Association of Plasma Level of TNF-Related Apoptosis-Inducing Ligand with Severity and Outcome of Sepsis
Abstract
:1. Introduction
2. Materials and Methods
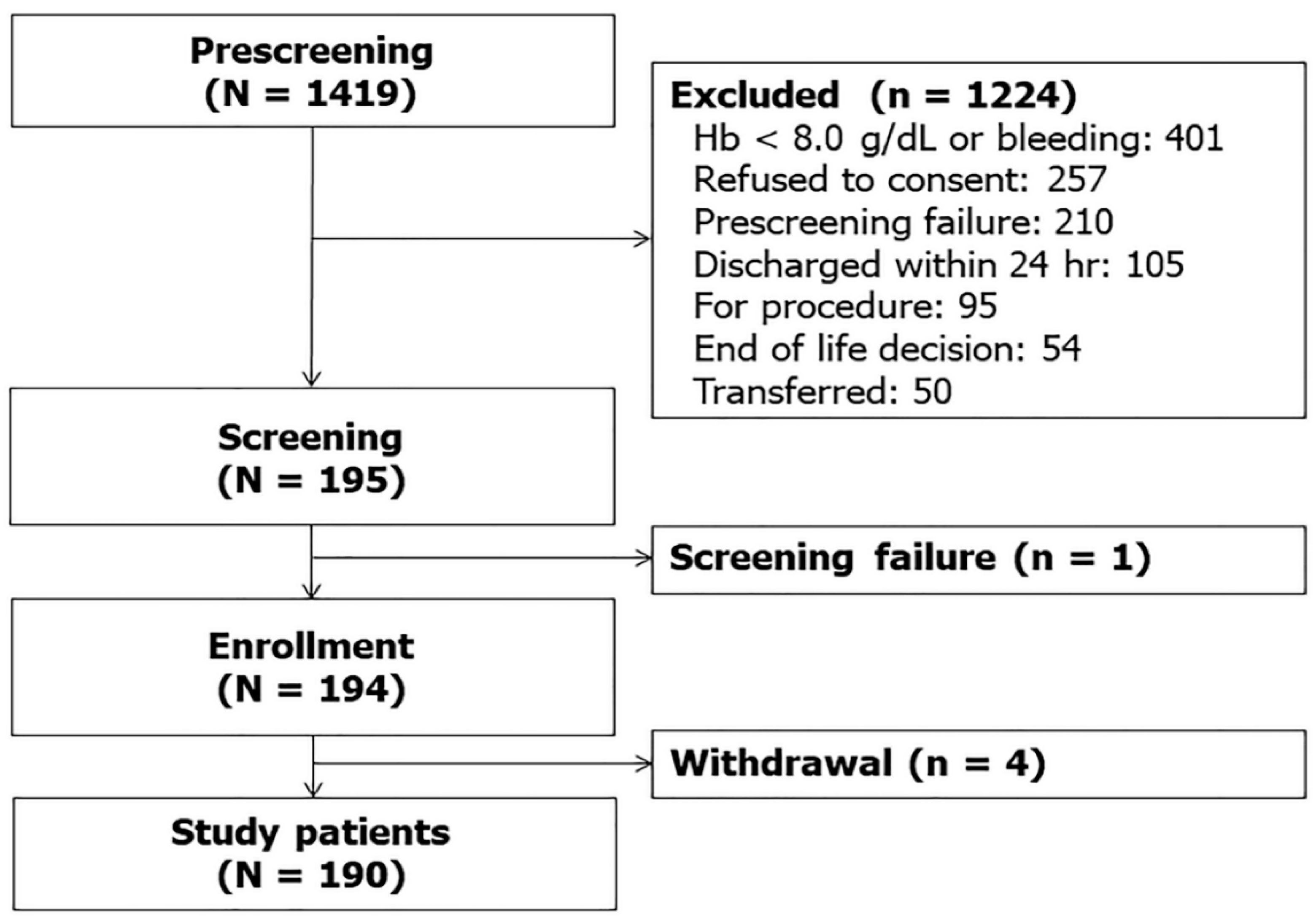
2.1. Study Design and Registry
2.2. Study Patients
2.3. Data Collection
2.4. Measurement of Plasma TRAIL and RIPK3
2.5. Statistical Analysis
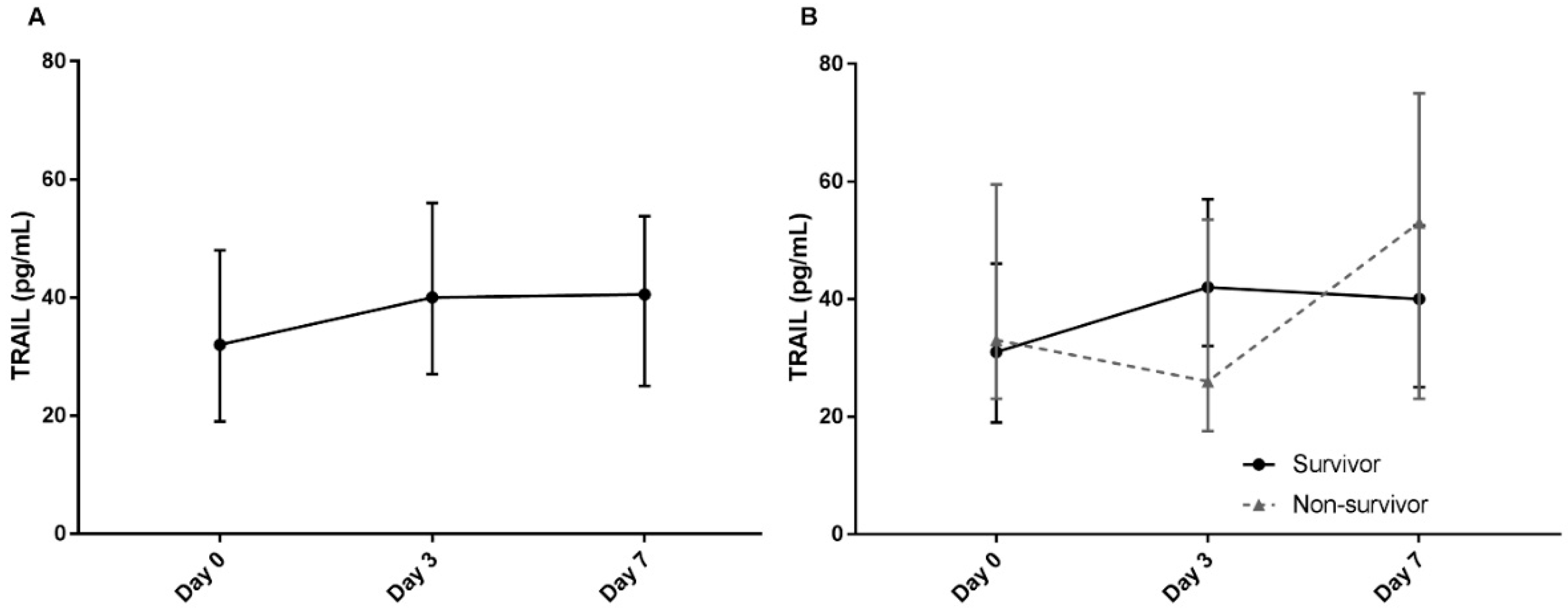
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
References
- Singer, M.; Deutschman, C.S.; Seymour, C.W.; Shankar-Hari, M.; Annane, D.; Bauer, M.; Bellomo, R.; Bernard, G.R.; Chiche, J.D.; Coopersmith, C.M.; et al. The Third International Consensus Definitions for Sepsis and Septic Shock (Sepsis-3). JAMA 2016, 315, 801–810. [Google Scholar] [CrossRef]
- Reinhart, K.; Daniels, R.; Kissoon, N.; Machado, F.R.; Schachter, R.D.; Finfer, S. Recognizing Sepsis as a Global Health Priority—A WHO Resolution. N. Engl. J. Med. 2017, 377, 414–417. [Google Scholar] [CrossRef]
- Rhodes, A.; Evans, L.E.; Alhazzani, W.; Levy, M.M.; Antonelli, M.; Ferrer, R.; Kumar, A.; Sevransky, J.E.; Sprung, C.L.; Nunnally, M.E.; et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Crit. Care Med. 2017, 45, 486–552. [Google Scholar] [CrossRef]
- Phua, J.; Koh, Y.; Du, B.; Tang, Y.Q.; Divatia, J.V.; Tan, C.C.; Gomersall, C.D.; Faruq, M.O.; Shrestha, B.R.; Gia Binh, N.; et al. Management of severe sepsis in patients admitted to Asian intensive care units: Prospective cohort study. BMJ 2011, 342, d3245. [Google Scholar] [CrossRef] [Green Version]
- Yang, Y.; Xie, J.; Guo, F.; Longhini, F.; Gao, Z.; Huang, Y.; Qiu, H. Combination of C-reactive protein, procalcitonin and sepsis-related organ failure score for the diagnosis of sepsis in critical patients. Ann. Intensive Care 2016, 6, 51. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Simon, L.; Saint-Louis, P.; Amre, D.K.; Lacroix, J.; Gauvin, F. Procalcitonin and C-reactive protein as markers of bacterial infection in critically ill children at onset of systemic inflammatory response syndrome. Pediatr Crit. Care Med. 2008, 9, 407–413. [Google Scholar] [CrossRef] [PubMed]
