Outcomes Associated with Respiratory Failure for Patients with Cardiogenic Shock and Acute Myocardial Infarction: A Substudy of the CULPRIT-SHOCK Trial
Abstract
1. Background
2. Methods
2.1. Trial Design
2.2. Outcomes
2.3. Statistical Analysis
3. Results
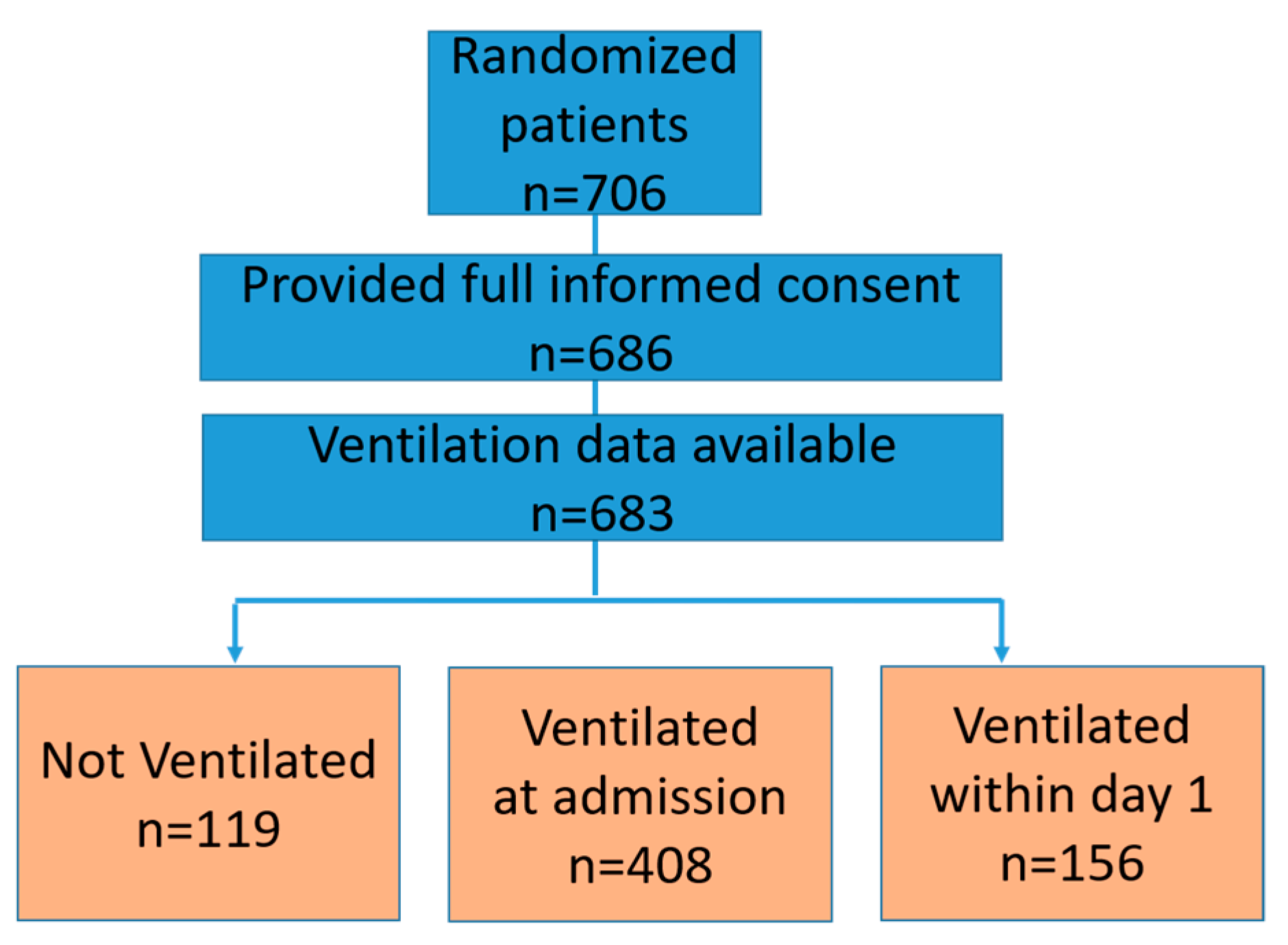
3.1. Patient Characteristics
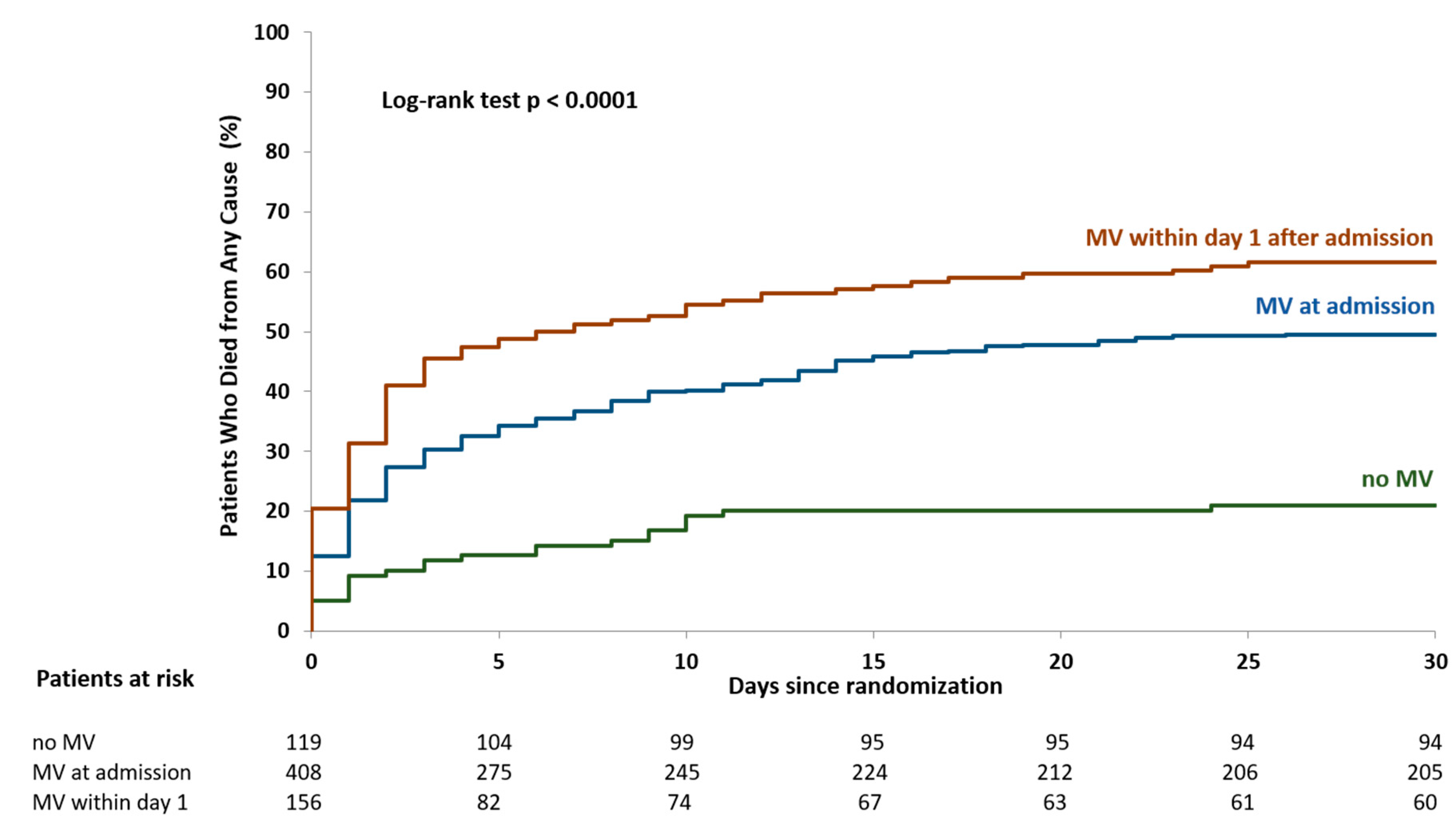
3.2. Clinical Outcomes
3.3. Sensitivity Analyses
4. Discussion
5. Limitations
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Alviar, C.L.; Miller, P.E.; McAreavey, D.; Katz, J.N.; Lee, B.; Moriyama, B.; Soble, J.; Van Diepen, S.; Solomon, M.A.; Morrow, D.A.; et al. Positive Pressure Ventilation in the Cardiac Intensive Care Unit. J. Am. Coll. Cardiol. 2018, 72, 1532–1553. [Google Scholar] [CrossRef] [PubMed]
- Helgestad, O.K.; Josiassen, J.; Hassager, C.; Jensen, L.O.; Holmvang, L.; Sørensen, A.; Frydland, M.; Lassen, A.T.; Udesen, N.L.; Schmidt, H.; et al. Temporal trends in incidence and patient characteristics in cardiogenic shock following acute myocardial infarction from 2010 to 2017: A Danish cohort study. Eur. J. Heart Fail. 2019, 21, 1370–1378. [Google Scholar] [CrossRef] [PubMed]
- Alexander, J.H.; Reynolds, H.R.; Stebbins, A.L.; Dzavik, V.; Harrington, R.A.; de Werf Van, F.; Hochman, J.S. Effect of tilarginine acetate in patients with acute myocardial infarction and cardiogenic shock: The TRIUMPH randomized controlled trial. JAMA 2007, 297, 1657–1666. [Google Scholar] [PubMed]
- Hochman, J.; Sleeper, L.A.; Webb, J.G.; A Sanborn, T.; White, H.D.; Talley, J.D.; Buller, C.E.; Jacobs, A.K.; Slater, J.; Col, J.; et al. Early Revascularization in Acute Myocardial Infarction Complicated by Cardiogenic Shock. N. Engl. J. Med. 1999, 341, 625–634. [Google Scholar] [CrossRef]
- Vallabhajosyula, S.; Dunlay, S.M.; Prasad, A.; Kashani, K.; Sakhuja, A.; Gersh, B.J.; Jaffe, A.S.; Holmes, D.R.; Barsness, G.W. Acute Noncardiac Organ Failure in Acute Myocardial Infarction With Cardiogenic Shock. J. Am. Coll. Cardiol. 2019, 73, 1781–1791. [Google Scholar] [CrossRef]
