Liver Transplant Patients with High Levels of Preoperative Serum Ammonia Are at Increased Risk for Postoperative Acute Kidney Injury: A Retrospective Study
Abstract
1. Introduction
2. Experimental Section
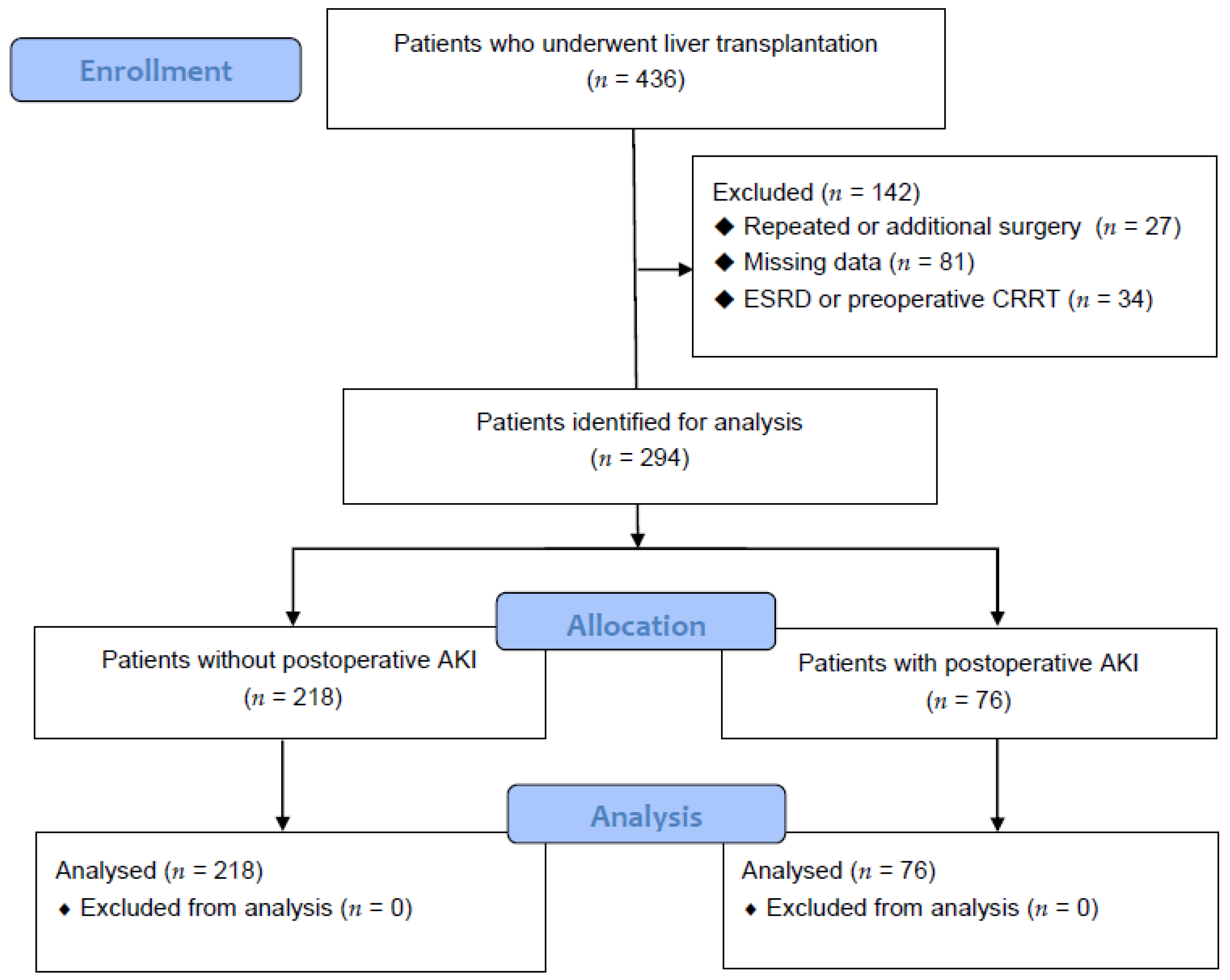
2.1. Patient Population
2.2. Data Collection
2.3. Intraoperative Protocol
2.4. Definition of AKI
2.5. Statistical Analysis
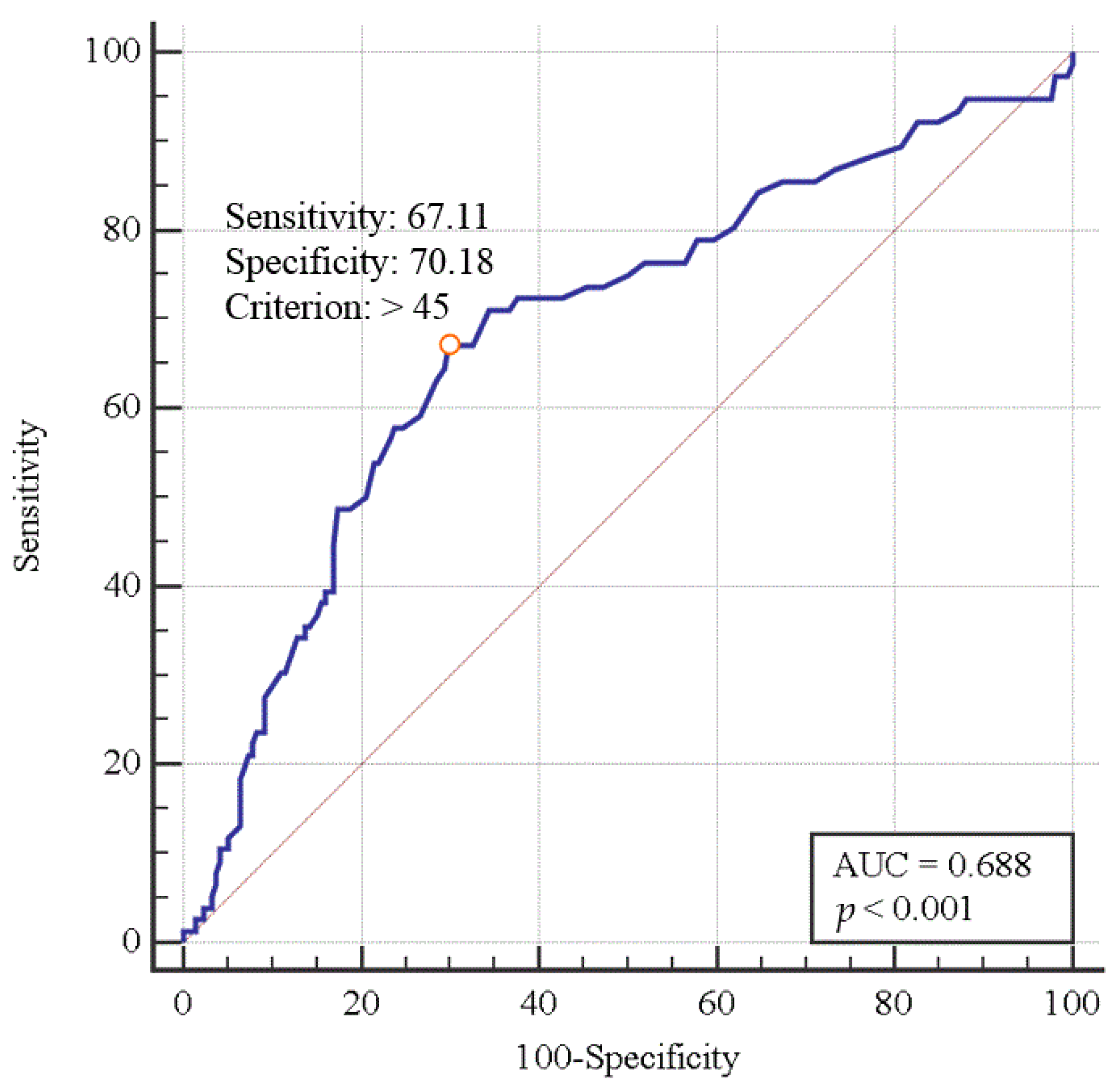
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lima, E.Q.; Zanetta, D.M.; Castro, I.; Massarollo, P.C.; Mies, S.; Machado, M.M.; Yu, L. Risk factors for development of acute renal failure after liver transplantation. Ren. Fail. 2003, 25, 553–560. [Google Scholar] [CrossRef]
- Karapanagiotou, A.; Kydona, C.; Dimitriadis, C.; Sgourou, K.; Giasnetsova, T.; Fouzas, I.; Imvrios, G.; Gritsi-Gerogianni, N. Acute kidney injury after orthotopic liver transplantation. Transplant. Proc. 2012, 44, 2727–2729. [Google Scholar] [CrossRef]
- Barreto, A.G.; Daher, E.F.; Silva Junior, G.B.; Garcia, J.H.; Magalhaes, C.B.; Lima, J.M.; Viana, C.F.; Pereira, E.D. Risk factors for acute kidney injury and 30-day mortality after liver transplantation. Ann. Hepatol. 2015, 14, 688–694. [Google Scholar] [CrossRef]
- Yalavarthy, R.; Edelstein, C.L.; Teitelbaum, I. Acute renal failure and chronic kidney disease following liver transplantation. Hemodial. Int. Int. Symp. Home Hemodial. 2007, 11 (Suppl. S3), S7–S12. [Google Scholar] [CrossRef] [PubMed]
- Afonso, R.C.; Hidalgo, R.; Zurstrassen, M.P.; Fonseca, L.E.; Pandullo, F.L.; Rezende, M.B.; Meira-Filho, S.P.; Ferraz-Neto, B.H. Impact of renal failure on liver transplantation survival. Transplant. Proc. 2008, 40, 808–810. [Google Scholar] [CrossRef]
- Gonwa, T.A.; Mai, M.L.; Melton, L.B.; Hays, S.R.; Goldstein, R.M.; Levy, M.F.; Klintmalm, G.B. Renal replacement therapy and orthotopic liver transplantation: The role of continuous veno-venous hemodialysis. Transplantation 2001, 71, 1424–1428. [Google Scholar] [CrossRef]
- Mehta, R.L.; Kellum, J.A.; Shah, S.V.; Molitoris, B.A.; Ronco, C.; Warnock, D.G.; Levin, A. Acute Kidney Injury Network: Report of an initiative to improve outcomes in acute kidney injury. Crit. Care 2007, 11, R31. [Google Scholar] [CrossRef]
