Effect of Low Intensity Pulsed Ultrasound (LIPUS) on Tooth Movement and Root Resorption: A Prospective Multi-Center Randomized Controlled Trial
Abstract
1. Introduction
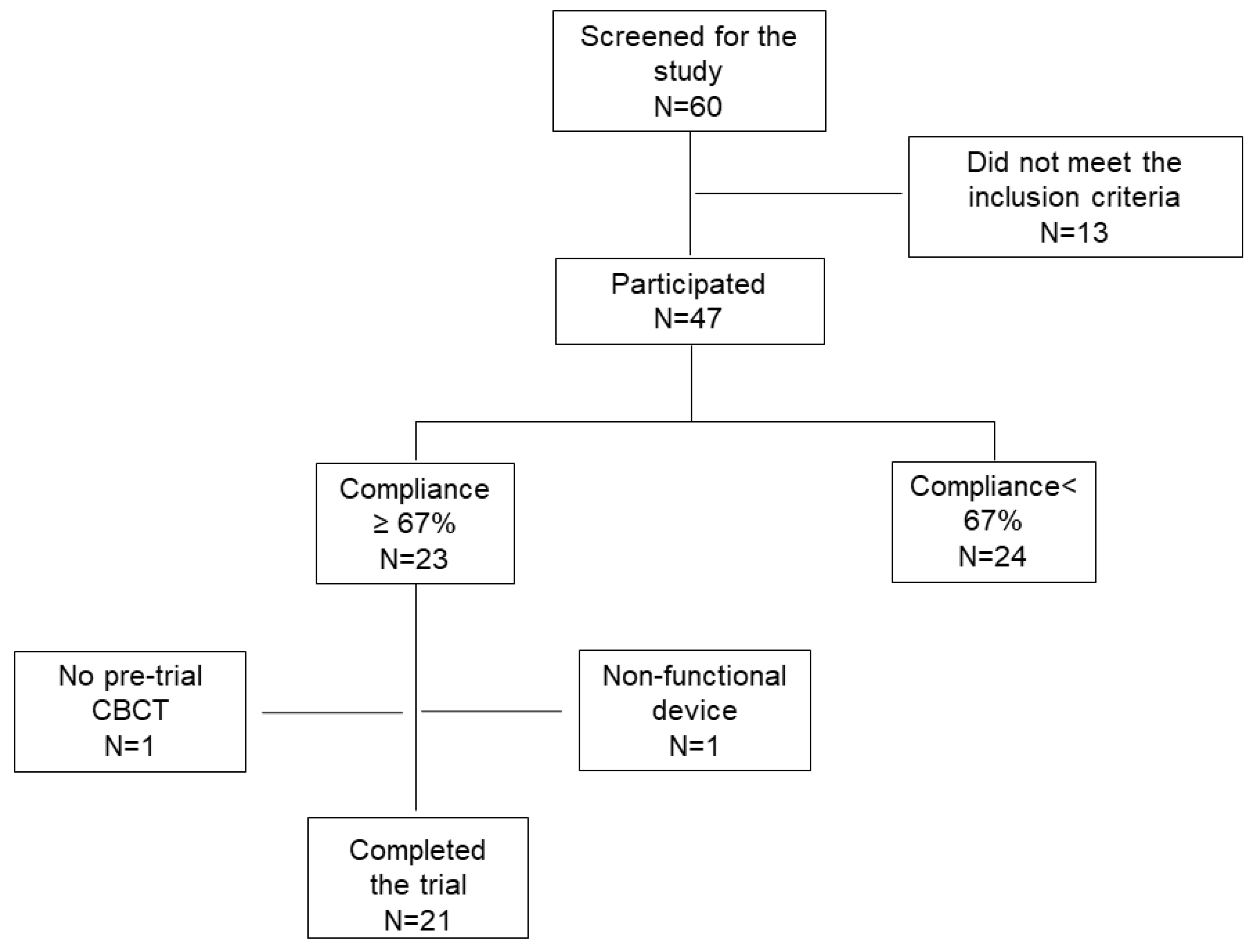
2. Experimental Section
- permanent dentition and ages between 12 and 40 years old;
- first premolar extractions indicated for correcting the existing dental malocclusion (to eliminate overjet or crowding) with a minimum of 3mm of extraction space;
- good oral hygiene and compliance; and,
- no history of systemic disease.
- any compromised medical or dental condition that prevents the subject from participating in the trial or using a medical device (like diabetes, renal failure, under corticosteroid treatment, etc.);
- any implanted assistive device e.g., pacemakers, cochlear implants, etc.;
- chronic use of medications affecting orthodontic tooth movement e.g., Bisphosphonate; and,
- pregnant females.
