Survival Outcomes of Patients with Pathologically Proven Positive Lymph Nodes at Time of Radical Cystectomy with or without Neoadjuvant Chemotherapy
Abstract
:1. Introduction
2. Materials and Methods
2.1. Patients
2.2. Primary and Secondary Endpoints and Statistics
3. Results
3.1. Clinical and Pathological Features of the Entire Cohort (n = 450)
3.2. Comparisons of Clinical and Pathological Features Stratified by NAC Administration
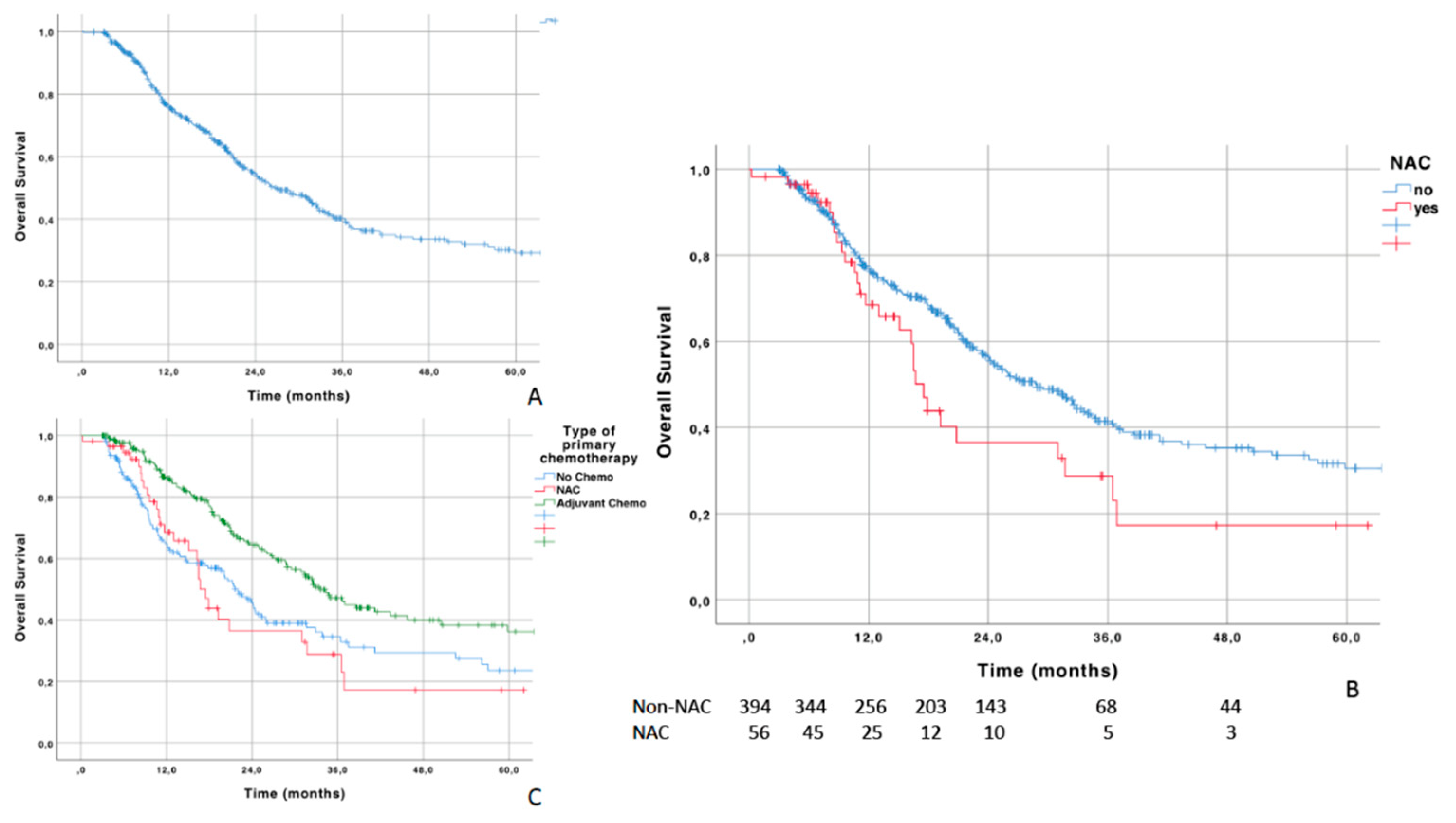
3.3. Survival Analysis in the Overall Cohort
3.4. Multivariable Analysis of Predictive Factors for OS in the Overall Cohort
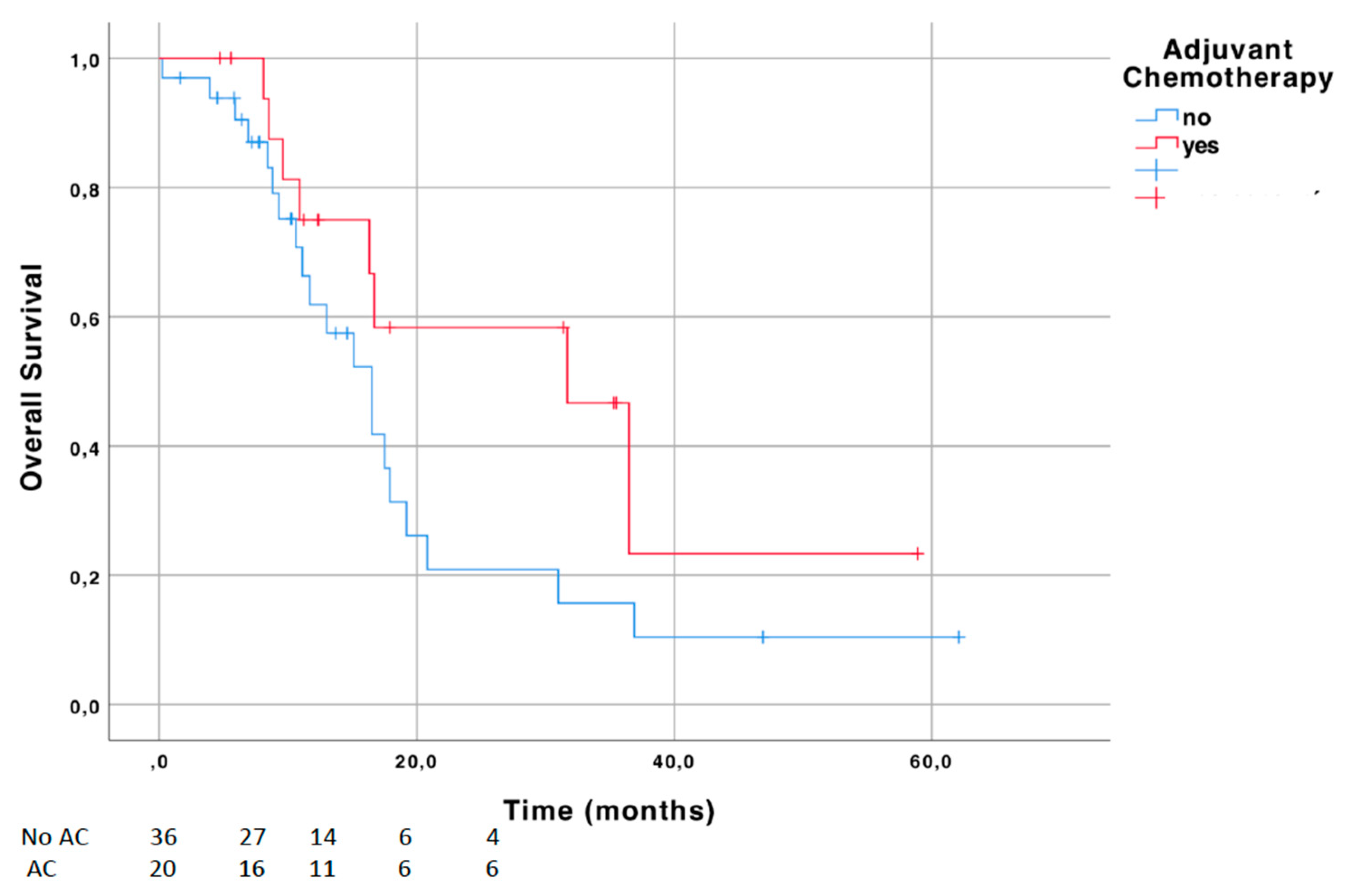
3.5. Stratified Survival Analysis in NAC Cohort
3.6. Multivariable Analysis of Factors Associated with Overall Mortality in the NAC Cohort
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Griffiths, G.; Hall, R.; Sylvester, R.; Raghavan, D.; Parmar, M.K.; Club Urologico Espanol de Tratamiento Oncologico Group. International phase III trial assessing neoadjuvant cisplatin, methotrexate, and vinblastine chemotherapy for muscle-invasive bladder cancer: Longterm results of the BA06 30894 trial. J. Clin. Oncol. 2011, 29, 2171. [Google Scholar] [PubMed] [Green Version]
- Grossman, H.B.; Natale, R.B.; Tangen, C.M.; Speights, V.O.; Vogelzang, N.J.; Trump, D.L.; White, R.W.D.; Sarosdy, M.F.; Wood, D.P., Jr.; Raghavan, D.; et al. Neoadjuvant chemotherapy plus cystectomy compared with cystectomy alone for locally advanced bladder cancer. N. Engl. J. Med. 2003, 349, 859–866. [Google Scholar] [CrossRef] [PubMed]
- Vale, C.L.; Advanced Bladder Cancer (ABC) Meta-analysis Collaboration. Neoadjuvant chemotherapy in invasive bladder cancer: Update of a systematic review and meta-analysis of individual patient data advanced bladder cancer (ABC) meta analysis collaboration. Eur. Urol. 2005, 48, 202–206. [Google Scholar] [CrossRef] [PubMed]