- Ojo, A.O.; Held, P.J.; Port, F.K.; Wolfe, R.A.; Leichtman, A.B.; Young, E.W.; Arndorfer, J.; Christensen, L.; Merion, R.M. Chronic renal failure after transplantation of a nonrenal organ. N. Engl. J. Med. 2003, 349, 931–940. [Google Scholar] [CrossRef]
- Goldberg, D.S.; Ruebner, R.L.; Abt, P.L. The Risk of End-Stage Renal Disease Among Living Donor Liver Transplant Recipients in the United States. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2015, 15, 2732–2738. [Google Scholar] [CrossRef]
- Tinti, F.; Umbro, I.; Mecule, A.; Rossi, M.; Merli, M.; Nofroni, I.; Corradini, S.G.; Poli, L.; Pugliese, F.; Ruberto, F.; et al. RIFLE criteria and hepatic function in the assessment of acute renal failure in liver transplantation. Transplant. Proc. 2010, 42, 1233–1236. [Google Scholar] [CrossRef]
- Park, M.H.; Shim, H.S.; Kim, W.H.; Kim, H.J.; Kim, D.J.; Lee, S.H.; Kim, C.S.; Gwak, M.S.; Kim, G.S. Clinical Risk Scoring Models for Prediction of Acute Kidney Injury after Living Donor Liver Transplantation: A Retrospective Observational Study. PLoS ONE 2015, 10, e0136230. [Google Scholar] [CrossRef] [PubMed]
- Weber, M.L.; Ibrahim, H.N.; Lake, J.R. Renal dysfunction in liver transplant recipients: Evaluation of the critical issues. Liver Transplant. Off. Publ. Am. Assoc. Study Liver Dis. Int. Liver Transplant. Soc. 2012, 18, 1290–1301. [Google Scholar] [CrossRef] [PubMed]
- Nuno, J.; Cuervas-Mons, V.; Vicente, E.; Turrion, V.; Pereira, F.; Mora, N.P.; Barrios, C.; Millan, I.; Ardaiz, J. Renal failure after liver transplantation: Analysis of risk factors in 139 liver transplant recipients. Transplant. Proc. 1995, 27, 2319–2320. [Google Scholar] [PubMed]
- Gonwa, T.A.; Mai, M.L.; Melton, L.B.; Hays, S.R.; Goldstein, R.M.; Levy, M.F.; Klintmalm, G.B. End-stage renal disease (ESRD) after orthotopic liver transplantation (OLTX) using calcineurin-based immunotherapy: Risk of development and treatment. Transplantation 2001, 72, 1934–1939. [Google Scholar] [CrossRef]
- Olde Damink, S.W.; Jalan, R.; Dejong, C.H. Interorgan ammonia trafficking in liver disease. Metab. Brain Dis. 2009, 24, 169–181. [Google Scholar] [CrossRef]