2.1. Sample Size Calculation
2.2. Ethics Approval and Consent to the Patients
2.3. Randomization
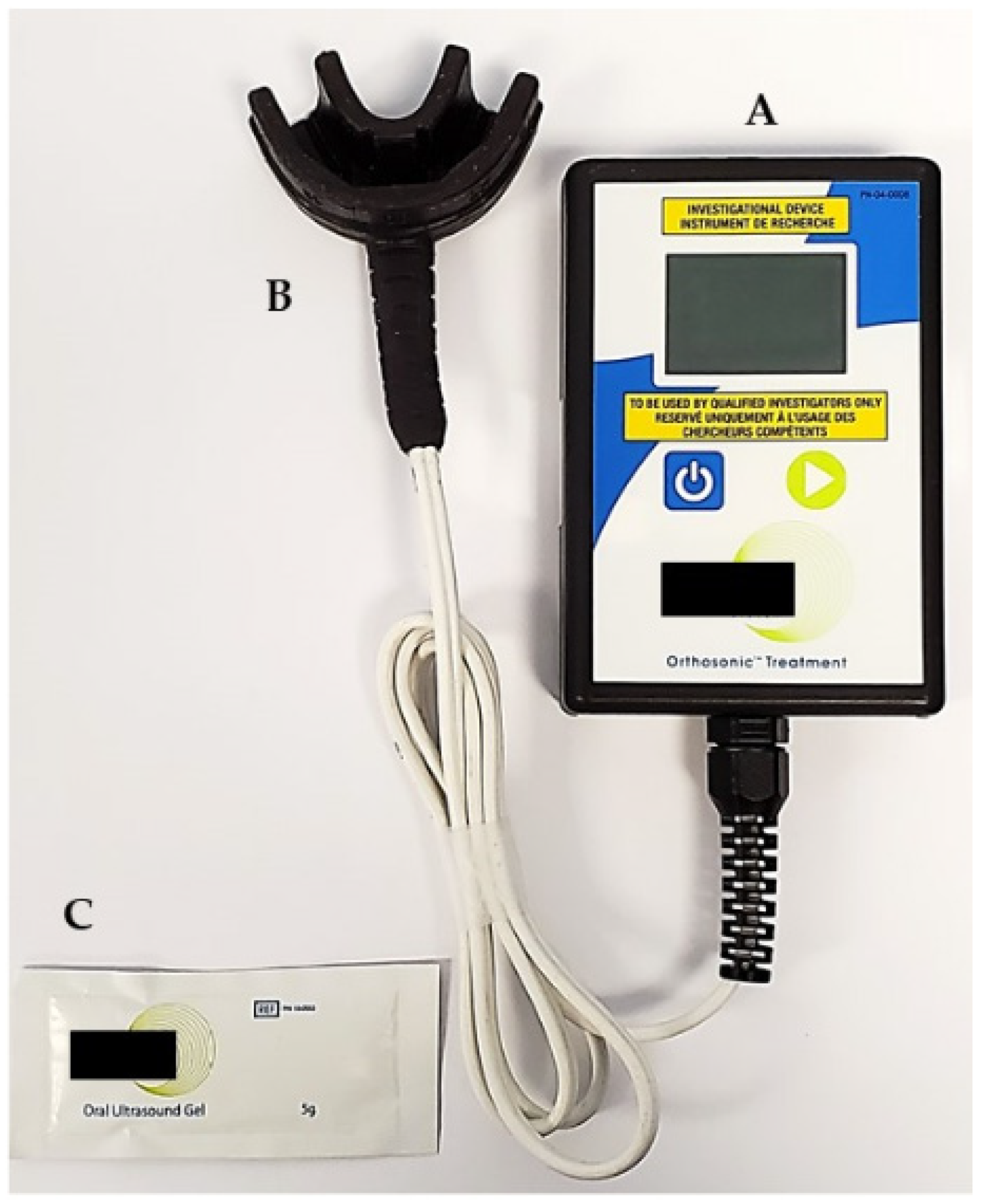
2.4. LIPUS Device
2.5. Intervention
2.6. Outcomes Assessment
2.6.1. Subject Compliance
2.6.2. Primary Outcome
- dCrown: the amount of tooth movement of the canine’s crown
- dRoot: the amount of tooth movement of the canine’s root apex
- dt0: the first extraction space measurement (from canine cusp tip to the mesiobuccal groove of the first molar);
- dt1: the last extraction space measurement prior to extraction space closure (i.e., extraction space = 0 mm) on either side; and,
- t: the number of weeks between dt0 and dt1.
- rUltrasound: Ultrasound tooth movement rate; and,
- rControl: Control tooth movement rate.
