Approach to Pulmonary Arteriovenous Malformations: A Comprehensive Update
Abstract
1. Introduction
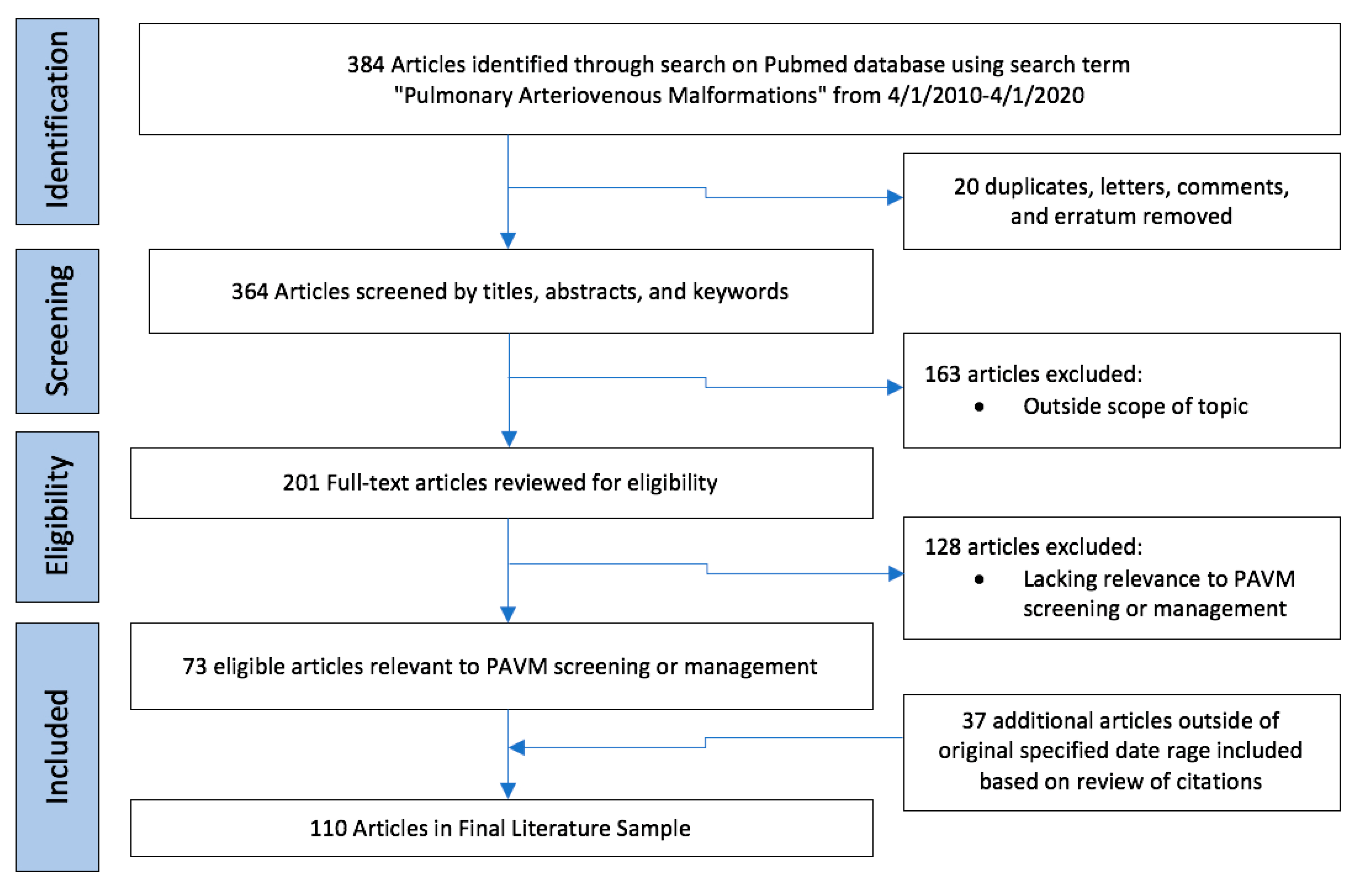
2. Methods
3. Screening Protocol in Patient with Suspicion for PAVM
3.1. Transthoracic Contrast Echocardiography
3.2. Contrast Versus Noncontrast Thoracic CT
4. Management of PAVM by Sub-Populations
4.1. Small PAVMs
4.2. Pediatric Patients
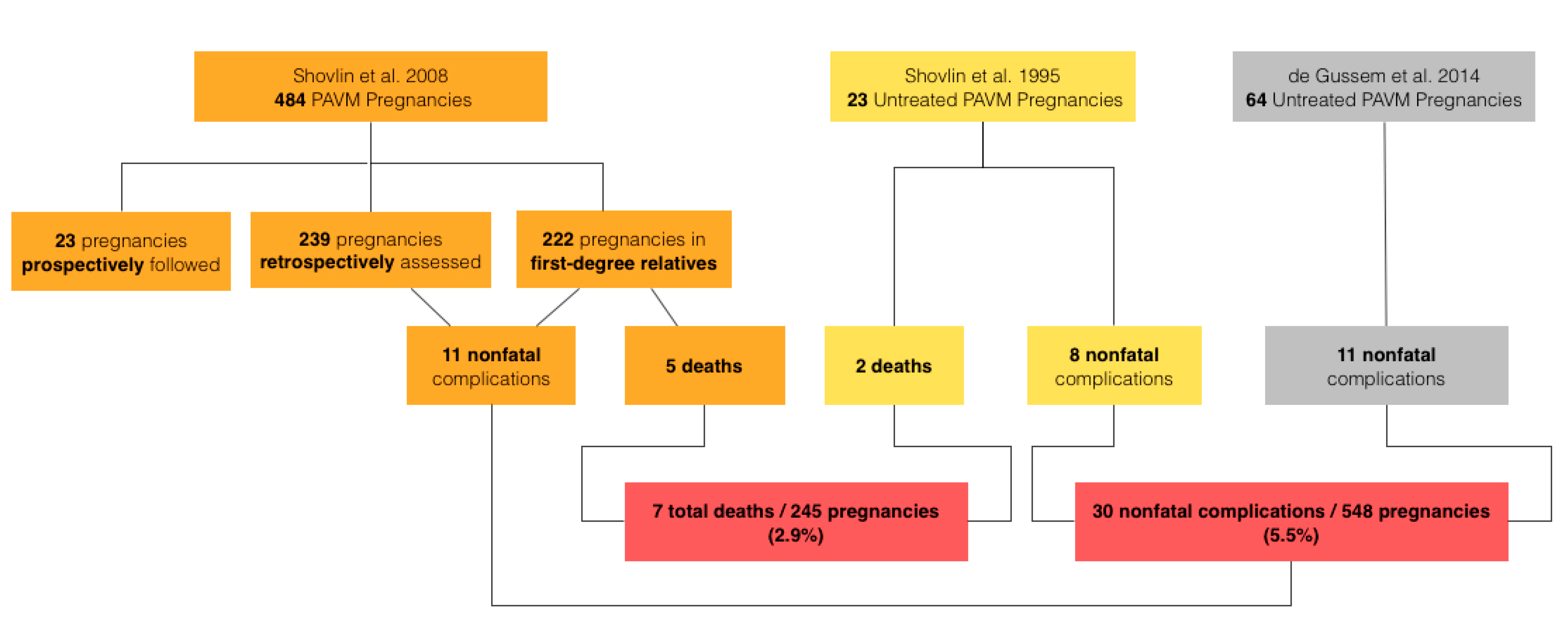
4.3. PAVMs in Pregnancy
4.4. Persistent PAVMs
4.5. Diffuse PAVMs
4.6. Pulmonary Hypertension
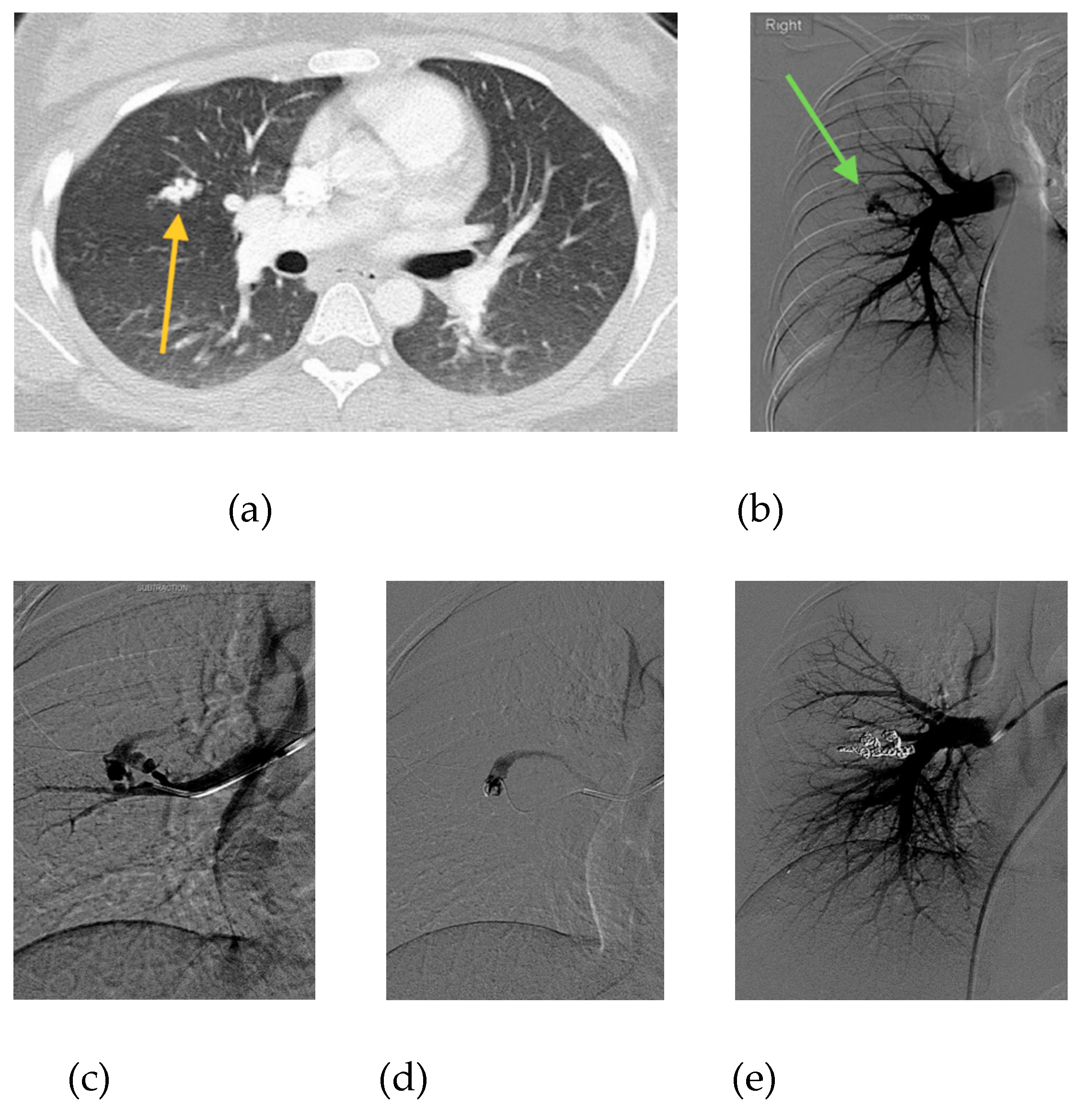
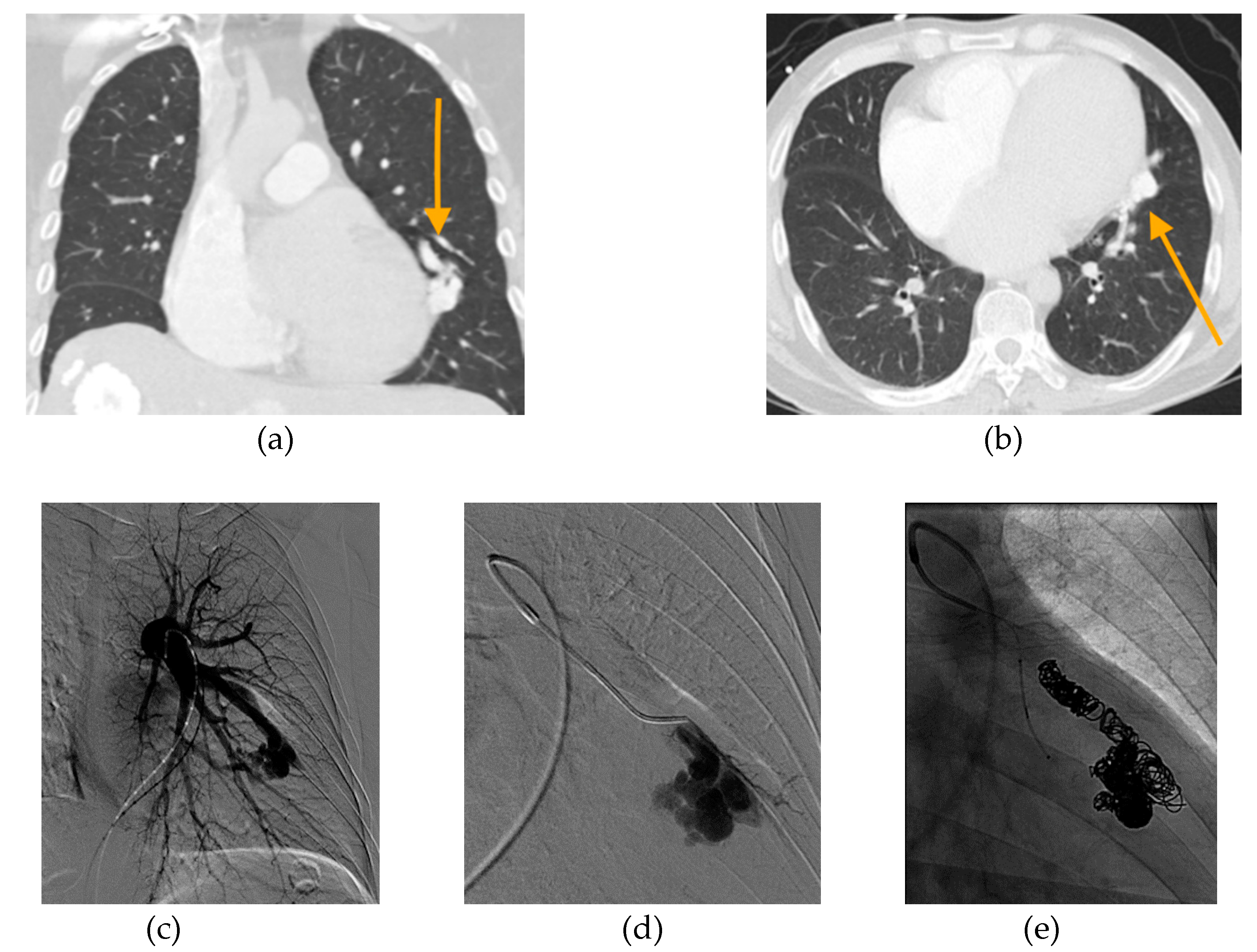
5. Embolic Devices
6. Follow-Up
7. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Shovlin, C.L.; Condliffe, R.; Donaldson, J.W.; Kiely, D.G.; Wort, S.J. British Thoracic Society clinical statement on pulmonary arteriovenous malformations. Thorax 2017, 72, 1154–1163. [Google Scholar] [CrossRef] [PubMed]
- Saboo, S.S.; Chamarthy, M.; Bhalla, S.; Park, H.; Sutphin, P.; Kay, F.; Battaile, J.; Kalva, S.P. Pulmonary arteriovenous malformations: Diagnosis. Cardiovasc. Diagn. Ther. 2018, 8, 325. [Google Scholar] [CrossRef]
- Contegiacomo, A.; del Ciello, A.; Rella, R.; Attempati, N.; Coppolino, D.; Larici, A.R.; Di Stasi, C.; Marano, G.; Manfredi, R. Pulmonary arteriovenous malformations: What the interventional radiologist needs to know. Radiol. Med. 2019, 124, 973–988. [Google Scholar] [CrossRef]
- Tellapuri, S.; Park, H.S.; Kalva, S.P. Pulmonary arteriovenous malformations. Int. J. Cardiovasc. Imaging 2019, 64, 1–8. [Google Scholar] [CrossRef] [PubMed]
- White, J.R.; Pollak, J.S.; Wirth, J.A. Pulmonary arteriovenous malformations: Diagnosis and transcatheter embolotherapy. J. Vasc. Interv. Radiol. 1996, 7, 787–804. [Google Scholar] [CrossRef]
- Wong, H.; Chan, R.; Klatt, R.; Faughnan, M. Idiopathic pulmonary arteriovenous malformations: Clinical and imaging characteristics. Eur. Respir. J. 2011, 38, 368–375. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Llorente, L.; Gallardo-Vara, E.; Rossi, E.; Smadja, D.M.; Botella, L.M.; Bernabeu, C. Endoglin and alk1 as therapeutic targets for hereditary hemorrhagic telangiectasia. Expert Opin. Ther. Targets 2017, 21, 933–947. [Google Scholar] [CrossRef] [PubMed]
- Dupuis-Girod, S.; Cottin, V.; Shovlin, C.L. The lung in hereditary hemorrhagic telangiectasia. Respiration 2017, 94, 315–330. [Google Scholar] [CrossRef]
- Mu, W.; Cordner, Z.A.; Yuqi Wang, K.; Reed, K.; Robinson, G.; Mitchell, S.; Lin, D. Characterization of pulmonary arteriovenous malformations in ACVRL1 versus ENG mutation carriers in hereditary hemorrhagic telangiectasia. Genet. Med. 2018, 20, 639–644. [Google Scholar] [CrossRef] [PubMed]
- Circo, S.; Gossage, J.R. Pulmonary vascular complications of hereditary haemorrhagic telangiectasia. Curr. Opin. Pulm. Med. 2014, 20, 421–428. [Google Scholar] [CrossRef]
- Salibe-Filho, W.; Piloto, B.M.; Oliveira, E.P.; Castro, M.A.; Affonso, B.B.; Motta-Leal-Filho, J.M.D.; Bortolini, E.; Terra-Filho, M. Pulmonary arteriovenous malformations: Diagnostic and treatment characteristics. J. Bras. Pneumol. 2019, 45, e20180137. [Google Scholar] [CrossRef]
- Alicea-Guevara, R.; Cruz Caliz, M.; Adorno, J.; Fernandez, R.; Rivera, K.; Gonzalez, G.; Hernandez-Castillo, R.A.; Fernandez, R.; Castillo Latorre, C. Life-threatening hemoptysis: Case of Osler–Weber–Rendu Syndrome. Oxf. Med. Case Rep. 2018, 2018, omx108. [Google Scholar] [CrossRef] [PubMed]
- Meier, N.M.; Foster, M.L.; Battaile, J.T. Hereditary hemorrhagic telangiectasia and pulmonary arteriovenous malformations: Clinical aspects. Cardiovasc. Diagn. Ther. 2018, 8, 316–324. [Google Scholar] [CrossRef] [PubMed]
- Kjeldsen, A.D.; Tørring, P.M.; Nissen, H.; Andersen, P.E. Cerebral abscesses among Danish patients with hereditary haemorrhagic telangiectasia. Acta Neurol. Scand. 2014, 129, 192–197. [Google Scholar] [CrossRef]
- Etievant, J.; Si-Mohamed, S.; Vinurel, N.; Dupuis-Girod, S.; Decullier, E.; Gamondes, D.; Khouatra, C.; Cottin, V.; Revel, D. Pulmonary arteriovenous malformations in hereditary haemorrhagic telangiectasia: Correlations between computed tomography findings and cerebral complications. Eur. Radiol. 2018, 28, 1338–1344. [Google Scholar] [CrossRef]
- Muller-Hulsbeck, S.; Marques, L.; Maleux, G.; Osuga, K.; Pelage, J.P.; Wohlgemuth, W.A.; Andersen, P.E. CIRSE standards of practice on diagnosis and treatment of pulmonary arteriovenous malformations. Cardiovasc. Interv. Radiol. 2020, 43, 353–361. [Google Scholar] [CrossRef]
