Transradial and Transfemoral Approach in Patients with Prior Coronary Artery Bypass Grafting
Abstract
1. Introduction
2. Methods
2.1. Study Design and Patient Population
2.2. Study Endpoints
2.3. Statistical Analysis
Femoral vs. Radial Access and Right vs. Left Radial Access
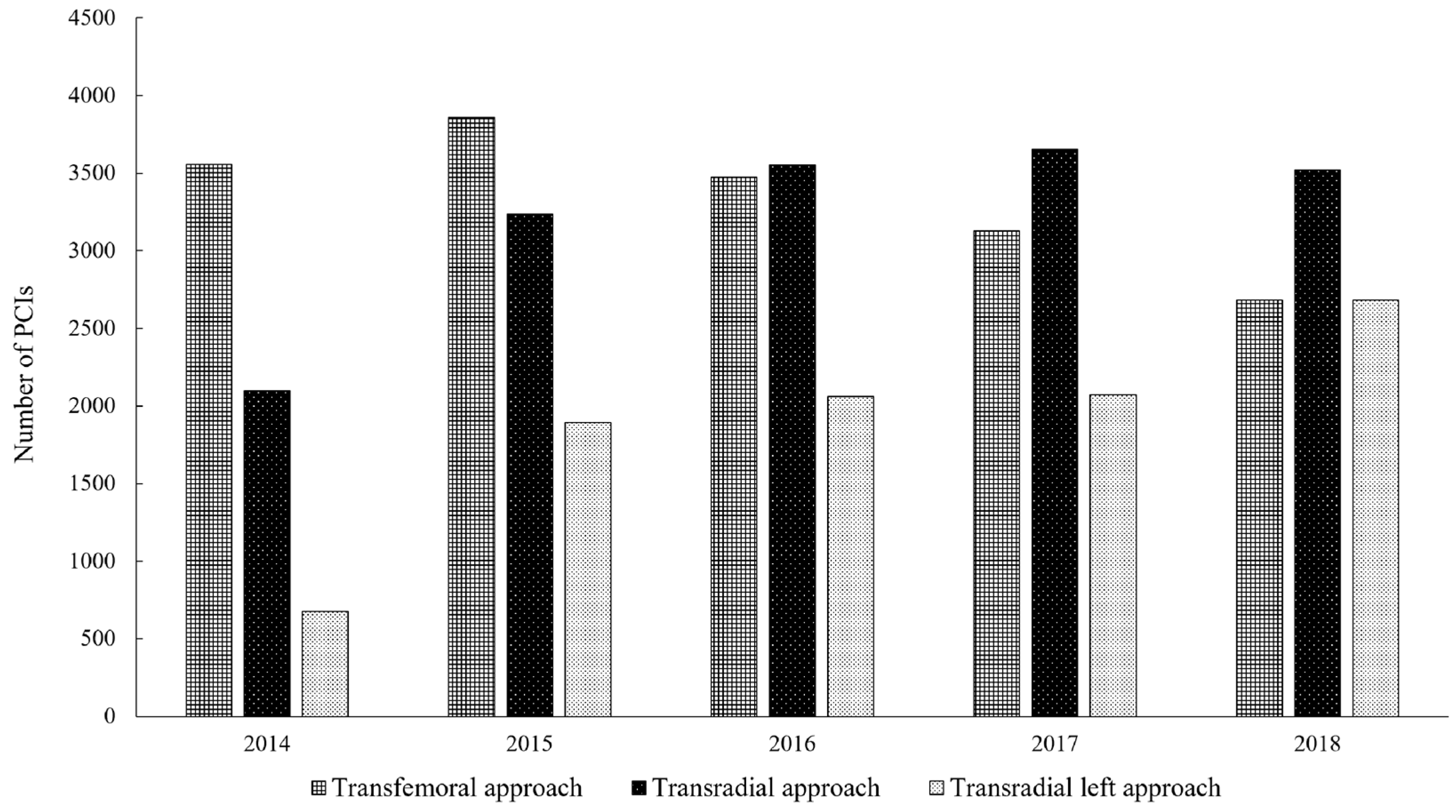
3. Results
3.1. Population
3.2. Procedural Indices
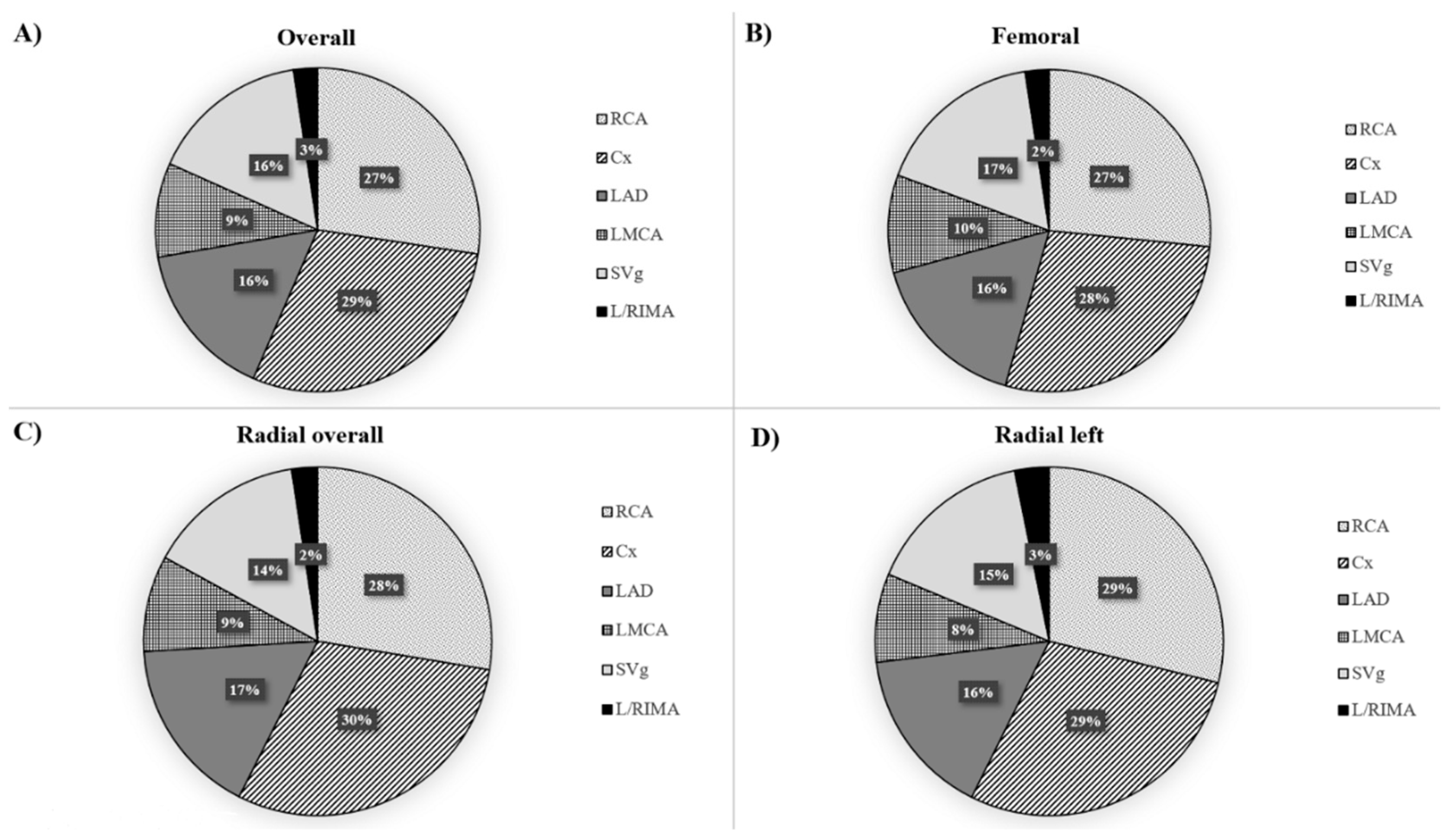
3.3. Femoral and Radial Access
3.4. Right and Left Radial Access
4. Discussion
5. Limitations
6. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Cooper, C.J.; El-Shiekh, R.A.; Cohen, D.J.; Blaesing, L.; Burket, M.W.; Basu, A.; Moore, J.A. Effect of transradial access on quality of life and cost of cardiac catheterization: A randomized comparison. Am. Heart J. 1999, 138, 430–436. [Google Scholar] [CrossRef]
- Jolly, S.S.; Yusuf, S.; Cairns, J.; Niemelä, K.; Xavier, D.; Widimsky, P.; Budaj, A.; Niemelä, M.; Valentin, V.; Lewis, B.S.; et al. Radial versus femoral access for coronary angiography and intervention in patients with acute coronary syndromes (RIVAL): A randomised, parallel group, multicentre trial. Lancet 2011, 377, 1409–1420. [Google Scholar] [CrossRef]
- Israeli, Z.; Lavi, S.; Pancholy, S.B.; Nombela-Franco, L.; Gilchrist, I.C.; Gilchrist, I.C., Jr.; Aldazabal, A.; Sharabi-Nov, A.; Levi, Y.; Hayman, S.; et al. Radial versus femoral approach for saphenous vein grafts angiography and interventions. Am. Heart J. 2019, 210, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, Y.; Shiomi, H.; Morimoto, T.; Yaku, H.; Kaji, S.; Furukawa, Y.; Nakagawa, Y.; Ando, K.; Kadota, K.; Abe, M.; et al. Transradial versus transfemoral approach in patients undergoing primary percutaneous coronary intervention for ST-elevation acute myocardial infarction: Insight from the CREDO-Kyoto AMI registry. Heart Vessels 2017, 32, 1448–1457. [Google Scholar] [CrossRef] [PubMed]
- Ziakas, A.; Klinke, P.; Mildenberger, R.; Fretz, E.; Williams, M.; Della Siega, A.; Kinloch, D.; Hilton, D. A comparison of the radial and the femoral approach in vein graft PCI. A retrospective study. Int. J. Cardiovasc. Interv. 2005, 7, 93–96. [Google Scholar] [CrossRef] [PubMed]
