A Single-Arm, Prospective, Exploratory Study to Preliminarily Test Effectiveness and Safety of Skin Electrical Stimulation for Leber Hereditary Optic Neuropathy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Ethics
2.2. Trial Registration
2.3. Inclusion and Exclusion Criteria
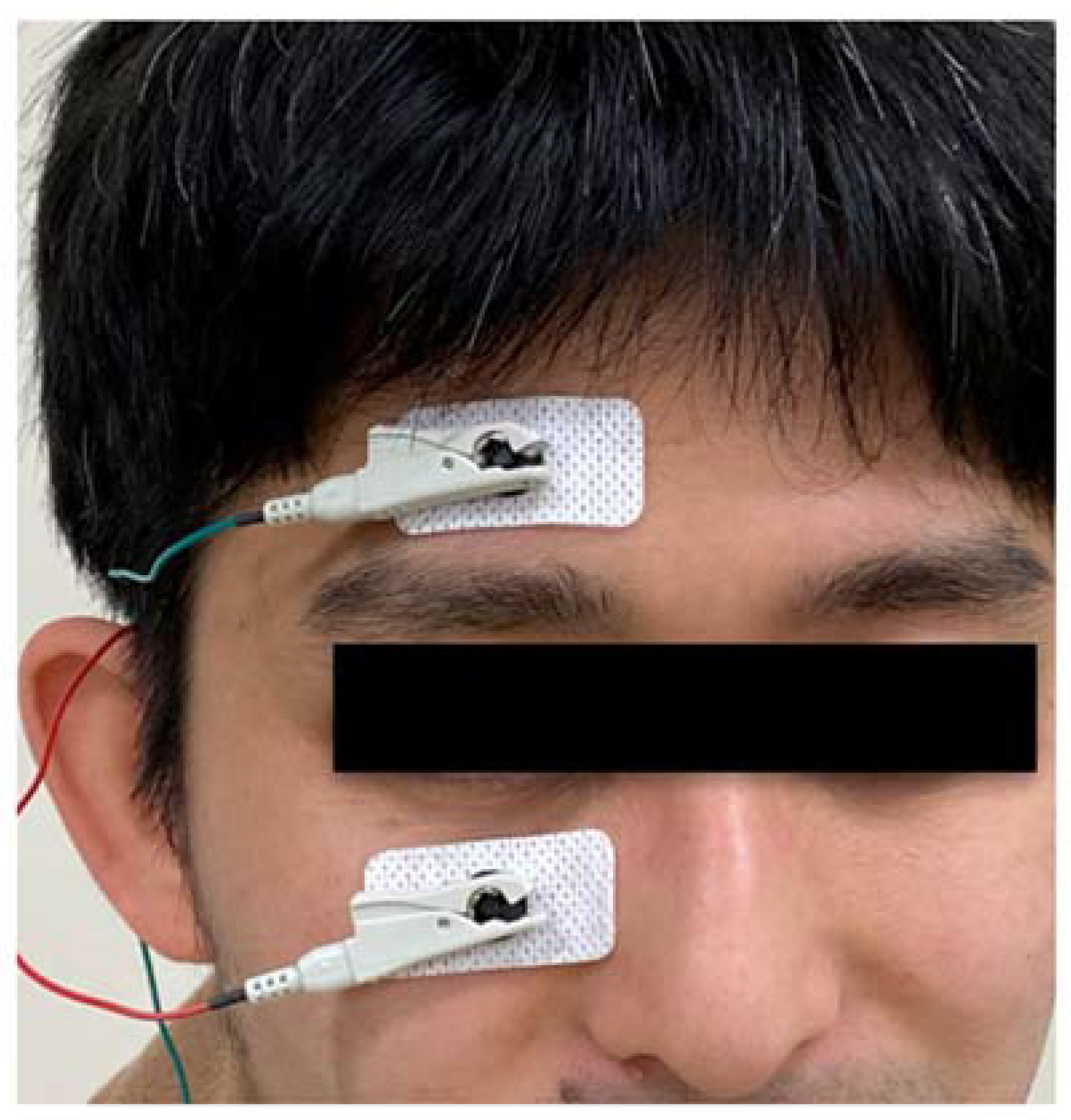
2.4. Interventions
2.5. Outcomes
2.5.1. Parameters
2.5.2. Primary and Secondary Outcomes
2.5.3. Calculating the SNR-AUC
2.6. Sample Size Determination and Power
2.7. Statistical Analysis
3. Results
3.1. Baseline Clinical Data
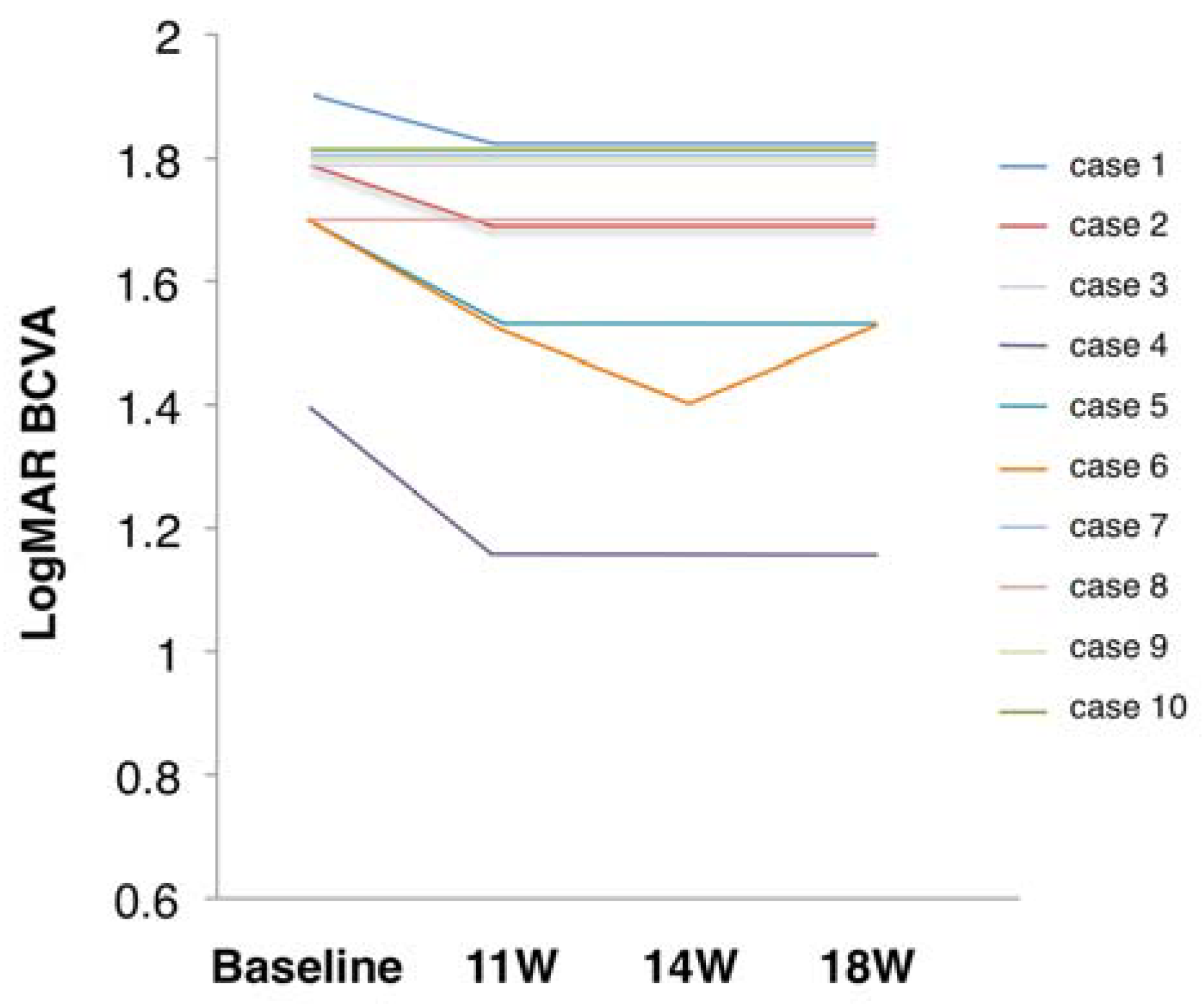
3.2. Primary Outcome Measure
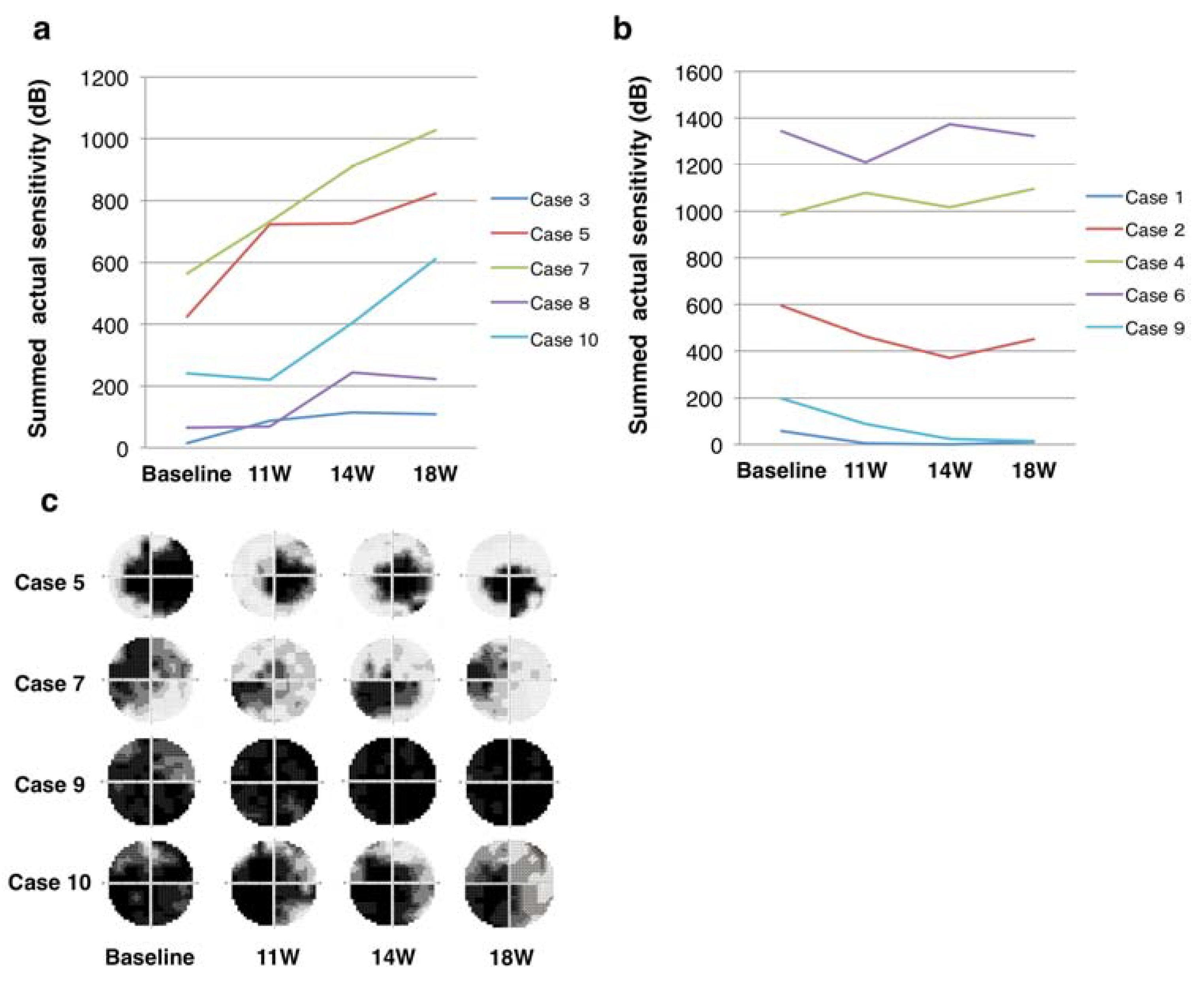
3.3. Secondary Outcome Measures
3.4. Safety and Tolerability
4. Discussion
4.1. Summary
4.2. Comparison with Treatment Alternatives
4.3. Prognostic Factors
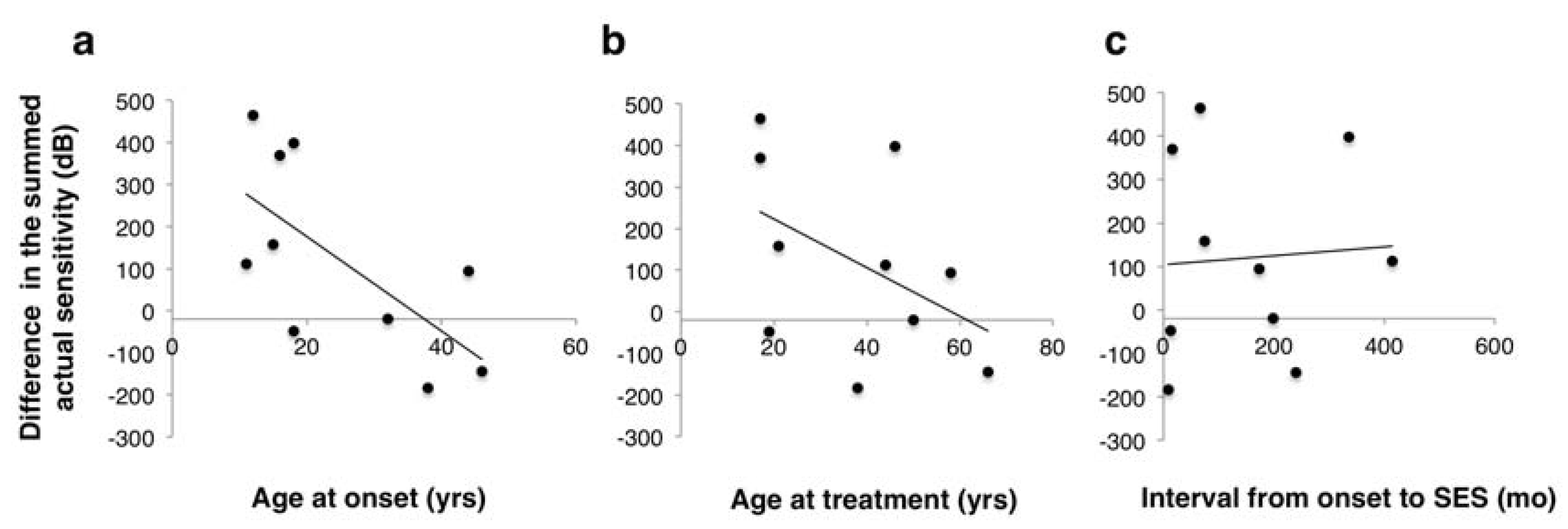
4.4. The Mechanisms of SES
4.5. Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Yu-Wai-Man, P.; Votruba, M.; Moore, A.T.; Chinnery, P.F. Treatment strategies for inherited optic neuropathies: Past, present and future. Eye 2014, 28, 521–537. [Google Scholar] [CrossRef] [PubMed]
