Complications in Patients with Acute Myocardial Infarction Supported with Extracorporeal Membrane Oxygenation
Abstract
:1. Introduction
2. Material and Methods
Statistical Analysis
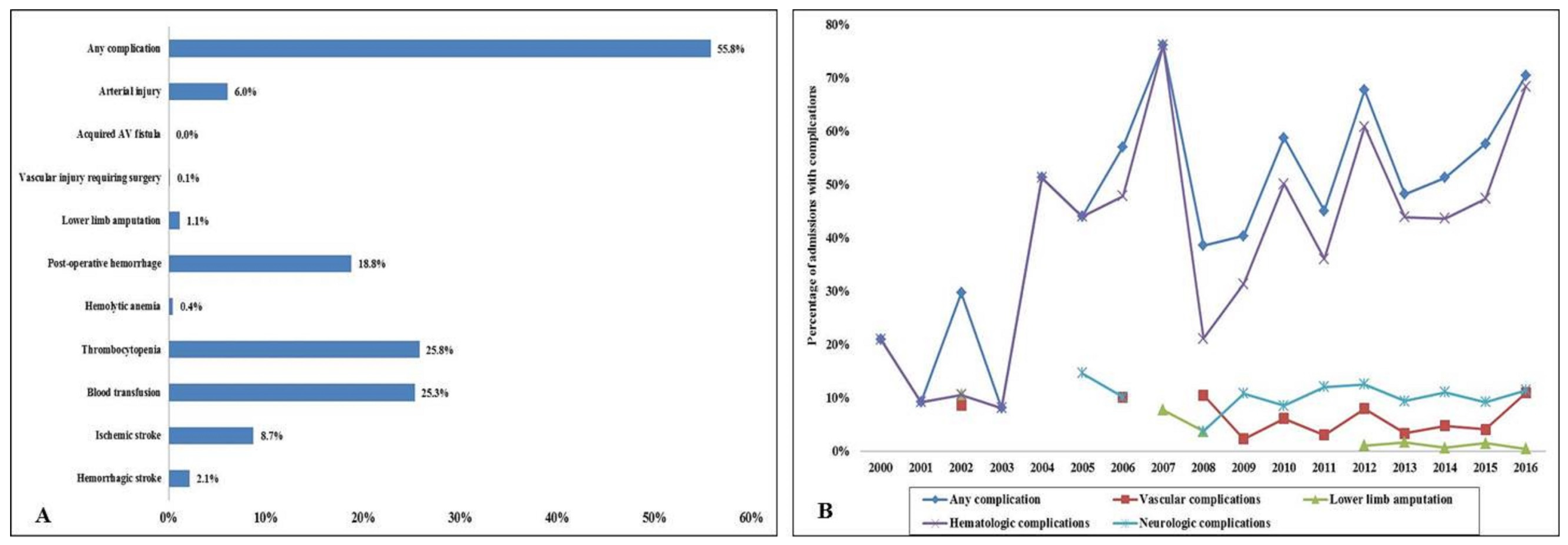
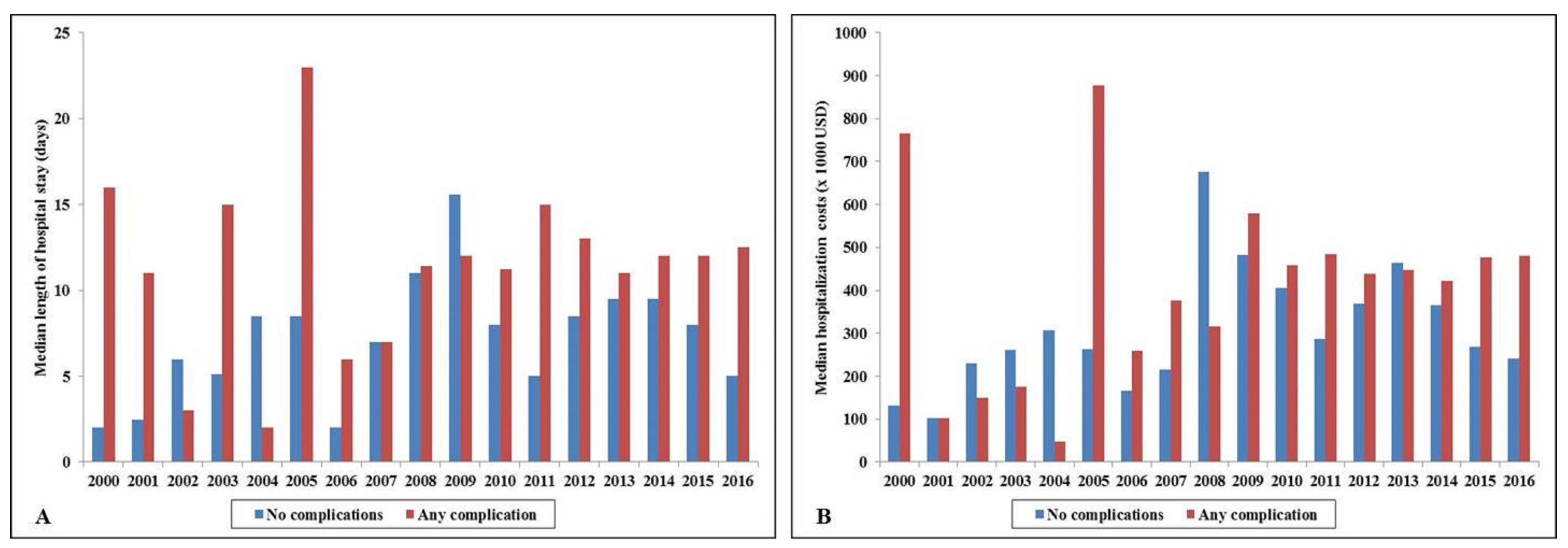
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| AMI | acute myocardial infarction |
| ECMO | extracorporeal membrane oxygenation |
| HCUP | Healthcare Cost and Utilization Project |
| IABP | intra-aortic balloon pump |
| ICD-9CM | International Classification of Diseases-9 Clinical Modification |
| ICD-10CM | International Classification of Diseases-10 Clinical Modification |
| IQR | interquartile range |
| NIS | National/Nationwide Inpatient Sample |
| pLVAD | percutaneous left ventricular assist device |
References
- Subramaniam, A.V.; Barsness, G.W.; Vallabhajosyula, S.; Vallabhajosyula, S. Complications of temporary percutaneous mechanical circulatory support for cardiogenic shock: an appraisal of contemporary literature. Cardiol. Ther. 2019, 8, 211–228. [Google Scholar]
- Vallabhajosyula, S.; Arora, S.; Lahewala, S.; Kumar, V.; Shantha GP, S.; Jentzer, J.C.; Stulak, J.M.; Gersh, B.J.; Gulati, R.; Rihal, C.S.; et al. Temporary mechanical circulatory support for refractory cardiogenic shock before left ventricular assist device surgery. J. Am. Heart Assoc. 2018, 7, e010193. [Google Scholar] [CrossRef] [Green Version]