- Pierrakos, C.; Vincent, J.L. Sepsis biomarkers: A review. Crit. Care 2010, 14, R15. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Condotta, S.A.; Cabrera-Perez, J.; Badovinac, V.P.; Griffith, T.S. T-cell-mediated immunity and the role of TRAIL in sepsis-induced immunosuppression. Crit. Rev. Immunol. 2013, 33, 23–40. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Janssen, E.M.; Droin, N.M.; Lemmens, E.E.; Pinkoski, M.J.; Bensinger, S.J.; Ehst, B.D.; Griffith, T.S.; Green, D.R.; Schoenberger, S.P. CD4+ T-cell help controls CD8+ T-cell memory via TRAIL-mediated activation-induced cell death. Nature 2005, 434, 88–93. [Google Scholar] [CrossRef]
- Jouan-Lanhouet, S.; Arshad, M.I.; Piquet-Pellorce, C.; Martin-Chouly, C.; Le Moigne-Muller, G.; Van Herreweghe, F.; Takahashi, N.; Sergent, O.; Lagadic-Gossmann, D.; Vandenabeele, P.; et al. TRAIL induces necroptosis involving RIPK1/RIPK3-dependent PARP-1 activation. Cell Death Differ. 2012, 19, 2003–2014. [Google Scholar] [CrossRef] [Green Version]
- Kaczmarek, A.; Vandenabeele, P.; Krysko, D.V. Necroptosis: The release of damage-associated molecular patterns and its physiological relevance. Immunity 2013, 38, 209–223. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tian, Y.; Tao, T.; Zhu, J.; Zou, Y.; Wang, J.; Li, J.; Bo, L.; Deng, X. Soluble tumor necrosis factor related apoptosis inducing ligand level as a predictor of severity of sepsis and the risk of mortality in septic patients. PLoS ONE 2013, 8, e82204. [Google Scholar] [CrossRef] [Green Version]
- Schenck, E.J.; Ma, K.C.; Price, D.R.; Nicholson, T.; Oromendia, C.; Gentzler, E.R.; Sanchez, E.; Baron, R.M.; Fredenburgh, L.E.; Huh, J.W.; et al. Circulating cell death biomarker TRAIL is associated with increased organ dysfunction in sepsis. JCI Insight 2019, 4, e127143. [Google Scholar] [CrossRef] [PubMed]