- Ueda, K.; Morizane, Y.; Shiraga, F.; Shikishima, K.; Ishikawa, H.; Wakakura, M.; Nakamura, M. Nationwide epidemiological survey of Leber hereditary optic neuropathy in Japan. J. Epidemiol. 2017, 27, 447–450. [Google Scholar] [CrossRef] [PubMed]
- Yu-Wai-Man, P.; Votruba, M.; Burte, F.; La Morgia, C.; Barboni, P.; Carelli, V. A neurodegenerative perspective on mitochondrial optic neuropathies. Acta Neuropathol. 2016, 132, 789–806. [Google Scholar] [CrossRef] [PubMed]
- Klopstock, T.; Yu-Wai-Man, P.; Dimitriadis, K.; Rouleau, J.; Heck, S.; Bailie, M.; Atawan, A.; Chattopadhyay, S.; Schubert, M.; Garip, A.; et al. A randomized placebo-controlled trial of idebenone in Leber’s hereditary optic neuropathy. Brain 2011, 134, 2677–2686. [Google Scholar] [CrossRef] [PubMed]
- Sadun, A.A.; Chicani, C.F.; Ross-Cisneros, F.N.; Barboni, P.; Thoolen, M.; Shrader, W.D.; Kubis, K.; Carelli, V.; Miller, G. Effect of EPI-743 on the clinical course of the mitochondrial disease Leber hereditary optic neuropathy. Arch Neurol. 2012, 69, 331–338. [Google Scholar] [CrossRef] [PubMed]