- Olde Damink, S.W.; Jalan, R.; Deutz, N.E.; Redhead, D.N.; Dejong, C.H.; Hynd, P.; Jalan, R.A.; Hayes, P.C.; Soeters, P.B. The kidney plays a major role in the hyperammonemia seen after simulated or actual GI bleeding in patients with cirrhosis. Hepatology 2003, 37, 1277–1285. [Google Scholar] [CrossRef]
- Olde Damink, S.W.; Dejong, C.H.; Deutz, N.E.; Redhead, D.N.; Hayes, P.C.; Soeters, P.B.; Jalan, R. Kidney plays a major role in ammonia homeostasis after portasystemic shunting in patients with cirrhosis. Am. J. Physiol. Gastrointest. Liver Physiol. 2006, 291, G189–G194. [Google Scholar] [CrossRef][Green Version]
- Dasarathy, S.; Mookerjee, R.P.; Rackayova, V.; Rangroo Thrane, V.; Vairappan, B.; Ott, P.; Rose, C.F. Ammonia toxicity: From head to toe? Metab. Brain Dis. 2017, 32, 529–538. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. Available online: https://www.R-project.org/ (accessed on 23 May 2020).
- Barri, Y.M.; Sanchez, E.Q.; Jennings, L.W.; Melton, L.B.; Hays, S.; Levy, M.F.; Klintmalm, G.B. Acute kidney injury following liver transplantation: Definition and outcome. Liver Transplant. Off. Publ. Am. Assoc. Study Liver Dis. Int. Liver Transplant. Soc. 2009, 15, 475–483. [Google Scholar] [CrossRef]
- Inoue, Y.; Soyama, A.; Takatsuki, M.; Hidaka, M.; Muraoka, I.; Kanematsu, T.; Eguchi, S. Acute kidney injury following living donor liver transplantation. Clin. Transplant. 2012, 26, E530–E535. [Google Scholar] [CrossRef]
- Akamatsu, N.; Sugawara, Y.; Tamura, S.; Kakeno, J.; Togashi, J.; Makuuchi, M. Renal impairment after living donor liver transplantation. Transplant. Proc. 2006, 38, 1474–1476. [Google Scholar] [CrossRef] [PubMed]
- Utsumi, M.; Umeda, Y.; Sadamori, H.; Nagasaka, T.; Takaki, A.; Matsuda, H.; Shinoura, S.; Yoshida, R.; Nobuoka, D.; Satoh, D.; et al. Risk factors for acute renal injury in living donor liver transplantation: Evaluation of the RIFLE criteria. Transpl. Int. Off. J. Eur. Soc. Organ Transplant. 2013, 26, 842–852. [Google Scholar] [CrossRef] [PubMed]