- Vallabhajosyula, S.; Arora, S.; Sakhuja, A.; Lahewala, S.; Kumar, V.; Shantha, G.P.S.; Egbe, A.C.; Stulak, J.M.; Gersh, B.J.; Gulati, R.; et al. Trends, predictors, and outcomes of temporary mechanical circulatory support for postcardiac surgery cardiogenic shock. Am. J. Cardiol. 2019, 123, 489–497. [Google Scholar]
- Vallabhajosyula, S.; O’Horo, J.C.; Antharam, P.; Ananthaneni, S.; Vallabhajosyula, S.; Stulak, J.M.; Dunlay, S.M.; Holmes, D.R.; Barsness, G.W. Venoarterial extracorporeal membrane oxygenation with concomitant Impella versus venoarterial extracorporeal membrane oxygenation for cardiogenic shock. ASAIO J. 2019. [Google Scholar] [CrossRef] [PubMed]
- Vallabhajosyula, S.; O’Horo, J.C.; Antharam, P.; Ananthaneni, S.; Vallabhajosyula, S.; Stulak, J.M.; Eleid, M.F.; Dunlay, S.M.; Gersh, B.J.; Rihal, C.S.; et al. Concomitant intra-aortic balloon pump use in cardiogenic shock requiring veno-arterial extracorporeal membrane oxygenation. Circ. Cardiovasc Interv. 2018, 11, e006930. [Google Scholar] [CrossRef] [PubMed]
- Vallabhajosyula, S.; Patlolla, S.H.; Sandhyavenu, H.; Vallabhajosyula, S.; Barsness, G.W.; Dunlay, S.M.; Greason, K.L.; Holmes, D.R.; Eleid, M.F. Periprocedural cardiopulmonary bypass or venoarterial extracorporeal membrane oxygenation during transcatheter aortic valve replacement: a systematic review. J. Am. Heart Assoc. 2018, 7, e009608. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vallabhajosyula, S.; Prasad, A.; Bell, M.R.; Sandhu, G.S.; Eleid, M.F.; Dunlay, S.M.; Schears, G.J.; Stulak, J.M.; Singh, M.; Gersh, B.J.; et al. Extracorporeal membrane oxygenation use in acute myocardial infarction in the United States, 2000 to 2014. Circ. Heart Fail. 2019, 12, e005929. [Google Scholar] [CrossRef]
