Abstract
Background: Pulpotomy of primary teeth provides favorable clinical results over time; however, to date, there is still not a consensus on an ideal pulp dressing material. Therefore, the aim of the present systematic review was to compare pulpotomy agents to establish a preferred material to use. Methods: After raising a PICO question, the PRISMA guideline was adopted to carry out an electronic search through the MEDLINE database to identify comparative studies on several pulp dressing agents, published up to October 2019. Results: The search resulted in 4274 records; after exclusion, a total of 41 papers were included in the present review. Mineral trioxide aggregate (MTA), Biodentine and ferric sulphate yielded good clinical results over time and might be safely used in the pulpotomies of primary molars. Among agents, MTA seemed to be the material of choice. On the contrary, calcium hydroxide showed the worst clinical performance. Although clinically successful, formocreosol should be replaced by other materials, due to its potential cytotoxicity and carcinogenicity. Conclusion: MTA seemed to be the gold standard material in the pulpotomy of primary teeth. Promising results were also provided by calcium silicate-based cements. Further randomized clinical trials (RCTs) with adequate sample sizes and long follow-ups are encouraged to support these outcomes.
1. Introduction
Dental caries is an infective, chronic, degenerative and multifactorial condition that represents the most prevalent chronic disease worldwide, mainly in children [1,2]. Tooth decay would seem to be one of the major public health problems related not only to primary teeth but also to permanent ones, and, despite the preventive strategies mostly adopted in developed countries, 2.4 billion adults and 486 million children are affected by dental decay in the permanent and deciduous dentition, respectively [3].
Early caries management should avoid the progressive destruction of dental hard tissue and subsequent loss of dental vitality [4], inducing critical conditions in which premature tooth extraction is required [5]. This is mostly true for primary teeth (due to anatomical considerations, reduced rate of mineralization and high prevalence of risk factors) that show a rapid progression of tooth decay [2,4,6]. Therefore, vital pulp therapy (VPT) has been proposed to preserve the pulp vitality of deciduous or young permanent teeth with immature roots affected by caries and without evidence of radicular pathology [7,8]. Nowadays, treatment options of VPT are represented by indirect pulp treatment (namely indirect pulp capping), direct pulp capping and pulpotomy [7]. Although clinically successful in primary molars, direct capping is mainly recommended in the VPT of permanent young teeth [9,10] and indirect capping seems to possess a relative effectiveness when compared to pulpotomy procedures [11]. The latter provides favorable clinical survival rates over time and allows the vitality of primary teeth until their natural exfoliation, avoiding pulpectomy procedures [2]. Pulpotomy consists of elimination of the bacterial infection by the removal of the pulp in the pulp chamber; then, the decontaminated tooth is filled with a medicament [11]. The most frequently used agents are mineral trioxide aggregate (MTA), Biodentine (BD), formocresol (FC), ferric sulphate (FS) and calcium hydroxide (CH). When compared, FC, FS and MTA seemed to provide significantly better clinical and radiographic results as pulpotomy agents than CH after two years of follow-up; moreover, MTA showed the best performance in respect to FC and FS over time [12]. Accordingly, Stringhini et al. [13] reported that MTA yielded superior clinical and radiographical results in comparison to FC. On the other hand, electrosurgery and FS showed similar success to FC, whereas CH did not show positive evidence as medicament in pulpotomies of primary teeth [13]. In the same way, Asgary et al. [14] further stressed that MTA demonstrated better long-term outcomes in pulpotomy of primary molars when compared with FS.
More recently, bioactive endodontic cements have been introduced as valid alternatives to MTA in VPT, showing promising clinical results [15]. In addition, calcium-silicate-based cement demonstrates no difference when compared to MTA in the pulpotomies of primary teeth [4]; however, further long-term studies with larger sample sizes are needed to confirm these preliminary outcomes.
To date there is still not an ideal pulp dressing material to be used in the pulpotomy of primary teeth. Therefore, the aim of the present systematic review was to compare several pulpotomy agents in order to establish a preferred material that performs better than others.
2. Materials and Methods
The present systematic review was conducted according to the PRISMA guidelines for Systematic Reviews [16]. The focused question was structured according to the PICO format (Population, Intervention, Comparison, and Outcome): is there a preferred material that performs better than others when used in pulpotomy of vital carious-exposed primary molars?
Population: Children with extensive caries involving vital dental pulp in primary teeth.
Intervention: Pulpotomy performed using different materials (MTA, Biodentine, ferric sulphate, calcium hydroxide).
Comparison: Between different materials applied in the same clinical conditions.
Outcome: Success of the therapy after at least 12 months of follow-up.
2.1. Search Strategy
An electronic search was conducted through the MEDLINE (PubMed) database to identify publications that met the inclusion criteria. The search was performed up to October 2019 in order to identify the studies that compare the performance of different materials in pulpotomy treatment of primary teeth, using the following search terms and key words alone or in combination with the Boolean operator “AND”: endodontics, pulpotomy, primary molars, deciduous teeth, primary teeth, biomaterials, biodentine, MTA, mineral trioxide aggregate, ferric sulphate, ferric sulfate, calcium hydroxide. Moreover, references of the eligible studies and relevant systematic reviews on the topic were manually checked and screened.
2.2. Study Selection
Two independent operators (F.I., G.D.G.) screened the studies according to the following inclusion/exclusion criteria:
2.2.1. Inclusion Criteria
- -
- Human in vivo studies written in English published in peer-reviewed journals;
- -
- Comparative clinical articles reporting on different materials applied in pulpotomy of primary teeth;
- -
- Definitive restorations of the primary teeth;
- -
- Clinical and/or radiographical follow-up of at least 12 months;
- -
- Random allocation of the samples.
2.2.2. Exclusion Criteria
- -
- In vitro studies on human and animals;
- -
- Systematic reviews, case series, case studies, retrospective studies;
- -
- Follow-up < 12 months;
- -
- Clinical studies without random allocation of the samples;
- -
- Non-comparative papers, namely reporting on only one material used in pulpotomy procedures;
- -
- Papers evaluating other clinical procedures that involved the pulp, such as direct capping, indirect capping, endodontic treatment.
After removing the duplicates, some papers were excluded subsequent to reading of the titles. Two review authors (F.I., G.D.G.) independently screened the selected abstracts to identify relevant studies according to the inclusion/exclusion criteria. In case of disagreement, a Senior Author (M.B.) was consulted and agreement was reached. Then, full reports of the selected studies were retrieved and a data extraction form was completed for each paper in an unblinded standardized manner, to determine whether the article should be included or excluded. Excluded studies and reasons for exclusion were reported.
2.3. Data Collection
Data extraction was performed by filling a form in with the following data: authors, title, publication year, aim, group distribution, materials compared, intervention, evaluated outcomes, reported results and conclusions.