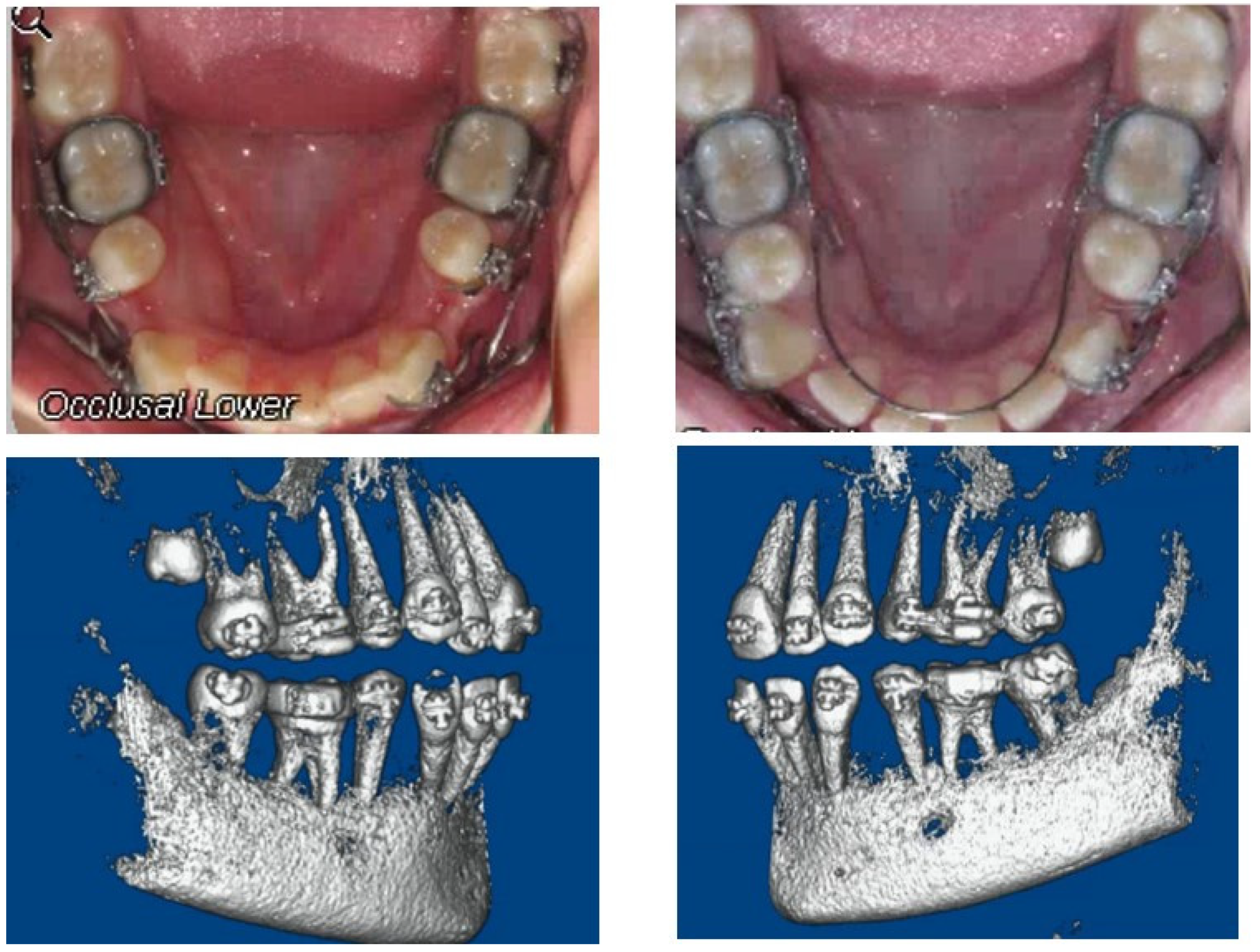
2.6.3. Secondary Outcome: Root Resorption Using CBCT
- l(pre-trial): the pre-trial tooth length;
- l(post-trial): the post-trial tooth length; and,
- t: the number of weeks between l(pre-trial) and l(post-trial).
- r Ultrasound: Ultrasound root resorption rate; and,
- r Control: Control root resorption rate.
2.7. Statistical Analysis
3. Results
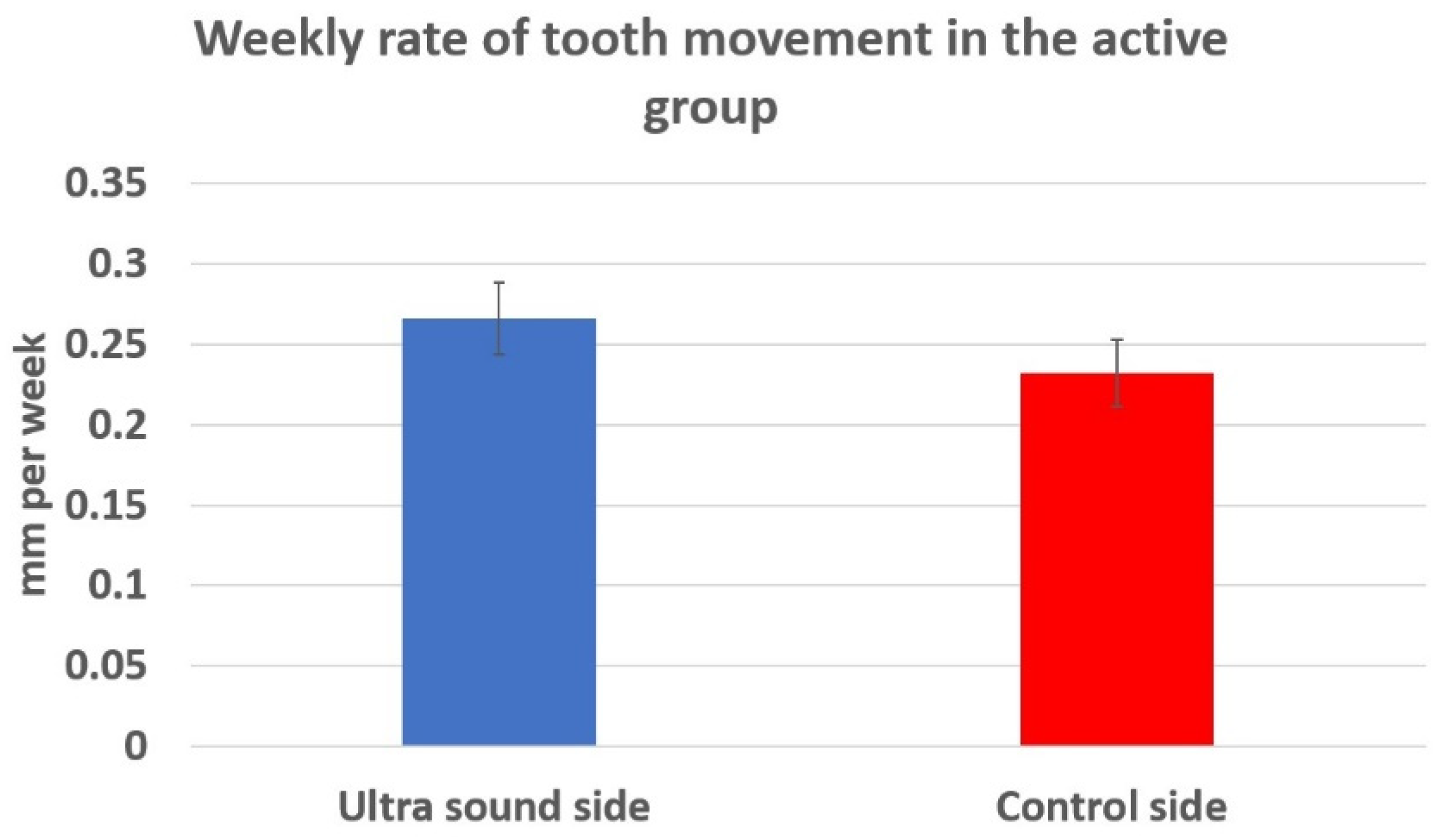
3.1. Tooth Movement Analysis
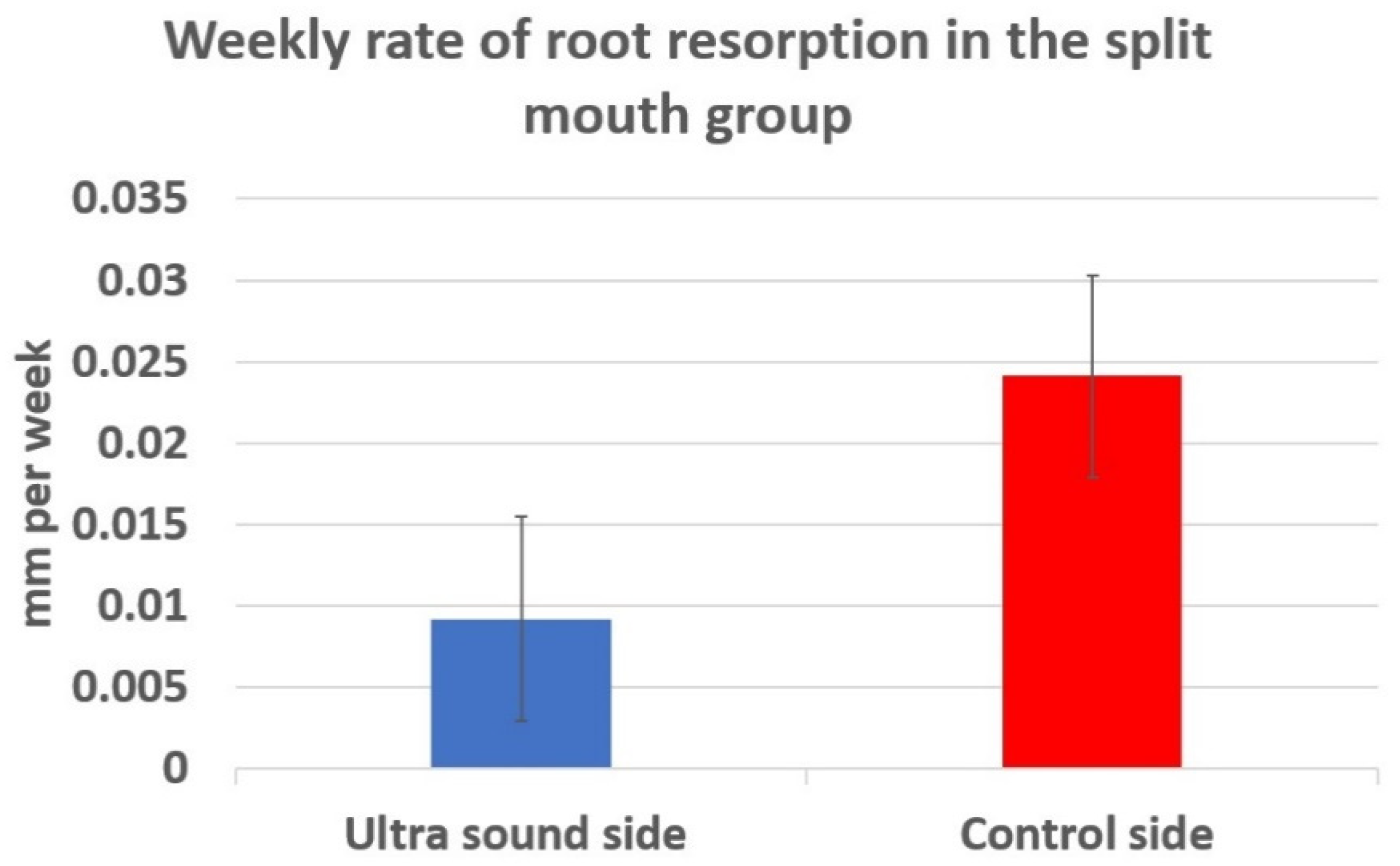
3.2. Root Resorption Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jung, M.H. Evaluation of the effects of malocclusion and orthodontic treatment on self-esteem in an adolescent population. Am. J. Orthod. Dentofacial. Orthop. 2010, 138, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Rusanen, J.; Lahti, S.; Tolvanen, M.; Pirttiniemi, P. Quality of life in patients with severe malocclusion before treatment. Eur. J. Orthod. 2010, 32, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Pabari, S.; Moles, D.R.; Cunningham, S.J. Assessment of motivation and psychological characteristics of adult orthodontic patients. Am. J. Orthod. Dentofacial. Orthop. 2011, 140, 263–272. [Google Scholar] [CrossRef] [PubMed]
- Sergl, H.G.; Zentner, A. Study of psychosocial aspects of adult orthodontic treatment. Int. J. Adult Orthodon. Orthognath. Surg. 1997, 12, 17–22. [Google Scholar]
- Bichara, L.M.; de Aragón, M.L.C.; Brandão, G.A.M.; Normando, D. Factors influencing orthodontic treatment time for non-surgical Class III malocclusion. J. Appl. Oral. Sci. 2016, 24, 431–436. [Google Scholar] [CrossRef]
- Skidmore, K.J.; Brook, K.J.; Thomson, W.M.; Harding, W.J. Factors influencing treatment time in orthodontic patients. Am. J. Orthod. Dentofacial. Orthop. 2006, 129, 230–238. [Google Scholar] [CrossRef]
- Long, H.; Pyakurel, U.; Wang, Y.; Liao, L.; Zhou, Y.; Lai, W. Interventions for accelerating orthodontic tooth movement: A systematic review. Angle Orthod. 2013, 83, 164–171. [Google Scholar] [CrossRef]
- Roykó, A.; Dénes, Z.; Razouk, G. The relationship between the length of orthodontic treatment and patient compliance. Fogorv. Sz 1999, 92, 79–86. [Google Scholar]
- Bishara, S.E.; Ostby, A.W. White spot lesions: Formation, prevention, and treatment. Semin. Orthod. 2008, 14, 174–182. [Google Scholar] [CrossRef]
- Pandis, N.; Nasika, M.; Polychronopoulou, A.; Eliades, T. External apical root resorption in patients treated with conventional and self-ligating brackets. Am. J. Orthod. Dentofacial. Orthop. 2008, 134, 646–651. [Google Scholar] [CrossRef]
