Antithrombotic Strategies in Patients with Atrial Fibrillation Following Percutaneous Coronary Intervention: A Systemic Review and Network Meta-Analysis of Randomized Controlled Trials
Abstract
1. Introduction
2. Method
2.1. Study Selection, Search Strategy and Outcome Measures
2.2. Statistical Analysis and Risk of Bias
3. Results
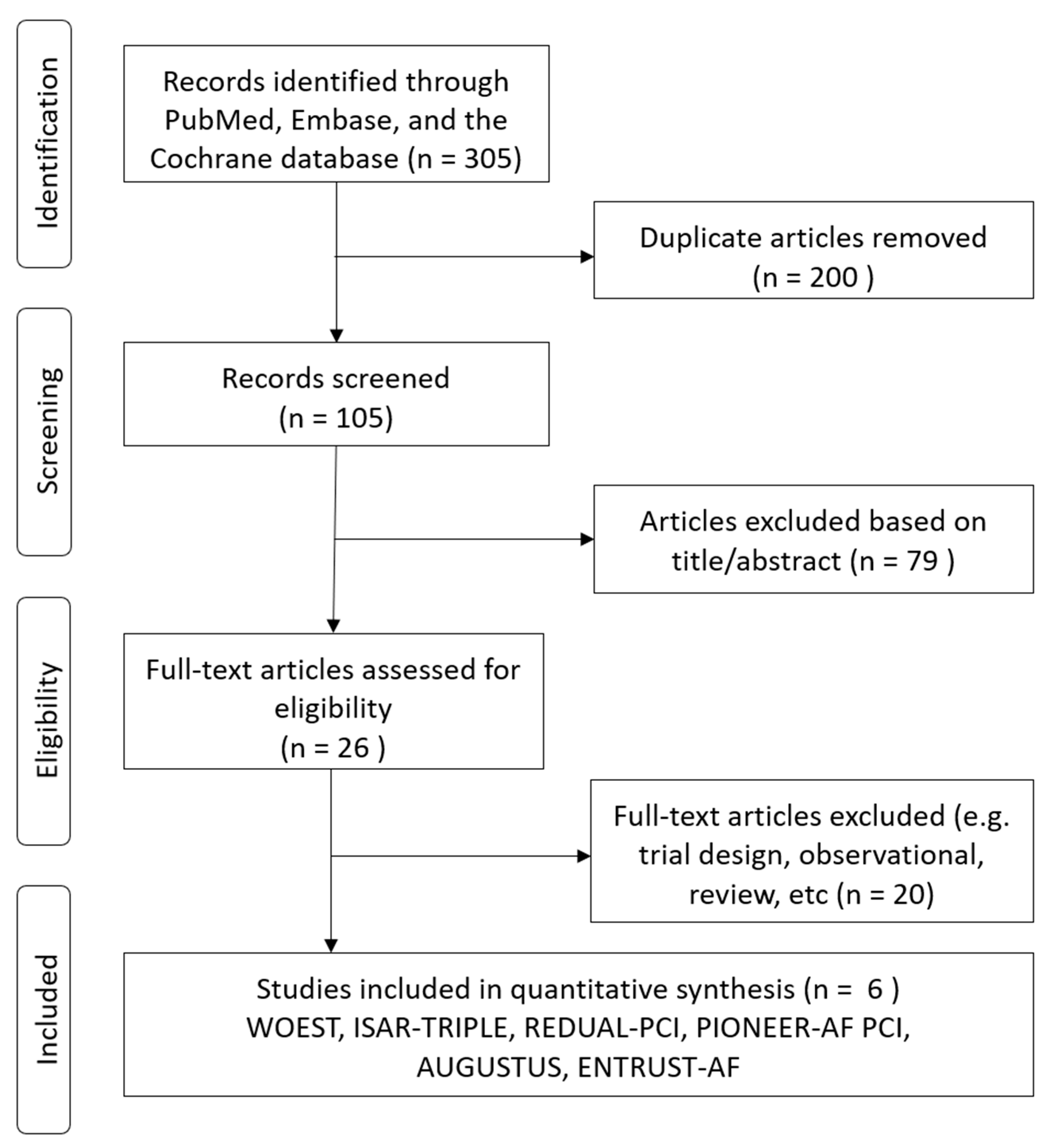
3.1. Enrollment of Studies
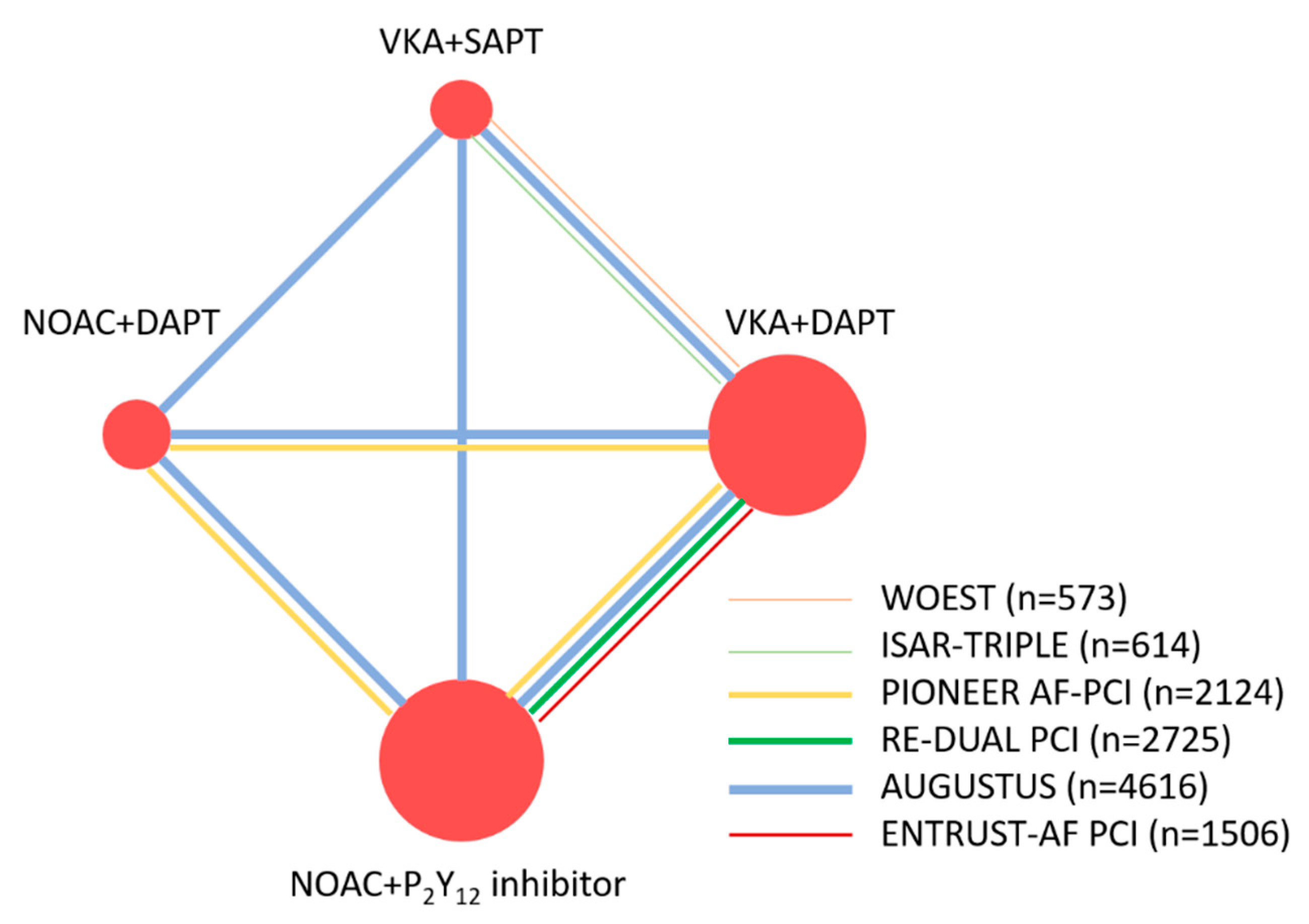
3.2. Structure of the Network Meta-Analysis
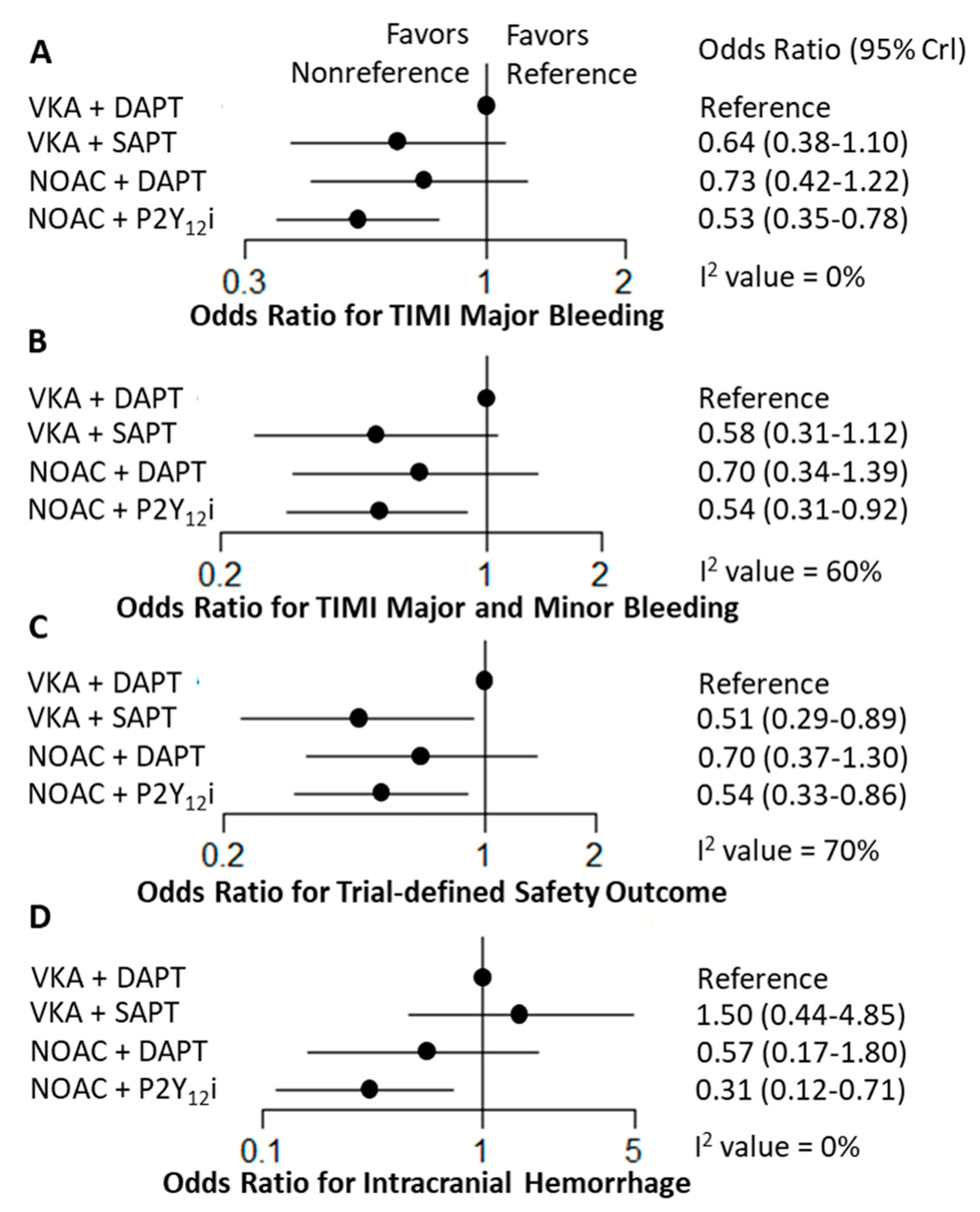
3.3. Network Meta-Analysis Safety Outcomes
3.4. Network Meta-Analysis for Efficacy Outcomes
4. Discussion
4.1. Dual Versus Triple Antithrombotic Therapy
4.2. Dual Antithrombotic Therapy with NOAC or VKA and P2Y12 Inhibitors
4.3. Previous and Present Meta-Analyses
4.4. Clinical Implication
5. Limitation
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Kralev, S.; Schneider, K.; Lang, S.; Suselbeck, T.; Borggrefe, M. Incidence and severity of coronary artery disease in patients with atrial fibrillation undergoing first-time coronary angiography. PLoS ONE 2011, 6, e24964. [Google Scholar] [CrossRef] [PubMed]
- January, C.T.; Wann, L.S.; Calkins, H.; Chen, L.Y.; Cigarroa, J.E.; Cleveland, J.C., Jr.; Ellinor, P.T.; Ezekowitz, M.D.; Field, M.E.; Furie, K.L.; et al. 2019 AHA/ACC/HRS Focused Update of the 2014 AHA/ACC/HRS Guideline for the Management of Patients With Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. J. Am. Coll. Cardiol. 2019, 74, 104–132. [Google Scholar] [CrossRef] [PubMed]
- Steffel, J.; Verhamme, P.; Potpara, T.S.; Albaladejo, P.; Antz, M.; Desteghe, L.; Haeusler, K.G.; Oldgren, J.; Reinecke, H.; Roldan-Schilling, V.; et al. The 2018 European Heart Rhythm Association Practical Guide on the use of non-vitamin K antagonist oral anticoagulants in patients with atrial fibrillation. Eur. Heart J. 2018, 39, 1330–1393. [Google Scholar] [CrossRef] [PubMed]