- Zargar-Shoshtari, K.; Zargar, H.; Lotan, Y.; Shah, J.B.; van Rhijn, B.W.; Daneshmand, S.; Spiess, P.E.; Black, P.C.; Fairey, L.S.M.C.A.S.; Fairey, A.S.; et al. A Multi-Institutional Analysis of Outcomes of Patients with Clinically Node Positive Urothelial Bladder Cancer Treated with Induction Chemotherapy and Radical Cystectomy. J. Urol. 2016, 195, 53–59. [Google Scholar] [CrossRef]
- Mertens, L.S.; Meijer, R.P.; Meinhardt, W.; Van Der Poel, H.G.; Bex, A.; Kerst, J.M.; Van Der Heijden, M.S.; Bergman, A.M.; Horenblas, S.; Van Rhijn, B.W.G. Occult lymph node metastases in patients with carcinoma invading bladder muscle: Incidence after neoadjuvant chemotherapy and cystectomy vs. after cystectomy alone. BJU Int. 2014, 114, 67–74. [Google Scholar] [CrossRef] [PubMed]
- Tan, W.S.; Lamb, B.W.; Payne, H.; Hughes, S.; Green, J.S.; Lane, T.; Adshead, J.; Boustead, G.; Vasdev, N. Management of Node-Positive Bladder Cancer after Neoadjuvant Chemotherapy and Radical Cystectomy: A Survey of Current UK Practice. Clin. Genitourin. Cancer 2015, 13, e153–e158. [Google Scholar] [CrossRef] [PubMed]
- Hermans, T.J.; van de Putte, E.E.F.; Horenblas, S.; Meijer, R.P.; Boormans, J.L.; Aben, K.K.H.; Van Der Heijden, M.S.; De Wit, R.; Beerepoot, L.V.; Verhoeven, R.; et al. Pathological downstaging and survival after induction chemotherapy and radical cystectomy for clinically node-positive bladder cancer-Results of a nationwide population-based study. Eur. J. Cancer 2016, 69, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Herr, H.W.; Dotan, Z.; Donat, S.M.; Bajorin, D.F. Defining optimal therapy for muscle invasive bladder cancer. J. Urol. 2007, 177, 437–443. [Google Scholar] [CrossRef] [PubMed]
- Kassouf, W.; Agarwal, P.K.; Grossman, H.B.; Leibovici, D.; Munsell, M.F.; Siefker-Radtke, A.; Pisters, L.L.; Swanson, D.A.; Dinney, C.P.N.; Kamatbe, A.M. Outcome of patients with bladder cancer with pNþ disease after preoperative chemotherapy and radical cystectomy. Urology 2009, 73, 147–152. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zargar, H.; Shah, J.B.; van Rhijn, B.W.; Daneshmand, S.; Bivalacqua, T.J.; Spiess, P.E.; Black, P.C.; Kassouf, W.; Van De Putte, E.E.F.; Horenblas, S.; et al. Neoadjuvant Dose Dense MVAC versus Gemcitabine and Cisplatin in Patients with cT3-4aN0M0 Bladder Cancer Treated with Radical Cystectomy. J. Urol. 2018, 199, 1452–1458. [Google Scholar] [CrossRef] [PubMed]
- Loehrer, P.J.; Einhorn, L.H.; Elson, P.J.; Crawford, E.D.; Kuebler, P.; Tannock, I.; Raghavan, D.; Stuart-Harris, R.; Sarosdy, M.F.; Lowe, B.A. A randomized comparison of cisplatin alone or in combination with methotrexate, vinblastine, and doxorubicin in patients with metastatic urothelial carcinoma: A cooperative group study. J. Clin. Oncol. 1992, 10, 1066–1073. [Google Scholar] [CrossRef] [PubMed]
- von der Maase, H.; Hansen, S.W.; Roberts, J.T.; Dogliotti, L.; Oliver, T.; Moore, M.; Bodrogi, I.; Albers, P.; Knuth, A.; Lippert, C.; et al. Gemcitabine and cisplatin versus methotrexate, vinblastine, doxorubicin, and cisplatin in advanced or metastatic bladder cancer: Results of a large, randomized, multinational, multicenter, phase III study. J. Clin. Oncol. 2000, 18, 3068–3077. [Google Scholar] [CrossRef] [PubMed]
- Paz-Ares, L.; Solsona, E.; Esteban, E.; Saez, A.; Gonzalez-Larriba, J.; Anton, A.; de la Rosa, F.; Guillem, V.; Bellmunt, J. On behalf of the SOGUG and GUO-AEU groups Randomized phase III trial comparing adjuvant paclitaxel/gemcitabine/cisplatin (PGC to observation in patients with resected invasive bladder cancer: Results of the SOGUG (Spanish Oncology Genito-Urinary Group) 99/01 study. J. Clin. Oncol. 2010, 4518. [Google Scholar] [CrossRef]
- Sternberg, C.N.; Skoneczna, I.; Kerst, J.M.; Albers, P.; Fossa, S.D.; Agerbaek, M.; Dumez, H.; de Santis, M.; Théodore, C.; Leahy, M.G.; et al. Immediate versus deferred chemotherapy after radical cystectomy in patients with pT3-pT4 or N1M0 urothelial carcinoma of the bladder (EORTC 30994): An intergroup, open-label, randomised phase 3 trial. Lancet Oncol. 2015, 16, 76–86. [Google Scholar] [CrossRef]
