Questionnaire on Perception of Threat from COVID-19
Abstract
1. Introduction
Perceived Threat from COVID-19
2. Method
2.1. Participants
2.2. Instruments
2.3. Procedure
2.4. Data Analysis
3. Results
3.1. Preliminary Analyses
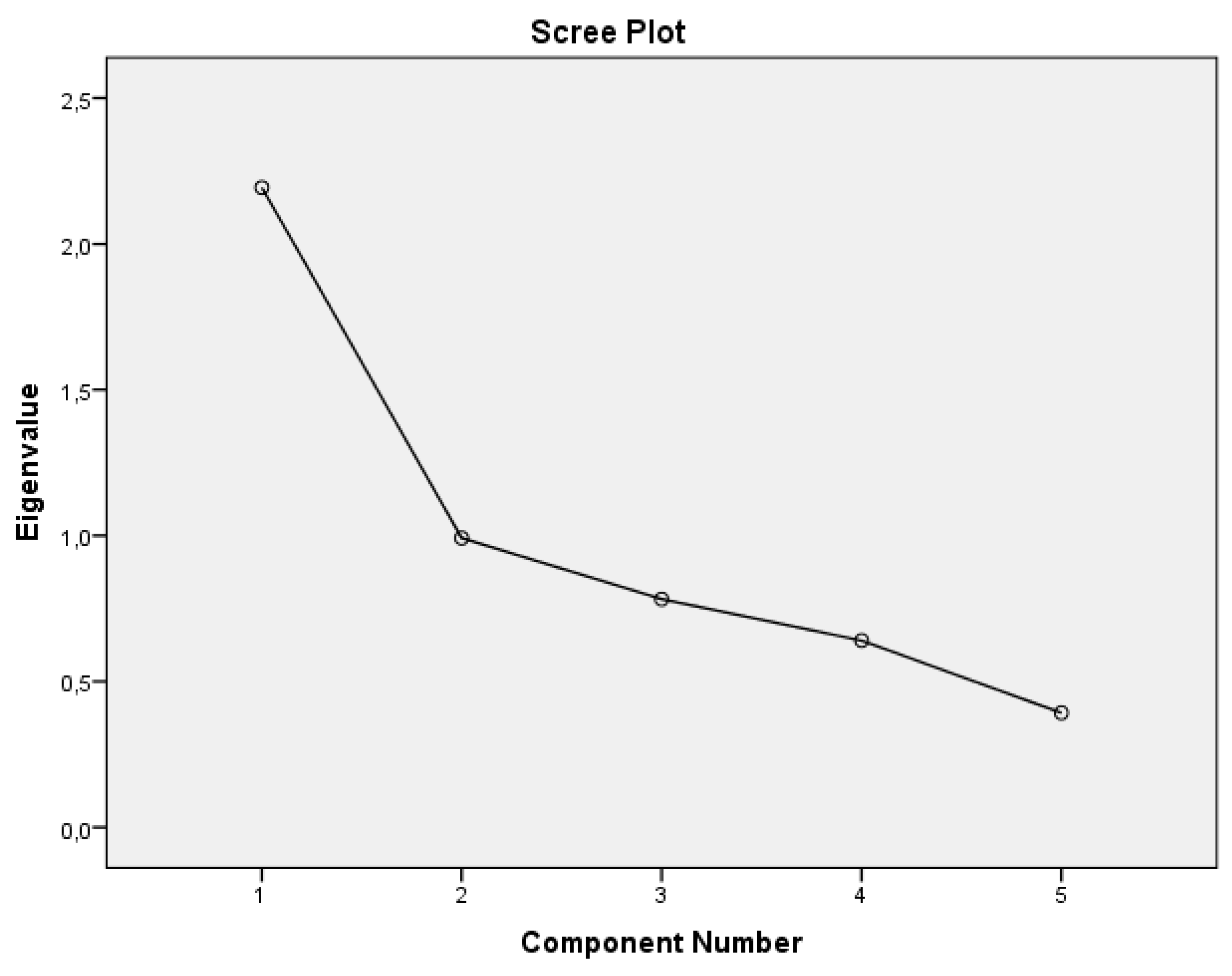
3.2. Exploratory Factor Analysis of the Original BIP-Q5 Model
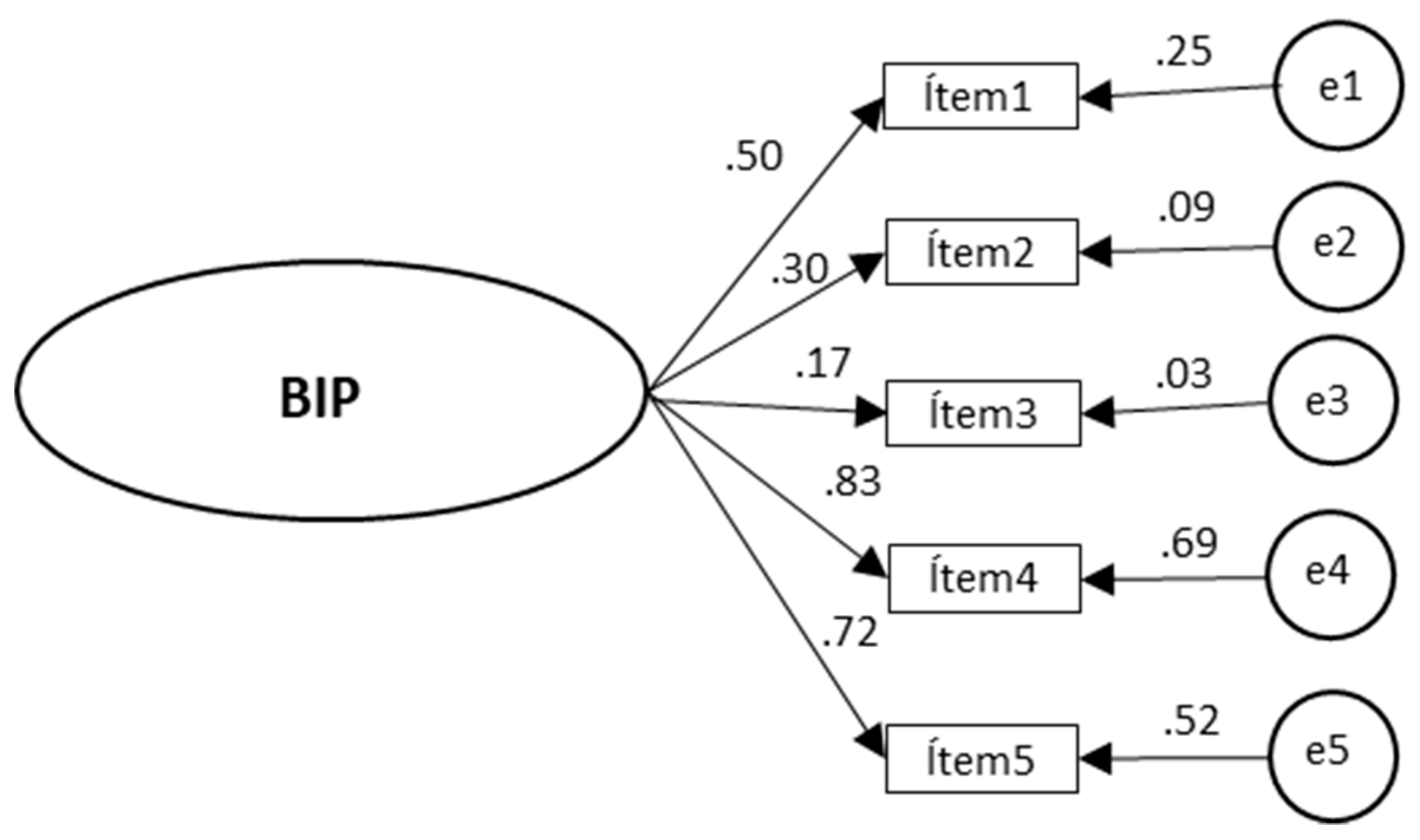
3.3. Confirmatory Factor Analysis of the BIP-Q5 Model for COVID-19
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Lai, C.C.; Shih, T.P.; Ko, W.C.; Tang, H.J.; Hsueh, P.R. Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) and coronavirus disease-2019 (COVID-19): The epidemic and the challenges. Int. J. Antimicrob. Agents 2020, 55, 105924. [Google Scholar] [CrossRef] [PubMed]
- Lake, M.A. What we know so far: COVID19 current clinical knowledge and research. Clin. Med. 2020, 20, 124–127. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.S.; Zhang, C. What to do next to control the 2019-nCoV epidemic? Lancet 2020, 395, 391–393. [Google Scholar] [CrossRef]
- Decaro, N.; Lorusso, A. Novel human coronavirus (SARS-CoV-2): A lesson from animal coronaviruses. Vet. Microbiol. 2020, 244, 108693. [Google Scholar] [CrossRef]
- European Centre for Disease Prevention and Control An Agency of the European Union. Situation Update Worldwide, as of 19 April 2020. Available online: https://www.ecdc.europa.eu/en/geographical-distribution-2019-ncov-cases (accessed on 19 April 2020).
- World Health Organization. Coronavirus Disease (COVID-19) Pandemic. Available online: https://www.who.int/emergencies/diseases/novel-coronavirus-2019 (accessed on 31 March 2020).
- Rabi, F.A.; Al Zoubi, M.S.; Kasasbeh, G.A.; Salameh, D.M.; Al-Nasser, A.D. SARS-CoV-2 and Coronavirus Disease 2019: What we know so far. Pathogens 2020, 9, 231. [Google Scholar] [CrossRef]
- Rodríguez-Morales, A.J.; MacGregor, K.; Kanagarajh, S.; Patel, D.; Schlagenhauf, P. Going Global- Travel and the 2019 Novel Coronavirus. Trop. Med. Infect. Dis. 2020, 33, 101578. [Google Scholar] [CrossRef]
