Maternal Hepatitis B Virus or Hepatitis C Virus Carrier Status and Long-Term Endocrine Morbidity of the Offspring—A Population-Based Cohort Study
Abstract
1. Introduction
2. Materials and Methods
2.1. Setting
2.2. Study Population
2.3. Data Collection
2.4. Statistical Analysis
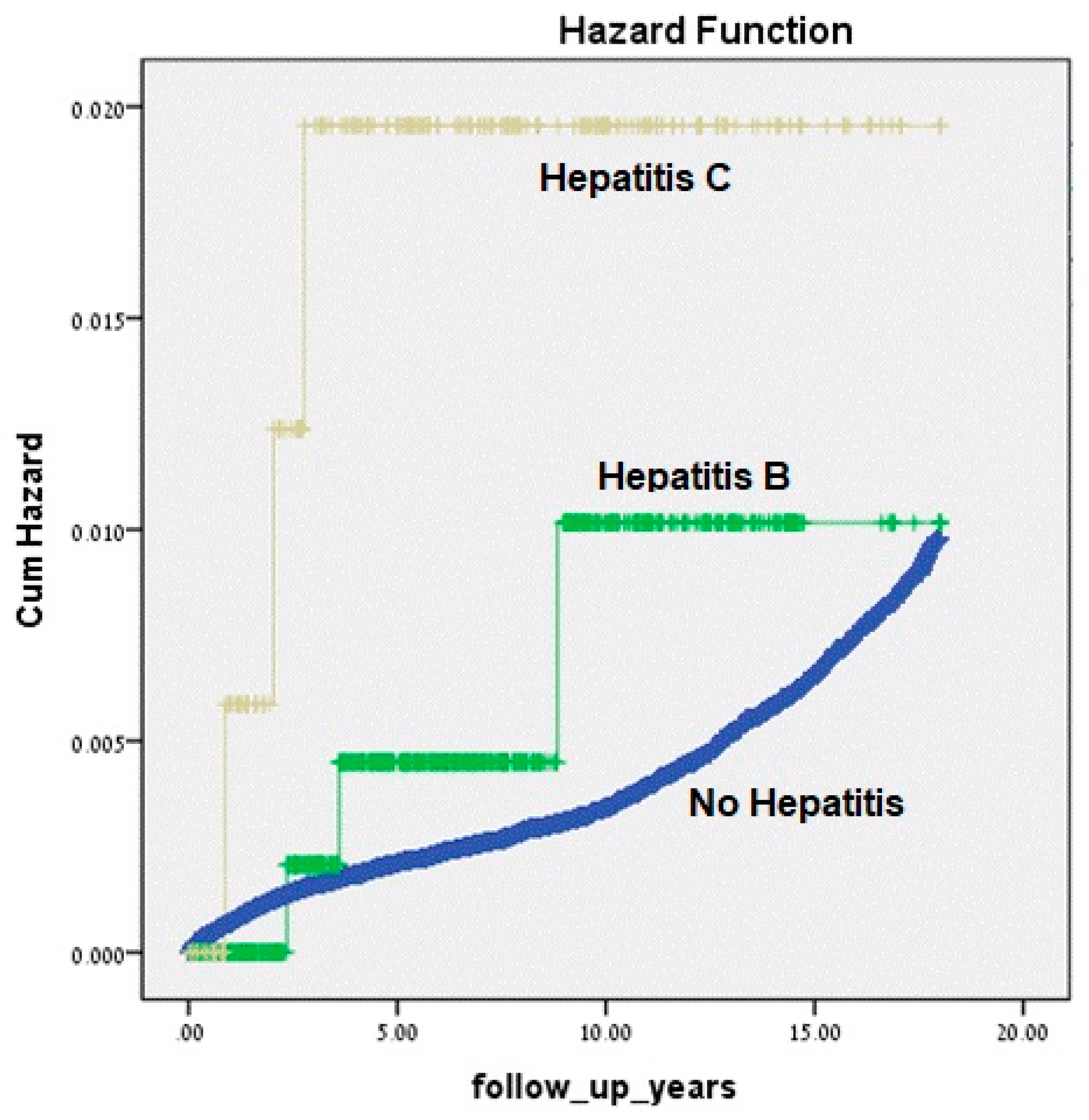
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Jonas, M.M. Hepatitis B and pregnancy: An underestimated issue. Liver Int. 2009, 29, 133–139. [Google Scholar] [CrossRef]
- Borgia, G.; Carleo, M.A.; Gaeta, G.B.; Gentile, I. Hepatitis B in pregnancy. World J. Gastroenterol. 2012, 14, 4677–4683. [Google Scholar] [CrossRef]
- Safir, A.; Levy, A.; Sikuler, E.; Sheiner, E. Maternal hepatitis B virus or hepatitis C virus carrier status as independent risk factor for adverse perinatal outcome. Liver Int. 2010, 30, 765–770. [Google Scholar] [CrossRef]
- Lu, J.; Hou, X.; Tu, H.; Tang, Z.; Xiang, Y.; Bao, Y.; Gu, J.; Jia, W. Chronic hepatitis B virus infection status is more prevalent in patients with type 2 diabetes. J. Diabetes Investig. 2017, 8, 619–625. [Google Scholar] [CrossRef]
- Wang, C.S.; Wang, S.T.; Yao, W.J.; Chang, T.T.; Chou, P. Hepatitis C virus infection and the development of type 2 diabetes in a community based longitudinal study. Am. J. Epidemiol. 2007, 166, 196–203. [Google Scholar] [CrossRef]
- Naing, C.; Mak, J.W.; Ahmed, S.I.; Maung, M. Relationship between hepatitis C virus infection and type 2 diabetes mellitus: Meta-analysis. World. J. Gastroenterol. 2012, 18, 1642–1651. [Google Scholar] [CrossRef]
- Li-Ng, M.; Tropp, S.; Danoff, A.; Bini, E.J. Association between chronic hepatitis B virus infection and diabetes among Asian Americans and Pacific Islanders. Dig. Liver Dis. 2007, 39, 549–556. [Google Scholar] [CrossRef] [PubMed]
- Iroezindu, M.O.; Isiguzo, G.C.; Young, E.E. Prevalence and predictors of impaired fasting glucose among Nigerian patients with hepatitis B virus infection. Diabetes Res. Clin. Pract. 2012, 98, 338–345. [Google Scholar] [CrossRef] [PubMed]
- Leandro, G.; Mangia, A.; Hui, J.; Fabris, P.; Rubbia-Brandt, L.; Colloredo, G.; Adinolfi, L.E.; Asselah, T.; Jonsson, J.R.; Smedile, A.; et al. HCV Meta-Analysis (on) Individual Patients’ Data Study Group. Relationship between steatosis, inflammation, and fibrosis in chronic hepatitis C: A meta-analysis of individual patient data. Gastroenterology 2006, 130, 1636–1642. [Google Scholar] [CrossRef] [PubMed]