- Gossage, J.R.; Kanj, G. Pulmonary arteriovenous malformations: A state of the art review. Am. J. Respir. Crit. Care Med. 1998, 158, 643–661. [Google Scholar] [CrossRef]
- Faughnan, M.; Palda, V.; Garcia-Tsao, G.; Geisthoff, U.; McDonald, J.; Proctor, D.; Spears, J.; Brown, D.; Buscarini, E.; Chesnutt, M. International guidelines for the diagnosis and management of hereditary haemorrhagic telangiectasia. J. Med. Genet. 2011, 48, 73–87. [Google Scholar] [CrossRef] [PubMed]
- Gossage, J.R. Role of contrast echocardiography in screening for pulmonary arteriovenous malformation in patients with hereditary hemorrhagic telangiectasia. Chest 2010, 138, 769–771. [Google Scholar] [CrossRef]
- Vorselaars, V.M.M.; Velthuis, S.; Huitema, M.P.; Hosman, A.E.; Westermann, C.J.J.; Snijder, R.J.; Mager, J.J.; Post, M.C. Reproducibility of right-to-left shunt quantification using transthoracic contrast echocardiography in hereditary haemorrhagic telangiectasia. Neth. Heart J. 2018, 26, 203–209. [Google Scholar] [CrossRef] [PubMed]
- Chick, J.F.B.; Reddy, S.N.; Pyeritz, R.E.; Trerotola, S.O. A survey of pulmonary arteriovenous malformation screening, management, and follow-up in hereditary hemorrhagic telangiectasia centers of excellence. Cardiovasc. Interv. Radiol. 2017, 40, 1003–1009. [Google Scholar] [CrossRef] [PubMed]
- Velthuis, S.; Buscarini, E.; Van Gent, M.W.; Gazzaniga, P.; Manfredi, G.; Danesino, C.; Schonewille, W.J.; Westermann, C.J.; Snijder, R.J.; Mager, J.J. Grade of pulmonary right-to-left shunt on contrast echocardiography and cerebral complications: A striking association. Chest 2013, 144, 542–548. [Google Scholar] [CrossRef] [PubMed]
- Velthuis, S.; Buscarini, E.; Mager, J.J.; Vorselaars, V.M.; Van Gent, M.W.; Gazzaniga, P.; Manfredi, G.; Danesino, C.; Diederik, A.L.; Vos, J.A. Predicting the size of pulmonary arteriovenous malformations on chest computed tomography: A role for transthoracic contrast echocardiography. Eur. Respir. J. 2014, 44, 150–159. [Google Scholar] [CrossRef]
- Zukotynski, K.; Chan, R.P.; Chow, C.-M.; Cohen, J.H.; Faughnan, M.E. Contrast echocardiography grading predicts pulmonary arteriovenous malformations on CT. Chest 2007, 132, 18–23. [Google Scholar] [CrossRef]
- Parra, J.A.; Bueno, J.; Zarauza, J.; Fariñas-Alvarez, C.; Cuesta, J.M.; Ortiz, P.; Zarrabeitia, R.; del Molino, A.P.; Bustamante, M.; Botella, L.M. Graded contrast echocardiography in pulmonary arteriovenous malformations. Eur. Respir. J. 2010, 35, 1279–1285. [Google Scholar] [CrossRef]
- Van Gent, M.W.F.; Post, M.C.; Snijder, R.J.; Westermann, C.J.J.; Plokker, H.W.M.; Mager, J.J. Real prevalence of pulmonary right-to-left shunt according to genotype in patients with hereditary hemorrhagic telangiectasia: A transthoracic contrast echocardiography study. Chest 2010, 138, 833–839. [Google Scholar] [CrossRef]
- Fernandopulle, N.; Mertens, L.; Klingel, M.; Manson, D.; Ratjen, F. Echocardiography grading for pulmonary arteriovenous malformation screening in children with hereditary hemorrhagic telangiectasia. J. Pediatr. 2018, 195, 288–291. [Google Scholar] [CrossRef] [PubMed]
- Parra, J.A.; Cuesta, J.M.; Zarrabeitia, R.; Fariñas-Álvarez, C.; Bueno, J.; Marqués, S.; Parra-Fariñas, C.; Botella, M.L.; Bernabéu, C.; Zarauza, J. Screening pulmonary arteriovenous malformations in a large cohort of Spanish patients with hemorrhagic hereditary telangiectasia. Int. J. Cardiol. 2016, 218, 240–245. [Google Scholar] [CrossRef]
- Van Gent, M.W.; Post, M.C.; Snijder, R.J.; Swaans, M.J.; Plokker, H.W.; Westermann, C.J.; Overtoom, T.T.; Mager, J.J. Grading of pulmonary right-to-left shunt with transthoracic contrast echocardiography: Does it predict the indication for embolotherapy? Chest 2009, 135, 1288–1292. [Google Scholar] [CrossRef]
- Karam, C.; Sellier, J.; Mansencal, N.; Fagnou, C.; Blivet, S.; Chinet, T.; Lacombe, P.; Dubourg, O. Reliability of contrast echocardiography to rule out pulmonary arteriovenous malformations and avoid CT irradiation in pediatric patients with hereditary hemorrhagic telangiectasia. Echocardiography 2015, 32, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Velthuis, S.; Buscarini, E.; Gossage, J.R.; Snijder, R.J.; Mager, J.J.; Post, M.C. Clinical implications of pulmonary shunting on saline contrast echocardiography. J. Am. Soc. Echocardiogr. 2015, 28, 255–263. [Google Scholar] [CrossRef]
- Moussouttas, M.; Fayad, P.; Rosenblatt, M.; Hashimoto, M.; Pollak, J.; Henderson, K.; Ma, T.-Z.; White, R. Pulmonary arteriovenous malformations: Cerebral ischemia and neurologic manifestations. Neurology 2000, 55, 959–964. [Google Scholar] [CrossRef]