- Vallabhajosyula, S.; Prasad, A.; Sandhu, G.S.; Gulati, R.; Eleid, M.F.; Best, P.J.M.; Gersh, B.J.; Singh, M.; Lerman, A.; Holmes, D.R.; et al. Mechanical Circulatory support-assisted early percutaneous coronary intervention in acute myocardial infarction with cardiogenic shock: 10-year national temporal trends, predictors and outcomes. EuroIntervention. 2019. [Google Scholar] [CrossRef]
- Vallabhajosyula, S.; Barsness, G.W.; Vallabhajosyula, S. Multidisciplinary teams for cardiogenic shock. Aging 2019, 11, 4774–4776. [Google Scholar] [CrossRef]
- Vallabhajosyula, S.; Vallabhajosyula, S.; Vaidya, V.R.; Patlolla, S.H.; Desai, V.; Mulpuru, S.K.; Noseworthy, P.A.; Suraj, K.; Egbe, A.C.; Gersh, B.J.; et al. Venoarterial extracorporeal membrane oxygenation support for ventricular tachycardia ablation: a systematic review. ASAIO J. 2020. [Google Scholar] [CrossRef]
- Vallabhajosyula, S.; Kashani, K.; Dunlay, S.M.; Vallabhajosyula, S.; Vallabhajosyula, S.; Sundrargiri, P.R.; Gersh, B.J.; Jaffe, A.S.; Barsness, G.W. Acute respiratory failure and mechanical ventilation in cardiogenic shock complicating acute myocardial infarction in the USA, 2000–2014. Ann. Intensive Care. 2019, 9, 96. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Introduction to the HCUP Nationwide Inpatient Sample 2009. Available online: http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_2009_INTRODUCTION.pdf (accessed on 18 January 2015).