After a preliminary evaluation of the selected papers, considerable heterogeneity was found in the study design, adopted procedures, outcome variables and results. Therefore, a descriptive analysis of the data was performed, since quantitative assessment and following meta-analysis could not be conducted.
2.4. Assessment of Heterogeneity
The following variables were checked to determine heterogeneity:
- Pulpotomy procedure
- Materials management
- Expertise of the clinician
- Restoration materials
- Outcome variables
2.5. Quality Assessment
The assessment of methodological study quality was performed by two independent authors (F.I. and G.D.G.) following the recommendations for systematic reviews of interventions of the Cochrane collaboration [17] focusing on the following criteria: random sequence generation and allocation concealment (both accounting for selection bias), blinding of participants and personnel (performance bias), blinding of outcome assessment (detection bias), incomplete outcome data (attrition bias), selective reporting (reporting bias), or other possible causes of bias.
Assessment of overall risk of bias was classified as follows: low risk of bias if all criteria were met; unclear risk of bias if one or more criteria were assessed as unclear; or high risk of bias if one or more criteria were not met [2].
3. Results
3.1. Search and Selection
The PubMed-MEDLINE search resulted in 4274 records. After duplicate removal, the titles and abstracts were screened according to the inclusion/exclusion criteria and a total of 75 papers underwent full-text reading. Thirty-four articles were excluded [18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51] since they did not meet the inclusion criteria; reasons of exclusion have been reported within Table 1. A total of 41 papers [52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85,86,87,88,89,90,91,92] were included in the present systematic review and processed for quality assessment and data extraction. The search strategy has been reported in Figure 1.

Table 1.
Excluded studies and reason of exclusion.
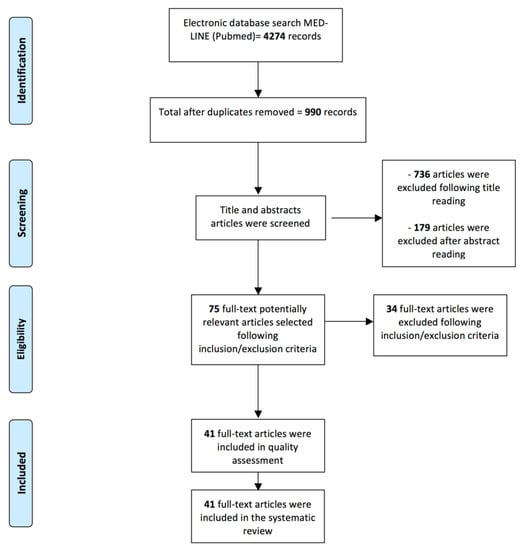
Figure 1.
Flowchart of the review process and search strategy according to PRISMA statement.
3.2. Assessment of Heterogeneity
The data extraction of the included studies yielded a considerable heterogeneity between the papers in terms of pulpotomy procedure, materials management, expertise of the clinician, restoration materials, and outcome variables. To better standardize the study comparison, papers reporting pulpotomy procedures different from the standard method were excluded (e.g., absence of the rubber dam, pulpotomy performed with laser ablation or electrosurgery, hemostasis obtained with several agents that could act as bias on the clinical outcomes).
Concerning materials management, the included studies evaluated several materials (e.g., MTA, BD, FS, CH, FC) that were applied with almost with the same procedure according to the manufacturer’s instructions; however, it should be considered that they were produced by various companies and might have a slightly different composition. Accordingly, the restoration materials reported by the included studies were different (composite, amalgam, glass ionomer cement, stainless steel crowns), however, in order to avoid bias, papers reporting teeth restored with temporary materials were excluded. Regarding the evaluated outcomes, all of the included studies assessed clinical and radiographical parameters; the success criteria used among the articles were similar but not the same and, therefore, it was only possible to make a descriptive comparison between the papers. Finally, the clinician expertise could not be evaluated in each study and the follow-up range varied between 12 and 42 months. Therefore, due to the lack of unequivocal data presentation, the results of the studies were reported separately.
3.3. Quality Assessment
Assessments of the risk of bias and of the methodological study quality have been reported in Table 2. Overall risk of bias of the included studies showed high risk mainly in blinding of participants and personnel (28/41 studies), followed by blinding of outcome assessment (12/41 studies) (Figure 2). The lack of blind clinicians involved in the treatment as well as evaluation of the outcomes could affect the interpretation of the reported results provided in each study, playing a central role in the variability of study conclusions.

Table 2.
Assessment of risk of bias of the included studies.
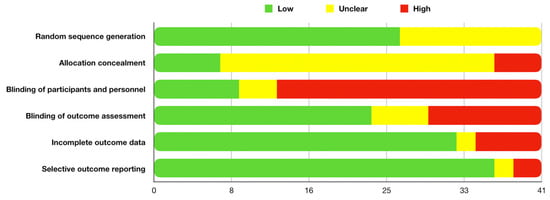
Figure 2.
Overall risk of bias.
The inter- inter-examiner agreement between the two independent authors that performed the quality assessment of the included studies was 0.95.
3.4. Outcomes
Data and results reported by each of the included studies are summarized in Table 3.

Table 3.
Summary of the data reported in the studies included in the present systematic review.
In order to ease the reading of the outcomes, the papers were further presented according to the material that yielded the best result after comparison.
3.4.1. MTA
Almost 65% of the included papers (27/41) demonstrated that MTA provided comparable or even better results over time when compared to other materials used in the pulpotomy procedures of deciduous teeth. Specifically, MTA showed better performance than FC after 12 months of evaluation [67,76,86], with a statistically significant difference reported in two out three of the evaluated studies [67,86]. Moreover, better results of MTA in comparison to FC were observed after 24 months of follow-up [55,70,72,85,90], although the differences did not reach a statistical significance except in one study [55]. The same trend was maintained even after 30 [77] and 42 [78] months of evaluation, respectively. In two additional studies [66,88], it was reported that FC showed slightly worse results than MTA at a 24-month evaluation; however, it performed better than other materials assessed during pulpotomy of primary teeth, such as Pulpotec and Emdogain [88], as well as Portland cement and enamel matrix protein [66]. On the other hand, Jamali et al. [65] reported a superiority of MTA in respect to FC after 24 months of evaluation, even though both groups yielded worse results when compared to 3Mixtatin (a combination of simvastatin and 3Mix antibiotic) (78.9% for FC, 90.5% for 3Mixtatin and 88.1% for MTA). However, the differences between groups were not statistically significant.
When solely compared to BD, MTA showed slightly better performances after 12 [56], 18 [61] and 24 [52] months of assessment, without any statistically significant differences among groups. No differences between MTA and BD were reported by Juneja et al. [59], evaluating pulpotomy procedures on primary teeth performed also with FC. However, the authors observed that there were statistically significant differences between FC and MTA at 12 and 18 months, both clinically and radiographically, and between FC and BD at 12 and 18 months, only clinically [59]. Accordingly, Guven et al. [57] demonstrated no differences between BD and MTA groups (total success rates at 24 months were 82.75% BD, 86.2% MTA-P and 93.1% PR-MTA); however, in the same study, primary teeth treated with FS showed the lowest success rate (75.86%) at a 24-month follow-up, although this was not statistically significant.