- Newton, K.; Dugger, D.L.; Wickliffe, K.E.; Kapoor, N.; de Almagro, M.C.; Vucic, D.; Komuves, L.; Ferrando, R.E.; French, D.M.; Webster, J.; et al. Activity of protein kinase RIPK3 determines whether cells die by necroptosis or apoptosis. Science 2014, 343, 1357–1360. [Google Scholar] [CrossRef] [PubMed]
- Ma, K.C.; Schenck, E.J.; Siempos, I.I.; Cloonan, S.M.; Finkelsztein, E.J.; Pabon, M.A.; Oromendia, C.; Ballman, K.V.; Baron, R.M.; Fredenburgh, L.E.; et al. Circulating RIPK3 levels are associated with mortality and organ failure during critical illness. JCI Insight 2018, 3, e99692. [Google Scholar] [CrossRef] [Green Version]
- Knaus, W.A.; Draper, E.A.; Wagner, D.P.; Zimmerman, J.E. APACHE II: A severity of disease classification system. Crit. Care Med. 1985, 13, 818–829. [Google Scholar] [CrossRef]
- Moreno, R.P.; Metnitz, P.G.; Almeida, E.; Jordan, B.; Bauer, P.; Campos, R.A.; Iapichino, G.; Edbrooke, D.; Capuzzo, M.; Le Gall, J.R.; et al. SAPS 3—From evaluation of the patient to evaluation of the intensive care unit. Part 2: Development of a prognostic model for hospital mortality at ICU admission. Intensive Care Med. 2005, 31, 1345–1355. [Google Scholar] [CrossRef] [Green Version]
- Vincent, J.L.; Moreno, R.; Takala, J.; Willatts, S.; De Mendonca, A.; Bruining, H.; Reinhart, C.K.; Suter, P.M.; Thijs, L.G. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996, 22, 707–710. [Google Scholar] [CrossRef]
- Champion, H.R.; Sacco, W.J.; Copes, W.S.; Gann, D.S.; Gennarelli, T.A.; Flanagan, M.E. A revision of the Trauma Score. J. Trauma 1989, 29, 623–629. [Google Scholar] [CrossRef]
- McGrath, E.E.; Marriott, H.M.; Lawrie, A.; Francis, S.E.; Sabroe, I.; Renshaw, S.A.; Dockrell, D.H.; Whyte, M.K. TNF-related apoptosis-inducing ligand (TRAIL) regulates inflammatory neutrophil apoptosis and enhances resolution of inflammation. J. Leukoc. Biol. 2011, 90, 855–865. [Google Scholar] [CrossRef]