- Guy, J.; Feuer, W.J.; Davis, J.L.; Porciatti, V.; Gonzalez, P.J.; Koilkonda, R.D.; Yuan, H.; Hauswirth, W.W.; Lam, B.L. Gene Therapy for Leber Hereditary Optic Neuropathy: Low- and Medium-Dose Visual Results. Ophthalmology. 2017, 124, 1621–1634. [Google Scholar] [CrossRef] [PubMed]
- Fujikado, T.; Morimoto, T.; Matsushita, K.; Shimojo, H.; Okawa, Y.; Tano, Y. Effect of transcorneal electrical stimulation in patients with nonarteritic ischemic optic neuropathy or traumatic optic neuropathy. Jpn. J. Ophthalmol. 2006, 50, 266–273. [Google Scholar] [CrossRef]
- Inomata, K.; Shinoda, K.; Ohde, H.; Tsunoda, K.; Hanazono, G.; Kimura, I.; Yuzawa, M.; Tsubota, K.; Miyake, Y. Transcorneal electrical stimulation of retina to treat longstanding retinal artery occlusion. Graefe’s Arch. Clin. Exp. Ophthalmol. 2007, 245, 1773–1780. [Google Scholar] [CrossRef]
- Naycheva, L.; Schatz, A.; Willmann, G.; Bartz-Schmidt, K.U.; Zrenner, E.; Rock, T.; Gekeler, F. Transcorneal electrical stimulation in patients with retinal artery occlusion: A prospective, randomized, sham-controlled pilot study. Ophthalmol. Ther. 2013, 2, 25–39. [Google Scholar] [CrossRef]
- Morimoto, T.; Miyoshi, T.; Matsuda, S.; Tano, Y.; Fujikado, T.; Fukuda, Y. Transcorneal electrical stimulation rescues axotomized retinal ganglion cells by activating endogenous retinal IGF-1 system. Investig. Ophthalmol. Vis. Sci. 2005, 46, 2147–2155. [Google Scholar] [CrossRef]