The comparison between MTA and FS yielded not significant differences after 18 [64] and 24 [71] months of evaluation; however, Doyle et al. [73] demonstrated a significantly lower survival rate for primary teeth treated with eugenol-free FS than MTA, after a follow-up period of 38 months. It should be noticed that Erdem et al. [71] not only reported the same performance for FS and FC (success rate of 88% for both groups) at a 24-month follow-up, but also demonstrated a statistically significant difference between MTA and a group of samples that underwent pulpotomy without use of any pulp dressing agent (96% vs. 68% after 24 months), suggesting the importance of the traditional pulpotomy procedure for the VTP of primary molars.
CH seemed to be the most ineffective material for pulpotomies of deciduous teeth and demonstrated the worst results when compared with MTA [63] after 12 months, and with MTA and FC (MTA 100%, FC 100%, CH 64%) [74], ProRoot MTA and MTA Angelus [68] and MTA and Portland cement [69] after 24 months of evaluation, respectively. In addition, the differences between CH and all tested materials were significantly different at all follow-up points.
Finally, the comparison of MTA with other pulpotomy agents, such as calcium-enriched mixture cement (CEM) [53] and Portland cement [54], provided the same clinical and radiographical performances of all evaluated materials after a follow-up period of 24 months.
3.4.2. Biodentine
El Meligy et al. [87] clinically and radiographically evaluated 108 primary teeth that underwent pulpotomy performed with BD or FC. After 12 months, the authors reported a 100% clinical success rate in both groups and a radiographic success rate of 100% and 98.1% in the BD and FC groups, respectively, although without any statistically significant difference.
Three out of the 41 included papers reported the same [60] or even slightly better results [58,62] of BD in respect to MTA. Specifically, after a follow-up period of 12 months, 39 pulpotomized primary teeth treated with MTA showed a clinical success rate of 92% (36/39) and a radiographical success rate of 97% (38/39), whereas 39 teeth belonging to the BD group showed a clinical and radiographical success rate of 97% (38/39) and 95% (37/39), respectively [62]. A 24-month follow-up evaluation revealed that the clinical success rate of 62 primary molars that underwent pulpotomy was 96.8% (30/31) for both BD and MTA groups and the radiographic success was 93.6% (29/31) for the BD group and 87.1% (27/31) for the MTA group [58].
Therefore, although BD showed slightly better clinical results after one year [62] and radiographic results after two years of follow-up [58], no statistically significant differences were found among groups.
3.4.3. Ferric Sulphate
A total of three out 41 included papers [80,83,92] demonstrated that FS performed better when compared to FC in the pulpotomy of carious deciduous teeth, however without reporting statistically significant differences. Specifically, after 12 months, a total success rate of 92.7% and 83.8% was reported by Fucks et al. [92] and a clinical success rate of 96.7% and 86.7% was reported by Havale et al. [80] in primary molars that underwent pulpotomy with FS and FC, respectively. The latest study [80] also demonstrated a gradual decrease of radiological success rate over time, showing rates of 56.7% and 63.3% for FS and FC, respectively. Moreover, Ozmen et al. [83] compared three pulpotomy agents, such as FC, FS and Ankaferd blood stopper (ABS), and reported a more favorable clinical success rate for FS (100%) than other evaluated materials (87% for both ABS and FC) after a follow-up of 24 months. Concerning radiographical success, the same authors reported gradually reduced rates that were comparable for FS and ABS (87%) and slightly lower for FC (80%).
3.4.4. Formocresol
According to the International Agency for Cancer Research, one of the main components of FC, namely formaldehyde, has been classified as a human carcinogen [93]; due to this reason, FC was not included as one of the keywords in the search strategy of the present systematic review. However, the same material is still largely used and was reported in more than half of the included studies (23/41). Among them, seven papers [75,79,81,82,84,89,91] reported similar or even better results of FC when compared to other agents used in pulpotomy of primary teeth. Durmus et al. [79] reported a 12-month clinical success rate of 97% and 92.5% of deciduous teeth pulpotomized and treated with FC and FS, respectively, as well as comparable radiographical results (87% FC vs.79% FS), without any statistically significant differences among groups. Moreover, FC and FS provided similar results in pulpotomy procedures after 12 (clinical success: 96% FC and 95.7% FS; radiographic success: 100% both FC and FS) and 18 months (clinical success: 96% FC and 87% FS; radiographic success: 100% FC and 91.3% FS) of evaluation [84]. Markovic et al. [82] compared the 18-month clinical and radiographical success of pulpotomies performed on 104 primary molars randomly divided into three groups and treated with FS, FC and CH. FS and FC showed comparable radiographical and clinical success (89.2% and 90.9%, respectively); on the other hand, the CH group demonstrated lower success than other groups (82.3%), although this was not statistically significant [82]. Accordingly, comparing pulpotomies with FS, FC and CH after 12, 24 and 36 months, CH showed the worst results after 24 and 36 months and, even though the values did not reach statistical significance, the failure rate for the CH group was three times higher than the FC one [81]. On the other hand, primary teeth treated with FC after pulpotomy showed slightly better results than the FS group after 12 months of evaluation (96% FC vs. 86% FS), and vice versa after 24 and 36 months of follow-up (85% FC vs. 86% FS and 72% FC vs. 76% FS, respectively) [81]. Fernandes et al. [89] reported a significantly better radiographical success rate of pulpotomy performed with FC compared to CH after 12 (100% FC vs. 50% CH) and 18 months (100% FC vs. 66.7% CH), demonstrating that CH may not be considered suitable in pulpotomy treatment of primary molars, even in combination with Low Level Laser Therapy [89]. Similar outcomes were also reported by Sonmez et al. [91], who observed 2-year follow-up success rates of 46.1%, 66.6%, 73.3% and 76.9% in 80 primary molars treated with CH, MTA, FS and FC, respectively. Although no statistically significant differences were detected among groups, CH seemed to be less clinically appropriate than other evaluated materials. Finally, Noorollahian [75] reported that, after 24 months of evaluation, primary teeth treated with FC during pulpotomy provided better radiographical results than ones that underwent MTA, although both groups yielded a 100% clinical success at the same follow-up point.
4. Discussion
VTP aims at preserving pulpal tissue and promoting repair of the mineralized tissue barrier (dentin bridge) [94]. In addition, the success of this technique would avoid pulpectomy and subsequent root canal obturation by several materials, that, on turn, could prevent the radicular resorption of the primary molars and alter the development of the permanent teeth [11].