- Van Diepen, S.; Katz, J.N.; Albert, N.M.; Henry, T.D.; Jacobs, A.K.; Kapur, N.K.; Kilic, A.; Menon, V.; Ohman, E.M.; Sweitzer, N.K.; et al. Contemporary Management of Cardiogenic Shock: A Scientific Statement From the American Heart Association. Circulation 2017, 136, e232–e268. [Google Scholar] [CrossRef]
- Thiele, H.; Ohman, E.M.; De Waha-Thiele, S.; Zeymer, U.; Desch, S. Management of cardiogenic shock complicating myocardial infarction: An update 2019. Eur. Heart J. 2019, 40, 2671–2683. [Google Scholar] [CrossRef]
- Masip, J.; Peacock, W.F.; Price, S.; Cullen, L.; Martín-Sánchez, F.J.; Seferovic, P.; Maisel, A.S.; Miro, O.; Filippatos, G.; Vrints, C.; et al. Indications and practical approach to non-invasive ventilation in acute heart failure. Eur. Heart J. 2018, 39, 17–25. [Google Scholar] [CrossRef]
- Miller, P.E.; Gimenez, M.R.; Thiele, H. Mechanical respiratory support in cardiogenic shock. Eur. J. Heart Fail. 2019, 22, 168. [Google Scholar] [CrossRef]
- Kouraki, K.; Schneider, S.; Uebis, R.; Tebbe, U.; Klein, H.H.; Janssens, U.; Zahn, R.; Senges, J.; Zeymer, U. Characteristics and clinical outcome of 458 patients with acute myocardial infarction requiring mechanical ventilation. Results of the BEAT registry of the ALKK-study group. Clin. Res. Cardiol. 2010, 100, 235–239. [Google Scholar] [CrossRef]
- Thiele, H.; Akin, I.; Sandri, M.; Fürnau, G.; De Waha, S.; Meyer-Saraei, R.; Nordbeck, P.; Geisler, T.; Landmesser, U.; Skurk, C.; et al. PCI Strategies in Patients with Acute Myocardial Infarction and Cardiogenic Shock. N. Engl. J. Med. 2017, 377, 2419–2432. [Google Scholar] [CrossRef] [PubMed]
- Thiele, H.; Akin, I.; Sandri, M.; De Waha-Thiele, S.; Meyer-Saraei, R.; Fürnau, G.; Eitel, I.; Nordbeck, P.; Geisler, T.; Landmesser, U.; et al. One-Year Outcomes after PCI Strategies in Cardiogenic Shock. N. Engl. J. Med. 2018, 379, 1699–1710. [Google Scholar] [CrossRef] [PubMed]
- Thiele, H.; Desch, S.; Piek, J.J.; Stepinska, J.; Oldroyd, K.; Serpytis, P.; Montalescot, G.; Noc, M.; Huber, K.; Fürnau, G.; et al. Multivessel versus culprit lesion only percutaneous revascularization plus potential staged revascularization in patients with acute myocardial infarction complicated by cardiogenic shock: Design and rationale of CULPRIT-SHOCK trial. Am. Heart J. 2016, 172, 160–169. [Google Scholar] [CrossRef]