- Vallabhajosyula, S.; Dunlay, S.M.; Barsness, G.W.; Rihal, C.S.; Holmes, D.R., Jr.; Prasad, A. Hospital-level disparities in the outcomes of acute myocardial infarction with cardiogenic shock. Am. J. Cardiol. 2019, 124, 491–498. [Google Scholar] [CrossRef] [PubMed]
- Vallabhajosyula, S.; Dunlay, S.M.; Barsness, G.W.; Vallabhajosyula, S.; Vallabhajosyula, S.; Sundrargiri, P.R.; Gersh, B.J.; Jaffe, A.S.; Kashani, K. Temporal trends, predictors, and outcomes of acute kidney injury and hemodialysis use in acute myocardial infarction-related cardiogenic shock. PLoS ONE 2019, 14, e0222894. [Google Scholar] [CrossRef] [PubMed]
- Vallabhajosyula, S.; Dunlay, S.M.; Kashani, K.; Vallabhajosyula, S.; Vallabhajosyula, S.; Sundrargiri, P.R.; Jaffe, A.S.; Barsness, G.W. Temporal trends and outcomes of prolonged invasive mechanical ventilation and tracheostomy use in acute myocardial infarction with cardiogenic shock in the United States. Int J. Cardiol. 2019, 285, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Vallabhajosyula, S.; Dunlay, S.M.; Murphree, D.H.; Barsness, G.W.; Sandhu, G.S.; Lerman, A.; Prasad, A. Cardiogenic shock in takotsubo cardiomyopathy versus acute myocardial infarction: an 8-year national perspective on clinical characteristics, management, and outcomes. JACC Heart Fail. 2019, 7, 469–476. [Google Scholar] [CrossRef] [PubMed]
- Vallabhajosyula, S.; Dunlay, S.M.; Prasad, A.; Kashani, K.; Sakhuja, A.; Gersh, B.J.; Jaffe, A.S.; Holmes, D.R.; Barsness, G.W. Acute noncardiac organ failure in acute myocardial infarction with cardiogenic shock. J. Am. Coll Cardiol. 2019, 73, 1781–1791. [Google Scholar] [CrossRef]
- Vallabhajosyula, S.; El Hajj, S.C.; Bell, M.R.; Prasad, A.; Lerman, A.; Rihal, C.S.; Holmes, D.R.; Barsness, G.W. Intravascular ultrasound, optical coherence tomography, and fractional flow reserve use in acute myocardial infarction. Catheter Cardiovasc Interv. 2019. [Google Scholar] [CrossRef]
- Vallabhajosyula, S.; Patlolla, S.H.; Dunlay, S.M.; Prasad, A.; Bell, M.R.; Jaffe, A.; Gersh, B.J.; Rihal, C.S.; Holmes, D.R.; Barsness, G.W. Regional variation in the management and outcomes of acute myocardial infarction with cardiogenic shock in the United States. Circ. Heart Fail. 2020, 13, e006661. [Google Scholar] [CrossRef]
- Vallabhajosyula, S.; Prasad, A.; Dunlay, S.M.; Murphee, D.H.; Ingram, C.; Mueller, P.S.; Gersh, B.J.; Holmes, D.R.; Barsness, G.W. Utilization of palliative care for cardiogenic shock complicating acute myocardial infarction: A 15-year national perspective on trends, disparities, predictors, and outcomes. J. Am. Heart Assoc. 2019, 8, e011954. [Google Scholar] [CrossRef] [Green Version]
- Vallabhajosyula, S.; Prasad, A.; Gulati, R.; Barsness, G.W. Contemporary prevalence, trends, and outcomes of coronary chronic total occlusions in acute myocardial infarction with cardiogenic shock. Int J. Cardiol Heart Vasc. 2019, 24, 100414. [Google Scholar] [CrossRef]
- Vallabhajosyula, S.; Vallabhajosyula, S.; Bell, M.R.; Prasad, A.; Singh, M.; White, R.D.; Jaffe, A.S.; Holmes, D.R.; Jentzer, J.C. Early vs. delayed in-hospital cardiac arrest complicating ST-elevation myocardial infarction receiving primary percutaneous coronary intervention. Resuscitation 2019. [Google Scholar] [CrossRef] [PubMed]