Since there is a lack of a general consensus regarding an ideal pulp dressing material, the aim of the present systematic review was to establish a preferred agent to be used in the pulpotomy procedure of primary teeth affected by deep caries, after raising a PICO question. The evaluation of the included studies suggested that MTA seemed to be the material of choice after pulpotomies. Although it showed successful clinical performances over time, the majority of the authors agreed on its drawbacks, such as high costs, difficult storage and long setting time [4]. Therefore, in some cases, alternative materials may be used. FC had historically been indicated as a valid option in the pulpotomy procedures of primary molars; however, the evidence-based scientific literature has already demonstrated its potential cytotoxicity and carcinogenicity [93]. Due to this reason, FC was not included in the search strategy of the present systematic review; nevertheless, it is largely used and provides some good clinical results. Thus, to supply a complete overview on the topic, papers that compared several materials with FC were included. Seven studies [75,79,81,82,84,89,91] reported better clinical outcomes of FC than FS. On the other hand, the comparison between FC and MTA [55,66,67,70,72,76,77,78,85,86,88,90], yielded a better performance of the latter after 12, 24, 30 and 42 months of evaluation. Accordingly, El Meligy et al. [87] observed slightly favorable clinical and radiographical outcomes of primary teeth underwent pulpotomy performed with BD than FC, although no statistically significant.
FS yielded more favorable clinical results when compared to FC in 3/41 studies included in the present review [80,83,92]. Even though it provided comparable or slightly worse outcomes than MTA [64,71,73], when the pulpotomized primary molars are going to be replaced by permanent teeth, FS may be used as a safe alternative [95].
In accordance with the scientific literature [95], the present review confirmed that CH seemed to be the most ineffective material for pulpotomies of deciduous teeth and demonstrated the worst results when compared with all tested materials, reaching statistically significant differences at all follow-up points [52,63,69,74,81,89].
The introduction of calcium-silicate-based cements (such as Biodentine) appears to be promising for VTP. Indeed, calcium-silicate-based cements seem to play a central role in regenerative endodontics, inducing pulp regeneration, healing and dentin formation [96]. The present review confirms the previously reported results [4,15], showing similar outcomes when MTA was compared to BD [52,56,57,58,59,60,61,62]. MTA and BD may be classified as bioactive endodontic cements, due to their bioactivity feature, despite the differences in their chemical compositions [15]. The encouraging clinical properties as well as biocompatibility of calcium-silicate-based cements indicate that they can be considered as a suitable alternative to MTA for pulpotomies in primary molars. However, these preliminary results should be supported by further studies.
Limitations
The main limitation of the present systematic review was the high heterogeneity of the included studies. Although only randomized clinical comparative studies with at least 12 months of follow-up were evaluated, the lack of univocal standard procedures made difficult a precise comparison of the data. Moreover, the use of several materials composition as well as slightly different outcomes evaluation provided high variability in the interpretation of the results and could let to a misjudgment in the Conclusions. Due to this reason, some “confounding” materials reported by several included studies, such as sodium hypochlorite [84], Er:YAG laser [81], diode laser [79] and low level laser therapy [89], were excluded in the evaluation of pulpotomy dressing agents.
It should be further considered the high variability given by the type of restoration material used, although definitive, its interaction with the pulpotomy agent as well as the inconstant time between the pulpotomy treatment and the physiological exfoliation of the same tooth, that would render very hard to establish the success of pulpotomy procedure over time.
The quality assessment of the included studies showed an overall high risk of bias, mainly in blinding of participants and personnel, followed by blinding of outcome assessment. This aspect highlighted the inadequacies in the published studies, as previously reported by Gopalakrishnan et al. [97]. High quality study design and standardized clinical and radiographical protocols are needed to prospectively assess the performances of pulpotomy medicaments used in deciduous teeth.
5. Conclusions
Within the limitation of the present systematic review, MTA seemed to be the gold standard material in the pulpotomy of primary teeth. Promising results were also provided by BD. On the contrary, CH should be firmly avoided during pulpotomy procedures. Further RCT studies with adequate sample sizes and long follow-ups are encouraged to confirm these outcomes.
Author Contributions
Conceptualization, M.B. and F.I.; methodology, G.D.G.; validation, M.B., F.I. and G.D.G.; investigation, A.S.; data curation, G.D.G.; writing – original draft preparation, F.I.; writing – review & editing, A.P.; supervision, S.D.C. All authors have read and agreed to the published version of the manuscript.
Funding
The authors deny any sources of funding.
Conflicts of Interest
The authors declare no conflict of interest.
References
- US Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health. Oral Health in America: A Report of the Surgeon General; U.S. Department of Health and Human Services, National Institute of Dental and Craniofacial Research, National Institutes of Health: Rockville, MD, USA, 2000. Available online: https://www.nidcr.niih.gov/sites/default/files/2017-10/hck1ocv.%40www.surgeon.fullrpt.pdf (accessed on 2 December 2019).