- Ni, Y.Q.; Gan, D.K.; Xu, H.D.; Xu, G.Z.; Da, C.D. Neuroprotective effect of transcorneal electrical stimulation on light-induced photoreceptor degeneration. Exp. Neurol. 2009, 219, 439–452. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Fujikado, T.; Lee, T.S.; Tano, Y. Direct effect of electrical stimulation on induction of brain-derived neurotrophic factor from cultured retinal Muller cells. Investig. Ophthalmol. Vis. Sci. 2008, 49, 4641–4646. [Google Scholar] [CrossRef] [PubMed]
- Sato, T.; Fujikado, T.; Morimoto, T.; Matsushita, K.; Harada, T.; Tano, Y. Effect of electrical stimulation on IGF-1 transcription by L-type calcium channels in cultured retinal Muller cells. Jpn. J. Ophthalmol. 2008, 52, 217–223. [Google Scholar] [CrossRef]
- Shimazu, K.; Miyake, Y.; Watanabe, S. Retinal ganglion cell response properties in the transcorneal electrically evoked response of the visual system. Vis. Res. 1999, 39, 2251–2260. [Google Scholar] [CrossRef]
- Morimoto, T.; Fukui, T.; Matsushita, K.; Okawa, Y.; Shimojyo, H.; Kusaka, S.; Tano, Y.; Fujikado, T. Evaluation of residual retinal function by pupillary constrictions and phosphenes using transcorneal electrical stimulation in patients with retinal degeneration. Graefe’s Arch. Clin. Exp. Ophthalmol. 2006, 244, 1283–1292. [Google Scholar] [CrossRef]
- Miura, G.; Sugawara, T.; Kawasaki, Y.; Tatsumi, T.; Nizawa, T.; Baba, T.; Hanaoka, H.; Yamamoto, S. Clinical Trial to Evaluate Safety and Efficacy of Transdermal Electrical Stimulation on Visual Functions of Patients with Retinitis Pigmentosa. Sci. Rep. 2019, 9, 11668. [Google Scholar] [CrossRef]
- Kurimoto, T.; Ueda, K.; Mori, S.; Sakamoto, M.; Yamada-Nakanishi, Y.; Matsumiya, W.; Nakamura, M. A study protocol for evaluating the efficacy and safety of skin electrical stimulation for Leber hereditary optic neuropathy: A single-arm, open-label, non-randomized prospective exploratory study. Clin. Ophthalmol. 2019, 13, 897–904. [Google Scholar] [CrossRef]
- International Council of Ophthalmology. Visual standards—Aspects and Ranges of Vision Loss with emphasis on Population Surveys. In Proceedings of the 29th International Congress of Ophthalmology, Sydney, Australia, 20 April 2002.