- Yamaguchi, M.; Hayashi, M.; Fujita, S.; Yoshida, T.; Utsunomiya, T.; Yamamoto, H.; Kasai, K. Low-energy laser irradiation facilitates the velocity of tooth movement and the expressions of matrix metalloproteinase-9, cathepsin K, and alpha(v) beta(3) integrin in rats. Eur. J. Orthod. 2010, 32, 131–139. [Google Scholar] [CrossRef] [PubMed]
- Showkatbakhsh, R.; Jamilian, A.; Showkatbakhsh, M. The effect of pulsed electromagnetic fields on the acceleration of tooth movement. World J. Orthod. 2010, 11, 52–56. [Google Scholar]
- Kim, D.H.; Park, Y.G.; Kang, S.G. The effects of electrical current from a micro-electrical device on tooth movement. Korean J. Orthod. 2008, 38, 337. [Google Scholar] [CrossRef]
- Hassan, A.H.; Al-Fraidi, A.A.; Al-Saeed, S.H. Corticotomy-assisted orthodontic treatment: Review. Open Dent. J. 2010, 13, 159–164. [Google Scholar] [CrossRef]
- Işeri, H.; Kişnişci, R.; Bzizi, N.; Tüz, H. Rapid canine retraction and orthodontic treatment with dentoalveolar distraction osteogenesis. Am. J. Orthod. Dentofacial. Orthop. 2005, 127, 533–541. [Google Scholar] [CrossRef] [PubMed]
- Nishimura, M.; Chiba, M.; Ohashi, T.; Sato, M.; Shimizu, Y.; Igarashi, K.; Mitani, H. Periodontal tissue activation by vibration: Intermittent stimulation by resonance vibration accelerates experimental tooth movement in rats. Am. J. Orthod. Dentofacial. Orthop. 2008, 133, 572–583. [Google Scholar] [CrossRef] [PubMed]
- Ojima, K.; Dan, C.; Kumagai, Y.; Schupp, W. Invisalign treatment accelerated by photobiomodulation. J. Clin. Orthod. 2016, 50, 309–317. [Google Scholar] [PubMed]
- Isola, G.; Matarese, G.; Cordasco, G.; Perillo, L.; Ramaglia, L. Mechanobiology of the tooth movement during the orthodontic treatment: A literature review. Minerva Stomatol. 2016, 65, 299–327. [Google Scholar]
- Huang, H.; Williams, R.C.; Kyrkanides, S. Accelerated orthodontic tooth movement: Molecular mechanisms. Am. J. Orthod. Dentofacial. Orthop. 2014, 146, 620–632. [Google Scholar] [CrossRef]
- Tsesis, I.; Fuss, Z.; Rosenberg, E.; Taicher, S. Radiographic evaluation of the prevalence of root resorption in a Middle Eastern population. Quintessence Int. 2008, 39, 40–44. [Google Scholar]
- Machen, D.E. Legal aspects of orthodontic practice: Risk management concepts. Diagnosis, root resorption, and progress monitoring. Am. J. Orthod. Dentofacial. Orthop. 1989, 95, 267–268. [Google Scholar] [CrossRef]
- Franklin, E. Why orthodontists get sued. Semin. Orthod. 2002, 8, 210–215. [Google Scholar] [CrossRef]
- Lupi, J.E.; Handelman, C.S.; Sadowsky, C. Prevalence and severity of apical root resorption and alveolar bone loss in orthodontically treated adults. Am. J. Orthod. Dentofacial. Orthop. 1996, 109, 28–37. [Google Scholar] [CrossRef]