- Neumann, F.J.; Sousa-Uva, M. Ten Commandments’ for the 2018 ESC/EACTS Guidelines on Myocardial Revascularization. Eur. Heart J. 2018, 39, 3759. [Google Scholar] [CrossRef] [PubMed]
- Levine, G.N.; Bates, E.R.; Blankenship, J.C.; Bailey, S.R.; Bittl, J.A.; Cercek, B.; Chambers, C.E.; Ellis, S.G.; Guyton, R.A.; Hollenberg, S.M.; et al. 2015 ACC/AHA/SCAI Focused Update on Primary Percutaneous Coronary Intervention for Patients With ST-Elevation Myocardial Infarction: An Update of the 2011 ACCF/AHA/SCAI Guideline for Percutaneous Coronary Intervention and the 2013 ACCF/AHA Guideline for the Management of ST-Elevation Myocardial Infarction: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 2016, 133, 1135–1147. [Google Scholar] [CrossRef]
- Paikin, J.S.; Wright, D.S.; Crowther, M.A.; Mehta, S.R.; Eikelboom, J.W. Triple antithrombotic therapy in patients with atrial fibrillation and coronary artery stents. Circulation 2010, 121, 2067–2070. [Google Scholar] [CrossRef]
- Holmes, D.R., Jr.; Kereiakes, D.J.; Kleiman, N.S.; Moliterno, D.J.; Patti, G.; Grines, C.L. Combining antiplatelet and anticoagulant therapies. J. Am. Coll. Cardiol. 2009, 54, 95–109. [Google Scholar] [CrossRef]
- Fiedler, K.A.; Maeng, M.; Mehilli, J.; Schulz-Schupke, S.; Byrne, R.A.; Sibbing, D.; Hoppmann, P.; Schneider, S.; Fusaro, M.; Ott, I.; et al. Duration of Triple Therapy in Patients Requiring Oral Anticoagulation After Drug-Eluting Stent Implantation: The ISAR-TRIPLE Trial. J. Am. Coll. Cardiol. 2015, 65, 1619–1629. [Google Scholar] [CrossRef]
- Dewilde, W.J.; Oirbans, T.; Verheugt, F.W.; Kelder, J.C.; De Smet, B.J.; Herrman, J.P.; Adriaenssens, T.; Vrolix, M.; Heestermans, A.A.; Vis, M.M.; et al. Use of clopidogrel with or without aspirin in patients taking oral anticoagulant therapy and undergoing percutaneous coronary intervention: An open-label, randomised, controlled trial. Lancet 2013, 381, 1107–1115. [Google Scholar] [CrossRef]