- Mehran, R.; Rao, S.V.; Bhatt, D.L.; Gibson, C.M.; Caixeta, A.; Eikelboom, J.; Kaul, S.; Wiviott, S.D.; Menon, V.; Nikolsky, E.; et al. Standardized Bleeding Definitions for Cardiovascular Clinical Trials: A Consensus Report From the Bleeding Academic Research Consortium. Circulation 2011, 123, 2736–2747. [Google Scholar] [CrossRef]
- Burkhoff, D.; Cohen, H.; Brunckhorst, C.; O’Neill, W.W. A randomized multicenter clinical study to evaluate the safety and efficacy of the TandemHeart percutaneous ventricular assist device versus conventional therapy with intraaortic balloon pumping for treatment of cardiogenic shock. Am. Heart J. 2006, 152, 469. [Google Scholar] [CrossRef]
- Ouweneel, D.; Eriksen, E.; Seyfarth, M.; Henriques, J.P.S. Percutaneous Mechanical Circulatory Support Versus Intra-Aortic Balloon Pump for Treating Cardiogenic Shock. J. Am. Coll. Cardiol. 2017, 69, 358–360. [Google Scholar] [CrossRef]
- Baran, D.A.; Grines, C.L.; Bailey, S.; Burkhoff, D.; Hall, S.A.; Henry, T.D.; Hollenberg, S.M.; Kapur, N.K.; O’Neill, W.; Ornato, J.P.; et al. SCAI clinical expert consensus statement on the classification of cardiogenic shock. Catheter. Cardiovasc. Interv. 2019, 94, 29–37. [Google Scholar] [CrossRef]
- Thiele, H.; Zeymer, U.; Neumann, D.M.F.-J.; Ferenc, M.; Olbrich, H.-G.; Hausleiter, J.; Richardt, G.; Hennersdorf, M.; Empen, K.; Fuernau, G.; et al. Intraaortic Balloon Support for Myocardial Infarction with Cardiogenic Shock. N. Engl. J. Med. 2012, 367, 1287–1296. [Google Scholar] [CrossRef]
- Marfella, R.; Sardu, C.; Balestrieri, M.L.; Siniscalchi, M.; Minicucci, F.; Signoriello, G.; Calabrò, P.; Mauro, C.; Pieretti, G.; Sardu, C.; et al. Effects of incretin treatment on cardiovascular outcomes in diabetic STEMI-patients with culprit obstructive and multivessel non obstructive-coronary-stenosis. Diabetol. Metab. Syndr. 2018, 10, 1. [Google Scholar] [CrossRef]
- Marfella, R.; Rizzo, M.R.; Siniscalchi, M.; Paolisso, P.; Barbieri, M.; Sardu, C.; Savinelli, A.; Angelico, N.; Del Gaudio, S.; Esposito, N.; et al. Peri-procedural tight glycemic control during early percutaneous coronary intervention up-regulates endothelial progenitor cell level and differentiation during acute ST-elevation myocardial infarction: Effects on myocardial salvage. Int. J. Cardiol. 2013, 168, 3954–3962. [Google Scholar] [CrossRef][Green Version]