- Ueda, K.; Mori, S.; Sakamoto, M.; Keshi, Y.; Kurimoto, T.; Yamada, Y.; Nakamura, M. Evaluation of central scotoma based on stimulus size of the visual field test in patients with Leber hereditary optic neuropathy. Neuro-Ophthalmol. Jpn. 2018, 35, 303–308. [Google Scholar]
- Nakamura, M.; Ishikawa, K.; Nagai, T.; Negi, A. Receiver-operating characteristic analysis of multifocal VEPs to diagnose and quantify glaucomatous functional damage. Doc. Ophthalmol. 2011, 123, 93–108. [Google Scholar] [CrossRef]
- Inoue, Y.; Kato, K.; Kamata, S.; Ishikawa, K.; Nakamura, M. Reproducibility in the global indices for multifocal visual evoked potentials and Humphrey visual fields in controls and glaucomatous eyes within a 2-year period. Doc. Ophthalmol. 2015, 131, 115–124. [Google Scholar] [CrossRef]
- Nakamura, M.; Mimura, O.; Wakakura, M.; Inatani, M.; Nakazawa, T.; Shiraga, F. Designation criteria for Leber’s hereditary optic neuropathy. Nippon Ganka Gakkai Zasshi 2015, 119, 339–346. [Google Scholar] [PubMed]
- Carelli, V.; Ross-Cisneros, F.N.; Sadun, A.A. Mitochondrial dysfunction as a cause of optic neuropathies. Prog. Retin. Eye Res. 2004, 23, 53–89. [Google Scholar] [CrossRef] [PubMed]
- Stone, E.M.; Newman, N.J.; Miller, N.R.; Johns, D.R.; Lott, M.T.; Wallace, D.C. Visual recovery in patients with Leber’s hereditary optic neuropathy and the 11778 mutation. J. Clin. Neuroophthalmol. 1992, 12, 10–14. [Google Scholar] [PubMed]
- Wan, X.; Pei, H.; Zhao, M.J.; Yang, S.; Hu, W.K.; He, H.; Ma, S.Q.; Zhang, G.; Dong, X.Y.; Chen, C.; et al. Efficacy and Safety of rAAV2-ND4 Treatment for Leber’s Hereditary Optic Neuropathy. Sci. Rep. 2016, 6, 21587. [Google Scholar] [CrossRef] [PubMed]
- Bouquet, C.; Vignal Clermont, C.; Galy, A.; Fitoussi, S.; Blouin, L.; Munk, M.R.; Valero, S.; Meunier, S.; Katz, B.; Sahel, J.A.; et al. Immune Response and Intraocular Inflammation in Patients With Leber Hereditary Optic Neuropathy Treated With Intravitreal Injection of Recombinant Adeno-Associated Virus 2 Carrying the ND4 Gene: A Secondary Analysis of a Phase 1/2 Clinical Trial. JAMA Ophthalmol. 2019, 137, 399–406. [Google Scholar] [CrossRef]
- Martinelli, D.; Catteruccia, M.; Piemonte, F.; Pastore, A.; Tozzi, G.; Dionisi-Vici, C.; Pontrelli, G.; Corsetti, T.; Livadiotti, S.; Kheifets, V.; et al. EPI-743 reverses the progression of the pediatric mitochondrial disease--genetically defined Leigh Syndrome. Mol. Genet. Metab. 2012, 107, 383–388. [Google Scholar] [CrossRef]
- Shrader, W.D.; Amagata, A.; Barnes, A.; Enns, G.M.; Hinman, A.; Jankowski, O.; Kheifets, V.; Komatsuzaki, R.; Lee, E.; Mollard, P.; et al. alpha-Tocotrienol quinone modulates oxidative stress response and the biochemistry of aging. Bioorg. Med. Chem. Lett. 2011, 21, 3693–3698. [Google Scholar] [CrossRef]
- Mashima, Y.; Kigasawa, K.; Shinoda, K.; Wakakura, M.; Oguchi, Y. Visual prognosis better in eyes with less severe reduction of visual acuity one year after onset of Leber hereditary optic neuropathy caused by the 11,778 mutation. BMC Ophthalmol. 2017, 17, 192. [Google Scholar] [CrossRef]