- Gibson, C.M.; Mehran, R.; Bode, C.; Halperin, J.; Verheugt, F.W.; Wildgoose, P.; Birmingham, M.; Ianus, J.; Burton, P.; van Eickels, M.; et al. Prevention of Bleeding in Patients with Atrial Fibrillation Undergoing PCI. N. Engl. J. Med. 2016, 375, 2423–2434. [Google Scholar] [CrossRef]
- Cannon, C.P.; Bhatt, D.L.; Oldgren, J.; Lip, G.Y.H.; Ellis, S.G.; Kimura, T.; Maeng, M.; Merkely, B.; Zeymer, U.; Gropper, S.; et al. Dual Antithrombotic Therapy with Dabigatran after PCI in Atrial Fibrillation. N. Engl. J. Med. 2017, 377, 1513–1524. [Google Scholar] [CrossRef] [PubMed]
- Lopes, R.D.; Heizer, G.; Aronson, R.; Vora, A.N.; Massaro, T.; Mehran, R.; Goodman, S.G.; Windecker, S.; Darius, H.; Li, J.; et al. Antithrombotic Therapy after Acute Coronary Syndrome or PCI in Atrial Fibrillation. N. Engl. J. Med. 2019, 380, 1509–1524. [Google Scholar] [CrossRef] [PubMed]
- Lopes, R.D.; Hong, H.; Harskamp, R.E.; Bhatt, D.L.; Mehran, R.; Cannon, C.P.; Granger, C.B.; Verheugt, F.W.A.; Li, J.; Ten Berg, J.M.; et al. Safety and Efficacy of Antithrombotic Strategies in Patients With Atrial Fibrillation Undergoing Percutaneous Coronary Intervention: A Network Meta-analysis of Randomized Controlled Trials. JAMA Cardiol. 2019. [Google Scholar] [CrossRef] [PubMed]
- Golwala, H.B.; Cannon, C.P.; Steg, P.G.; Doros, G.; Qamar, A.; Ellis, S.G.; Oldgren, J.; Ten Berg, J.M.; Kimura, T.; Hohnloser, S.H.; et al. Safety and efficacy of dual vs. triple antithrombotic therapy in patients with atrial fibrillation following percutaneous coronary intervention: A systematic review and meta-analysis of randomized clinical trials. Eur. Heart J. 2018, 39, 1726a–1735a. [Google Scholar] [CrossRef] [PubMed]
- Brunetti, N.D.; Tarantino, N.; De Gennaro, L.; Correale, M.; Santoro, F.; Di Biase, M. Direct oral anticoagulants versus standard triple therapy in atrial fibrillation and PCI: Meta-analysis. Open Heart 2018, 5, e000785. [Google Scholar] [CrossRef]