- Todo, K.; Moriwaki, H.; Higashi, M.; Kimura, K.; Naritomi, H. A small pulmonary arteriovenous malformation as a cause of recurrent brain embolism. Am. J. Neuroradiol. 2004, 25, 428–430. [Google Scholar] [PubMed]
- Mager, J.J.; Overtoom, T.T.; Blauw, H.; Lammers, J.W.; Westermann, C.J. Embolotherapy of pulmonary arteriovenous malformations: Long-term results in 112 patients. J. Vasc. Interv. Radiol. 2004, 15, 451–456. [Google Scholar] [CrossRef] [PubMed]
- Pollak, J.S.; Saluja, S.; Thabet, A.; Henderson, K.J.; Denbow, N.; White, R.I., Jr. Clinical and anatomic outcomes after embolotherapy of pulmonary arteriovenous malformations. J. Vasc. Interv. Radiol. 2006, 17, 35–45. [Google Scholar] [CrossRef]
- Shovlin, C.L.; Jackson, J.E.; Bamford, K.B.; Jenkins, I.H.; Benjamin, A.R.; Ramadan, H.; Kulinskaya, E. Primary determinants of ischaemic stroke/brain abscess risks are independent of severity of pulmonary arteriovenous malformations in hereditary haemorrhagic telangiectasia. Thorax 2008, 63, 259–266. [Google Scholar] [CrossRef] [PubMed]
- Al-Saleh, S.; Dragulescu, A.; Manson, D.; Golding, F.; Traubici, J.; Mei-Zahav, M.; MacLusky, I.B.; Faughnan, M.E.; Carpenter, S.; Ratjen, F. Utility of contrast echocardiography for pulmonary arteriovenous malformation screening in pediatric hereditary hemorrhagic telangiectasia. J. Pediatr. 2012, 160, 1039–1043. [Google Scholar] [CrossRef] [PubMed]
- Mowers, K.L.; Sekarski, L.; White, A.J.; Grady, R.M. Pulmonary arteriovenous malformations in children with hereditary hemorrhagic telangiectasia: A longitudinal study. Pulm. Circ. 2018, 8. [Google Scholar] [CrossRef]
- Hosman, A.E.; de Gussem, E.M.; Balemans, W.A.; Gauthier, A.; Westermann, C.J.; Snijder, R.J.; Post, M.C.; Mager, J.J. Screening children for pulmonary arteriovenous malformations: Evaluation of 18 years of experience. Pediatr. Pulmonol. 2017, 52, 1206–1211. [Google Scholar] [CrossRef]
- Ratjen, A.; Au, J.; Bscn, S.C.; John, P.; Ratjen, F. Growth of pulmonary arteriovenous malformations in pediatric patients with hereditary hemorrhagic telangiectasia. J. Pediatr. 2019. [Google Scholar] [CrossRef]
- Faughnan, M.E.; Thabet, A.; Mei-Zahav, M.; Colombo, M.; MacLusky, I.; Hyland, R.H.; Pugash, R.A.; Chait, P.; Henderson, K.J.; White, R.I., Jr. Pulmonary arteriovenous malformations in children: Outcomes of transcatheter embolotherapy. J. Pediatr. 2004, 145, 826–831. [Google Scholar] [CrossRef] [PubMed]
- Giordano, P.; Lenato, G.M.; Suppressa, P.; Lastella, P.; Dicuonzo, F.; Chiumarulo, L.; Sangerardi, M.; Piccarreta, P.; Valerio, R.; Scardapane, A. Hereditary hemorrhagic telangiectasia: Arteriovenous malformations in children. J. Pediatr. 2013, 163, 179–186. [Google Scholar] [CrossRef]
- Ibrahim, S.M.; Henderson, K.J.; Rashid, S.; Hussein, S.M.; White, R.I., Jr.; Pollak, J.S. Correlation of oxygen saturation and serious adverse events in pediatric patients with documented or suspected pulmonary arteriovenous malformation. Angiogenesis 2015, 18, 537–538. [Google Scholar]
- Gershon, A.S.; Faughnan, M.E.; Chon, K.S.; Pugash, R.A.; Clark, J.A.; Bohan, M.J.; Henderson, K.J.; Hyland, R.H.; White, R.I., Jr. Transcatheter embolotherapy of maternal pulmonary arteriovenous malformations during pregnancy. Chest 2001, 119, 470–477. [Google Scholar] [CrossRef] [PubMed]
- Moore, B. Pulmonary arterio-venous fistula. Thorax 1969, 24, 381. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ference, B.A.; Shannon, T.M.; White, R.I., Jr.; Zawin, M.; Burdge, C.M. Life-threatening pulmonary hemorrhage with pulmonary arteriovenous malformations and hereditary hemorrhagic telangiectasia. Chest 1994, 106, 1387–1390. [Google Scholar] [CrossRef]
- Swinburne, A.; Fedullo, A.; Gangemi, R.; Mijangos, J. Hereditary telangiectasia and multiple pulmonary arteriovenous fistulas: Clinical deterioration during pregnancy. Chest 1986, 89, 459–460. [Google Scholar] [CrossRef]
- Gammon, R.B.; Miksa, A.K.; Keller, F.S. Osler-Weber-Rendu disease and pulmonary arteriovenous fistulas: Deterioration and embolotherapy during pregnancy. Chest 1990, 98, 1522–1524. [Google Scholar] [CrossRef]
- Laroche, C.M.; Wells, F.; Shneerson, J. Massive hemothorax due to enlarging arteriovenous fistula in pregnancy. Chest 1992, 101, 1452–1454. [Google Scholar] [CrossRef]
- Chanatry, B.J. Acute hemothorax owing to pulmonary arteriovenous malformation in pregnancy. Anesth. Analg. 1992, 74, 613–615. [Google Scholar] [CrossRef]