- Sanmartin, M.; Cuevas, D.; Moxica, J.; Valdes, M.; Esparza, J.; Baz, J.A.; Mantilla, R.; Iñiguez, A. Transradial cardiac catheterization in patients with coronary bypass grafts: Feasibility analysis and comparison with transfemoral approach. Catheter. Cardiovasc. Interv. 2006, 67, 580–584. [Google Scholar] [CrossRef] [PubMed]
- Rathore, S.; Roberts, E.; Hakeem, A.R.; Pauriah, M.; Beaumont, A.; Morris, J.L. The feasibility of percutaneous transradial coronary intervention for saphenous vein graft lesions and comparison with transfemoral route. J. Interv. Cardiol. 2009, 22, 336–340. [Google Scholar] [CrossRef] [PubMed]
- Bundhoo, S.S.; Earp, E.; Ivanauskiene, T.; Kunadian, V.; Freeman, P.; Edwards, R.; Kinnaird, T.D.; Zaman, A.; Anderson, R.A. Saphenous vein graft percutaneous coronary intervention via radial artery access: Safe and effective with reduced hospital length of stay. Am. Heart J. 2012, 164, 468–472. [Google Scholar] [CrossRef] [PubMed]
- Feldman, D.N.; Swaminathan, R.V.; Kaltenbach, L.A.; Baklanov, D.V.; Kim, L.K.; Wong, S.C.; Minutello, R.M.; Messenger, J.C.; Moussa, I.; Garratt, K.N.; et al. Adoption of radial access and comparison of outcomes to femoral access in percutaneous coronary intervention: An updated report from the national cardiovascular data registry (2007–2012). Circulation 2013, 127, 2295–2306. [Google Scholar] [CrossRef] [PubMed]
- Januszek, R.; Siudak, Z.; Reczuch, K.; Dobrzycki, S.; Lesiak, M.; Legutko, J.; Kleczyński, P.; Rzeszutko, Ł.; Dudek, D.; Bartuś, S. Current trends and procedural outcomes in the era of rotational atherectomy expansion in Poland in the period 2014–2017 (based on the nationwide ORPKI registry). Postepy Kardiol. Interwencyjnej 2019, 15, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Malenka, D.J.; Leavitt, B.J.; Hearne, M.J.; Robb, J.F.; Baribeau, Y.R.; Ryan, T.J.; Helm, R.E.; Kellett, M.A.; Dauerman, H.L.; Dacey, L.J.; et al. Comparing long-term survival of patients with multivessel coronary disease after CABG or PCI: Analysis of BARI-like patients in northern New England. Circulation 2005, 112, I371–I376. [Google Scholar] [CrossRef] [PubMed]