- Vranckx, P.; Valgimigli, M.; Eckardt, L.; Tijssen, J.; Lewalter, T.; Gargiulo, G.; Batushkin, V.; Campo, G.; Lysak, Z.; Vakaliuk, I.; et al. Edoxaban-based versus vitamin K antagonist-based antithrombotic regimen after successful coronary stenting in patients with atrial fibrillation (ENTRUST-AF PCI): A randomised, open-label, phase 3b trial. Lancet 2019. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA Statement. Open Med. 2009, 3, e123–e130. [Google Scholar]
- Neumann, F.J.; Sousa-Uva, M.; Ahlsson, A.; Alfonso, F.; Banning, A.P.; Benedetto, U.; Byrne, R.A.; Collet, J.P.; Falk, V.; Head, S.J.; et al. 2018 ESC/EACTS Guidelines on myocardial revascularization. Eur. Heart J. 2019, 40, 87–165. [Google Scholar] [CrossRef]
- Chen, J.; Wang, L.Y.; Deng, C.; Jiang, X.H.; Chen, T.G. The safety and efficacy of oral anticoagulants with dual versus single antiplatelet therapy in patients after percutaneous coronary intervention: A meta-analysis. Medicine (Baltim.) 2017, 96, e8015. [Google Scholar] [CrossRef]
- Zhu, W.; Guo, L.; Liu, F.; Wan, R.; Shen, Y.; Lip, G.Y.H.; Hong, K. Efficacy and safety of triple versus dual antithrombotic therapy in atrial fibrillation and ischemic heart disease: A systematic review and meta-analysis. Oncotarget 2017, 8, 81154–81166. [Google Scholar] [CrossRef]
- Gong, X.; Tang, S.; Li, J.; Zhang, X.; Tian, X.; Ma, S. Antithrombotic therapy strategies for atrial fibrillation patients undergoing percutaneous coronary intervention: A systematic review and network meta-analysis. PLoS ONE 2017, 12, e0186449. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, N.; Jain, A.; Mahmoud, A.N.; Bishnoi, R.; Golwala, H.; Karimi, A.; Mojadidi, M.K.; Garg, J.; Gupta, T.; Patel, N.K.; et al. Safety and Efficacy of Dual Versus Triple Antithrombotic Therapy in Patients Undergoing Percutaneous Coronary Intervention. Am. J. Med. 2017, 130, 1280–1289. [Google Scholar] [CrossRef] [PubMed]
- Yu, J.J.; Zou, C.; Liu, W.Y.; Yang, G.P. Dual versus single antiplatelet therapy for patients with long-term oral anticoagulation undergoing coronary intervention: A systematic review and meta-analysis. J. Geriatr. Cardiol. 2017, 14, 725–736. [Google Scholar] [CrossRef] [PubMed]