- Dupuis, O.; Delagrange, L.; Dupuis-Girod, S. Hereditary haemorrhagic telangiectasia and pregnancy: A review of the literature. Orphanet J. Rare Dis. 2020, 15, 5. [Google Scholar] [CrossRef] [PubMed]
- Shovlin, C.; Sodhi, V.; McCarthy, A.; Lasjaunias, P.; Jackson, J.; Sheppard, M. Estimates of maternal risks of pregnancy for women with hereditary haemorrhagic telangiectasia (Osler–Weber–Rendu syndrome): Suggested approach for obstetric services. BJOG Int. J. Obstet. Gynaecol. 2008, 115, 1108–1115. [Google Scholar] [CrossRef] [PubMed]
- Shovlin, C.; Winstock, A.; Peters, A.; Jackson, J.; Hughes, J. Medical complications of pregnancy in hereditary haemorrhagic telangiectasia. Qjm Int. J. Med. 1995, 88, 879–887. [Google Scholar]
- De Gussem, E.M.; Lausman, A.Y.; Beder, A.J.; Edwards, C.P.; Blanker, M.H.; Terbrugge, K.G.; Mager, J.J.; Faughnan, M.E. Outcomes of pregnancy in women with hereditary hemorrhagic telangiectasia. Obstet. Gynecol. 2014, 123, 514–520. [Google Scholar] [CrossRef] [PubMed]
- Dauer, L.T.; Thornton, R.H.; Miller, D.L.; Damilakis, J.; Dixon, R.G.; Marx, M.V.; Schueler, B.A.; Vañó, E.; Venkatesan, A.M.; Bartal, G. Radiation management for interventions using fluoroscopic or computed tomographic guidance during pregnancy: A joint guideline of the Society of Interventional Radiology and the Cardiovascular and Interventional Radiological Society of Europe with Endorsement by the Canadian Interventional Radiology Association. J. Vasc. Interv. Radiol. 2012, 23, 19–32. [Google Scholar] [CrossRef] [PubMed]
- Puac, P.; Rodríguez, A.; Vallejo, C.; Zamora, C.A.; Castillo, M. Safety of contrast material use during pregnancy and lactation. Magn. Reson. Imaging Clin. N. Am. 2017, 25, 787–797. [Google Scholar] [CrossRef] [PubMed]
- Woodward, C.S.; Pyeritz, R.E.; Chittams, J.L.; Trerotola, S.O. Treated pulmonary arteriovenous malformations: Patterns of persistence and associated retreatment success. Radiology 2013, 269, 919–926. [Google Scholar] [CrossRef] [PubMed]
- Remy-Jardin, M.; Dumont, P.; Brillet, P.-Y.; Dupuis, P.; Duhamel, A.; Remy, J. Pulmonary arteriovenous malformations treated with embolotherapy: Helical CT evaluation of long-term effectiveness after 2–21-year follow-up. Radiology 2006, 239, 576–585. [Google Scholar] [CrossRef] [PubMed]
- Chan, R.P.; Faughnan, M.; White, R. Pulmonary arteriovenous malformations treated with embolotherapy. Radiology 2007, 244, 932. [Google Scholar] [CrossRef]
- Shimohira, M.; Kawai, T.; Hashizume, T.; Ohta, K.; Suzuki, K.; Shibamoto, Y. Pulmonary arteriovenous malformations: Current technique of transcatheter embolization and subsequent management. Interv. Radiol. 2017, 2, 116–121. [Google Scholar] [CrossRef][Green Version]
- Trerotola, S.O.; Pyeritz, R.E. Does use of coils in addition to amplatzer vascular plugs prevent recanalization? Am. J. Roentgenol. 2010, 195, 766–771. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.W.; White, R.I.; Egglin, T.K.; Pollak, J.S.; Fayad, P.B.; Wirth, J.A.; Rosenblatt, M.M.; Dickey, K.W.; Burdge, C.M. Embolotherapy of large pulmonary arteriovenous malformations: Long-term results. Ann. Thorac. Surg. 1997, 64, 930–940. [Google Scholar] [CrossRef]
- Milic, A.; Chan, R.P.; Cohen, J.H.; Faughnan, M.E. Reperfusion of pulmonary arteriovenous malformations after embolotherapy. J. Vasc. Interv. Radiol. 2005, 16, 1675–1683. [Google Scholar] [CrossRef] [PubMed]
- Shimohira, M.; Kawai, T.; Hashizume, T.; Ohta, K.; Nakagawa, M.; Ozawa, Y.; Sakurai, K.; Shibamoto, Y. Reperfusion rates of pulmonary arteriovenous malformations after coil embolization: Evaluation with time-resolved MR angiography or pulmonary angiography. J. Vasc. Interv. Radiol. 2015, 26, 856–864. [Google Scholar] [CrossRef]
- Cusumano, L.R.; Duckwiler, G.R.; Roberts, D.G.; McWilliams, J.P. Treatment of recurrent pulmonary arteriovenous malformations: Comparison of proximal versus distal embolization technique. Cardiovasc. Interv. Radiol. 2020, 43, 29–36. [Google Scholar] [CrossRef]
- Hayashi, S.; Baba, Y.; Senokuchi, T.; Nakajo, M. Efficacy of venous sac embolization for pulmonary arteriovenous malformations: Comparison with feeding artery embolization. J. Vasc. Interv. Radiol. 2012, 23, 1566–1577. [Google Scholar] [CrossRef] [PubMed]
- Kajiwara, K.; Urashima, M.; Yamagami, T.; Kakizawa, H.; Matsuura, N.; Matsuura, A.; Ohnari, T.; Ishikawa, M.; Awai, K. Venous sac embolization of pulmonary arteriovenous malformation: Safety and effectiveness at mid-term follow-up. Acta Radiol. 2014, 55, 1093–1098. [Google Scholar] [CrossRef]
