- Barbaux, S.; Niaudet, P.; Gubler, M.C.; Grünfeld, J.P.; Jaubert, F.; Kuttenn, F.; Fékété, C.N.; Souleyreau-Therville, N.; Thibaud, E.; Fellous, M.; et al. Donor splice-site mutations in WT1 are responsible for Frasier syndrome. Nat. Genet. 1997, 17, 467–470. [Google Scholar] [CrossRef]
- Pelletier, J.; Bruening, W.; Kashtan, C.E.; Mauer, S.M.; Manivel, J.C.; Striegel, J.E.; Houghton, D.C.; Junien, C.; Habib, R.; Fouser, L.; et al. Germline mutations in the Wilms’ tumor suppressor gene are associated with abnormal urogenital development in Denys-Drash syndrome. Cell 1991, 67, 437–447. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).