- Ho, C.S.; Chee, C.Y.; Ho, R.C. Mental Health strategies to combat the psychological impact of COVID-19 beyond paranoia and panic. Ann. Acad. Med. Singap. 2020, 49, 1–3. [Google Scholar]
- Hernández, B.C.; Rugarcía, Y.T. Attitudes toward the risk prevention in health professionals in cases of epidemiological alert. Med. Segur. Trab. 2015, 61, 254–272. [Google Scholar]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors Associated With Mental Health Outcomes Among Health Care Workers Exposed to Coronavirus Disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Broadbent, E.; Wilkes, C.; Koschwanez, H.; Weinman, J.; Norton, S.; Petrie, K.J. A systematic review and meta-analysis of the Brief Illness Perception Questionnaire. Psychol. Health 2015, 30, 1361–1385. [Google Scholar] [CrossRef]
- Johnson, J.; Hall, L.H.; Berzins, K.; Baker, J.; Melling, K.; Thompson, C. Mental healthcare staff well-being and burnout: A narrative review of trends, causes, implications, and recommendations for future interventions. Int. J. Ment. Health Nurs. 2018, 27, 20–32. [Google Scholar] [CrossRef] [PubMed]
- Molero, M.M.; Pérez-Fuentes, M.C.; Gázquez, J.J.; Simón, M.M.; y Martos, Á. Burnout risk and protection factors in certified nursing aides. Int. J. Environ. Res. Public Health 2018, 15, 1116. [Google Scholar] [CrossRef] [PubMed]
- Beléndez, M.; Bermejo, R.M.; García-Ayala, M.D. Estructura factorial de la versión española del Revised Illness Perception Questionnaire en una muestra de hipertensos. Psicothema 2005, 17, 318–324. [Google Scholar]
- Broadbent, E.; Petrie, K.J.; Main, J.; Weinman, J. The brief illness perception questionnaire. J. Psychosom. Res. 2006, 60, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Moss-Morris, R.; Weinman, J.; Petrie, K.; Home, R.; Cameron, L.; Buick, D. The revised illness perception questionnaire (IPQ-R). Psychol. Health 2002, 17, 1–16. [Google Scholar] [CrossRef]
- Taylor, S. Psicología de la Salud, 6th ed.; McGraw-Hill: New York, NY, USA, 2007. [Google Scholar]