- Thongprayoon, C.; Kaewput, W.; Thamcharoen, N.; Bathini, T.; Watthanasuntorn, K.; Lertjitbanjong, P.; Sharma, K.; Salim, S.A.; Ungprasert, P.; Wijarnpreecha, K.; et al. Incidence and Impact of Acute Kidney Injury after Liver Transplantation: A Meta-Analysis. J. Clin. Med. 2019, 8, 372. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.L.; Gonwa, T.A.; Wilkinson, A.H. Pathophysiology of renal disease associated with liver disorders: Implications for liver transplantation. Part I. Liver Transplant. Off. Publ. Am. Assoc. Study Liver Dis. Int. Liver Transplant. Soc. 2002, 8, 91–109. [Google Scholar] [CrossRef]
- Biancofiore, G.; Pucci, L.; Cerutti, E.; Penno, G.; Pardini, E.; Esposito, M.; Bindi, L.; Pelati, E.; Romanelli, A.; Triscornia, S.; et al. Cystatin C as a marker of renal function immediately after liver transplantation. Liver Transplant. Off. Publ. Am. Assoc. Study Liver Dis. Int. Liver Transplant. Soc. 2006, 12, 285–291. [Google Scholar] [CrossRef]
- Aberg, F.; Koivusalo, A.M.; Hockerstedt, K.; Isoniemi, H. Renal dysfunction in liver transplant patients: Comparing patients transplanted for liver tumor or acute or chronic disease. Transpl. Int. Off. J. Eur. Soc. Organ Transplant. 2007, 20, 591–599. [Google Scholar] [CrossRef]
- Tomozawa, A.; Ishikawa, S.; Shiota, N.; Cholvisudhi, P.; Makita, K. Perioperative risk factors for acute kidney injury after liver resection surgery: An historical cohort study. Can. J. Anaesth. J. Can. D’anesth. 2015, 62, 753–761. [Google Scholar] [CrossRef] [PubMed]
- Peres, L.A.; Bredt, L.C.; Cipriani, R.F. Acute renal injury after partial hepatectomy. World J. Hepatol. 2016, 8, 891–901. [Google Scholar] [CrossRef] [PubMed]
- Weiner, I.D.; Verlander, J.W. Recent advances in understanding renal ammonia metabolism and transport. Curr. Opin. Nephrol. Hypertens. 2016, 25, 436–443. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Weiner, I.D.; Mitch, W.E.; Sands, J.M. Urea and Ammonia Metabolism and the Control of Renal Nitrogen Excretion. Clin. J. Am. Soc. Nephrol. CJASN 2015, 10, 1444–1458. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.W. Renal dysfunction in patients with chronic liver disease. Electrolyte Blood Press. EBP 2009, 7, 42–50. [Google Scholar] [CrossRef] [PubMed]
- Cardenas, A. Hepatorenal syndrome: A dreaded complication of end-stage liver disease. Am. J. Gastroenterol. 2005, 100, 460–467. [Google Scholar] [CrossRef]