- Leow, J.J.; Martin-Doyle, W.; Rajagopal, P.S.; Patel, C.G.; Anderson, E.M.; Rothman, A.T.; Cote, R.J.; Urun, Y.; Chang, S.L.; Choueiri, T.K.; et al. Adjuvant chemotherapy for invasive bladder cancer: A 2013 updated systematic review and meta-analysis of randomized trials. Eur. Urol. 2014, 66, 42–54. [Google Scholar] [CrossRef] [PubMed]
- Wosnitzer, M.S.; Hruby, G.W.; Murphy, A.M.; Barlow, L.J.; Cordon-Cardo, C.; Mansukhani, M.; Petrylak, D.P.; Benson, M.C.; McKiernan, J.M.; Cordon-Cardo, C. A comparison of the outcomes of neoadjuvant and adjuvant chemotherapy for clinical T2-T4aN0-N2M0 bladder cancer. Cancer 2012, 118, 358–364. [Google Scholar] [CrossRef] [PubMed]
- Necchi, A.; Anichini, A.; Raggi, D.; Briganti, A.; Massa, S.; Lucianò, R.; Colecchia, M.; Giannatempo, P.; Mortarini, R.; Bianchi, M.; et al. Pembrolizumab as Neoadjuvant Therapy Before Radical Cystectomy in Patients With Muscle-Invasive Urothelial Bladder Carcinoma (PURE-01): An Open-Label, Single-Arm, Phase II Study. J. Clin. Oncol. 2018, 20, 3353–3360. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zaghloul, M.S.; Christodouleas, J.P.; Smith, A.; Abdallah, A.; William, H.; Khaled, H.M.; Hwang, W.-T.; Baumann, B.C. Adjuvant sandwich chemotherapy plus radiotherapy vs. adjuvant chemotherapy alone for locally advanced bladder cancer after radical cystectomy. A randomized phase 2 trial. JAMA Surg. 2018, 153, e174591. [Google Scholar] [CrossRef] [PubMed]
| N = 450 | |
|---|---|
| Gender (n, %): | |
| Male | 329 (73.1) |
| Female | 121 (26.9) |
| Age (years): | |
| Mean | 67.5 |
| Median (range) IQR | 69.0 (25–93) |
| Pathological stage (n, %): | |
| pT0-pTis | 12 (2.6) |
| pT1 | 11 (2.4) |
| pT2 | 78 (17.3) |
| pT3 | 247 (54.9) |
| pT4 | 102 (22.7) |
| Presence of lymphovascular invasion (n, %) | 302 (67.1) |
| Presence of concomitant CIS (n, %) | 181 (40.2) |
| Presence of soft tissue surgical margins (n, %) | 58 (12.9) |