- Lloyd, K.R.; Jacob, K.S.; Patel, V.; Louis, L.S.; Bhugra, D.; Mann, A.H. The development of the Short Explanatory Model Interview (SEMI) and its use among primary-care attenders with common mental disorders. Psychol. Med. 1998, 28, 1231–1237. [Google Scholar] [CrossRef]
- Rüdell, K.; Bhui, K.; Priebe, S. Concept, development and application of a new mixed method assessment of cultural variations in illness perceptions barts explanatory model inventory. J. Health Psychol. 2009, 14, 336–347. [Google Scholar] [CrossRef]
- Quiceno, J.M.; Vinaccia, S. Percepción de enfermedad: Una aproximación a partir del Illness Perception Questionnaire [Illness perception: An approximation from the Illness Perception Questionnaire]. Psicol. Caribe 2010, 25, 56–83. [Google Scholar]
- Karataş, T.; Özen, Ş.; Kutlutürkan, S. Factor structure and psychometric properties of the brief illness perception questionnaire in Turkish cancer patients. Asia Pac. J. Oncol. Nurs. 2017, 4, 77–83. [Google Scholar]
- Zhang, N.; Fielding, R.; Soong, I.; Chan, K.K.; Lee, C.; Ng, A.; Wing, K.; Janice, T.; Lee, V.; Wendy, W.; et al. Psychometric assessment of the Chinese version of the brief illness perception questionnaire in breast cancer survivors. PLoS ONE 2017, 12, e0174093. [Google Scholar] [CrossRef]
- Valero-Moreno, S.; Lacomba-Trejo, L.; Casaña-Granell, S.; Prado-Gascó, V.J.; Montoya-Castilla, I.; Pérez-Marín, M. Propiedades psicométricas del cuestionario de percepción de amenaza de la enfermedad crónica en pediatría. Rev. Lat. Am. Enferm. 2020, 28, e3242. [Google Scholar] [CrossRef]
- Leventhal, H.; Meyer, D.; Nerenz, D.R. The common sense representation of illness danger. In Contributions to Medical Psychology; Rachman, S., Ed.; Pergamon Press: New York, NY, USA, 1980; pp. 17–30. [Google Scholar]
- Leventhal, H.; Phillips, L.A.; Burns, E. The Common-Sense Model of Self-Regulation (CSM): A dynamic framework for understanding illness self-management. Int. J. Behav. Med. 2016, 39, 935–946. [Google Scholar] [CrossRef] [PubMed]