- Vallabhajosyula, S.; Ya’Qoub, L.; Dunlay, S.M.; Vallabhajosyula, S.; Vallabhajosyula, S.; Sundaragiri, P.R.; Jaffe, A.S.; Gersh, B.J.; Kashani, K. Sex disparities in acute kidney injury complicating acute myocardial infarction with cardiogenic shock. ESC Heart Fail. 2019, 6, 874–877. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Overall Cohort (n = 4608) | Odds Ratio | 95% Confidence Interval | p | ||
|---|---|---|---|---|---|
| Lower Limit | Upper Limit | ||||
| Any complication | 0.89 | 0.77 | 1.02 | 0.10 | |
| Age groups (years) | ≤75 years | Reference category | |||
| >75 years | 1.54 | 1.16 | 2.03 | 0.003 | |
| Sex | Male | Reference category | |||
| Female | 1.21 | 1.04 | 1.40 | 0.01 | |
| Race | White | Reference category | |||
| Non-White a | 1.42 | 1.25 | 1.63 | <0.001 | |
| Primary payer | Medicare | Reference category | |||
| Medicaid | 0.59 | 0.47 | 0.74 | <0.001 | |
| Private | 0.49 | 0.41 | 0.57 | <0.001 | |
| Others b | 1.02 | 0.80 | 1.29 | 0.89 | |
| Charlson Comorbidity Index | 0–3 | Reference category | |||
| 4–6 | 1.00 | 0.86 | 1.16 | 0.99 | |
| ≥7 | 0.97 | 0.76 | 1.24 | 0.82 | |
| Hospital teaching status and location | Rural | Reference category | |||
| Urban non-teaching | 0.67 | 0.37 | 1.21 | 0.19 | |
| Urban teaching | 1.57 | 0.91 | 2.69 | 0.10 | |
| Hospital bed-size | Small | Reference category | |||
| Medium | 0.99 | 0.66 | 1.47 | 0.95 | |
| Large | 1.60 | 1.11 | 2.31 | 0.01 | |
| Hospital region | Northeast | Reference category | |||
| Midwest | 0.93 | 0.78 | 1.11 | 0.44 | |
| South | 0.77 | 0.66 | 0.91 | 0.002 | |
| West | 0.98 | 0.79 | 1.23 | 0.89 | |
| AMI type | STEMI | Reference category | |||
| NSTEMI | 1.00 | 0.86 | 1.15 | 0.96 | |
| Acute organ dysfunction | Respiratory | 1.18 | 1.02 | 1.35 | 0.02 |
| Renal | 1.63 | 1.41 | 1.88 | <0.001 | |
| Hepatic | 1.42 | 1.23 | 1.65 | <0.001 | |
| Cardiogenic shock | 0.86 | 0.72 | 1.01 | 0.07 | |
| Cardiac arrest | 1.01 | 0.89 | 1.15 | 0.85 | |
| Coronary angiography | 1.36 | 1.17 | 1.57 | <0.001 | |
| Percutaneous coronary intervention | 0.66 | 0.57 | 0.76 | <0.001 | |
| Pulmonary artery catheterization | 0.66 | 0.54 | 0.81 | <0.001 | |
| Second mechanical circulatory support use | 0.97 | 0.85 | 1.11 | 0.66 | |
| Invasive mechanical ventilation | 1.21 | 1.06 | 1.39 | 0.005 | |
| Hemodialysis use | 1.81 | 1.39 | 2.35 | <0.001 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vallabhajosyula, S.; Bell, M.R.; Sandhu, G.S.; Jaffe, A.S.; Holmes, D.R., Jr.; Barsness, G.W. Complications in Patients with Acute Myocardial Infarction Supported with Extracorporeal Membrane Oxygenation. J. Clin. Med. 2020, 9, 839. https://doi.org/10.3390/jcm9030839
Vallabhajosyula S, Bell MR, Sandhu GS, Jaffe AS, Holmes DR Jr., Barsness GW. Complications in Patients with Acute Myocardial Infarction Supported with Extracorporeal Membrane Oxygenation. Journal of Clinical Medicine. 2020; 9(3):839. https://doi.org/10.3390/jcm9030839
Chicago/Turabian StyleVallabhajosyula, Saraschandra, Malcolm R. Bell, Gurpreet S. Sandhu, Allan S. Jaffe, David R. Holmes, Jr., and Gregory W. Barsness. 2020. "Complications in Patients with Acute Myocardial Infarction Supported with Extracorporeal Membrane Oxygenation" Journal of Clinical Medicine 9, no. 3: 839. https://doi.org/10.3390/jcm9030839
APA StyleVallabhajosyula, S., Bell, M. R., Sandhu, G. S., Jaffe, A. S., Holmes, D. R., Jr., & Barsness, G. W. (2020). Complications in Patients with Acute Myocardial Infarction Supported with Extracorporeal Membrane Oxygenation. Journal of Clinical Medicine, 9(3), 839. https://doi.org/10.3390/jcm9030839