- Brilakis, E.S.; Rao, S.V.; Banerjee, S.; Goldman, S.; Shunk, K.A.; Holmes, D.R., Jr.; Honeycutt, E.; Roe, M.T. Percutaneous coronary intervention in native arteries versus bypass grafts in prior coronary artery bypass grafting patients: A report from the National Cardiovascular Data Registry. JACC. Cardiovasc. Interv. 2011, 4, 844–850. [Google Scholar] [CrossRef] [PubMed]
- Boatman, D.M.; Saeed, B.; Varghese, I.; Peters, C.T.; Daye, J.; Haider, A.; Roesle, M.; Banerjee, S.; Brilakis, E.S. Prior coronary artery bypass graft surgery patients undergoing diagnostic coronary angiography have multiple uncontrolled coronary artery disease risk factors and high risk for cardiovascular events. Heart Vessels 2009, 24, 241–246. [Google Scholar] [CrossRef] [PubMed]
- Morrison, D.A.; Sethi, G.; Sacks, J.; Henderson, W.G.; Grover, F.; Sedlis, S.; Esposito, R.; Investigators of the Department of Veterans Affairs Cooperative Study #385, Angina With Extremely Serious Operative Mortality Evaluation. Percutaneous coronary intervention versus repeat bypass surgery for patients with medically refractory myocardial ischemia: AWESOME randomized trial and registry experience with post-CABG patients. J. Am. Coll. Cardiol. 2002, 40, 1951–1954. [Google Scholar] [CrossRef]
- Welsh, R.C.; Granger, C.B.; Westerhout, C.M.; Blankenship, J.C.; Holmes, D.R., Jr.; O’Neill, W.W.; Hamm, C.W.; Van de Werf, F.; Armstrong, P.W.; APEX AMI Investigators. Prior coronary artery bypass graft patients with ST-segment elevation myocardial infarction treated with primary percutaneous coronary intervention. JACC. Cardiovasc. Interv. 2010, 3, 343–351. [Google Scholar] [CrossRef] [PubMed]
- Al Suwaidi, J.; Velianou, J.L.; Berger, P.B.; Mathew, V.; Garratt, K.N.; Reeder, G.S.; Grill, D.E.; Holmes, D.R., Jr. Primary percutaneous coronary interventions in patients with acute myocardial infarction and prior coronary artery bypass grafting. Am. Heart J. 2001, 142, 452–459. [Google Scholar] [CrossRef] [PubMed]
- Burzotta, F.; Trani, C.; Todaro, D.; Romagnoli, E.; Niccoli, G.; Ginnico, F.; Talarico, G.P.; Tommasino, A.; Mazzari, M.A.; Mongiardo, R.; et al. Comparison of the transradial and transfemoral approaches for coronary angiographic evaluation in patients with internal mammary artery grafts. J. Cardiovasc. Med. (Hagerstown) 2008, 9, 263–266. [Google Scholar] [CrossRef] [PubMed]