- Owen, E.E.; Johnson, J.H.; Tyor, M.P. The effect of induced hyperammonemia on renal ammonia metabolism. J. Clin. Investig. 1961, 40, 215–221. [Google Scholar] [CrossRef] [PubMed]
- Dan, H.; Peng, R.X.; Ao, Y.; Liu, Y.H. Segment-specific proximal tubule injury in tripterygium glycosides intoxicated rats. J. Biochem. Mol. Toxicol. 2008, 22, 422–428. [Google Scholar] [CrossRef]
- Cauli, O.; Rodrigo, R.; Piedrafita, B.; Boix, J.; Felipo, V. Inflammation and hepatic encephalopathy: Ibuprofen restores learning ability in rats with portacaval shunts. Hepatology 2007, 46, 514–519. [Google Scholar] [CrossRef]
- Basile, D.P.; Anderson, M.D.; Sutton, T.A. Pathophysiology of acute kidney injury. Compr. Physiol. 2012, 2, 1303–1353. [Google Scholar] [CrossRef]
- Orvell, B.D.; Wesson, L.G. Some effects of ammonium salts on renal histology and function in the dog. Nephron 1976, 16, 42–49. [Google Scholar] [CrossRef]
| C Group (n = 218) | AKI Group (n = 76) | p-Value | |
|---|---|---|---|
| Age (yr) | 52.72 ± 8.49 | 55.09 ± 7.50 | 0.032 * |
| Sex (F/M) | 156 (71.56)/62 (28.44) | 55 (72.37)/21 (27.63) | 0.893 |
| Body mass index (kg/m2) | 22.05 ± 3.19 | 22.76 ± 3.66 | 0.108 |
| CDLT/LDLT | 62 (28.44)/156 (71.56) | 40 (52.63)/36 (47.37) | <0.001 * |
| Cause of LT | 0.007 * | ||
| Alcoholic cirrhosis | 46 (21.1) | 22 (28.95) | |
| HBV/HCV infection | 149 (68.35) | 37 (48.68) | |
| NBNC LC | 11 (5.05) | 5 (6.58) | |
| Toxic hepatitis | 8 (3.67) | 10 (13.16) | |
| Primary biliary cirrhosis | 4 (1.83) | 2 (2.63) | |
| MELD score | 17.52 ± 11.06 | 22.20 ± 10.48 | 0.001 * |
| Hypertension | 43 (19.72) | 15 (19.74) | 0.998 |
| Diabetes mellitus | 53 (24.31) | 22 (28.95) | 0.425 |
| Ischemic heart disease | 1 (0.46) | 1 (1.32) | 0.451 |
| Congestive heart failure | 1 (0.46) | 2 (2.63) | 0.165 |
| Cerebrovascular accidents | 2 (0.92) | 0 (0.00) | 1.000 |
| Cardiac arrhythmia | 5 (2.29) | 3 (3.95) | 0.430 |
| With diuretics | 46 (21.1) | 14 (18.42) | 0.618 |
| With insulin | 8 (3.67) | 4 (5.26) | 0.515 |
| With ß-blocker | 8 (3.67) | 2 (2.63) | 1.000 |
| With calcium channel blocker | 14 (6.42) | 2 (2.63) | 0.256 |