- Cretney, E.; McQualter, J.L.; Kayagaki, N.; Yagita, H.; Bernard, C.C.; Grewal, I.S.; Ashkenazi, A.; Smyth, M.J. TNF-related apoptosis-inducing ligand (TRAIL)/Apo2L suppresses experimental autoimmune encephalomyelitis in mice. Immunol. Cell Biol. 2005, 83, 511–519. [Google Scholar] [CrossRef]
- Hoffmann, O.; Priller, J.; Prozorovski, T.; Schulze-Topphoff, U.; Baeva, N.; Lunemann, J.D.; Aktas, O.; Mahrhofer, C.; Stricker, S.; Zipp, F.; et al. TRAIL limits excessive host immune responses in bacterial meningitis. J. Clin. Investig. 2007, 117, 2004–2013. [Google Scholar] [CrossRef] [Green Version]
- Lamhamedi-Cherradi, S.E.; Zheng, S.J.; Maguschak, K.A.; Peschon, J.; Chen, Y.H. Defective thymocyte apoptosis and accelerated autoimmune diseases in TRAIL-/- mice. Nat. Immunol. 2003, 4, 255–260. [Google Scholar] [CrossRef]
- Unsinger, J.; Kazama, H.; McDonough, J.S.; Griffith, T.S.; Hotchkiss, R.S.; Ferguson, T.A. Sepsis-induced apoptosis leads to active suppression of delayed-type hypersensitivity by CD8+ regulatory T cells through a TRAIL-dependent mechanism. J. Immunol. 2010, 184, 6766–6772. [Google Scholar] [CrossRef] [Green Version]
- Gurung, P.; Rai, D.; Condotta, S.A.; Babcock, J.C.; Badovinac, V.P.; Griffith, T.S. Immune unresponsiveness to secondary heterologous bacterial infection after sepsis induction is TRAIL dependent. J. Immunol. 2011, 187, 2148–2154. [Google Scholar] [CrossRef] [Green Version]
- Brincks, E.L.; Katewa, A.; Kucaba, T.A.; Griffith, T.S.; Legge, K.L. CD8 T cells utilize TRAIL to control influenza virus infection. J. Immunol. 2008, 181, 4918–4925. [Google Scholar] [CrossRef]
- Sato, K.; Hida, S.; Takayanagi, H.; Yokochi, T.; Kayagaki, N.; Takeda, K.; Yagita, H.; Okumura, K.; Tanaka, N.; Taniguchi, T.; et al. Antiviral response by natural killer cells through TRAIL gene induction by IFN-alpha/beta. Eur. J. Immunol. 2001, 31, 3138–3146. [Google Scholar] [CrossRef]
- Cardoso Alves, L.; Berger, M.D.; Koutsandreas, T.; Kirschke, N.; Lauer, C.; Sporri, R.; Chatziioannou, A.; Corazza, N.; Krebs, P. Non-apoptotic TRAIL function modulates NK cell activity during viral infection. EMBO Rep. 2020, 21, e48789. [Google Scholar] [CrossRef]