- Dinkel, H.P.; Triller, J. Pulmonary arteriovenous malformations: Embolotherapy with superselective coaxial catheter placement and filling of venous sac with Guglielmi detachable coils. Radiology 2002, 223, 709–714. [Google Scholar] [CrossRef] [PubMed]
- Haddad, M.M.; Bendel, E.C.; Harmsen, W.S.; Iyer, V.N.; Misra, S. Smoking significantly impacts persistence rates in embolized pulmonary arteriovenous malformations in patients with hereditary hemorrhagic telangiectasia. Radiology 2019, 292, 762–770. [Google Scholar] [CrossRef]
- Faughnan, M.E.; Lui, Y.W.; Wirth, J.A.; Pugash, R.A.; Redelmeier, D.A.; Hyland, R.H.; White, R.I., Jr. Diffuse pulmonary arteriovenous malformations: Characteristics and prognosis. Chest 2000, 117, 31–38. [Google Scholar] [CrossRef]
- Pierucci, P.; Murphy, J.; Henderson, K.J.; Chyun, D.A.; White, R.I., Jr. New definition and natural history of patients with diffuse pulmonary arteriovenous malformations: Twenty-seven–year experience. Chest 2008, 133, 653–661. [Google Scholar] [CrossRef] [PubMed]
- Lacombe, P.; Lagrange, C.; Beauchet, A.; El Hajjam, M.; Chinet, T.; Pelage, J.-P. Diffuse pulmonary arteriovenous malformations in hereditary hemorrhagic telangiectasia: Long-term results of embolization according to the extent of lung involvement. Chest 2009, 135, 1031–1037. [Google Scholar] [CrossRef] [PubMed]
- Fukushima, H.; Mitsuhashi, T.; Oto, T.; Sano, Y.; Kusano, K.F.; Goto, K.; Okazaki, M.; Date, H.; Kojima, Y.; Yamagishi, H.; et al. Successful lung transplantation in a case with diffuse pulmonary arteriovenous malformations and hereditary hemorrhagic telangiectasia. Am. J. Transpl. 2013, 13, 3278–3281. [Google Scholar] [CrossRef] [PubMed]
- Svetliza, G.; De la Canal, A.; Beveraggi, E.; Giacoia, A.; Ruiz, C.; Caruso, E.; Rodríguez Giménez, J.; Vassallo, B. Lung transplantation in a patient with arteriovenous malformations. J. Heart Lung Transplant. 2002, 21, 506–508. [Google Scholar] [CrossRef]
- Reynaud-Gaubert, M.; Thomas, P.; Gaubert, J.; Pietri, P.; Garbe, L.; Giudicelli, R.; Orehek, J.; Fuentes, P. Pulmonary arteriovenous malformations: Lung transplantation as a therapeutic option. Eur. Respir. J. 1999, 14, 1425–1428. [Google Scholar] [CrossRef]
- Chambers, D.C.; Yusen, R.D.; Cherikh, W.S.; Goldfarb, S.B.; Kucheryavaya, A.Y.; Khusch, K.; Levvey, B.J.; Lund, L.H.; Meiser, B.; Rossano, J.W.; et al. The registry of the international society for heart and lung transplantation: Thirty-fourth adult lung and heart-lung transplantation report—2017; focus theme: Allograft ischemic time. J. Heart Lung Transplant. 2017, 36, 1047–1059. [Google Scholar] [CrossRef] [PubMed]
- Shovlin, C.L.; Buscarini, E.; Hughes, J.M.B.; Allison, D.J.; Jackson, J.E. Long-term outcomes of patients with pulmonary arteriovenous malformations considered for lung transplantation, compared with similarly hypoxaemic cohorts. BMJ Open Respir. Res. 2017, 4, e000198. [Google Scholar] [CrossRef]
- Simonneau, G.; Montani, D.; Celermajer, D.S.; Denton, C.P.; Gatzoulis, M.A.; Krowka, M.; Williams, P.G.; Souza, R. Haemodynamic definitions and updated clinical classification of pulmonary hypertension. Eur. Respir. J. 2019, 53, 1801913. [Google Scholar] [CrossRef]
- Olivieri, C.; Lanzarini, L.; Pagella, F.; Semino, L.; Corno, S.; Valacca, C.; Plauchu, H.; Lesca, G.; Barthelet, M.; Buscarini, E. Echocardiographic screening discloses increased values of pulmonary artery systolic pressure in 9 of 68 unselected patients affected with hereditary hemorrhagic telangiectasia. Genet. Med. 2006, 8, 183–190. [Google Scholar] [CrossRef]
- Revuz, S.; Decullier, E.; Ginon, I.; Lamblin, N.; Hatron, P.Y.; Kaminsky, P.; Carette, M.F.; Lacombe, P.; Simon, A.C.; Rivière, S.; et al. Pulmonary hypertension subtypes associated with hereditary haemorrhagic telangiectasia: Haemodynamic profiles and survival probability. PLoS ONE 2017, 12, e0184227. [Google Scholar] [CrossRef]
- Chizinga, M.; Rudkovskaia, A.A.; Henderson, K.; Pollak, J.; Garcia-Tsao, G.; Young, L.H.; Fares, W.H. Pulmonary hypertension prevalence and prognosis in a cohort of patients with hereditary hemorrhagic telangiectasia undergoing embolization of pulmonary arteriovenous malformations. Am. J. Respir. Crit. Care Med. 2017, 196, 1353–1356. [Google Scholar] [CrossRef]
- De Picciotto, C.; El Hajjam, M.; Karam, C.; Chinet, T.; Bonay, M. Pulmonary gas exchange in hereditary hemorrhagic telangiectasia patients with liver arteriovenous malformations. Respir. Res. 2019, 20, 137. [Google Scholar] [CrossRef] [PubMed]