- Sardu, C.; D’Onofrio, N.; Torella, M.; Portoghese, M.; Loreni, F.; Mureddu, S.; Signoriello, G.; Scisciola, L.; Barbieri, M.; Rizzo, M.R.; et al. Pericoronary fat inflammation and Major Adverse Cardiac Events (MACE) in prediabetic patients with acute myocardial infarction: Effects of metformin. Cardiovasc. Diabetol. 2019, 18, 126. [Google Scholar] [CrossRef] [PubMed]
- Jentzer, J.; Van Diepen, S.; Barsness, G.W.; Henry, T.D.; Menon, V.; Rihal, C.S.; Naidu, S.S.; Baran, D.A. Cardiogenic Shock Classification to Predict Mortality in the Cardiac Intensive Care Unit. J. Am. Coll. Cardiol. 2019, 74, 2117–2128. [Google Scholar] [CrossRef] [PubMed]
- Magder, S.A.; Lichtenstein, S.; Adelman, A.G. Effects of negative pleural pressure on left ventricular hemodynamics. Am. J. Cardiol. 1983, 52, 588–593. [Google Scholar] [CrossRef]
- Fessler, H.; Brower, R.; Wise, R. Mechanism of reduced LV afterload by systolic and diastolic positive pleural pressure. J. Appl. Physiol. 1988, 65, 1244–1250. [Google Scholar] [CrossRef]
- Grace, M.P.; Greenbaum, D.M. Cardiac performance in response to PEEP in patients with cardiac dysfunction. Crit. Care Med. 1982, 10, 358–360. [Google Scholar] [CrossRef]
- Wiesen, J.; Ornstein, M.C.; Tonelli, A.R.; Menon, V.; Ashton, R.W. State of the evidence: Mechanical ventilation with PEEP in patients with cardiogenic shock. Heart 2013, 99, 1812–1817. [Google Scholar] [CrossRef]
- Hongisto, M.; Lassus, J.; Tarvasmäki, T.; Sionis, A.; Tolppanen, H.; Lindholm, M.G.; Banaszewski, M.; Parissis, J.; Spinar, J.; Silva-Cardoso, J.; et al. Use of noninvasive and invasive mechanical ventilation in cardiogenic shock: A prospective multicenter study. Int. J. Cardiol. 2017, 230, 191–197. [Google Scholar] [CrossRef]
- Esteban, A.; Anzueto, A.; Frutos-Vivar, F.; Alía, I.; Brochard, L.; Stewart, T.E.; Benito, S.; Epstein, S.K.; Apezteguía, C.; Nightingale, P.; et al. Characteristics and Outcomes in Adult Patients Receiving Mechanical VentilationA 28-Day International Study. JAMA 2002, 287, 345. [Google Scholar] [CrossRef]