- Yatim, N.; Cullen, S.; Albert, M.L. Dying cells actively regulate adaptive immune responses. Nat. Rev. Immunol. 2017, 17, 262–275. [Google Scholar] [CrossRef]
- Moreno-Gonzalez, G.; Vandenabeele, P.; Krysko, D.V. Necroptosis: A Novel Cell Death Modality and Its Potential Relevance for Critical Care Medicine. Am. J. Respir. Crit. Care Med. 2016, 194, 415–428. [Google Scholar] [CrossRef]
- Kirkpatrick, A.W.; Coccolini, F.; Ansaloni, L.; Roberts, D.J.; Tolonen, M.; McKee, J.L.; Leppaniemi, A.; Faris, P.; Doig, C.J.; Catena, F.; et al. Closed Or Open after Source Control Laparotomy for Severe Complicated Intra-Abdominal Sepsis (the COOL trial): Study protocol for a randomized controlled trial. World J. Emerg. Surg. 2018, 13, 26. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Li, J.; Gao, H.M.; Xing, Y.H.; Lin, Z.; Li, H.J.; Wang, Y.Q. Necroptosis regulated proteins expression is an early prognostic biomarker in patient with sepsis: A prospective observational study. Oncotarget 2017, 8, 84066–84073. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vucur, M.; Roderburg, C.; Kaiser, L.; Schneider, A.T.; Roy, S.; Loosen, S.H.; Luedde, M.; Trautwein, C.; Koch, A.; Tacke, F.; et al. Elevated Serum Levels of Mixed Lineage Kinase Domain-Like Protein Predict Survival of Patients during Intensive Care Unit Treatment. Dis. Markers 2018, 2018, 1983421. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Gonzalvez, F.; Ashkenazi, A. New insights into apoptosis signaling by Apo2L/TRAIL. Oncogene 2010, 29, 4752–4765. [Google Scholar] [CrossRef] [Green Version]


| Characteristics | Total (N = 190) | Control (n = 47) | Sepsis (n = 143) | p Value |
|---|---|---|---|---|
| Age, years | 64 (54–73) | 60 (54–68) | 67 (53–74) | 0.086 |
| Gender, male | 121 (63.7) | 25 (46.8) | 96 (67.1) | 0.085 |
| Co-morbidities | ||||
| Solid tumor | 62 (32.6) | 11 (23.4) | 51 (35.7) | 0.120 |
| Hematologic malignancy | 32 (16.8) | 7 (14.9) | 25 (17.5) | 0.681 |