- Pacheco-Huergo, V.; Viladrich, C.; Pujol-Ribera, E.; Cabezas-Pena, C.; Núnez, M.; Roura-Olmeda, P.; Amado-Guiradoh, E.; Núñez, E.; del Val, J.L. Percepción en enfermedades crónicas: Validación lingüística del Illness Perception Questionnaire Revised y del Brief Illness Perception Questionnaire para la población española. Aten. Prim. 2012, 44, 280–287. [Google Scholar] [CrossRef] [PubMed]
- Chew, B.H.; Vos, R.C.; Heijmans, M.; Shariff-Ghazali, S.; Fernandez, A.; Rutten, G.E. Validity and reliability of a Malay version of the brief illness perception for patients with type 2 diabetes mellitus. BMC Med. Res. Methodol. 2017, 17, 118. [Google Scholar] [CrossRef] [PubMed]
- Leysen, M.; Nijs, J.; Meeus, M.; Van Wilgen, C.P.; Struyf, F.; Vermandel, A.; Kuppens, A.; Roussel, N. Clinimetric properties of illness perception questionnaire revised (IPQ-R) and brief illness perception questionnaire (Brief IPQ) in patients with musculoskeletal disorders: A systematic review. Man. Ther. 2015, 20, 10–17. [Google Scholar] [CrossRef]
- Quiles, Y.; Terol, M.C.; Tirado, S.; Beléndez, M. Estructura factorial de la versión española del “Cuestionario de Percepción de Enfermedad Revisado” (IPQ-R) en pacientes con un trastorno del comportamiento alimentario y sus familiares. Cuad. Med. Psicosom. Psiquiatr. Enlace 2007, 82, 9–22. [Google Scholar]
- Pérez-Fuentes, M.C.; Herrera-Peco, I.; Molero, M.M.; Oropesa, N.F.; Ayuso, D.; Gázquez, J.J. The Development and Validation of the Healthcare Professional Humanization Scale (HUMAS) for Nursing. Int. J. Environ. Res. Public Health 2019, 16, 3999. [Google Scholar] [CrossRef]
- Bentler, P.M. EQS Structural Equations Program Manual; BMDP Statistical Software: Los Angeles, CA, USA, 1989. [Google Scholar]
- McDonald, R.P.; Ho, M.H.R. Principles and practice in reporting structural equation analyses. Psychol. Methods 2002, 7, 64. [Google Scholar] [CrossRef]
- Akaike, H. A new look at the statistical model identification. IEEE Trans. Automat. Control 1974, 19, 716–723. [Google Scholar] [CrossRef]
- Cronbach, L.J. Coefficient alpha and the internal structure of tests. Psychometrika 1951, 16, 297–334. [Google Scholar] [CrossRef]