| Number of lymph nodes analyzed: | |
| Mean | 17.5 |
| Median (range) IQR | 16.0 (1–70) |
| Number of positive lymph nodes: | |
| Mean | 3.9 |
| Median (range) IQR | 2.0 (1–41) |
| Type of chemotherapy regimen (%): | |
| None | 170 (37.8) |
| Neoadjuvant without adjuvant | 36 (8.0) |
| Neoadjuvant + adjuvant | 20 (4.4) |
| Adjuvant only | 224 (54.2) |
| All-cause death (%) | 220 (48.9) |
| Follow-up (months): | |
| Mean | 23.0 |
| Median (range) IQR | 17.3 (3–130) |
| NAC Cohort | Non-NAC Cohort | p-Value | |
|---|---|---|---|
| N = 56 | N = 394 | ||
| Male (%) gender | 46 (82.1) | 283 (71.8) | 0.103 |
| Age (mean) | 65.0 | 68.0 | 0.051 |
| Pathological stage (%): | 0.097 | ||
| pT0-pTis | 3 (5.4) | 9 (2.3) | |
| pT1 | 3 (5.4) | 8 (2.0) | |
| pT2 | 6 (10.7) | 72 (18.3) | |
| pT3 | 29 (51.8) | 218 (55.3) | |
| pT4 | 15 (26.8) | 87 (22.1) | |
| Previous history of non-muscle-invasive bladder tumor before T2-4 diagnosis (%) | 6 (10.7) | 17 (4.3) | 0.042 |
| Presence of lymphovascular invasion (%) | 42 (75.0) | 260 (66.0) | 0.179 |
| Presence of concomitant CIS (%) | 17 (30.4) | 164 (41.6) | 0.108 |
| Soft tissue surgical margins (%) | 7 (12.5) | 51 (12.9) | 0.926 |
| Number of lymph nodes analyzed yield (mean) | 17.6 | 17.1 | 0.777 |
| Number of positive lymph nodes (mean) | 3.8 | 4.8 | 0.197 |
| Adjuvant chemotherapy administration (%) | 20 (35.7) | 224 (56.9) | 0.003 |
| Distant metastases (%) | 34 (60.7) | 154 (39.1) | 0.002 |
| HR | 95% CI | p-Value | |
|---|---|---|---|
| Overall cohort | |||
| Model 1 | |||
| Gender | 0.884 | 0.647–1.209 | 0.441 |
| Age (continuous) | 1.009 | 0.996–1.023 | 0.178 |
| Muscle-invasive disease | 2.404 | 1.062–5.442 | 0.035 |
| Lymphovascular invasion | 0.882 | 0.664–1.171 | 0.385 |
| Concomitant CIS | 1.088 | 0.830–1.427 | 0.540 |
| Soft tissue surgical margin | 1.338 | 0.910–1.965 | 0.138 |
| Positive lymph nodes >3 | 1.283 | 0.959–1.717 | 0.093 |
| NAC | 1.638 | 1.089–2.465 | 0.018 |
| Model 2 | |||