- Michael, T.T.; Alomar, M.; Papayannis, A.; Mogabgab, O.; Patel, V.G.; Rangan, B.V.; Luna, M.; Hastings, J.L.; Grodin, J.; Abdullah, S.; et al. A randomized comparison of the transradial and transfemoral approaches for coronary artery bypass graft angiography and intervention: The RADIAL-CABG Trial (RADIAL Versus Femoral Access for Coronary Artery Bypass Graft Angiography and Intervention). JACC. Cardiovasc. Interv. 2013, 6, 1138–1144. [Google Scholar] [CrossRef] [PubMed]
- Shah, B.; Bangalore, S.; Feit, F.; Fernandez, G.; Coppola, J.; Attubato, M.J.; Slater, J. Radiation exposure during coronary angiography via transradial or transfemoral approaches when performed by experienced operators. Am. Heart J. 2013, 165, 286–292. [Google Scholar] [CrossRef] [PubMed]
- Singh, G.; Campos, E.; Kavinsky, C.J.; Snell, J.R.; Schaer, G.L.; Jolly, N. Comparative Analysis of Radial Versus Femoral Diagnostic Cardiac Catheterization Procedures in a Cardiology Training Program. J. Invasive. Cardiol. 2016, 28, 254–257. [Google Scholar] [PubMed]


| Selected Indices | Radial Artery n = 17,609 | Femoral Artery n = 15,154 | p Value |
|---|---|---|---|
| Age, years | 69.8 ± 8.8 | 69.5 ± 8.5 | 0.002 |
| Gender, males | 13,560 (77) | 11,270 (74.4) | <0.001 |
| Weight, kg | 81.8 ± 16.5 | 81.1 ± 16.5 | <0.001 |
| Diabetes | 5957 (33.8) | 4832 (31.9) | <0.001 |
| Prior cerebral stroke | 763 (4.3) | 646 (4.26) | 0.75 |
| Prior myocardial infarction | 10,201 (57.9) | 8367 (55.2) | <0.001 |
| Prior PCI | 10,031 (57) | 8876 (58.6) | 0.003 |
| Smoking | 1971 (11.2) | 1549 (10.2) | 0.004 |
| Hypertension | 13,910 (79) | 11,929 (78.7) | 0.54 |
| Kidney failure | 1719 (9.8) | 1513 (10) | 0.5 |
| Diagnosis | |||
| stable angina | 6324 (36) | 4687 (31) | <0.001 |
| unstable angina | 6640 (37.8) | 6099 (40.3) | <0.001 |
| NSTEMI | 3167 (18) | 2899 (19.1) | 0.008 |
| STEMI | 1207 (6.8) | 1235 (8.2) | <0.001 |
| others | 242 (1.4) | 211 (1.4) | 0.89 |
| Coronary angiography | |||
| SVD | 4937 (33.2) | 4644 (35.3) | <0.001 |
| MVD | 6945 (46.8) | 6328 (48.2) | 0.02 |
| LMCA +/− MVD | 2968 (20) | 2171 (16.5) | <0.001 |
| Imaging studies | |||
| fractional flow reserve | 183 (1.04) | 103 (0.7) | <0.001 |
| intravascular ultrasound | 281 (1.6) | 220 (1.4) | 0.28 |