- Moon, Y.; Kim, U.S.; Han, J.; Ahn, H.; Lim, H.T. Clinical and Optic Disc Characteristics of Patients Showing Visual Recovery in Leber Hereditary Optic Neuropathy. J. Neuroophthalmol. 2020, 40, 15–21. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, X.; Yuan, J.; Tian, Z.; Liu, H.; Wang, D.; Li, B. Prognostic factors for visual acuity in patients with Leber’s hereditary optic neuropathy after rAAV2-ND4 gene therapy. Clin. Exp. Ophthalmol. 2019, 47, 774–778. [Google Scholar] [CrossRef]
- Ota, Y.; Ozeki, N.; Yuki, K.; Shiba, D.; Kimura, I.; Tsunoda, K.; Shinoda, K.; Ohde, H.; Tsubota, K. The Efficacy of Transcorneal Electrical Stimulation for the Treatment of Primary Open-angle Glaucoma: A Pilot Study. Keio J. Med. 2018, 67, 45–53. [Google Scholar] [CrossRef] [PubMed]
- Gall, C.; Schmidt, S.; Schittkowski, M.P.; Antal, A.; Ambrus, G.G.; Paulus, W.; Dannhauer, M.; Michalik, R.; Mante, A.; Bola, M.; et al. Alternating Current Stimulation for Vision Restoration after Optic Nerve Damage: A Randomized Clinical Trial. PLoS ONE. 2016, 11, e0156134. [Google Scholar] [CrossRef] [PubMed]
- Sabel, B.A.; Fedorov, A.B.; Naue, N.; Borrmann, A.; Herrmann, C.; Gall, C. Non-invasive alternating current stimulation improves vision in optic neuropathy. Restor. Neurol. Neurosci. 2011, 29, 493–505. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Youle, R.J. The role of mitochondria in apoptosis *. Annu. Rev. Genet. 2009, 43, 95–118. [Google Scholar] [CrossRef] [PubMed]
- Annex, B.H.; Kraus, W.E.; Dohm, G.L.; Williams, R.S. Mitochondrial biogenesis in striated muscles: Rapid induction of citrate synthase mRNA by nerve stimulation. Am. J. Physiol. 1991, 260, C266–C270. [Google Scholar] [CrossRef] [PubMed]
- Sajic, M.; Mastrolia, V.; Lee, C.Y.; Trigo, D.; Sadeghian, M.; Mosley, A.J.; Gregson, N.A.; Duchen, M.R.; Smith, K.J. Impulse conduction increases mitochondrial transport in adult mammalian peripheral nerves in vivo. PLoS Biol. 2013, 11, e1001754. [Google Scholar] [CrossRef]
- Markham, A.; Cameron, I.; Bains, R.; Franklin, P.; Kiss, J.P.; Schwendimann, L.; Gressens, P.; Spedding, M. Brain-derived neurotrophic factor-mediated effects on mitochondrial respiratory coupling and neuroprotection share the same molecular signalling pathways. Eur. J. Neurosci. 2012, 35, 366–374. [Google Scholar] [CrossRef]
- Schatz, A.; Pach, J.; Gosheva, M.; Naycheva, L.; Willmann, G.; Wilhelm, B.; Peters, T.; Bartz-Schmidt, K.U.; Zrenner, E.; Messias, A.; et al. Transcorneal electrical stimulation for patients with retinitis pigmentosa: A prospective, randomized, sham-controlled follow-up study over 1 year. Investig. Ophthalmol. Vis. Sci. 2017, 58, 257–269. [Google Scholar] [CrossRef]
- Morimoto, T.; Miyoshi, T.; Sawai, H.; Fujikado, T. Optimal parameters of transcorneal electrical stimulation (TES) to be neuroprotective of axotomized RGCs in adult rats. Exp. Eye Res. 2010, 90, 285–291. [Google Scholar] [CrossRef]
- Tagami, Y.; Kurimoto, T.; Miyoshi, T.; Morimoto, T.; Sawai, H.; Mimura, O. Axonal regeneration induced by repetitive electrical stimulation of crushed optic nerve in adult rats. Jpn. J. Ophthalmol. 2009, 53, 257–266. [Google Scholar] [CrossRef]



| Inclusion Criteria |
| Aged ≥ 16 and < 80 years (males and females) |
| More than 8 months without visual improvement |
| Mutation of mt DNA at the position 11,778 |
| Best-corrected decimal visual acuity <0.1 |