- Antonelli, A.; Ferri, C.; Ferrari, S.M.; Colaci, M.; Sansonno, D.; Fallahi, P. Endocrine manifestation of hepatitis C virus infection. Nat. Clin. Pract. Endocrinol. Metab. 2009, 5, 26–34. [Google Scholar] [CrossRef]
- Ploix, C.; Verber, S.; Chevallier-Queyron, P.; Ritter, J.; Bousset, G.; Monier, J.C.; Fabien, N. Hepatitis C virus infection is frequently associated with high titers of anti-thyroid antibodies. Int. J. Immunopathol. Pharmacol. 1999, 12, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Antonelli, A.; Ferri, C.; Fallahi, P.; Ferrari, S.M.; Ghinoi, A.; Rotondi, M.; Ferrannini, E. Thyroid disorders in chronic hepatitis C virus infection. Thyroid 2006, 16, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Okolicsanyi, L.; Cscomos, G.; Crepaldi, G. Assessment and Management of Hepatobiliary Disease, 1st ed.; Springer: Heidelberg, Germany, 1987; pp. 17–225. [Google Scholar]
- Abokaf, H.; Shoham-Vardi, I.; Sergienko, R.; Landau, E.; Sheiner, E. In utero exposure to gestational diabetes mellitus and long-term endocrine morbidity of the offspring. Diabetes Res. Clin. Pract. 2018, 144, 233–235. [Google Scholar] [CrossRef] [PubMed]
- Paz Levy, D.; Sheiner, E.; Wainstock, T.; Sergienko, R.; Landau, D.; Walfisch, A. Evidence that children born at early term (37-38 6/7 weeks) are at increased risk for diabetes and obesity-related disorders. Am. J. Obstet. Gynecol. 2017, 217, 588.e1–588.e11. [Google Scholar] [CrossRef] [PubMed]
- Ortega-Prieto, A.; Dorner, M. Immune Evasion Strategies during Chronic Hepatitis B and C Virus Infection. Vaccines 2017, 5, 24. [Google Scholar] [CrossRef] [PubMed]
- Flores-Chávez, A.; Carrion, J.A.; Forns, X.; Ramos-Casals, M. Extrahepatic manifestations associated with chronic Hepatitis C Virus infection. Rev. Esp. Sanid. Penit. 2017, 19, 87–97. [Google Scholar]
- Bugianesi, E.; Salamone, F.; Negro, F. The interaction of metabolic factors with HCV infection: Does it matter. J. Hepatol. 2012, 56, 56–65. [Google Scholar] [CrossRef]
- Fensterl, V.; Chattopadhyay, S.; Sen, G.C. No love lost between viruses and interferons. Annu. Rev. Virol. 2015, 2, 549–572. [Google Scholar] [CrossRef]