- Cavallari, I.; Patti, G. Meta-Analysis Comparing the Safety and Efficacy of Dual Versus Triple Antithrombotic Therapy in Patients With Atrial Fibrillation Undergoing Percutaneous Coronary Intervention. Am. J. Cardiol. 2018, 121, 718–724. [Google Scholar] [CrossRef]
- Liu, L.; Huang, J.; Zhang, X.; Tang, X. Efficacy and safety of triple therapy versus dual antiplatelet therapy in patients with atrial fibrillation undergoing coronary stenting: A meta-analysis. PLoS ONE 2018, 13, e0199232. [Google Scholar] [CrossRef]
- Bunmark, W.; Jinatongthai, P.; Vathesatogkit, P.; Thakkinstian, A.; Reid, C.M.; Wongcharoen, W.; Chaiyakunapruk, N.; Nathisuwan, S. Antithrombotic Regimens in Patients With Percutaneous Coronary Intervention Whom an Anticoagulant Is Indicated: A Systematic Review and Network Meta-Analysis. Front. Pharmacol. 2018, 9, 1322. [Google Scholar] [CrossRef]
- Mahmoud, A.N.; Shah, N.H.; Elgendy, I.Y.; Agarwal, N.; Elgendy, A.Y.; Mentias, A.; Barakat, A.F.; Mahtta, D.; David Anderson, R.; Bavry, A.A. Safety and efficacy of second-generation drug-eluting stents compared with bare-metal stents: An updated meta-analysis and regression of 9 randomized clinical trials. Clin. Cardiol. 2018, 41, 151–158. [Google Scholar] [CrossRef]
- Committee, C.S. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). CAPRIE Steering Committee. Lancet 1996, 348, 1329–1339. [Google Scholar] [CrossRef]
- Gargiulo, G.; Goette, A.; Tijssen, J.; Eckardt, L.; Lewalter, T.; Vranckx, P.; Valgimigli, M. Safety and efficacy outcomes of double vs. triple antithrombotic therapy in patients with atrial fibrillation following percutaneous coronary intervention: A systematic review and meta-analysis of non-vitamin K antagonist oral anticoagulant-based randomized clinical trials. Eur. Heart J. 2019, 40, 3757–3767. [Google Scholar] [CrossRef]