| Exclusion Criteria |
| A history of smoking within past 6 months |
| Implanted electronic device such as cardiac pacemaker etc. |
| Intraocular surgery within the past 1 year |
| A history of eye diseases other than early-stage cataract and artificial intraocular lens |
| Idebenone treatment within the last year |
| Participants on any of the following drugs: ethambutol, chloramphenicol, linezolid, erythromycin, streptomycin, antiretroviral drugs, amiodarone, infliximab, clioquinol, dapsone, quinine, pheniprazine, suramin sodium, or isoniazid |
| A history of epilepsy |
| Current pregnancy |
| Severe allergic diseases, including atopic dermatitis |
| Currently participating in other clinical studies |
| Participants judged inappropriate for other reasons by responsible doctors |
| Parameters | Baseline |
|---|---|
| Number of cases/eyes | 10/10 |
| Age at enrollment (years) | 37.6 ± 17.2 |
| Male/Female | 10/0 |
| Age at onset (years) | 25.0 ± 12.9 |
| Intervals from onset to SES (months) | 154 ± 135 |
| LogMAR BCVA | 1.80 (1.70–1.80) |
| Critical flicker frequency (Hz) | 29.1 ± 13.3 |
| Ganglion cell complex thickness (μm) | 56.6 ± 4.0 |
| cpRNFL thickness (μm) | 65.6 ± 18.1 |
| Corneal endothelial cell density (/mm2) | 2855 ± 272 |
| SNR-AUC in all 60 sectors | 0.54 (0.51–0.60) |
| SNR-AUC in central 36 sectors | 0.57 (0.55–0.60) |
| Case | LogMAR BCVA | CFF | Summed Actual Sensitivity (dB) |
|---|---|---|---|
| 1 | 1.90 → 1.80 | NR | ↓↓ |
| 2 | 1.80 → 1.70 | ↑ | → |
| 3 | 1.80 → 1.80 | ↓ | ↑↑ |
| 4 | 1.40 → 1.15 | → | → |
| 5 | 1.70 → 1.52 | → | ↑ |
| 6 | 1.70 → 1.40 | ↑ | → |
| 7 | 1.80 → 1.80 | → | ↑ |
| 8 | 1.70 → 1.70 | → | ↑↑ |
| 9 | 1.80 → 1.80 | → | ↓↓ |
| 10 | 1.80 → 1.80 | → | ↑↑ |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kurimoto, T.; Ueda, K.; Mori, S.; Kamada, S.; Sakamoto, M.; Yamada-Nakanishi, Y.; Matsumiya, W.; Nakamura, M. A Single-Arm, Prospective, Exploratory Study to Preliminarily Test Effectiveness and Safety of Skin Electrical Stimulation for Leber Hereditary Optic Neuropathy. J. Clin. Med. 2020, 9, 1359. https://doi.org/10.3390/jcm9051359
Kurimoto T, Ueda K, Mori S, Kamada S, Sakamoto M, Yamada-Nakanishi Y, Matsumiya W, Nakamura M. A Single-Arm, Prospective, Exploratory Study to Preliminarily Test Effectiveness and Safety of Skin Electrical Stimulation for Leber Hereditary Optic Neuropathy. Journal of Clinical Medicine. 2020; 9(5):1359. https://doi.org/10.3390/jcm9051359
Chicago/Turabian StyleKurimoto, Takuji, Kaori Ueda, Sotaro Mori, Seiko Kamada, Mari Sakamoto, Yuko Yamada-Nakanishi, Wataru Matsumiya, and Makoto Nakamura. 2020. "A Single-Arm, Prospective, Exploratory Study to Preliminarily Test Effectiveness and Safety of Skin Electrical Stimulation for Leber Hereditary Optic Neuropathy" Journal of Clinical Medicine 9, no. 5: 1359. https://doi.org/10.3390/jcm9051359
APA StyleKurimoto, T., Ueda, K., Mori, S., Kamada, S., Sakamoto, M., Yamada-Nakanishi, Y., Matsumiya, W., & Nakamura, M. (2020). A Single-Arm, Prospective, Exploratory Study to Preliminarily Test Effectiveness and Safety of Skin Electrical Stimulation for Leber Hereditary Optic Neuropathy. Journal of Clinical Medicine, 9(5), 1359. https://doi.org/10.3390/jcm9051359