- Byrne, B.M.; Stewart, S.M. The MACS approach to testing for multigroup invariance of a second-order structure: A walk through the process. Struct. Equ. Model. 2006, 13, 287–321. [Google Scholar] [CrossRef]
- Cheung, G.W.; Rensvold, R.B. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct. Equ. Model. 2002, 9, 233–255. [Google Scholar] [CrossRef]
- Finney, S.J.; di Stefano, C. Non-normal and categorical data in structural equation modeling. In Structural Equation Modeling: A Second Course; Hancock, G.R., Mueller, R.O., Eds.; Information Age: Greenwich, CT, USA, 2006; pp. 269–314. [Google Scholar]
| Items | n | M | SD | Skewness | Kurtosis | ||
|---|---|---|---|---|---|---|---|
| Statistic | Std. Error | Statistic | Std. Error | ||||
| BIP-Q5 1 | 505 | 7.66 | 2.11 | −1.27 | 0.11 | 1.75 | 0.22 |
| BIP-Q5 2 | 505 | 6.95 | 1.68 | −0.65 | 0.11 | 0.61 | 0.22 |
| BIP-Q5 3 | 505 | 2.02 | 1.86 | 2.1 | 0.11 | 3.8 | 0.22 |
| BIP-Q5 4 | 505 | 7.75 | 2.17 | −1.02 | 0.11 | 0.48 | 0.22 |
| BIP-Q5 5 | 505 | 6.61 | 2.39 | −0.51 | 0.11 | −0.52 | 0.22 |
| F1 | h2 | |
|---|---|---|
| Item 1 | 0.618 | 0.383 |
| Item 2 | 0.607 | 0.369 |
| Item 3 | 0.314 | 0.099 |
| Item 4 | 0.817 | 0.667 |
| Item 5 | 0.822 | 0.676 |
| Percentage explained variance | 43.87 | |
| Kaiser–Meyer–Olkin | 0.71 | |
| Barlett’s sphericity | χ2(10) = 426.320, p < 0.000 | |
| Cronbach’s alpha | 0.663 |
| Model | CFI | TLI | RMSEA | ||||
|---|---|---|---|---|---|---|---|
| χ2 (df) | χ2/df | RMSEA | CI 90% | ||||
| Lower. | Upper | ||||||
| One-factor model of the BIP-Q5 | 10.2 (5) | 2.1 | 0.988 | 0.975 | 0.045 | 0.000 | 0.085 |
| Two-factor model of the BIP-Q5 | 9.999 (4) | 2.49 | 0.986 | 0.964 | 0.055 | 0.010 | 0.098 |
| Model | χ2 | df | χ2 / df | Δχ2 | CFI | ΔCFI | IFI | RMSEA (CI 90%) |
|---|---|---|---|---|---|---|---|---|
| M0a (male) | 29.129 (p = 0.001) | 10 | 2.912 | 0.976 | 0.976 | 0.044 (0.026–0.063) | ||
| M0b (female) | 29.129 (p = 0.001) | 10 | 2.912 | 0.976 | 0.976 | 0.044 (0.026–0.063) | ||
| M1 (base model set) | 29.129 (p = 0.001) | 10 | 2.912 | 0.976 | 0.976 | 0.044 (0.026–0.063) | ||