| C Group (n = 218) | AKI Group (n = 76) | p-Value | |
|---|---|---|---|
| Hemoglobin (g/dL) | 11.04 ± 2.34 | 10.17 ± 2.07 | 0.004 * |
| Platelets (×103/mL) | 66.50 (46.00, 106.00) | 57.00 (43.67, 81.25) | 0.067 |
| Creatinine (mg/dL) | 0.77 (0.63, 0.98) | 0.84 (0.63, 1.00) | 0.492 |
| AST (unit/L) | 50.50 (34.00, 76.00) | 45.50 (34.00, 80.75) | 0.474 |
| ALT (unit/L) | 31.00 (21.25, 50.00) | 27.00 (17.00, 43.75) | 0.113 |
| Protein (g/dL) | 6.01 ± 0.87 | 5.96 ± 0.90 | 0.652 |
| Albumin (g/dL) | 3.19 ± 0.58 | 3.06 ± 0.53 | 0.085 |
| Ammonia (μg/dL) | 35.50 (24.00, 49.00) | 55.50 (35.75, 76.25) | <0.001 * |
| ≤45 μg/dL | 153 (70.2) | 25 (32.9) | <0.001 * |
| >45 μg/dL | 65 (29.8) | 51 (67.1) | |
| Bilirubin (mg/dL) | 2.40 (1.22, 12.02) | 4.40 (2.18, 15.57) | 0.001 * |
| PT (INR) | 1.47 (1.21, 2.10) | 1.91 (1.54, 2.43) | <0.001 * |
| Sodium (mEq/L) | 136.49 ± 5.63 | 136.75 ± 5.38 | 0.722 |
| Potassium (mEq/L) | 3.93 ± 0.49 | 4.04 ± 0.52 | 0.086 |
| C Group (n = 218) | AKI Group (n = 76) | p-Value | |
|---|---|---|---|
| Anesthesia duration (h) | 11.00 (9.50, 12.50) | 10.00 (8.50, 12.00) | 0.013 * |
| Estimated blood loss (L) | 2.50 (1.50, 4.50) | 3.35 (2.50, 6.00) | <0.001 * |
| Total fluid intake (L) | 6.90 (5.18, 9.67) | 8.07 (6.08, 12.23) | 0.006 * |
| pRBC (unit) | 4.00 (0.00, 8.00) | 7.00 (2.00, 12.00) | 0.001 * |
| Fresh frozen plasma (unit) | 4.00 (0.00, 9.00) | 7.50 (2.00, 12.00) | 0.001 * |
| Cryoprecipitate (unit) | 0.00 (0.00, 0.00) | 0.00 (0.00, 0.00) | 0.428 |
| Platelets (unit) | 0.00 (0.00, 0.00) | 0.00 (0.00, 8.00) | 0.001 * |
| C Group (n = 218) | AKI Group (n = 76) | p-Value | |
|---|---|---|---|
| Hemoglobin (g/dL) | 9.04 ± 1.45 | 8.94 ± 1.58 | 0.633 |
| Platelets (×103/mL) | 53.50 (39.25, 77.00) | 46.50 (36.00, 61.50) | 0.053 |
| PT (INR) | 1.76 (1.54, 1.95) | 1.80 (1.42, 2.04) | 0.919 |
| Bilirubin (mg/dL) | 4.10 (2.10, 6.68) | 5.75 (2.98, 8.65) | 0.007 * |
| Protein (g/dL) | 5.30 ± 0.65 | 5.09 ± 0.74 | 0.018 * |
| Albumin (g/dL) | 3.66 ± 0.45 | 3.56 ± 0.56 | 0.160 |
| Creatinine (mg/dL) | 0.90 ± 0.33 | 1.39 ± 0.48 | <0.001 * |
| Sodium (mEq/L) | 139.30 ± 3.71 | 140.12 ± 4.23 | 0.111 |
| Potassium (mEq/L) | 3.96 ± 0.38 | 4.12 ± 0.47 | 0.007 * |