- Harris, E.F.; Boggan, B.W.; Wheeler, D.A. Apical root resorption in patients treated with comprehensive orthodontics. J. Tenn. Dent. Assoc. 2001, 81, 30–33. [Google Scholar]
- El-Bialy, T.; Lam, B.; Al-Daghreer, S.; Sloan, A.J. The effect of low intensity pulsed ultrasound in a 3D ex vivo orthodontic model. J. Dent. 2011, 39, 693–699. [Google Scholar] [CrossRef]
- Al-Daghreer, S.; Doschak, M.; Sloan, A.J.; Major, P.W.; Heo, G.; Scurtescu, C.; Tsui, Y.Y. Effect of low-intensity pulsed ultrasound on orthodontically induced root resorption in beagle dogs. Ultrasound Med. Biol. 2014, 40, 1187–1196. [Google Scholar] [CrossRef]
- Tanaka, E.; Kuroda, S.; Horiuchi, S.; Tabata, A.; El-Bialy, T. Low-intensity pulsed ultrasound in dentofacial tissue engineering. Ann. Biomed. Eng. 2015, 43, 871–886. [Google Scholar] [CrossRef] [PubMed]
- Salem, K.H.; Schmelz, A. Low-intensity pulsed ultrasound shortens the treatment time in tibial distraction osteogenesis. Int. Orthop. 2014, 38, 1477–1482. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Heckman, J.D.; Ryaby, J.P.; McCabe, J.; Frey, J.J.; Kilcoyne, R.F. Acceleration of tibial fracture-healing by non-invasive, low-intensity pulsed ultrasound. J. Bone Joint Surg. Am. 1994, 76, 26–34. [Google Scholar] [CrossRef]
- Maurya, R.K.; Singh, H.; Kapoor, P.; Jain, U.; Mitra, R. Effects of low-level laser and low-intensity pulsed ultrasound therapy on treatment duration and pain perception. J. Clin. Orthod. 2019, 53, 154–162. [Google Scholar]
- El-Bialy, T.H.; Royston, T.J.; Magin, R.L.; Evans, C.A.; Zaki, A.E.; Frizzell, L.A. The effect of pulsed ultrasound on mandibular distraction. Ann. Biomed. Eng. 2002, 30, 1251–1261. [Google Scholar] [CrossRef] [PubMed]
- Nightingale, C.; Jones, S.P. A clinical investigation of force delivery systems for orthodontic space closure. J. Orthod. 2003, 30, 229–236. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, K.; Uechi, J.; Lee, S.P.; Mizoguchi, I. Three-dimensional analysis of orthodontic tooth movement based on XYZ and finite helical axis systems. Eur. J. Orthod. 2007, 29, 589–595. [Google Scholar] [CrossRef] [PubMed]
- Burstone, C.J. Rationale of the segmented arch. Am. J. Orthod. 1962, 48, 805–822. [Google Scholar] [CrossRef]
- Lagravère, M.O.; Carey, J.; Heo, G.; Toogood, R.W.; Major, P.W. Transverse, vertical, and anteroposterior changes from bone-anchored maxillary expansion vs. traditional rapid maxillary expansion: A randomized clinical trial. Am. J. Orthod. Dentofacial. Orthop. 2010, 137, 1–12. [Google Scholar]
- Shia, G.J. Treatment overruns. J. Clin. Orthod. 1986, 20, 602–604. [Google Scholar]