- Esteban, A.; Frutos-Vivar, F.; Ferguson, N.; Arabi, Y.M.; Apezteguía, C.; González, M.; Epstein, S.K.; Hill, N.; Nava, S.; Soares, M.-A.; et al. Noninvasive Positive-Pressure Ventilation for Respiratory Failure after Extubation. N. Engl. J. Med. 2004, 350, 2452–2460. [Google Scholar] [CrossRef]
| No Ventilation | Ventilation at Admission | Ventilation within Day 1 after Admission | ||
|---|---|---|---|---|
| n = 119 | n = 408 | n = 156 | p-Value | |
| Age‒years | ||||
| Median (IQR) | 70 (60,78) | 68 (59, 77) | 73 (63, 80) | < 0.001 |
| BMI kg/m2 | ||||
| Median (IQR) | 25.7 (23.4, 28.4) | 27.1 (24.7, 29.4) | 26.6 (24.5, 30.1) | 0.008 |
| Cardiovascular risk factors n/N (%) | ||||
| Current smoking | 43/118 (36.4) | 96/391 (24.6) | 34/148 (23.0) | 0.02 |
| Hypertension | 69/119 (58.0) | 240/401 (59.9) | 95/152 (62.5) | 0.74 |
| Dyslipidemia | 44/119 (37.0) | 134/398 (33.7) | 48/152 (31.6) | 0.65 |
| Diabetes mellitus | 38/119 (31.9) | 126/398 (31.7) | 54/153 (35.3) | 0.71 |
| Family history of CAD | 19/118 (16.1) | 43/385 (11.2) | 17/144 (11.8) | 0.35 |
| Previous myocardial infarction n/N (%) | 24/118 (20.3) | 65/400 (16.3) | 24/153 (15.7) | 0.53 |
| Previous stroke n/N (%) | 9/119 (7.6) | 23/401 (5.7) | 17/154 (1.9) | 0.12 |
| Known peripheral artery disease n/N (%) | 15/119 (12.6) | 40/402 (10.0) | 25/154 (16.2) | 0.12 |
| Known renal insufficiency (GFR < 30 mL/min) n/N (%) | 6/119 (5.0) | 27/402 (10.0) | 13/152 (8.6) | 0.52 |
| Chronic dialysis n/N (%) | 1/119 (0.8) | 2/402 (0.5) | 2/154 (1.3) | 0.61 |
| Previous PCI n/N (%) | 25/118 (21.2) | 81/400 (20.3) | 20/153 (13.1) | 0.12 |
| Previous CABG no (%) n/N (%) | 4/119 (3.4) | 25/402 (6.2) | 3/154 (1.9) | 0.08 |
| Signs of impaired organ perfusion n/N (%) | ||||
| Altered mental status | 54/119 (45.4) | 327/406 (80.5) | 79/155 (51.0) | <0.001 |
| Cold, clammy skin and limbs | 67/119 (56.3) | 296/399 (74.2) | 105/153 (68.6) | <0.001 |
| Oliguria (≤ 30 mL/h) | 12/117 (10.3) | 121/394 (30.7) | 40/147 (27.2) | <0.001 |
| Arterial lactate > 2.0 mmol/L | 49/117 (41.9) | 279/396 (70.5) | 111/149 (74.5) | <0.001 |
| Resuscitation before randomization n/N (%) | 18/119 (15.1) | 323/408 (79.2) | 111/149 (74.5) | <0.001 |