| optical coherence tomography | 28 (0.1) | 23 (0.1) | 0.86 |
| Thrombectomy | 226 (1.3) | 257 (1.7) | 0.002 |
| Rotablation | 194 (1.1) | 164 (1.1) | 0.86 |
| Acetylsalicylic acid before PCI | 5974 (33.9) | 5125 (33.8) | 0.83 |
| TIMI 2/3 before PCI | 12,655 (74.2) | 10,347 (70.5) | <0.001 |
| Contrast, ml | 204.7 ± 96.9 | 213 ± 99.8 | <0.001 |
| Radiation dose, mGy | 1309.8 ± 1117.2 | 1289.5 ± 1051 | <0.001 |
| Selected Indices | Radial Artery n = 12,261 | Femoral Artery n = 12,261 | p Value |
|---|---|---|---|
| Age, years | 69.7 ± 8.8 | 69.5 ± 9 | 0.14 |
| Gender, males | 9225 (75.2) | 9134 (74.5) | 0.18 |
| Weight, kg | 81.7 ± 14.4 | 81.4 ± 14.4 | 0.1 |
| Diabetes | 3984 (32.5) | 3933 (21.1) | 0.49 |
| Prior cerebral stroke | 538 (4.4) | 552 (4.5) | 0.68 |
| Prior myocardial infarction | 6938 (56.6) | 6830 (55.7) | 0.17 |
| Prior PCI | 7059 (57.6) | 7078 (57.7) | 0.81 |
| Smoking | 1281 (10.4) | 1289 (10.5) | 0.88 |
| Hypertension | 9667 (78.8) | 9733 (79.4) | 0.3 |
| Kidney failure | 1175 (9.6) | 1257 (10.3) | 0.08 |
| Diagnosis | 0.006 | ||
| stable angina | 3574 (29.1) | 3447 (28.1) | 0.07 |
| unstable angina | 5270 (43) | 5254 (42.9) | 0.84 |
| NSTEMI | 2434 (19.9) | 2432 (19.8) | 0.98 |
| STEMI | 793 (6.5) | 938 (7.7) | <0.001 |
| others | 190 (1.5) | 190 (1.5) | 1 |
| Coronary angiography | <0.001 | ||
| single-vessel disease | 4063 (33.1) | 4351 (33.5) | |
| multi-vessel disease | 5745 (46.9) | 5882 (48) | |
| LMCA +/− MVD | 2453 (20) | 2028 (16.5) | |
| Imaging studies | |||
| fractional flow reserve | 115 (0.9) | 83 (0.7) | 0.03 |
| intravascular ultrasound | 141 (1.1) | 131 (1.1) | 0.58 |
| optical coherence tomography | 22 (0.2) | 18 (0.1) | 0.63 |
| Thrombectomy | 200 (1.6) | 236 (1.9) | 0.09 |
| Rotablation | 79 (0.6) | 87 (0.7) | 0.58 |
| Acetylsalicylic acid before PCI | 4212 (34.4) | 4268 (34.8) | 0.46 |
| TIMI 2/3 before PCI | 8895 (72.5) | 8571 (69.9) | <0.001 |
| Contrast, ml | 210.6 ± 91.1 | 218.3 ± 92.8 | <0.001 |
| Radiation dose, mGy | 1316.5 ± 1107.8 | 1301.2 ± 1040.6 | 0.26 |
| Selected Indices | Radial Artery n = 9661 | Femoral Artery n = 9661 | p Value |
|---|---|---|---|
| Age, years | 69.7 ± 8.8 | 69.5 ± 9 | 0.08 |
| Gender, males | 7226 (74.8) | 7175 (74.3) | 0.41 |