- Trembath, R.C.; Thomson, J.R.; Machado, R.D.; Morgan, N.V.; Atkinson, C.; Winship, I.; Simonneau, G.; Galie, N.; Loyd, J.E.; Humbert, M. Clinical and molecular genetic features of pulmonary hypertension in patients with hereditary hemorrhagic telangiectasia. N. Engl. J. Med. 2001, 345, 325–334. [Google Scholar] [CrossRef]
- Cottin, V.; Dupuis-Girod, S.; Lesca, G.; Cordier, J.F. Pulmonary vascular manifestations of hereditary hemorrhagic telangiectasia (rendu-osler disease). Respiration 2007, 74, 361–378. [Google Scholar] [CrossRef] [PubMed]
- Sopeña, B.; Pérez-Rodríguez, M.T.; Portela, D.; Rivera, A.; Freire, M.; Martínez-Vázquez, C. High prevalence of pulmonary hypertension in patients with hereditary hemorrhagic telangiectasia. Eur. J. Intern. Med. 2013, 24, e30–e34. [Google Scholar] [CrossRef] [PubMed]
- Yokokawa, T.; Sugimoto, K.; Kimishima, Y.; Misaka, T.; Yoshihisa, A.; Morisaki, H.; Yamada, O.; Nakazato, K.; Ishida, T.; Takeishi, Y. A case of pulmonary hypertension and hereditary hemorrhagic telangiectasia related to an ACVRL1 mutation. Intern. Med. 2020. [Google Scholar] [CrossRef] [PubMed]
- Andrivet, P.; Lofaso, F.; Carette, M.; Allegrini, J.; Adnot, S. Haemodynamics and gas exchange before and after coil embolization of pulmonary arteriovenous malformations. Eur. Respir. J. 1995, 8, 1228–1230. [Google Scholar] [CrossRef]
- Shovlin, C.; Tighe, H.; Davies, R.; Gibbs, J.; Jackson, J. Embolisation of pulmonary arteriovenous malformations: No consistent effect on pulmonary artery pressure. Eur. Respir. J. 2008, 32, 162–169. [Google Scholar] [CrossRef]
- Vorselaars, V.M.M.; Velthuis, S.; Mager, J.J.; Snijder, R.J.; Bos, W.J.; Vos, J.A.; van Strijen, M.J.L.; Post, M.C. Direct haemodynamic effects of pulmonary arteriovenous malformation embolisation. Neth. Heart J. 2014, 22, 328–333. [Google Scholar] [CrossRef]
- Haitjerm, T.; Jurrien, M.; Overtoom, T.T.C.; Ernst, J.M.; Westermann, C.J. Unusual complications after embolization of a pulmonary arteriovenous malformation. Chest 1996, 109, 1401–1404. [Google Scholar] [CrossRef]
- Montani, D.; Price, L.; Girerd, B.; Chinet, T.; Lacombe, P.; Simonneau, G.; Humbert, M. Fatal rupture of pulmonary arteriovenous malformation in hereditary haemorrhagic telangiectasis and severe PAH. Eur. Respir. Rev. 2009, 18, 42–46. [Google Scholar] [CrossRef] [PubMed]
- Vaidya, S.; Tozer, K.R.; Chen, J. An overview of embolic agents. Semin. Interv. Radiol. 2008, 25, 204–215. [Google Scholar] [CrossRef] [PubMed]
- Prasad, V.; Chan, R.P.; Faughnan, M.E. Embolotherapy of pulmonary arteriovenous malformations: Efficacy of platinum versus stainless steel coils. J. Vasc. Interv. Radiol. 2004, 15, 153–160. [Google Scholar] [CrossRef] [PubMed]
- Kennedy, S.A.; Faughnan, M.E.; Vozoris, N.T.; Prabhudesai, V. Reperfusion of pulmonary arteriovenous malformations following embolotherapy: A randomized controlled trial of detachable versus pushable coils. Cardiovasc. Interv. Radiol. 2020. [Google Scholar] [CrossRef]
- Stein, E.J.; Chittams, J.L.; Miller, M.; Trerotola, S.O. Persistence in coil-embolized pulmonary arteriovenous malformations with feeding artery diameters of 3 mm or less: A retrospective single-center observational study. J. Vasc. Interv. Radiol. 2017, 28, 442–449. [Google Scholar] [CrossRef]
- Alsafi, A.; Jackson, J.E.; Fatania, G.; Patel, M.C.; Glover, A.; Shovlin, C.L. Patients with in-situ metallic coils and Amplatzer vascular plugs used to treat pulmonary arteriovenous malformations since 1984 can safely undergo magnetic resonance imaging. Br. J. Radiol. 2019, 92, 20180752. [Google Scholar] [CrossRef]
- Corvino, F.; Silvestre, M.; Cervo, A.; Giurazza, F.; Corvino, A.; Maglione, F. Endovascular occlusion of pulmonary arteriovenous malformations with the ArtVentive Endoluminal Occlusion System™. Diagn. Interv. Radiol. 2016, 22, 463. [Google Scholar] [CrossRef]
- Lee, S.Y.; Lee, J.; Kim, Y.H.; Kang, U.R.; Cha, J.G.; Lee, J.; Cha, S.I.; Kim, C.H. Efficacy and safety of AMPLATZER vascular plug type IV for embolization of pulmonary arteriovenous malformations. J. Vasc. Interv. Radiol. 2019, 30, 1082–1088. [Google Scholar] [CrossRef]
- Adachi, A.; Ohta, K.; Jahangiri, Y.; Matsui, Y.; Horikawa, M.; Geeratikun, Y.; Chansanti, O.; Yata, S.; Fujii, S.; Steinberger, J.; et al. Treatment of pulmonary arteriovenous malformations: Clinical experience using different embolization strategies. Jpn. J. Radiol. 2020, 38, 382–386. [Google Scholar] [CrossRef]