| Diabetes | 55 (28.9 | 12 (25.5) | 43 (30.1) | 0.552 |
| Chronic obstructive pulmonary disease | 18 (9.5) | 7 (14.9) | 11 (7.7) | 0.157 |
| Chronic kidney disease | 15 (7.9) | 4 (8.5) | 11 (7.7) | 1.000 |
| Myocardial infarction | 11 (5.8) | 4 (8.5) | 7 (4.9) | 0.470 |
| Congestive heart failure | 9 (4.7) | 4 (8.5) | 5 (3.5) | 0.228 |
| Cerebrovascular disease | 6 (3.2) | 0 | 6 (4.2) | 0.339 |
| Chronic liver disease | 1 (0.5) | 0 | 1 (0.7) | 1.000 |
| Charlson Comorbidity Index | 2 (1–3) | 2 (1–3) | 2 (1–3) | 0.554 |
| Clinical status on ICU admission | ||||
| Need for MV | 95 (50.0) | 32 (68.1) | 66 (46.2) | 0.009 |
| Need for vasopressor support | 116 (61.1) | 15 (31.9) | 101 (70.6) | <0.001 |
| Laboratory findings | ||||
| PaO2/FiO2 ratio | 139.3 (125.2–298.1) | 255.1 (125.4–362.1) | 181.3 (124.7–280.5) | 0.112 |
| CRP, mg/dL | 10.0 (3.0–19.0) | 5.4 (0.8–9.1) | 12.5 (4.1–22.5) | <0.001 |
| Lactic acid, mg/dL | 3.0 (2.0–4.0) | 2.4 (1.2–4.3) | 2.7 (1.8–4.0) | 0.230 |
| Severity of illness | ||||
| SAPS 3, points | 52 (44–59) | 48 (35–56) | 53 (46–59) | 0.008 |
| APACHE II score | 23 (18–28) | 22 (15–27) | 23 (19–29) | 0.184 |
| SOFA score, initial | 8 (5–11) | 5 (3–9) | 6 (6–11) | <0.001 |
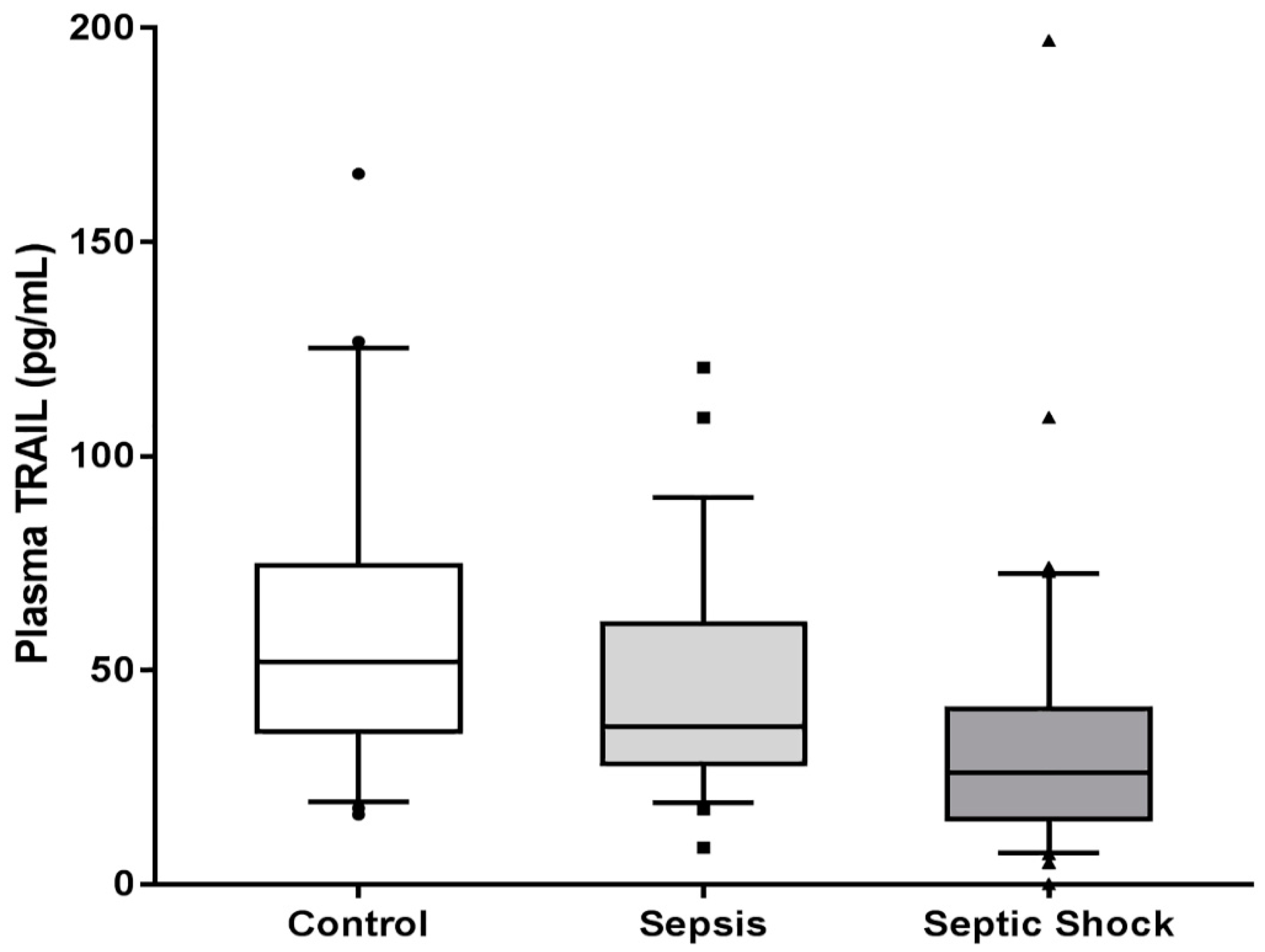
| Plasma TRAIL, pg/mL | 34.482 (23.446–56.946) | 52.000 (35.657–74.410) | 31.545 (19.289–47.564) | <0.001 |
| Outcome | ||||
| 28-day ICU mortality | 39 (20.5) | 10 (21.3) | 29 (20.3) | 0.883 |
| In-hospital mortality | 48 (25.3) | 12 (25.5) | 36 (25.2) | 0.961 |
| Characteristics | Low TRAIL (n = 72) | High TRAIL (n = 71) | p Value |
|---|---|---|---|
| Age, years | 67 (55–73) | 62 (51–74) | 0.418 |
| Gender, male | 40 (69.4) | 46 (64.8) | 0.553 |
| Co-morbidities | |||
| Solid tumor | 10 (13.9) | 16 (22.5) | 0.448 |
| Hematologic malignancy | 14 (19.4) | 11 (15.5) | 0.534 |
| Diabetes | 23 (31.9) | 20 (28.2) | 0.623 |
| Chronic kidney disease | 11 (11.6) | 7 (7.4) | 0.322 |
| Myocardial infarction | 8 (11.1) | 4 (5.6) | 0.217 |