| ST-segment elevation n/N (%) | 85/117 (72.6) | 223/392 (56.9) | 105/153 (68.6) | 0.002 |
| anterior n/N (%) | 40/84 (47.6) | 121/221 (54.8) | 59/104 (56.7) | 0.42 |
| non-anterior n/N (%) | 44/84 (52.4) | 100/221 (45.2) | 45/104 (43.3) | 0.42 |
| ST-segment depression n/N (%) | 45/117 (38.5) | 189/392 (48.2) | 72/153 (47.1) | 0.17 |
| LBBB n/N (%) | 11/117 (9.4) | 68/393 (17.3) | 20/153 (13.1) | 0.08 |
| Mean arterial pressure‒mmHg | ||||
| Median (IQR) | 78 (63, 93) | 75 (63, 91) | 75 (63, 95) | 0.89 |
| Heart rate-beats/min | ||||
| Median (IQR) | 79 (61, 101) | 91 (78, 108) | 94 (72, 109) | < 0.001 |
| Creatinine (mmol/l) | ||||
| Median (IQR) | 8.8 (7.2, 13.4) | 13.1 (9.3, 17.6) | 12.3 (9.8, 17.4) | < 0.001 |
| N°of affected vessels n/N (%) | 0.03 | |||
| 1 n/N (%) | 2/119 (1.7) | 3/408 (0.7) | 0/155 (0.0) | |
| 2 n/N (%) | 54/119 (45.4) | 137/408 (33.6) | 54/155 (34.8) | |
| 3 n/N (%) | 63/119 (52.9) | 268/408 (65.7) | 101/155 (65.2) | |
| Artery with culprit lesion n/N (%) | 0.003 | |||
| Left anterior descending | 45/119 (37.8) | 176/408 (43.1) | 66/155 (28.4) | |
| Left circumflex | 21/119 (17.6) | 98/408 (24.0) | 27/155 (17.4) | |
| Right coronary | 46/119 (38.7) | 100/408 (24.5) | 44/155 (28.4) | |
| Left main | 7/119 (5.9) | 27/408 (6.6) | 18/155 (11.6) | |
| Bypass | 0/119 (0.0) | 7/408 (1.7) | 0/155 (0.0) | |
| Left ventricular ejection fraction‒% | ||||
| Median (IQR) | 38 (30, 48) | 33 (25, 40) | 30 (20, 38) | 0.01 |
| No Ventilation | Ventilation at Admission | Ventilation within Day 1 after Admission | ||
|---|---|---|---|---|
| n = 119 | n = 408 | n = 156 | p-Value | |
| Arterial access no/total n/N (%) | ||||
| Femoral | 85/119 (71.4) | 352/408 (86.3) | 124/155 (80.0) | <0.001 |
| Radial | 34/119 (28.6) | 60/408 (14.7) | 32/155 (20.6) | 0.002 |
| Brachial | 0/119 (0.0) | 2/408 (0.5) | 1/155 (0.6) | 0.71 |
| Stent in culprit lesion n/N (%) | ||||
| Any | 115/119 (96.6) | 391/408 (95.8) | 142/155 (91.6) | 0.08 |
| Bare metal | 6/115 (5.2) | 21/391 (5.4) | 10/142 (7.0) | 0.74 |
| Drug eluting | 105/115 (91.3) | 373/391 (95.4) | 133/142 (93.7) | 0.23 |
| Direct Stenting n/N (%) | 27/119 (22.7) | 78/408 (19.1) | 28/155 (18.1) | 0.60 |