| Stay in the intensive care unit (days) | 7.00 (5.00, 11.00) | 11.00 (6.00, 17.50) | <0.001 * |
| Time from surgery to discharge (days) | 27.00 (22.00, 38.00) | 32.50 (25.00, 52.50) | 0.006 * |
| Predictors | OR | 95% CI | p-Value * | OR | 95% CI | p-Value † | ||
|---|---|---|---|---|---|---|---|---|
| Lower | Upper | Lower | Upper | |||||
| Ammonia (>45) | 4.802 | 2.744 | 8.403 | <0.0001 * | 4.081 | 2.242 | 7.427 | <0.0001 † |
| Preoperative patient characteristics | ||||||||
| Age | 1.038 | 1.003 | 1.075 | 0.033 * | 1.040 | 1.003 | 1.079 | 0.034 † |
| Sex | 1.041 | 0.581 | 1.863 | 0.893 | ||||
| Body mass index | 1.066 | 0.986 | 1.153 | 0.109 | ||||
| MELD score | 1.037 | 1.014 | 1.062 | 0.002 * | 1.010 | 0.980 | 1.041 | 0.531 |
| Hypertension | 1.001 | 0.519 | 1.929 | 0.998 | ||||
| Diabetes mellitus | 1.268 | 0.707 | 2.275 | 0.425 | ||||
| IHD | 2.889 | 0.178 | 46.766 | 0.455 | ||||
| CHF | 5.864 | 0.524 | 65.604 | 0.151 | ||||
| With ß-blocker | 0.394 | 0.087 | 1.774 | 0.225 | ||||
| With CCB | 0.710 | 0.147 | 3.417 | 0.669 | ||||
| With diuretics | 0.844 | 0.434 | 1.642 | 0.618 | ||||
| With insulin | 1.459 | 0.426 | 4.988 | 0.547 | ||||
| Preoperative laboratory data | ||||||||
| Hemoglobin | 0.736 | 0.639 | 0.849 | <0.0001 * | 0.921 | 0.789 | 1.074 | 0.295 |
| Platelets | 0.994 | 0.989 | 1.000 | 0.069 | ||||
| Bilirubin | 1.016 | 0.996 | 1.037 | 0.124 | ||||
| Albumin | 0.660 | 0.410 | 1.061 | 0.086 | ||||
| Na | 1.009 | 0.962 | 1.057 | 0.721 | ||||
| K | 1.590 | 0.934 | 2.707 | 0.087 | ||||
| Cr | 1.100 | 0.649 | 1.866 | 0.723 | ||||
| Intraoperative data | ||||||||
| Anesthesia duration | 0.899 | 0.805 | 1.003 | 0.058 | ||||
| EBL | 1.070 | 0.993 | 1.152 | 0.075 | ||||
| Total fluid | 1.046 | 1.003 | 1.091 | 0.038 * | 0.992 | 0.932 | 1.055 | 0.798 |
| pRBC | 1.051 | 1.014 | 1.090 | 0.007 * | 1.020 | 0.974 | 1.068 | 0.394 |
| Overall (n = 294) | ≤45 μg/dL (n = 178) | >45 μg/dL (n = 116) | p-Value | |
|---|---|---|---|---|
| Total | <0.0001 * | |||
| Normal | 218 (74.15) | 153 (85.96) | 65 (56.03) | |
| AKI | 76 (25.85) | 25 (14.04) | 51 (43.97) | |
| AKI stage | <0.0001 * | |||
| 0 | 218 (74.15) | 153 (85.96) | 65 (56.03) | |