- Tapping, C.R.; Ettles, D.F.; Robinson, G.J. Long-term follow-up of treatment of pulmonary arteriovenous malformations with AMPLATZER Vascular Plug and AMPLATZER Vascular Plug II devices. J. Vasc. Interv. Radiol. 2011, 22, 1740–1746. [Google Scholar] [CrossRef] [PubMed]
- Letourneau-Guillon, L.; Faughnan, M.E.; Soulez, G.; Giroux, M.F.; Oliva, V.L.; Boucher, L.M.; Dubois, J.; Prabhudesai, V.; Therasse, E. Embolization of pulmonary arteriovenous malformations with amplatzer vascular plugs: Safety and midterm effectiveness. J. Vasc. Interv. Radiol. 2010, 21, 649–656. [Google Scholar] [CrossRef] [PubMed]
- Kucukay, F.; Özdemir, M.; Şenol, E.; Okten, S.; Ereren, M.; Karan, A. Large pulmonary arteriovenous malformations: Long-term results of embolization with AMPLATZER vascular plugs. J. Vasc. Interv. Radiol. 2014, 25, 1327–1332. [Google Scholar] [CrossRef]
- Andersen, P.E.; Duvnjak, S.; Gerke, O.; Kjeldsen, A.D. Long-term single-center retrospective follow-up after embolization of pulmonary arteriovenous malformations treated over a 20-year period: Frequency of re-canalization with various embolization materials and clinical outcome. Cardiovasc. Interv. Radiol. 2019, 42, 1102–1109. [Google Scholar] [CrossRef] [PubMed]
- Tau, N.; Atar, E.; Mei-Zahav, M.; Bachar, G.N.; Dagan, T.; Birk, E.; Bruckheimer, E. Amplatzer vascular plugs versus coils for embolization of pulmonary arteriovenous malformations in patients with hereditary hemorrhagic telangiectasia. Cardiovasc. Interv. Radiol. 2016, 39, 1110–1114. [Google Scholar] [CrossRef]
- Hundt, W.; Kalinowski, M.; Kiessling, A.; Heverhagen, J.T.; Eivazi, B.; Werner, J.; Steinbach, S.; Klose, K.J.; Burbelko, M. Novel approach to complex pulmonary arteriovenous malformation embolization using detachable coils and Amplatzer vascular plugs. Eur. J. Radiol. 2012, 81, e732–e738. [Google Scholar] [CrossRef] [PubMed]
- Conrad, M.B.; Ishaque, B.M.; Surman, A.M.; Kerlan, R.K., Jr.; Hope, M.D.; Dickey, M.A.; Hetts, S.W.; Wilson, M.W. Intraprocedural safety and technical success of the MVP micro vascular plug for embolization of pulmonary arteriovenous malformations. J. Vasc. Interv. Radiol. 2015, 26, 1735–1739. [Google Scholar] [CrossRef] [PubMed]
- Chamarthy, M.R.; Park, H.; Sutphin, P.; Kumar, G.; Lamus, D.; Saboo, S.; Anderson, M.; Kalva, S.P. Pulmonary arteriovenous malformations: Endovascular therapy. Cardiovasc. Diagn. Ther. 2018, 8, 338–349. [Google Scholar] [CrossRef]
- Mahdjoub, E.; Tavolaro, S.; Parrot, A.; Cornelis, F.; Khalil, A.; Carette, M.F. Pulmonary arteriovenous malformations: Safety and efficacy of microvascular plugs. Am. J. Roentgenol. 2018, 211, 1135–1143. [Google Scholar] [CrossRef]
- Ratnani, R.; Sutphin, P.D.; Koshti, V.; Park, H.; Chamarthy, M.; Battaile, J.; Kalva, S.P. Retrospective comparison of pulmonary arteriovenous malformation embolization with the polytetrafluoroethylene-covered nitinol microvascular plug, AMPLATZER plug, and coils in patients with hereditary hemorrhagic telangiectasia. J. Vasc. Interv. Radiol. 2019, 30, 1089–1097. [Google Scholar] [CrossRef]
- Bailey, C.R.; Arun, A.; Towsley, M.; Choi, W.K.; Betz, J.F.; MacKenzie, S.; Areda, M.A.; Duvvuri, M.; Mitchell, S.; Weiss, C.R. MVP micro vascular plug systems for the treatment of pulmonary arteriovenous malformations. Cardiovasc. Interv. Radiol. 2019, 42, 389–395. [Google Scholar] [CrossRef]
- Curnes, N.R.; Desjardins, B.; Pyeritz, R.; Chittams, J.; Sienko, D.; Trerotola, S.O. Lack of growth of small (≤2 mm feeding artery) untreated pulmonary arteriovenous malformations in patients with hereditary hemorrhagic telangiectasia. J. Vasc. Interv. Radiol. 2019, 30, 1259–1264. [Google Scholar] [CrossRef]
- Ryan, D.J.; O‘Connor, T.M.; Murphy, M.M.; Brady, A.P. Follow-up interval for small untreated pulmonary arteriovenous malformations in hereditary haemorrhagic telangiectasia. Clin. Radiol. 2017, 72, 236–241. [Google Scholar] [CrossRef]
- Brinjikji, W.; Latino, G.A.; Parvinian, A.; Gauthier, A.; Pantalone, R.; Yamaki, V.; Apala, D.R.; Prabhudesai, V.; Cyr, V.; Chartrand-Lefebvre, C.; et al. Diagnostic yield of rescreening adults for pulmonary arteriovenous malformations. J. Vasc. Interv. Radiol. 2019, 30, 1982–1987. [Google Scholar] [CrossRef] [PubMed]
- DePietro, D.M.; Curnes, N.R.; Chittams, J.; Ferrari, V.A.; Pyeritz, R.E.; Trerotola, S.O. Postembolotherapy pulmonary arteriovenous malformation follow-up: A role for graded transthoracic contrast echocardiography prior to high-resolution chest CT scan. Chest 2019. [Google Scholar] [CrossRef]