| Weight, kg | 81.6 ± 14.1 | 81.4 ± 14.5 | 0.36 |
| Diabetes | 3187 (33) | 3125 (32.3) | 0.34 |
| Prior cerebral stroke | 419 (4.3) | 436 (4.5) | 0.57 |
| Prior myocardial infarction | 5484 (56.8) | 5373 (55.6) | 0.11 |
| Prior PCI | 5558 (57.5) | 5563 (57.6) | 0.95 |
| Smoking | 1083 (11.2) | 1085 (11.2) | 0.98 |
| Hypertension | 7636 (79.0) | 7718 (79.9) | 0.14 |
| Kidney failure | 1006 (10.4) | 1023 (10.6) | 0.7 |
| Diagnosis | 0.01 | ||
| stable angina | 2483 (25.7) | 2369 (24.5) | |
| unstable angina | 4317 (44.7) | 4272 (44.2) | |
| NSTEMI | 2039 (21.1) | 2075 (21.5) | |
| STEMI | 668 (6.9) | 789 (8.2) | |
| others | 154 (1.6) | 156 (1.6) | |
| Cardiac arrest before PCI | 59 (0.6) | 151 (1.6) | <0.001 |
| Killip class grade before PCI | |||
| 1 | 8810 (91.2) | 8658 (89.6) | <0.001 |
| 2 | 667 (6.9) | 694 (7.2) | |
| 3 | 103 (1.1) | 125 (1.3) | |
| 4 | 81 (0.8) | 184 (1.9) | |
| Coronary angiography | 0.26 | ||
| single-vessel disease | 3222 (33.4) | 3321 (34.4) | |
| multi-vessel disease | 4749 (49.2) | 4706 (48.7) | |
| LMCA +/− MVD | 1690 (17.5) | 1634 (16.9) | |
| Imaging studies | |||
| fractional flow reserve | 69 (0.7) | 60 (0.6) | 0.48 |
| intravascular ultrasound | 88 (0.9) | 84 (0.9) | 0.81 |
| optical coherence tomography | 18 (0.2) | 16 (0.2) | 0.86 |
| Thrombectomy | 173 (1.8) | 195 (2.0) | 0.26 |
| Rotablation | 41 (0.4) | 44 (0.5) | 0.82 |
| Acetylsalicylic acid before PCI | 3357 (34.7) | 3357 (34.7) | 1.0 |
| TIMI 2/3 before PCI | 6809 (70.5) | 6621 (68.5) | 0.003 |
| Contrast, ml | 216.1 ± 92.3 | 217.3 ± 91.5 | 0.35 |
| Radiation dose, mGy | 1309.2 ± 1058.9 | 1299.7 ± 1052.7 | 0.52 |
| Selected Indices | Right Radial Artery n = 6420 | Left Radial Artery n = 6420 | p Value |
|---|---|---|---|
| Age, years | 69.7 ± 8.8 | 69.9 ± 8.8 | 0.22 |
| Gender, males | 4879 (76) | 4912 (76.5) | 0.51 |
| Weight, kg | 82.1 ± 14.6 | 82.1 ± 14.3 | 0.88 |
| Diabetes | 2176 (33.9) | 2189 (34.1) | 0.82 |
| Prior cerebral stroke | 299 (4.7) | 268 (4.2) | 0.2 |
| Prior myocardial infarction | 3730 (58.1) | 3756 (58.5) | 0.65 |
| Prior PCI | 3806 (59.3) | 3749 (58.4) | 0.31 |
| Smoking | 729 (11.4) | 748 (11.7) | 0.61 |
| Hypertension | 5083 (79.2) | 5109 (79.6) | 0.58 |
| Kidney failure | 635 (9.9) | 634 (9.9) | 1.0 |