| M2 (FS) | 34.822 (p = 0.002) | 14 | 2.487 | 0.424 | 0.973 | 0.003 | 0.974 | 0.039 (0.023–0.055) |
| M3 (FS + Int) | 65.620 (p = 0.000) | 19 | 3.453 | 0.966 | 0.940 | 0.033 | 0.940 | 0.050 (0.037–0.063) |
| M4 (FS + Int + Err) | 76.002 (p = 0.000) | 25 | 3.041 | 0.412 | 0.935 | 0.005 | 0.934 | 0.045 (0.034–0.057) |
| General | Male | Female | ||
|---|---|---|---|---|
| M | 30.74 | 29.22 | 31.48 | |
| SD | 6.63 | 7.03 | 6.29 | |
| Min | 8 | 8 | 11 | |
| Max. | 50 | 50 | 48 | |
| Percentiles | 10 | 21 | 20 | 23 |
| 20 | 25 | 23 | 26 | |
| 30 | 28 | 27 | 29 | |
| 40 | 30 | 28 | 30 | |
| 50 | 31.5 | 30 | 32 | |
| 60 | 33 | 32 | 34 | |
| 70 | 34 | 33 | 35 | |
| 80 | 36 | 35 | 37 | |
| 90 | 38 | 37 | 39 | |
| 95 | 40 | 39 | 41 | |
| 99 | 45 | 43.66 | 45 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pérez-Fuentes, M.d.C.; Molero Jurado, M.d.M.; Oropesa Ruiz, N.F.; Martos Martínez, Á.; Simón Márquez, M.d.M.; Herrera-Peco, I.; Gázquez Linares, J.J. Questionnaire on Perception of Threat from COVID-19. J. Clin. Med. 2020, 9, 1196. https://doi.org/10.3390/jcm9041196
Pérez-Fuentes MdC, Molero Jurado MdM, Oropesa Ruiz NF, Martos Martínez Á, Simón Márquez MdM, Herrera-Peco I, Gázquez Linares JJ. Questionnaire on Perception of Threat from COVID-19. Journal of Clinical Medicine. 2020; 9(4):1196. https://doi.org/10.3390/jcm9041196
Chicago/Turabian StylePérez-Fuentes, María del Carmen, María del Mar Molero Jurado, Nieves Fátima Oropesa Ruiz, África Martos Martínez, María del Mar Simón Márquez, Iván Herrera-Peco, and José Jesús Gázquez Linares. 2020. "Questionnaire on Perception of Threat from COVID-19" Journal of Clinical Medicine 9, no. 4: 1196. https://doi.org/10.3390/jcm9041196
APA StylePérez-Fuentes, M. d. C., Molero Jurado, M. d. M., Oropesa Ruiz, N. F., Martos Martínez, Á., Simón Márquez, M. d. M., Herrera-Peco, I., & Gázquez Linares, J. J. (2020). Questionnaire on Perception of Threat from COVID-19. Journal of Clinical Medicine, 9(4), 1196. https://doi.org/10.3390/jcm9041196