| NAC | 1.445 | 0.968–2.159 | 0.072 |
| Adjuvant Chemotherapy | 0.557 | 0.426–0.728 | <0.001 |
| NAC cohort | |||
| Muscle-invasive disease | 0.296 | 0.060–1.470 | 0.137 |
| Positive lymph nodes >3 | 3.281 | 1.287–8.365 | 0.013 |
| Adjuvant chemotherapy | 0.310 | 0.120–0.800 | 0.015 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ploussard, G.; Pradere, B.; Beauval, J.-B.; Chevreau, C.; Almeras, C.; Suc, E.; Gautier, J.-R.; Laurenty, A.-P.; Roumiguié, M.; Loison, G.; et al. Survival Outcomes of Patients with Pathologically Proven Positive Lymph Nodes at Time of Radical Cystectomy with or without Neoadjuvant Chemotherapy. J. Clin. Med. 2020, 9, 1962. https://doi.org/10.3390/jcm9061962
Ploussard G, Pradere B, Beauval J-B, Chevreau C, Almeras C, Suc E, Gautier J-R, Laurenty A-P, Roumiguié M, Loison G, et al. Survival Outcomes of Patients with Pathologically Proven Positive Lymph Nodes at Time of Radical Cystectomy with or without Neoadjuvant Chemotherapy. Journal of Clinical Medicine. 2020; 9(6):1962. https://doi.org/10.3390/jcm9061962
Chicago/Turabian StylePloussard, Guillaume, Benjamin Pradere, Jean-Baptiste Beauval, Christine Chevreau, Christophe Almeras, Etienne Suc, Jean-Romain Gautier, Anne-Pascale Laurenty, Mathieu Roumiguié, Guillaume Loison, and et al. 2020. "Survival Outcomes of Patients with Pathologically Proven Positive Lymph Nodes at Time of Radical Cystectomy with or without Neoadjuvant Chemotherapy" Journal of Clinical Medicine 9, no. 6: 1962. https://doi.org/10.3390/jcm9061962
APA StylePloussard, G., Pradere, B., Beauval, J.-B., Chevreau, C., Almeras, C., Suc, E., Gautier, J.-R., Laurenty, A.-P., Roumiguié, M., Loison, G., Tollon, C., Mourey, L., Salin, A., Xylinas, E., & Pouessel, D. (2020). Survival Outcomes of Patients with Pathologically Proven Positive Lymph Nodes at Time of Radical Cystectomy with or without Neoadjuvant Chemotherapy. Journal of Clinical Medicine, 9(6), 1962. https://doi.org/10.3390/jcm9061962