| 1 | 62 (21.09) | 21 (11.80) | 41 (35.34) | |
| 2 | 11 (3.74) | 3 (1.69) | 8 (6.90) | |
| 3 | 3 (1.02) | 1 (0.56) | 2 (1.72) | |
| Creatinine ≤ 1.2 mg/dL | ||||
| Normal | 185 (74.9) | 140 (86.4) | 45 (52.9) | <0.001 * |
| AKI | 62 (25.1) | 22 (13.6) | 40 (47.1) | |
| AKI stage | ||||
| 0 | 185 (74.9) | 140 (86.4) | 45 (52.9) | <0.001 * |
| 1 | 48 (19.4) | 18 (11.1) | 30 (35.3) | |
| 2 | 11 (4.5) | 3 (1.9) | 8 (9.4) | |
| 3 | 3 (1.2) | 1 (0.6) | 2 (2.4) | |
| Creatinine > 1.2 mg/dL | ||||
| Normal | 33 (70.2) | 13 (81.2) | 20 (64.5) | 0.321 |
| AKI | 14 (29.8) | 3 (18.8) | 11 (35.5) | |
| AKI stage | <0.0001 * | |||
| 0 | 218 (74.15) | 153 (85.96) | 65 (56.03) | |
| 1 | 62 (21.09) | 21 (11.80) | 41 (35.34) | |
| 2 | 11 (3.74) | 3 (1.69) | 8 (6.90) | |
| 3 | 3 (1.02) | 1 (0.56) | 2 (1.72) | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lee, Y.S.; Choi, Y.J.; Park, K.H.; Park, B.S.; Son, J.-M.; Park, J.Y.; Ri, H.-S.; Ryu, J.H. Liver Transplant Patients with High Levels of Preoperative Serum Ammonia Are at Increased Risk for Postoperative Acute Kidney Injury: A Retrospective Study. J. Clin. Med. 2020, 9, 1629. https://doi.org/10.3390/jcm9061629
Lee YS, Choi YJ, Park KH, Park BS, Son J-M, Park JY, Ri H-S, Ryu JH. Liver Transplant Patients with High Levels of Preoperative Serum Ammonia Are at Increased Risk for Postoperative Acute Kidney Injury: A Retrospective Study. Journal of Clinical Medicine. 2020; 9(6):1629. https://doi.org/10.3390/jcm9061629
Chicago/Turabian StyleLee, Yoon Sook, Yoon Ji Choi, Kyu Hee Park, Byeong Seon Park, Jung-Min Son, Ju Yeon Park, Hyun-Su Ri, and Je Ho Ryu. 2020. "Liver Transplant Patients with High Levels of Preoperative Serum Ammonia Are at Increased Risk for Postoperative Acute Kidney Injury: A Retrospective Study" Journal of Clinical Medicine 9, no. 6: 1629. https://doi.org/10.3390/jcm9061629
APA StyleLee, Y. S., Choi, Y. J., Park, K. H., Park, B. S., Son, J.-M., Park, J. Y., Ri, H.-S., & Ryu, J. H. (2020). Liver Transplant Patients with High Levels of Preoperative Serum Ammonia Are at Increased Risk for Postoperative Acute Kidney Injury: A Retrospective Study. Journal of Clinical Medicine, 9(6), 1629. https://doi.org/10.3390/jcm9061629