- Keim, R.G.; Gottlieb, E.L.; Nelson, A.H.; Vogels, D.S. 2003 JCO orthodontic practice study. Part 4: Additional breakdowns. J. Clin. Orthod. 2004, 38, 17–27. [Google Scholar]
- Lee, W. Corticotomy for orthodontic tooth movement. J. Korean Assoc. Oral Maxillofac. Surg. 2018, 44, 251–258. [Google Scholar] [CrossRef]
- Zainal, A.S.H.; Yamamoto, Z.; Zainol, A.L.Z.; Megat, A.W.R.; Zainal, A.Z. Cellular and molecular changes in orthodontic tooth movement. Sci. World J. 2011, 11, 1788–1803. [Google Scholar] [CrossRef]
- Roberts, W.E.; Huja, S.; Roberts, J.A. Bone modeling: Biomechanics, molecular mechanisms, and clinical perspectives. Semin. Orthod. 2004, 10, 123–161. [Google Scholar] [CrossRef]
- Brudvik, P.; Rygh, P. The initial phase of orthodontic root resorption incident to local compression of the periodontal ligament. Eur. J. Orthod. 1993, 15, 249–263. [Google Scholar] [CrossRef] [PubMed]
- Tsuchiya, M.; Akiba, Y.; Takahashi, I.; Sasano, Y.; Kashiwazaki, J.; Tsuchiya, S.; Watanabe, M. Comparison of expression patterns of cathepsin K and MMP-9 in odontoclasts and osteoclasts in physiological root resorption in the rat molar. Arch. Histol. Cytol. 2008, 71, 89–100. [Google Scholar] [CrossRef] [PubMed]
- El-Bialy, T.; El-Shamy, I.; Graber, T.M. Repair of orthodontically induced root resorption by ultrasound in humans. Am. J. Orthod. Dentofacial. Orthop. 2004, 126, 186–193. [Google Scholar] [CrossRef] [PubMed]
- Watabe, H.; Furuhama, T.; Tani-Ishii, N.; Mikuni-Takagaki, Y. Mechanotransduction activates α₅β₁ integrin and PI3K/Akt signaling pathways in mandibular osteoblasts. Exp. Cell Res. 2011, 317, 2642–2649. [Google Scholar] [CrossRef] [PubMed]
- Xia, P.; Wang, X.; Qu, Y.; Lin, Q.; Cheng, K.; Gao, M.; Ren, S.; Zhang, T.; Li, X. TGF-β1-induced chondrogenesis of bone marrow mesenchymal stem cells is promoted by low-intensity pulsed ultrasound through the integrin-mTOR signaling pathway. Stem Cell Res. Ther. 2017, 8, 281. [Google Scholar] [CrossRef]
- Padilla, F.; Puts, R.; Vico, L.; Raum, K. Stimulation of bone repair with ultrasound: A review of the possible mechanic effects. Ultrasonics 2014, 54, 1125–1145. [Google Scholar] [CrossRef]
- Li, J.K.; Chang, W.H.; Lin, J.C.; Ruaan, R.C.; Liu, H.C.; Sun, J.S. Cytokine release from osteoblasts in response to ultrasound stimulation. Biomaterials 2003, 24, 2379–2385. [Google Scholar] [CrossRef]
- Fávaro-Pípi, E.; Bossini, P.; de Oliveira, P.; Ribeiro, J.U.; Tim, C.; Parizotto, N.A.; Alves, J.M.; Ribeiro, D.A.; Selistre de Araujo, H.; Renno, A.C.M. Low-intensity pulsed ultrasound produced an increase of osteogenic genes expression during the process of bone healing in rats. Ultrasound Med. Biol. 2010, 36, 2057–2064. [Google Scholar] [CrossRef]