- Hamamoto, K.; Matsuura, K.; Chiba, E.; Okochi, T.; Tanno, K.; Tanaka, O. Feasibility of non-contrast-enhanced MR angiography using the time-SLIP technique for the assessment of pulmonary arteriovenous malformation. Magn. Reson. Med. Sci. 2016. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kawai, T.; Shimohira, M.; Kan, H.; Hashizume, T.; Ohta, K.; Kurosaka, K.; Muto, M.; Suzuki, K.; Shibamoto, Y. Feasibility of time-resolved MR angiography for detecting recanalization of pulmonary arteriovenous malformations treated with embolization with platinum coils. J. Vasc. Interv. Radiol. 2014, 25, 1339–1347. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.N.; Finn, J.P.; Bista, B.; Kee, S.; McWilliams, J.P. Comparison of ferumoxtyol MR angiography and CT angiography for the detection of pulmonary arterial venous malformations (AVMs) in hereditary hemorrhagic telangiectasia: Initial results. Radiol. Cardiothorac. Imaging 2020, 2. [Google Scholar] [CrossRef]

| Study | Total # PAVMs Embolized | # Persistent PAVMs Embolized | Mean PAVM Feeding Artery Diameter (mm, ±SD) * | Embolic Devices | Technical Success ** | Mean Follow-Up, Years | Persistence Rate at Follow-Up | Complications † |
|---|---|---|---|---|---|---|---|---|
| Letourneau-Guillon 2010 [101] | 35 | 0 | 5.0 (3.0–10.0) | AVP | 97% | 1.1 | 7% | Major: None Minor: Chest pain (4) |
| Trerotola 2010 [61] | 37 | 0 | Not reported (all ≥ 5 mm) | AVP + coils | 100% | 1.1 | 0% | Major: None Minor: Chest pain (7) |
| Tapping 2011 [100] | 19 | 2 | Not reported (3.0–12.0 mm) | AVP type I (8) AVP type II (11) | 100% | 2.3 (Type I) 1.5 (Type II) | 5% (Type I) 0% (Type II) | Major: None Minor: Chest pain (1) |
| Hundt 2012 [105] | 11 | 0 | 4.4 ± 1.4 | AVP + coils | 91% | Not specified | 12.5% | Major: None Minor: Chest pain (4) Hemoptysis (1) |
| Kucukay 2014 [102] | 24 | 0 | 11.5 ± 2.2 | AVP | 100% | 3.0 | 0% | Major: None Minor: Chest pain (5) |
| Shimohira 2015 [64] | 24 | 12 | 3.8 (1.4–5.2) | Coils | 100% | 2 (median) | 49% (primary embolization) 100% (repeat embolization) | Not reported |
| Conrad 2015 [106] | 20 | 0 | 3.5 (1.9–5.0) | MVP (19) MVP + coils (1) | 100% | 0.3 | 10% | Major: None Minor: Microemboli to toe (1) |
| Tau 2016 [104] | 63 | 0 | Not reported | Coils (37) AVP (21) AVP + coils (5) | 100% | 7.7 | 18.9% (coils) 0% (AVP) 0% (AVP + coils) | Major: None Minor: None |
| Stein 2017 [95] | 141 | 0 | 2.4 ± 1.1 | Coils | 100% | 1.6 | 21% | Major: None Minor: Chest pain (21) Groin infection (1) Hematoma (Not specified) Effusion (Not specified Flushing (Not specified) |
| Mahdjoub 2018 [108] | 39 | 6 | 2.3 ± 0.7 | MVP | 98% | 1.0 | 6% | Not reported |
| Andersen 2019 [103] | 322 | 30 | Not reported (all ≥ 2 mm) | Coils (213) AVP (89) Detachable balloon (13) AVP + coils (7) | 100% | 4.8 | 11.7% (Coils) 4.5% (AVP) 0% (Balloon) 14.3% (AVP + coils) | Not reported |
| Bailey 2019 [110] | 119 | 0 | 3.3 ± 1.2 | MVP | 100% | 0.9 | 0% | Major: None Minor: Chest pain (1) |
| Ratnani 2019 [109] | 157 | 0 | 2.3 (1.0–5.9, MVP) 2.8 (1.0–7.6, Other) | MVP (92) Coils (24) AVP (35) AVP + coils (6) | 100% (MVP) 100% (Coils) 97% (AVP) 100% (AVP + coils) | 1.4 (MVP) 3.3 (Other) | 2% (MVPs) 46.7% (Coils) 15% (AVP) 20% (AVP + coils) | Major: None Minor: Asymptomatic Pulmonary Infarcts (1) |
| Lee 2019 [98] | 19 | 0 | 3.1 ± 0.7 | AVP | 100% | 1.2 | 16% | Major: None Minor: Tachycardia (1) Chest pain (1) |
| Kennedy 2020 [94] | 46 | 0 | 4.3 ± 1.5 (Nester) 4.4 ± 1.4 (Interlock) | Nester coils (26) Interlock coils (20) | 100% | 1.2 | 0% (Nester) 5.6% (Interlock) | Major: None Minor: Chest pain (5) Migraine (3) Minor hemoptysis (1) |
| Adachi 2020 [99] | 88 | 0 | 4.1 ± 2.1 | Coils (50) AVP (20) AVP + coils (18) | 100% | 3.2 | 22% (Coils) 10% (AVP) 39% (AVP + coils) | Major: None Minor: Not reported |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Majumdar, S.; McWilliams, J.P. Approach to Pulmonary Arteriovenous Malformations: A Comprehensive Update. J. Clin. Med. 2020, 9, 1927. https://doi.org/10.3390/jcm9061927
Majumdar S, McWilliams JP. Approach to Pulmonary Arteriovenous Malformations: A Comprehensive Update. Journal of Clinical Medicine. 2020; 9(6):1927. https://doi.org/10.3390/jcm9061927
Chicago/Turabian StyleMajumdar, Shamaita, and Justin P. McWilliams. 2020. "Approach to Pulmonary Arteriovenous Malformations: A Comprehensive Update" Journal of Clinical Medicine 9, no. 6: 1927. https://doi.org/10.3390/jcm9061927
APA StyleMajumdar, S., & McWilliams, J. P. (2020). Approach to Pulmonary Arteriovenous Malformations: A Comprehensive Update. Journal of Clinical Medicine, 9(6), 1927. https://doi.org/10.3390/jcm9061927