| Aspiration thrombectomy before stenting n/N (%) | 27/119 (22.7) | 43/408 (10.5) | 28/155 (18.1) | 0.76 |
| TIMI grade for blood flow n/N (%) | ||||
| Before PCI n/N (%) | <0.001 | |||
| 0 | 77/116 (66.4) | 191/404 (47.3) | 96/153 (62.7) | |
| I | 10/116 (8.6) | 56/404 (13.9) | 16/153 (10.5) | |
| II | 15/116 (12.9) | 67/404 (16.6) | 24/153 (15.7) | |
| III | 14/116 (12.1) | 90/404 (22.3) | 17/153 (11.1) | |
| After PCI n/N (%) | 0.07 | |||
| 0 | 1/118 (0.8) | 19/405 (4.7) | 7/154 (4.5) | |
| I | 1/118 (0.8) | 10/405 (2.5) | 9/154 (5.8) | |
| II | 10/118 (8.5) | 25/405 (6.2) | 13/154 (8.4) | |
| III | 106/118 (89.8) | 351/405 (86.7) | 125/154 (81.2) | |
| Mechanical support n/N (%) | 25/119 (21.0) | 107/408 (26.2) | 61/156 (39.1) | 0.002 |
| IABP | 12/25 (48.0) | 19/107 (17.8) | 19/61 (31.1) | 0.004 |
| Impella 2.5 | 3/25 (12.0) | 21/107 (19.6) | 10/61 (16.4) | 0.64 |
| Impella CP | 5/25 (20.0) | 30/107 (28.0) | 13/61 (21.3) | 0.52 |
| TandemHeart | 0/25 (0.0) | 2/107 (1.9) | 0/61 (0.0) | 0.44 |
| ECMO | 1/25 (4.0) | 25/107 (23.4) | 19/61 (31.1) | 0.026 |
| Other | 4/25 (16.0) | 11/107 (10.3) | 5/61 (8.2) | 0.56 |
| Mild induced hypothermia n/N (%) | 1/119 (0.8) | 205/406 (50.5) | 23/156 (14.7) | < 0.001 |
| Procedural success (TIMI 3 flow or successful complete revascularization) n/N (%) | 105/108 (97.2) | 351/377 (93.1) | 126/137 (92.0) | 0.21 |
| Duration of mechanical ventilation‒days | ||||
| Median (IQR) | n = 0 | 3 (1, 8) | 2 (1, 6) | < 0.001 |
| Duration of ICU treatment‒days | ||||
| Median (IQR) | 3 (2, 6) | 6 (2, 12) | 4 (1, 11) | < 0.001 |
| Catecholamine requirement n/N (%) | 75/119 (63.0) | 391/406 (96.3) | 146/156 (93.6) | < 0.001 |
| Duration of catecholamine days | ||||
| Median (IQR) | 1 (1, 3) | 2 (1, 5) | 2 (1, 5) | < 0.001 |
| Days to hemodynamic stabilization‒days | ||||
| Median (IQR) | 1 (1, 4) | 3 (1, 6) | 2 (1, 8) | < 0.001 |
| No Ventilation | Ventilation at Admission | Ventilation within Day 1 after Admission | ||
|---|---|---|---|---|
| n = 119 | n = 408 | n = 156 | p-Value | |
| Primary endpoint n/N (%) | ||||
| Death | 25/119 (21.0) | 202/407 (49.6) | 96/156 (61.5) | <0.001 |
| Secondary endpoints n/N (%) | ||||
| Renal replacement therapy | 9/119 (7.6) | 63/407 (15.5) | 24/156 (15.4) | 0.08 |