- Mehran, R.; Rao, S.V.; Bhatt, D.L.; Gibson, C.M.; Caixeta, A.; Eikelboom, J.; Kaul, S.; Wiviott, S.D.; Menon, V.; Nikolsky, E.; et al. Standardized bleeding definitions for cardiovascular clinical trials: A consensus report from the Bleeding Academic Research Consortium. Circulation 2011, 123, 2736–2747. [Google Scholar] [CrossRef]


| Author, Year | Target Population | Number of Included Studies | Timespan of All Studies | Total Number of Patients | Safety Outcome (Major Bleeding) | Efficacy Outcome |
|---|---|---|---|---|---|---|
| Network Meta-Analysis of RCTs | ||||||
| Gong et al., 2017 [21] | Patients with AF undergoing PCI | 7 P, 5 R, 3 RCTs (WOEST, PIONEER -AF PCI, ROCKET AF post-hoc) | 2008 to 2016 | 13,104 | DT vs. TT Risk Ratio = 0.97 (95% CI: 0.29–3.35) | MACE: DT vs. TT Risk Ratio = 0.68 (95% CI: 0.43–0.98) |
| Bunmark et al., 2018 [26] | Patients with OAC undergoing PCI | 4 RCTs (WOEST, PIONEER-AF PCI, REDUAL-PCI), 12 P, 14 R | 2007 to 2017 | 22,179 | DT vs. TT RR = 0.68 (95% CI: 0.49–0.94) | All-cause death: DT vs. TT RR = 0.40 (95% CI: 0.17–0.93) |
| Lopes et al., 2019 [13] | Patients with AF undergoing PCI | 5 RCTs (WOEST, ISAR-TRIPLE, PIONEER AF-PCI, RE-DUAL PCI, AGUSTUS) | 2013 to 2018 | 10,026 | DT vs. TT OR = 0.49 (95% CI: 0.30–0.82) | MACE: DT vs. TT OR = 1.02 (95% CI: 0.71–1.47) All-cause death: DT vs. TT OR = 1.02 (95% CI: 0.59–1.74) Stroke: DT vs. TT OR = 0.77 (95% CI: 0.34–1.67) |
| Present study, 2020 | Patients with AF undergoing PCI | 6 RCTs (WOEST, ISAR-TRIPLE, PIONEER AF-PCI, RE-DUAL PCI, AGUSTUS, ENTRUST-AF PCI) | 2013 to 2019 | 11,532 | DT vs. TT HR = 0.53 (95% CI: 0.35–078) | MACE: DT vs. TT OR = 1.02 (95% CI: 0.72–1.42) All-cause death: DT vs. TT OR = 1.08 (95% CI: 0.72–1.60) Stroke: DT vs. TT: 0.80 (95% CI: 0.41–1.48) |
| Systemic Review and Meta-Analysis | ||||||
| Chen et al., 2017 [19] | Patients with OAC undergoing PCI | 2 RCTs (WOEST, ISAR-TRIPLE), 5 P, 5 R | 2007 to 2016 | 30,823 | TT vs. DT RR = 0.86 (95% CI: 0.74–0.99) | MACE: TT vs. DT RR = 0.82 (95% CI: 0.58–1.17) All-cause death: TT vs. DT RR = 0.90 (95% CI: 0.54–1.51) Stroke: TT vs. DT RR = 1.08 (95% CI: 0.56–2.07) |