| Congestive heart failure | 3 (4.2) | 3 (4.2) | 1.000 |
| Charlson Comorbidity Index | 2 (1–3) | 2 (1–3) | 0.668 |
| Septic shock | 52 (72.2%) | 32 (45.1%) | 0.001 |
| Clinical status on ICU admission | |||
| Need for MV | 36 (50.0) | 30 (42.3) | 0.353 |
| Need for vasopressor support | 61 (84.7) | 40 (56.3) | <0.001 |
| Laboratory findings | |||
| PaO2/FiO2 ratio | 191.7 (120.2–282.6) | 180.6 (130.5–277.5) | 0.436 |
| CRP, mg/dL | 13.7 (4.2–13.7) | 12.0 (4.0–22.5) | 0.305 |
| Lactic acid, mg/dL | 3.1 (2.1–4.5) | 2.3 (1.7–3.3) | <0.001 |
| Severity of illness | |||
| SAPS 3, points | 56 (50–68) | 50 (42–56) | <0.001 |
| APACHE II score | 24 (19–30) | 22 (19–27) | 0.007 |
| SOFA score, initial | 9 (7–11) | 7 (5–11) | <0.001 |
| Outcome | |||
| 28-day ICU mortality | 12 (16.7) | 17 (23.9) | 0.279 |
| In-hospital mortality | 19 (26.4) | 17 (23.9) | 0.736 |
| 90-day mortality | 23 (31.9) | 26 (36.6) | 0.556 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yoo, H.; Lee, J.Y.; Park, J.; Yang, J.H.; Suh, G.Y.; Jeon, K. Association of Plasma Level of TNF-Related Apoptosis-Inducing Ligand with Severity and Outcome of Sepsis. J. Clin. Med. 2020, 9, 1661. https://doi.org/10.3390/jcm9061661
Yoo H, Lee JY, Park J, Yang JH, Suh GY, Jeon K. Association of Plasma Level of TNF-Related Apoptosis-Inducing Ligand with Severity and Outcome of Sepsis. Journal of Clinical Medicine. 2020; 9(6):1661. https://doi.org/10.3390/jcm9061661
Chicago/Turabian StyleYoo, Hongseok, Jin Young Lee, Junseon Park, Jeong Hoon Yang, Gee Young Suh, and Kyeongman Jeon. 2020. "Association of Plasma Level of TNF-Related Apoptosis-Inducing Ligand with Severity and Outcome of Sepsis" Journal of Clinical Medicine 9, no. 6: 1661. https://doi.org/10.3390/jcm9061661
APA StyleYoo, H., Lee, J. Y., Park, J., Yang, J. H., Suh, G. Y., & Jeon, K. (2020). Association of Plasma Level of TNF-Related Apoptosis-Inducing Ligand with Severity and Outcome of Sepsis. Journal of Clinical Medicine, 9(6), 1661. https://doi.org/10.3390/jcm9061661