- Spiegel, E.; Shoham-Vardi, I.; Sergienko, R.; Landau, D.; Sheiner, E. The association between birth weight at term and long-term endocrine morbidity of the offspring. J. Mat-Fet. Neonat Med. 2018, 32, 2657–2661. [Google Scholar] [CrossRef]
- Govrin-yehudain, Y.; Wainstock, T.; Abu-Freha, N.; Sheiner, E. Maternal hepatitis B Virus and Hepatitis C virus Carrier Status During Pregnancy and Long-Term Respiratory Complication in Offspring. Early Hum. Dev. 2019, 140, 104904. [Google Scholar] [CrossRef]
- Yoles, I.; Sheiner, E.; Abu-Freha, N.; Wainstock, T. Maternal hepatitis B or C and Long-Term Gastrointestinal Morbidity for Offspring: A Population-Based Cohort Study. Liver Int. 2019, 39, 2046–2051. [Google Scholar] [CrossRef] [PubMed]
- EASL Recommendation on Treatment of Hepatitis C. J. Hepatol. 2018, 69, 461–511. [CrossRef] [PubMed]
- Hepatitis C Guidance 2018 Update: AASLD-IDSA Recommendations for Testing, Managing, and Treating Hepatitis C Virus Infection. Clin. Infec. Dis. 2018, 67, 1477–1492. [CrossRef] [PubMed]
| Characteristics | No Hepatitis n (%), 242,905 (99.7) | Hepatitis B n (%), 591 (0.2) | Hepatitis C n (%), 186 (0.1) | p-Value |
|---|---|---|---|---|
| Mother’s age at birth (years ± SD) | 28.16 ± 5.8 | 28.8 ± 5.9 | 30.6 ± 5.1 | <0.001 * |
| Gestational age-Weeks | 39.1 ± 1.9 | 38.8 ± 2 | 38.2 ± 2.4 | <0.001 * |
| Gravidity group | ||||
| 1 | 47,872 (19.7) | 120 (20.3) | 39 (21) | 0.972 ** |
| 2–4 | 116,182 (47.8) | 282 (47.7) | 85 (45.7) | |
| 5+ | 78,808 (32.4) | 189 (32) | 62 (33.3) | |
| Diabetes Mellitus (gestational and pre-gestational) | 12,120 (5) | 30 (5.1) | 9 (4.8) | 0.991 ** |
| Hypertensive disorders of pregnancy | 12,191 (5) | 41 (6.9) | 15 (8.1) | 0.017 ** |
| Preterm delivery | ||||
| <37 | 16,647 (6.9) | 46 (7.8) | 27 (14.5) | <0.001 ** |
| <34 | 3289 (1.4) | 12 (2) | 8 (4.3) | 0.001 ** |
| Birth weight | ||||
| Low ≤ 2500 g | 16,330 (6.7) | 42 (7.1) | 32 (17.2) | <0.001 ** |
| very low ≤ 1500 g | 1454 (0.6) | 6 (1) | 2 (1.1) | 0.298 *** |
| Infant Gender | ||||
| Male | 123,468 (50.8) | 320 (54.1) | 89 (47.8) | 0.196 ** |
| Apgar 1 min < 7 | 12,947 (5.3) | 33 (5.6) | 10 (5.4) | 0.963 ** |
| Apgar 5 min < 7 | 5,497 (2.3) | 9 (1.5) | 3 (1.6) | 0.403 *** |