- Yang, Z.; Ren, L.; Deng, F.; Wang, Z.; Song, J. Low-intensity pulsed ultrasound induces osteogenic differentiation of human periodontal ligament cells through activation of bone morphogenetic protein-smad signaling. J. Ultrasound Med. 2014, 33, 865–873. [Google Scholar] [CrossRef]
- Chiu, C.Y.; Tsai, T.L.; Vanderby, R.; Bradica, G.; Lou, S.L.; Li, W.J. Osteoblastogenesis of mesenchymal stem cells in 3-D culture enhanced by low-intensity pulsed ultrasound through soluble receptor activator of nuclear factor kappa B ligand. Ultrasound Med. Biol. 2015, 41, 1842–1852. [Google Scholar] [CrossRef]
- Rego, E.B.; Inubushi, T.; Miyauchi, M.; Kawazoe, A.; Tanaka, E.; Takata, T.; Tanne, K. Ultrasound stimulation attenuates root resorption of rat replanted molars and impairs tumor necrosis factor-α signaling in vitro. J. Periodont. Res. 2011, 46, 648–654. [Google Scholar] [CrossRef] [PubMed]
- Akagi, H.; Nakanishi, Y.; Nakanishi, K.; Matsubara, H.; Hirose, Y.; Wang, P.L.; Ochi, M. Influence of low-intensity pulsed ultrasound stimulation on expression of bone-related genes in rat bone marrow cells. J. Hard Tissue Biol. 2016, 25, 1–5. [Google Scholar] [CrossRef]
- Inubushi, T.; Tanaka, E.; Rego, E.B.; Ohtani, J.; Kawazoe, A.; Tanne, K.; Miyauchi, M.; Takata, T. Ultrasound stimulation attenuates resorption of tooth root induced by experimental force application. Bone 2013, 53, 497–506. [Google Scholar] [CrossRef] [PubMed]
- Unsworth, J.; Kaneez, S.; Harris, S.; Ridgway, J.; Fenwick, S.; Chenery, D.; Harrison, A. Pulsed low intensity ultrasound enhances mineralisation in preosteoblast cells. Ultrasound Med. Biol. 2007, 33, 1468–1474. [Google Scholar] [CrossRef]
- Raza, H.; Major, P.; Dederich, D.; El-Bialy, T. Effect of low-intensity pulsed ultrasound on orthodontically induced root resorption caused by torque: A prospective, double-blind, controlled clinical trial. Angle Orthod. 2016, 86, 550–557. [Google Scholar] [CrossRef]
- Dalla-Bona, D.A.; Tanaka, E.; Inubushi, T.; Oka, H.; Ohta, A.; Okada, H.; Miyauchi, M.; Takata, T.; Tanne, K. Cementoblast response to low- and high-intensity ultrasound. Arch. Oral Biol. 2008, 53, 318–323. [Google Scholar] [CrossRef]
- Rego, E.B.; Inubushi, T.; Kawazoe, A.; Tanimoto, K.; Miyauchi, M.; Tanaka, E.; Takata, T.; Tanne, K. Ultrasound stimulation induces PGE2 synthesis promoting cementoblastic differentiation through EP2/EP4 receptor pathway. Ultrasound Med. Biol. 2010, 36, 907–915. [Google Scholar] [CrossRef]
- Baldwin, D.C. Appearance and aesthetics in oral health. Commun. Dent. Oral Epidemiol. 1980, 8, 244–256. [Google Scholar] [CrossRef]