- Smaïl-Faugeron, V.; Glenny, A.M.; Courson, F.; Durieux, P.; Muller-Bolla, M.; Fron Chabouis, H. Pulp treatment for extensive decay in primary teeth. Cochrane Database Syst. Rev. 2018, 5, CD003220. [Google Scholar]
- GBD 2016 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 328 diseases and injuries for 195 countries, 1990–2016: A systematic analysis for the Global Burden of Disease Study 2016. Lancet 2017, 390, 1211–1259. [Google Scholar] [CrossRef]
- Stringhini Junior, E.; Dos Santos, M.G.C.; Oliveira, L.B.; Mercadé, M. MTA and biodentine for primary teeth pulpotomy: A systematic review and meta-analysis of clinical trials. Clin. Oral Investig. 2019, 23, 1967–1976. [Google Scholar] [CrossRef] [PubMed]
- Bhujel, N.; Duggal, M.S.; Saini, P.; Day, P.F. The effect of premature extraction of primary teeth on the subsequent need for orthodontic treatment. Eur. Arch. Paediatr. Dent. 2016, 17, 423–434. [Google Scholar] [CrossRef]
- American Academy on Pediatric Dentistry; American Academy of Pediatrics. Policy on early childhood caries (ECC): Classifications, consequences, and preventive strategies. Pediatr. Dent. 2008, 30, 40–43. [Google Scholar]
- Dhar, V.; Marghalani, A.A.; Crystal, Y.O.; Kumar, A.; Ritwik, P.; Tulunoglu, O.; Graham, L. Use of vital pulp therapies in primary teeth with deep caries lesions. Pediatr. Dent. 2017, 39, E146–E159. [Google Scholar]
- American Academy on Pediatric Dentistry. Pulp Therapy for Primary and Immature Permanent Teeth. Pediatr. Dent. 2017, 39, 325–333. [Google Scholar]
- Brizuela, C.; Ormeño, A.; Cabrera, C.; Cabezas, R.; Silva, C.I.; Ramírez, V.; Mercade, M. Direct pulp capping with calcium hydroxide, mineral trioxide aggregate, and biodentine in permanent young teeth with caries: A randomized clinical trial. J. Endod. 2017, 43, 1776–1780. [Google Scholar] [CrossRef]
- Li, Z.; Cao, L.; Fan, M.; Xu, Q. Direct pulp capping with calcium hydroxide or mineral trioxide aggregate: A meta-analysis. J. Endod. 2015, 41, 1412–1417. [Google Scholar] [CrossRef]
- Smaïl-Faugeron, V.; Porot, A.; Muller-Bolla, M.; Courson, F. Indirect pulp capping versus pulpotomy for treating deep carious lesions approaching the pulp in primary teeth: A systematic review. Eur. J. Paediatr. Dent. 2016, 17, 107–112. [Google Scholar]
- Omar, S. MTA, formocresol, and ferric sulfate have significantly better clinical and radiographic outcomes than calcium hydroxide and laser therapies in primary molar pulpotomies after 18-24 months. J. Evid. Based Dent. Pract. 2015, 15, 58–60. [Google Scholar] [CrossRef] [PubMed]
- Stringhini Junior, E.; Vitcel, M.E.; Oliveira, L.B. Evidence of pulpotomy in primary teeth comparing MTA, calcium hydroxide, ferric sulphate, and electrosurgery with formocresol. Eur. Arch. Paediatr. Dent. 2015, 16, 303–312. [Google Scholar] [CrossRef] [PubMed]
- Asgary, S.; Shirvani, A.; Fazlyab, M. MTA and ferric sulfate in pulpotomy outcomes of primary molars: A systematic review and meta-analysis. J. Clin. Pediatr. Dent. 2014, 39, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Parirokh, M.; Torabinejad, M.; Dummer, P.M.H. Mineral trioxide aggregate and other bioactive endodontic cements: An updated overview - part I: Vital pulp therapy. Int. Endod. J. 2018, 51, 177–205. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int. J. Surg. 2010, 8, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0; The Cochrane Collaboration: 2011. Available online: http://training.cochrane.org/handbook/archive/v5.1/ (accessed on 24 October 2019).
- Kathal, S.; Gupta, S.; Bhayya, D.P.; Rao, A.; Roy, A.P.; Sabhlok, A. A comparative evaluation of clinical and radiographic success rate of pulpotomy in primary molars using antioxidant mix and mineral trioxide aggregate: An in vivo 1-year follow-up study. J. Indian Soc. Pedod. Prev. Dent. 2017, 35, 327–331. [Google Scholar] [CrossRef]
- Alsanouni, M.; Bawazir, O.A. A randomized clinical trial of neomta plus in primary molar pulpotomies. Pediatr. Dent. 2019, 41, 107–111. [Google Scholar]
- Pratima, B.; Chandan, G.D.; Nidhi, T.; Nitish, I.; Sankriti, M.; Nagaveni, S.; Shweta, S. Postoperative assessment of diode laser zinc oxide eugenol and mineral trioxide aggregate pulpotomy procedures in children: A comparative clinical study. J. Indian Soc. Pedod. Prev. Dent. 2018, 36, 308–314. [Google Scholar] [CrossRef]
- Kang, C.M.; Kim, S.H.; Shin, Y.; Lee, H.S.; Lee, J.H.; Kim, G.T.; Song, J.S. A randomized controlled trial of ProRoot MTA, OrthoMTA and RetroMTA for pulpotomy in primary molars. Oral. Dis. 2015, 21, 785–791. [Google Scholar] [CrossRef]
- Akcay, M.; Sari, S. The effect of sodium hypochlorite application on the success of calcium hydroxide and mineral trioxide aggregate pulpotomies in primary teeth. Pediatr. Dent. 2014, 36, 316–321. [Google Scholar]
- Fernández, C.C.; Martínez, S.S.; Jimeno, F.G.; Lorente Rodríguez, A.I.; Mercadé, M. Clinical and radiographic outcomes of the use of four dressing materials in pulpotomized primary molars: A randomized clinical trial with 2-year follow-up. Int. J. Paediatr. Dent. 2013, 23, 400–407. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Zhou, Q.; Qin, M. Mineral trioxide aggregate versus calcium hydroxide for pulpotomy in primary molars. Chin. J. Dent. Res. 2011, 14, 121–125. [Google Scholar]
- Holan, G.; Eidelman, E.; Fuks, A.B. Long-term evaluation of pulpotomy in primary molars using mineral trioxide aggregate or formocresol. Pediatr. Dent. 2005, 27, 129–136. [Google Scholar] [PubMed]
- Nematollahi, H.; Noorollahian, H.; Bagherian, A.; Yarbakht, M.; Nematollahi, S. Mineral trioxide aggregate partial pulpotomy versus formocresol pulpotomy: A randomized, split-mouth, controlled clinical trial with 24 months follow-up. Pediatr. Dent. 2018, 40, 184–189. [Google Scholar] [PubMed]