| Diagnosis | 0.67 | ||
| stable angina | 2152 (33.5) | 2081 (32.4) | 0.18 |
| unstable angina | 2618 (40.8) | 2693 (41.9) | 0.18 |
| NSTEMI | 1176 (18.3) | 1173 (18.3) | 0.96 |
| STEMI | 375 (5.8) | 371 (5.8) | 0.91 |
| others | 99 (1.5) | 102 (1.6) | 0.88 |
| Coronary angiography | <0.001 | ||
| single vessel disease | 2025 (31.5) | 2230 (34.7) | |
| multi-vessel disease | 3163 (49.3) | 2856 (44.5) | |
| LMCA +/− MVD | 1232 (19.2) | 1334 (20.8) | |
| Imaging studies | |||
| fractional flow reserve | 83 (1.3) | 49 (0.8) | 0.004 |
| intravascular ultrasound | 90 (1.4) | 63 (1) | 0.03 |
| optical coherence tomography | 13 (0.2) | 9 (0.1) | 0.52 |
| Thrombectomy | 104 (1.6) | 83 (1.3) | 0.14 |
| Rotablation | 63 (1) | 26 (0.4) | <0.001 |
| Acetylsalicylic acid before PCI | 2200 (34.3) | 2220 (34.6) | 0.72 |
| TIMI 2/3 before PCI | 4681 (72.9) | 4753 (74) | 0.15 |
| Contrast, ml | 207.5 ± 91.3 | 212.3 ± 90.7 | 0.003 |
| Radiation dose, mGy | 1325.5 ± 1166.8 | 1312.3 ± 1054.2 | 0.5 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Januszek, R.; Siudak, Z.; Malinowski, K.P.; Wańha, W.; Wojakowski, W.; Gąsior, M.; Bartuś, S.; Dudek, D. Transradial and Transfemoral Approach in Patients with Prior Coronary Artery Bypass Grafting. J. Clin. Med. 2020, 9, 764. https://doi.org/10.3390/jcm9030764
Januszek R, Siudak Z, Malinowski KP, Wańha W, Wojakowski W, Gąsior M, Bartuś S, Dudek D. Transradial and Transfemoral Approach in Patients with Prior Coronary Artery Bypass Grafting. Journal of Clinical Medicine. 2020; 9(3):764. https://doi.org/10.3390/jcm9030764
Chicago/Turabian StyleJanuszek, Rafał, Zbigniew Siudak, Krzysztof Piotr Malinowski, Wojciech Wańha, Wojciech Wojakowski, Mariusz Gąsior, Stanisław Bartuś, and Dariusz Dudek. 2020. "Transradial and Transfemoral Approach in Patients with Prior Coronary Artery Bypass Grafting" Journal of Clinical Medicine 9, no. 3: 764. https://doi.org/10.3390/jcm9030764
APA StyleJanuszek, R., Siudak, Z., Malinowski, K. P., Wańha, W., Wojakowski, W., Gąsior, M., Bartuś, S., & Dudek, D. (2020). Transradial and Transfemoral Approach in Patients with Prior Coronary Artery Bypass Grafting. Journal of Clinical Medicine, 9(3), 764. https://doi.org/10.3390/jcm9030764