| Zhu et al., 2017 [20] | Patients with AF and ischemic heart disease | 8 P, 9 R | 2010 to 2017 | 38,099 | TT vs. DT RR = 1.65 (95% CI: 1.23–2.21) | MACE: TT vs. DT RR = 1.14 (95% CI: 0.75–1.73, p = 0.55) All-cause death: TT vs. DT RR = 1.21 (95% CI: 0.78–1.88) TE: TT vs. DT RR: 1.55 (95% CI: 0.89–2.72; p = 0.12) |
| Agarwal et al., 2017 [22] | Patients with OAC undergoing PCI | 2 RCTs (WOEST, PIONEER-AF PCI), 6 P, 3 R | 2007 to 2016 | 7276 | TT vs. DT RR = 1.54 (95% CI: 1.20 to 1.98) | MACE: TT vs. DT RR = 1.03 (95% CI: 0.90 to 1.32) All-cause death: TT vs. DR RR = 0.98 (95% CI: 0.68 to 1.43) TE: TT vs. DR RR = 1.02 (95% CI: 0.49 to 2.10) |
| Yu et al., 2017 [23] | Patients with OAC undergoing PCI | 3 RCTs (WOEST, ISAR-TRIPLE, PIONEER AF-PCI), 5 P, 6 R | 2000 to 2016 | 32,825 | TT vs. DT OR = 1.56 (95% CI: 0.98–2.49); | MACE: TT vs. DT OR = 0.97 (95% CI: 0.68 to 1.387) All-cause death: TT vs. DT OR = 2.11 (95% CI: 1.10–4.06) SE: TT vs. DT OR = 0.43 (95% CI: 0.30–0.62) |
| Cavallari et al., 2018 [24] | Patients with AF undergoing PCI | 4 RCTs (WOEST, ISAR-TRIPLE, PIONEER AF-PCI, RE-DUAL PCI) | 2013 to 2017 | 6036 | DT vs. TT OR = 0.55 (95% CI: 0.39 to 0.78) | All-cause death: DT vs. TT OR = 0.81 (95% CI: 0.50 to 1.29) Stroke: DT vs. TT OR = 0.95 (95% CI: 0.58 to 1.57) |
| Golwala et al., 2018 [14] | Patients with AF undergoing PCI | 4 RCTs (WOEST, ISAR-TRIPLE, PIONEER AF-PCI, RE-DUAL PCI) | 2013 to 2017 | 5317 | DT vs. TT HR = 0.53 95% CI: 0.36–0.85) | MACE: DT vs. TT HR = 0.85 (95% CI: 0.48–1.29) All-cause death: DT vs TT HR = 0.85 (95% CI: 0.46–1.37) Stroke: DT vs. TT HR = 0.94 (95% CI: 0.45–1.84) |
| Brunetti et al., 2018 [15] | Patients with AF undergoing PCI | 2 RCTs (PIONEER AF-PCI, RE-DUAL PC) | 2016 to 2017 | 4849 | DT vs. TT RR = 0.59 (95% CI: 0.47–0.73) | MACE: DT vs. TT RR = 1.03 (95% CI: 0.89–1.19) |