| Birth-weight | 3205 ± 528 | 3236 ± 528 | 3065 ± 634 | <0.001 * |
| Perinatal mortality | 1,334 (0.5) | 3 (0.5) | 3 (1.6) | 0.145 *** |
| Endocrine Morbidity | No hepatitis n = 241,571 (%) | Hepatitis B n = 588 (%) | Hepatitis C n = 183 (%) | p-Value |
|---|---|---|---|---|
| Thyroid Disease | 110 (0.04) | 0 (0) | 0 (0) | 0.839 |
| Diabetes mellitus | 215 (0.09) | 0 (0) | 1 (0.55) | 0.090 |
| Hypoglycemia | 287 (0.12) | 1 (0.17) | 2 (1.1) | 0.001 |
| Obesity | 435 (0.18) | 2 (0.34) | 0 (0) | 0.558 |
| Adrenal disease | 43 (0.018) | 0 (0) | 0 (0) | 0.934 |
| Endocrine hospitalization | 1145 (0.47) | 3 (0.51) | 3 (1.64) | 0.072 |
| Variables | Adjusted HR | 95% CI | p-Value |
|---|---|---|---|
| Hepatitis B | 1.8 | 0.607–5.859 | 0.273 |
| Hepatitis C | 5.05 | 1.625–15.695 | 0.005 |
| Maternal age at birth (years) | 1.0 | 0.992–1.012 | 0.653 |
| Diabetes mellitus (gestational and pregestational) | 1.82 | 1.494–2.219 | <0.001 |
| Hypertensive disorders of pregnancy | 1.308 | 1.053–1.625 | 0.015 |
| Gestational age (weeks) | 0.935 | 0.913–0.957 | <0.001 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abu Freha, N.; Wainstock, T.; Menachem, T.N.; Sheiner, E. Maternal Hepatitis B Virus or Hepatitis C Virus Carrier Status and Long-Term Endocrine Morbidity of the Offspring—A Population-Based Cohort Study. J. Clin. Med. 2020, 9, 796. https://doi.org/10.3390/jcm9030796
Abu Freha N, Wainstock T, Menachem TN, Sheiner E. Maternal Hepatitis B Virus or Hepatitis C Virus Carrier Status and Long-Term Endocrine Morbidity of the Offspring—A Population-Based Cohort Study. Journal of Clinical Medicine. 2020; 9(3):796. https://doi.org/10.3390/jcm9030796
Chicago/Turabian StyleAbu Freha, Naim, Tamar Wainstock, Tzvi Najman Menachem, and Eyal Sheiner. 2020. "Maternal Hepatitis B Virus or Hepatitis C Virus Carrier Status and Long-Term Endocrine Morbidity of the Offspring—A Population-Based Cohort Study" Journal of Clinical Medicine 9, no. 3: 796. https://doi.org/10.3390/jcm9030796
APA StyleAbu Freha, N., Wainstock, T., Menachem, T. N., & Sheiner, E. (2020). Maternal Hepatitis B Virus or Hepatitis C Virus Carrier Status and Long-Term Endocrine Morbidity of the Offspring—A Population-Based Cohort Study. Journal of Clinical Medicine, 9(3), 796. https://doi.org/10.3390/jcm9030796