| Myocardial Infarction | 0/119 (0.0) | 7/407 (1.7) | 0/156 (0.0) | 0.09 |
| Rehospitalization | 1/119 (0.8) | 1/407 (0.2) | 0/156 (0.0) | 0.43 |
| Repeat revascularization | 22/119 (18.5) | 46/407 (11.3) | 18/156 (11.5) | 0.10 |
| Safety endpoints n/N (%) | ||||
| Bleeding event | 20/119 (16.8) | 94/407 (23.1) | 34/156 (21.8) | 0.10 |
| Stroke | 2/119 (1.7) | 12/407 (2.9) | 9/156 (5.8) | 0.13 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rubini Giménez, M.; Miller, P.E.; Alviar, C.L.; van Diepen, S.; Granger, C.B.; Montalescot, G.; Windecker, S.; Maier, L.; Serpytis, P.; Serpytis, R.; et al. Outcomes Associated with Respiratory Failure for Patients with Cardiogenic Shock and Acute Myocardial Infarction: A Substudy of the CULPRIT-SHOCK Trial. J. Clin. Med. 2020, 9, 860. https://doi.org/10.3390/jcm9030860
Rubini Giménez M, Miller PE, Alviar CL, van Diepen S, Granger CB, Montalescot G, Windecker S, Maier L, Serpytis P, Serpytis R, et al. Outcomes Associated with Respiratory Failure for Patients with Cardiogenic Shock and Acute Myocardial Infarction: A Substudy of the CULPRIT-SHOCK Trial. Journal of Clinical Medicine. 2020; 9(3):860. https://doi.org/10.3390/jcm9030860
Chicago/Turabian StyleRubini Giménez, Maria, P. Elliott Miller, Carlos L. Alviar, Sean van Diepen, Christopher B. Granger, Gilles Montalescot, Stephan Windecker, Lars Maier, Pranas Serpytis, Rokas Serpytis, and et al. 2020. "Outcomes Associated with Respiratory Failure for Patients with Cardiogenic Shock and Acute Myocardial Infarction: A Substudy of the CULPRIT-SHOCK Trial" Journal of Clinical Medicine 9, no. 3: 860. https://doi.org/10.3390/jcm9030860
APA StyleRubini Giménez, M., Miller, P. E., Alviar, C. L., van Diepen, S., Granger, C. B., Montalescot, G., Windecker, S., Maier, L., Serpytis, P., Serpytis, R., Oldroyd, K. G., Noc, M., Fuernau, G., Huber, K., Sandri, M., de Waha-Thiele, S., Schneider, S., Ouarrak, T., Zeymer, U., ... Thiele, H. (2020). Outcomes Associated with Respiratory Failure for Patients with Cardiogenic Shock and Acute Myocardial Infarction: A Substudy of the CULPRIT-SHOCK Trial. Journal of Clinical Medicine, 9(3), 860. https://doi.org/10.3390/jcm9030860