| Liu et al., 2018 [25] | Patients with AF undergoing PCI | 5 P, 9 R | 2010 to 2016 | 11,697 | TT vs. DT OR = 1.55 (95% CI: 1.16–2.09) | MACE: TT vs. DT OR = 0.97 (95% CI: 0.87–1.07) All-cause death: TT vs. DT OR = 0.92 (95% CI: 0.83–1.03) Stroke: TT vs. DT OR = 0.74 (95% CI: 0.59–0.93) |
| Gargiulo et al., 2019 [29] | Patients with AF undergoing PCI | 4 RCTs (PIONEER AF-PCI, RE-DUAL PCI, AUGUSTUS, ENTRUST-AF PCI) | 2016 to 2019 | 10,234 | DT vs. TT RR = 0,66 (95% CI: 0.56-0.78) | MACE: DT vs. TT OR = 1.08 (95% CI: 0.95–1.23) All-cause death: DT vs. TT OR = 1.10 (95% CI: 0.91–1.34) Stroke: DT vs. TT OR = 1.00 (95% CI: 0.69–1.45) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chua, S.-K.; Chen, L.-C.; Shyu, K.-G.; Cheng, J.-J.; Hung, H.-F.; Chiu, C.-Z.; Lin, C.-M. Antithrombotic Strategies in Patients with Atrial Fibrillation Following Percutaneous Coronary Intervention: A Systemic Review and Network Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2020, 9, 1062. https://doi.org/10.3390/jcm9041062
Chua S-K, Chen L-C, Shyu K-G, Cheng J-J, Hung H-F, Chiu C-Z, Lin C-M. Antithrombotic Strategies in Patients with Atrial Fibrillation Following Percutaneous Coronary Intervention: A Systemic Review and Network Meta-Analysis of Randomized Controlled Trials. Journal of Clinical Medicine. 2020; 9(4):1062. https://doi.org/10.3390/jcm9041062
Chicago/Turabian StyleChua, Su-Kiat, Lung-Ching Chen, Kou-Gi Shyu, Jun-Jack Cheng, Huei-Fong Hung, Chiung-Zuan Chiu, and Chiu-Mei Lin. 2020. "Antithrombotic Strategies in Patients with Atrial Fibrillation Following Percutaneous Coronary Intervention: A Systemic Review and Network Meta-Analysis of Randomized Controlled Trials" Journal of Clinical Medicine 9, no. 4: 1062. https://doi.org/10.3390/jcm9041062
APA StyleChua, S.-K., Chen, L.-C., Shyu, K.-G., Cheng, J.-J., Hung, H.-F., Chiu, C.-Z., & Lin, C.-M. (2020). Antithrombotic Strategies in Patients with Atrial Fibrillation Following Percutaneous Coronary Intervention: A Systemic Review and Network Meta-Analysis of Randomized Controlled Trials. Journal of Clinical Medicine, 9(4), 1062. https://doi.org/10.3390/jcm9041062