- Grzić, R.; Spalj, S.; Lajnert, V.; Glavicić, S.; Uhac, I.; Pavicić, D.K. Factors influencing a patient’s decision to choose the type of treatment to improve dental esthetics. Vojnosanit Pregl. 2012, 69, 978–985. [Google Scholar] [CrossRef]
- Ashari, A.; Mohamed, A.M. Relationship of the dental aesthetic index to the oral health-related quality of life. Angle Orthod. 2016, 86, 337–342. [Google Scholar] [CrossRef]
| Tooth Movement | Root Resorption | |||||
|---|---|---|---|---|---|---|
| Mean (mm/Week) | SD | p Value | Mean (mm/Week) | SD | p Value | |
| Positive control | 0.232 | 0.0855 | 0.11 | 0.0241 | 0.0226 | 0.32 |
| Negative control (n = 10) | 0.201 | 0.0398 | 0.02836 | 0.0247 | ||
| Max (mm/Week) | Min (mm/Week) | Mean (mm/Week) | SD | Percent Change * | p Value | |
|---|---|---|---|---|---|---|
| LIPUS (n = 17) | 0.495 | 0.138 | 0.266 | 0.0927 | 29% | 0.0164 |
| Positive control (n = 17) | 0.388 | 0.045 | 0.232 | 0.0855 |
| Max (mm/Week) | Min (mm/Week) | Mean (mm/Week) | SD | Percent Change * | p Value | |
|---|---|---|---|---|---|---|
| LIPUS (n = 13) | 0.49 | −0.03 | 0.0092 | 0.0226 | 220.8% | 0.0423 |
| Positive control (n = 13) | 0.057 | −0.014 | 0.0241 | 0.0223 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
El-Bialy, T.; Farouk, K.; Carlyle, T.D.; Wiltshire, W.; Drummond, R.; Dumore, T.; Knowlton, K.; Tompson, B. Effect of Low Intensity Pulsed Ultrasound (LIPUS) on Tooth Movement and Root Resorption: A Prospective Multi-Center Randomized Controlled Trial. J. Clin. Med. 2020, 9, 804. https://doi.org/10.3390/jcm9030804
El-Bialy T, Farouk K, Carlyle TD, Wiltshire W, Drummond R, Dumore T, Knowlton K, Tompson B. Effect of Low Intensity Pulsed Ultrasound (LIPUS) on Tooth Movement and Root Resorption: A Prospective Multi-Center Randomized Controlled Trial. Journal of Clinical Medicine. 2020; 9(3):804. https://doi.org/10.3390/jcm9030804
Chicago/Turabian StyleEl-Bialy, Tarek, Khaled Farouk, Terry D. Carlyle, William Wiltshire, Robert Drummond, Tim Dumore, Kevin Knowlton, and Bryan Tompson. 2020. "Effect of Low Intensity Pulsed Ultrasound (LIPUS) on Tooth Movement and Root Resorption: A Prospective Multi-Center Randomized Controlled Trial" Journal of Clinical Medicine 9, no. 3: 804. https://doi.org/10.3390/jcm9030804
APA StyleEl-Bialy, T., Farouk, K., Carlyle, T. D., Wiltshire, W., Drummond, R., Dumore, T., Knowlton, K., & Tompson, B. (2020). Effect of Low Intensity Pulsed Ultrasound (LIPUS) on Tooth Movement and Root Resorption: A Prospective Multi-Center Randomized Controlled Trial. Journal of Clinical Medicine, 9(3), 804. https://doi.org/10.3390/jcm9030804