- Musale, P.K.; Soni, A.S. Clinical pulpotomy trial of copaifera langsdorffii oil resin versus formocresol and white mineral trioxide aggregate in primary teeth. Pediatr. Dent. 2016, 38, 5–12. [Google Scholar] [PubMed]
- Atasever, G.; Keceli, T.I.; Uysal, S.; Gungor, H.C.; Olmez, S. Primary molar pulpotomies with different hemorrhage control agents and base materials: A randomized clinical trial. Niger J. Clin. Pract. 2019, 22, 305–312. [Google Scholar] [PubMed]
- Huth, K.C.; Paschos, E.; Hajek-Al-Khatar, N.; Hollweck, R.; Crispin, A.; Hickel, R.; Folwaczny, M. Effectiveness of 4 pulpotomy techniques--randomized controlled trial. J. Dent. Res. 2005, 84, 1144–1148. [Google Scholar] [CrossRef]
- Nguyen, T.D.; Judd, P.L.; Barrett, E.J.; Sidhu, N.; Casas, M.J. Comparison of ferric sulfate combined mineral trioxide aggregate pulpotomy and zinc oxide eugenol pulpectomy of primary maxillary incisors: An 18-month randomized, controlled trial. Pediatr. Dent. 2017, 39, 34–38. [Google Scholar]
- Saltzman, B.; Sigal, M.; Clokie, C.; Rukavina, J.; Titley, K.; Kulkarni, G.V. Assessment of a novel alternative to conventional formocresol-zinc oxide eugenol pulpotomy for the treatment of pulpally involved human primary teeth: Diode laser-mineral trioxide aggregate pulpotomy. Int. J. Paediatr. Dent. 2005, 15, 437–447. [Google Scholar] [CrossRef]
- Grewal, N.; Salhan, R.; Kaur, N.; Patel, H.B. Comparative evaluation of calcium silicate-based dentin substitute (Biodentine®) and calcium hydroxide (pulpdent) in the formation of reactive dentin bridge in regenerative pulpotomy of vital primary teeth: Triple blind, randomized clinical trial. Contemp. Clin. Dent. 2016, 7, 457–463. [Google Scholar] [CrossRef]
- Hugar, S.M.; Kukreja, P.; Hugar, S.S.; Gokhale, N.; Assudani, H. Comparative evaluation of clinical and radiographic success of formocresol, propolis, turmeric gel, and calcium hydroxide on pulpotomized primary molars: A preliminary study. Int. J. Clin. Pediatr. Dent. 2017, 10, 18–23. [Google Scholar] [CrossRef] [PubMed]
- Kalra, M.; Garg, N.; Rallan, M.; Pathivada, L.; Yeluri, R. Comparative evaluation of fresh aloe barbadensis plant extract and mineral trioxide aggregate as pulpotomy agents in primary molars: A 12-month follow-up study. Contemp. Clin. Dent. 2017, 8, 106–111. [Google Scholar]
- Uloopi, K.S.; Vinay, C.; Ratnaditya, A.; Gopal, A.S.; Mrudula, K.J.; Rao, R.C. Clinical evaluation of low level diode laser application for primary teeth pulpotomy. J. Clin. Diagn Res. 2016, 10, ZC67–ZC70. [Google Scholar] [CrossRef] [PubMed]
- Yildiz, E.; Tosun, G. Evaluation of formocresol, calcium hydroxide, ferric sulfate, and MTA primary molar pulpotomies. Eur. J. Dent. 2014, 8, 234–240. [Google Scholar] [CrossRef] [PubMed]
- Ansari, G.; Morovati, S.P.; Asgary, S. Evaluation of four pulpotomy techniques in primary molars: A randomized controlled trial. Iran Endod. J. 2018, 13, 7–12. [Google Scholar] [PubMed]
- Gupta, G.; Rana, V.; Srivastava, N.; Chandna, P. Laser pulpotomy-an effective alternative to conventional techniques: A 12 months clinicoradiographic study. Int. J. Clin. Pediatr. Dent. 2015, 8, 18–21. [Google Scholar] [PubMed]
- Cantekin, K.; Gümüş, H. Success rates of ankaferd blood stopper and ferric sulfate as pulpotomy agents in primary molars. Int. Sch. Res. Notices 2014, 2014, 819605. [Google Scholar] [CrossRef]
- Trairatvorakul, C.; Koothiratrakarn, A. Calcium hydroxide partial pulpotomy is an alternative to formocresol pulpotomy based on a 3-year randomized trial. Int. J. Paediatr. Dent 2012, 22, 382–389. [Google Scholar] [CrossRef]
- Zurn, D.; Seale, N.S. Light-cured calcium hydroxide vs. formocresol in human primary molar pulpotomies: A randomized controlled trial. Pediatr. Dent 2008, 30, 34–41. [Google Scholar]
- Percinoto, C.; de Castro, A.M.; Pinto, L.M. Clinical and radiographic evaluation of pulpotomies employing calcium hydroxide and trioxide mineral aggregate. Gen Dent 2006, 54, 258–261. [Google Scholar]
- Ghoniem, N.; Vaidyanathan, V.; Zealand, C.M.; Sushynski, J.M.; Mettlach, S.M.; Botero, T.M.; Majewski, R.F.; Boynton, J.R.; Hu, J.C. Mineral trioxide aggregate and diluted formocresol pulpotomy: Prospective and retrospective study outcomes. J. Mich. Dent. Assoc. 2018, 100, 40–65. [Google Scholar]
- Biedma Perea, M.; Solano Mendoza, B.; Garcia-Godoy, F.; Mendoza Mendoza, A.; Iglesias-Linares, A. Clinical and radiographic evaluation of white MTA versus formocresol pulpotomy: A 48-month follow-up study. Am. J. Dent. 2017, 30, 131–136. [Google Scholar] [PubMed]
- Airen, P.; Shigli, A.; Airen, B. Comparative evaluation of formocresol and mineral trioxide aggregate in pulpotomized primary molars--2 year follow up. J. Clin. Pediatr. Dent. 2012, 37, 143–147. [Google Scholar] [CrossRef] [PubMed]
- Frenkel, G.; Kaufman, A.; Ashkenazi, M. Clinical and radiographic outcomes of pulpotomized primary molars treated with white or gray mineral trioxide aggregate and ferric sulfate--long-term follow-up. J. Clin. Pediatr. Dent. 2012, 37, 137–141. [Google Scholar] [CrossRef] [PubMed]
- Cardoso-Silva, C.; Barbería, E.; Maroto, M.; García-Godoy, F. Clinical study of Mineral Trioxide Aggregate in primary molars. Comparison between Grey and White MTA--a long term follow-up (84 months). J. Dent. 2011, 39, 187–193. [Google Scholar] [CrossRef]
- Ibricevic, H.; Al-Jame, Q. Ferric sulphate and formocresol in pulpotomy of primary molars: Long term follow-up study. Eur. J. Paediatr. Dent. 2003, 4, 28–32. [Google Scholar] [PubMed]
- Godhi, B.; Tyagi, R. Success rate of MTA pulpotomy on vital pulp of primary molars: A 3-year observational study. Int. J. Clin. Pediatr. Dent. 2016, 9, 222–227. [Google Scholar] [CrossRef]
- Hugar, S.M.; Deshpande, S.D. Comparative investigation of clinical/radiographical signs of mineral trioxide aggregate and formocresol on pulpotomized primary molars. Contemp. Clin. Dent. 2010, 1, 146–151. [Google Scholar] [CrossRef]
- Ibricevic, H.; Al-Jame, Q. Ferric sulfate as pulpotomy agent in primary teeth: Twenty month clinical follow-up. J. Clin. Pediatr. Dent. 2000, 24, 269–272. [Google Scholar] [CrossRef]
- Çelik, B.N.; Mutluay, M.S.; Arıkan, V.; Sarı, Ş. The evaluation of MTA and Biodentine as a pulpotomy materials for carious exposures in primary teeth. Clin. Oral Investig. 2019, 23, 661–666. [Google Scholar] [CrossRef]
- Malekafzali, B.; Shekarchi, F.; Asgary, S. Treatment outcomes of pulpotomy in primary molars using two endodontic biomaterials. A 2-year randomised clinical trial. Eur. J. Paediatr. Dent. 2011, 12, 189–193. [Google Scholar] [PubMed]
- Sakai, V.T.; Moretti, A.B.; Oliveira, T.M.; Fornetti, A.P.; Santos, C.F.; Machado, M.A.; Abdo, R.C. Pulpotomy of human primary molars with MTA and Portland cement: A randomised controlled trial. Br. Dent. J. 2009, 207, 128–129. [Google Scholar] [CrossRef] [PubMed]
- Farsi, N.; Alamoudi, N.; Balto, K.; Mushayt, A. Success of mineral trioxide aggregate in pulpotomized primary molars. J. Clin. Pediatr. Dent. 2005, 29, 307–311. [Google Scholar] [CrossRef]
- Carti, O.; Oznurhan, F. Evaluation and comparison of mineral trioxide aggregate and biodentine in primary tooth pulpotomy: Clinical and radiographic study. Niger J. Clin. Pract. 2017, 20, 1604–1609. [Google Scholar] [PubMed]
- Guven, Y.; Aksakal, S.D.; Avcu, N.; Unsal, G.; Tuna, E.B.; Aktoren, O. Success rates of pulpotomies in primary molars using calcium silicate-based materials: A randomized control trial. Biomed. Res. Int. 2017, 2017, 4059703. [Google Scholar] [CrossRef] [PubMed]
- Bani, M.; Aktaş, N.; Çınar, Ç.; Odabaş, M.E. The clinical and radiographic success of primary molar pulpotomy using Biodentine™ and mineral trioxide aggregate: A 24-month randomized clinical trial. Pediatr. Dent. 2017, 39, 284–288. [Google Scholar]
- Juneja, P.; Kulkarni, S. Clinical and radiographic comparison of biodentine, mineral trioxide aggregate and formocresol as pulpotomy agents in primary molars. Eur. Arch. Paediatr. Dent. 2017, 18, 271–278. [Google Scholar] [CrossRef]
- Togaru, H.; Muppa, R.; Srinivas, N.; Naveen, K.; Reddy, V.K.; Rebecca, V.C. Clinical and radiographic evaluation of success of two commercially available pulpotomy agents in primary teeth: An in vivo study. J. Contemp. Dent. Pract. 2016, 17, 557–563. [Google Scholar]
- Rajasekharan, S.; Martens, L.C.; Vandenbulcke, J.; Jacquet, W.; Bottenberg, P.; Cauwels, R.G. Efficacy of three different pulpotomy agents in primary molars: A randomized control trial. Int. Endod. J. 2017, 50, 215–228. [Google Scholar] [CrossRef]
- Cuadros-Fernández, C.; Lorente Rodríguez, A.I.; Sáez-Martínez, S.; García-Binimelis, J.; About, I.; Mercadé, M. Short-term treatment outcome of pulpotomies in primary molars using mineral trioxide aggregate and Biodentine: A randomized clinical trial. Clin. Oral Investig. 2016, 20, 1639–1645. [Google Scholar] [CrossRef]
- Silva, L.L.C.E.; Cosme-Silva, L.; Sakai, V.T.; Lopes, C.S.; Silveira, A.P.P.D.; Moretti Neto, R.T.; Gomes-Filho, J.E.; Oliveira, T.M.; Moretti, A.B.D.S. Comparison between calcium hydroxide mixtures and mineral trioxide aggregate in primary teeth pulpotomy: A randomized controlled trial. J. Appl. Oral Sci. 2019, 27, e20180030. [Google Scholar] [CrossRef] [PubMed]
- Junqueira, M.A.; Cunha, N.N.O.; Caixeta, F.F.; Marques, N.C.T.; Oliveira, T.M.; Moretti, A.B.D.S.; Cosme-Silva, L.; Sakai, V.T. Clinical, radiographic and histological evaluation of primary teeth pulpotomy using MTA and ferric sulfate. Braz. Dent. J. 2018, 29, 159–165. [Google Scholar] [CrossRef] [PubMed]
- Jamali, Z.; Alavi, V.; Najafpour, E.; Aminabadi, N.A.; Shirazi, S. Randomized controlled trial of pulpotomy in primary molars using MTA and formocresol compared to 3Mixtatin: A novel biomaterial. J. Clin. Pediatr. Dent. 2018, 42, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Yildirim, C.; Basak, F.; Akgun, O.M.; Polat, G.G.; Altun, C. Clinical and radiographic evaluation of the effectiveness of formocresol, mineral trioxide aggregate, portland cement, and enamel matrix derivative in primary teeth pulpotomies: A two year follow-up. J. Clin. Pediatr. Dent. 2016, 40, 14–20. [Google Scholar] [CrossRef] [PubMed]
- Olatosi, O.O.; Sote, E.O.; Orenuga, O.O. Effect of mineral trioxide aggregate and formocresol pulpotomy on vital primary teeth: A clinical and radiographic study. Niger J. Clin. Pract. 2015, 18, 292–296. [Google Scholar] [CrossRef] [PubMed]
- Celik, B.; Ataç, A.S.; Cehreli, Z.C.; Uysal, S. A randomized trial of mineral trioxide aggregate cements in primary tooth pulpotomies. J. Dent. Child (Chic) 2013, 80, 126–132. [Google Scholar]
- Oliveira, T.M.; Moretti, A.B.; Sakai, V.T.; Lourenço Neto, N.; Santos, C.F.; Machado, M.A.; Abdo, R.C. Clinical, radiographic and histologic analysis of the effects of pulp capping materials used in pulpotomies of human primary teeth. Eur. Arch. Paediatr. Dent 2013, 14, 65–71. [Google Scholar] [CrossRef]
- Sushynski, J.M.; Zealand, C.M.; Botero, T.M.; Boynton, J.R.; Majewski, R.F.; Shelburne, C.E.; Hu, J.C. Comparison of gray mineral trioxide aggregate and diluted formocresol in pulpotomized primary molars: A 6- to 24-month observation. Pediatr. Dent 2012, 34, 120–128. [Google Scholar]
- Erdem, A.P.; Guven, Y.; Balli, B.; Ilhan, B.; Sepet, E.; Ulukapi, I.; Aktoren, O. Success rates of mineral trioxide aggregate, ferric sulfate, and formocresol pulpotomies: A 24-month study. Pediatr. Dent. 2011, 33, 165–170. [Google Scholar]
- Ansari, G.; Ranjpour, M. Mineral trioxide aggregate and formocresol pulpotomy of primary teeth: A 2-year follow-up. Int. Endod. J. 2010, 43, 413–418. [Google Scholar] [CrossRef]
- Doyle, T.L.; Casas, M.J.; Kenny, D.J.; Judd, P.L. Mineral trioxide aggregate produces superior outcomes in vital primary molar pulpotomy. Pediatr. Dent. 2010, 32, 41–47. [Google Scholar] [PubMed]
- Moretti, A.B.; Sakai, V.T.; Oliveira, T.M.; Fornetti, A.P.; Santos, C.F.; Machado, M.A.; Abdo, R.C. The effectiveness of mineral trioxide aggregate, calcium hydroxide and formocresol for pulpotomies in primary teeth. Int. Endod. J. 2008, 41, 547–555. [Google Scholar] [CrossRef] [PubMed]
- Noorollahian, H. Comparison of mineral trioxide aggregate and formocresol as pulp medicaments for pulpotomies in primary molars. Br. Dent. J. 2008, 204, E20. [Google Scholar] [CrossRef] [PubMed]
- Agamy, H.A.; Bakry, N.S.; Mounir, M.M.; Avery, D.R. Comparison of mineral trioxide aggregate and formocresol as pulp-capping agents in pulpotomized primary teeth. Pediatr. Dent. 2004, 26, 302–309. [Google Scholar]
- Eidelman, E.; Holan, G.; Fuks, A.B. Mineral trioxide aggregate vs. formocresol in pulpotomized primary molars: A preliminary report. Pediatr. Dent. 2001, 23, 15–18. [Google Scholar]
- Mettlach, S.E.; Zealand, C.M.; Botero, T.M.; Boynton, J.R.; Majewski, R.F.; Hu, J.C. Comparison of mineral trioxide aggregate and diluted formocresol in pulpotomized human primary molars: 42-month follow-up and survival analysis. Pediatr. Dent. 2013, 35, E87–E94. [Google Scholar]
- Durmus, B.; Tanboga, I. In vivo evaluation of the treatment outcome of pulpotomy in primary molars using diode laser, formocresol, and ferric sulphate. Photomed. Laser Surg. 2014, 32, 289–295. [Google Scholar] [CrossRef]
- Havale, R.; Anegundi, R.T.; Indushekar, K.; Sudha, P. Clinical and radiographic evaluation of pulpotomies in primary molars with formocresol, glutaraldehyde and ferric sulphate. Oral Health Dent. Manag. 2013, 12, 24–31. [Google Scholar]
- Huth, K.C.; Hajek-Al-Khatar, N.; Wolf, P.; Ilie, N.; Hickel, R.; Paschos, E. Long-term effectiveness of four pulpotomy techniques: 3-year randomised controlled trial. Clin. Oral Investig. 2012, 16, 1243–1250. [Google Scholar] [CrossRef]
- Markovic, D.; Zivojinovic, V.; Vucetic, M. Evaluation of three pulpotomy medicaments in primary teeth. Eur. J. Paediatr. Dent. 2005, 6, 133–138. [Google Scholar]
- Ozmen, B.; Bayrak, S. Comparative evaluation of ankaferd blood stopper, ferric sulfate, and formocresol as pulpotomy agent in primary teeth: A clinical study. Niger J. Clin. Pract. 2017, 20, 832–838. [Google Scholar] [CrossRef] [PubMed]
- Farsi, D.J.; El-Khodary, H.M.; Farsi, N.M.; El Ashiry, E.A.; Yagmoor, M.A.; Alzain, S.M. Sodium hypochlorite versus formocresol and ferric sulfate pulpotomies in primary molars: 18-month follow-up. Pediatr. Dent. 2015, 37, 535–540. [Google Scholar] [PubMed]
- Jayam, C.; Mitra, M.; Mishra, J.; Bhattacharya, B.; Jana, B. Evaluation and comparison of white mineral trioxide aggregate and formocresol medicaments in primary tooth pulpotomy: Clinical and radiographic study. J. Indian Soc. Pedod. Prev. Dent. 2014, 32, 13–18. [Google Scholar] [CrossRef]
- Srinivasan, D.; Jayanthi, M. Comparative evaluation of formocresol and mineral trioxide aggregate as pulpotomy agents in deciduous teeth. Indian J. Dent. Res. 2011, 22, 385–390. [Google Scholar] [CrossRef] [PubMed]
- El Meligy, O.A.E.S.; Alamoudi, N.M.; Allazzam, S.M.; El-Housseiny, A.A.M. BiodentineTM versus formocresol pulpotomy technique in primary molars: A 12-month randomized controlled clinical trial. BMC Oral Health 2019, 19, 3. [Google Scholar] [CrossRef] [PubMed]
- Sunitha, B.; Puppala, R.; Kethineni, B.K.; Mallela, M.; Peddi, R.; Tarasingh, P. Clinical and radiographic evaluation of four different pulpotomy agents in primary molars: A longitudinal study. Int. J. Clin. Pediatr. Dent. 2017, 10, 240–244. [Google Scholar]
- Fernandes, A.P.; Lourenço Neto, N.; Teixeira Marques, N.C.; Silveira Moretti, A.B.; Sakai, V.T.; Cruvinel Silva, T.; Andrade Moreira Machado, M.A.; Marchini Oliveira, T. Clinical and radiographic outcomes of the use of Low-Level Laser Therapy in vital pulp of primary teeth. Int. J. Paediatr. Dent. 2015, 25, 144–150. [Google Scholar] [CrossRef]
- Subramaniam, P.; Konde, S.; Mathew, S.; Sugnani, S. Mineral trioxide aggregate as pulp capping agent for primary teeth pulpotomy: 2 year follow up study. J. Clin. Pediatr. Dent. 2009, 33, 311–314. [Google Scholar] [CrossRef]
- Sonmez, D.; Sari, S.; Cetinbaş, T. A Comparison of four pulpotomy techniques in primary molars: A long-term follow-up. J. Endod. 2008, 34, 950–955. [Google Scholar] [CrossRef]
- Fuks, A.B.; Holan, G.; Davis, J.M.; Eidelman, E. Ferric sulfate versus dilute formocresol in pulpotomized primary molars: Long-term follow up. Pediatr. Dent. 1997, 19, 327–330. [Google Scholar]
- International Agency for Research on Cancer. Pres Release no. 153. 15 June. Available online: www.iarc.fr/ENG/Press_Releases/archives/ pr153a.html (accessed on 16 March 2020).
- Coll, J.A.; Seale, N.S.; Vargas, K.; Marghalani, A.A.; Al Shamali, S.; Graham, L. Primary tooth vital pulp therapy: A systematic review and meta-analysis. Pediatr. Dent. 2017, 39, 16–123. [Google Scholar] [PubMed]
- Lin, P.Y.; Chen, H.S.; Wang, Y.H.; Tu, Y.K. Primary molar pulpotomy: A systematic review and network meta-analysis. J. Dent. 2014, 42, 1060–1077. [Google Scholar] [CrossRef] [PubMed]
- Gandolfi, M.G.; Spagnuolo, G.; Siboni, F.; Procino, A.; Rivieccio, V.; Pelliccioni, G.A.; Prati, C.; Rengo, S. Calcium silicate/calcium phosphate biphasic cements for vital pulp therapy: Chemical-physical properties and human pulp cells response. Clin. Oral. Investig. 2015, 19, 2075–2089. [Google Scholar] [CrossRef] [PubMed]
- Gopalakrishnan, V.; Anthonappa, R.; Ekambaram, M.; King, N.M. Qualitative assessment of published studies on pulpotomy medicaments for primary molar teeth. J. Investig. Clin. Dent. 2019, 10, e12389. [Google Scholar] [CrossRef]
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).