Non-Pharmacological Interventions for Post-Stroke Fatigue: Systematic Review and Network Meta-Analysis
Abstract
:1. Introduction
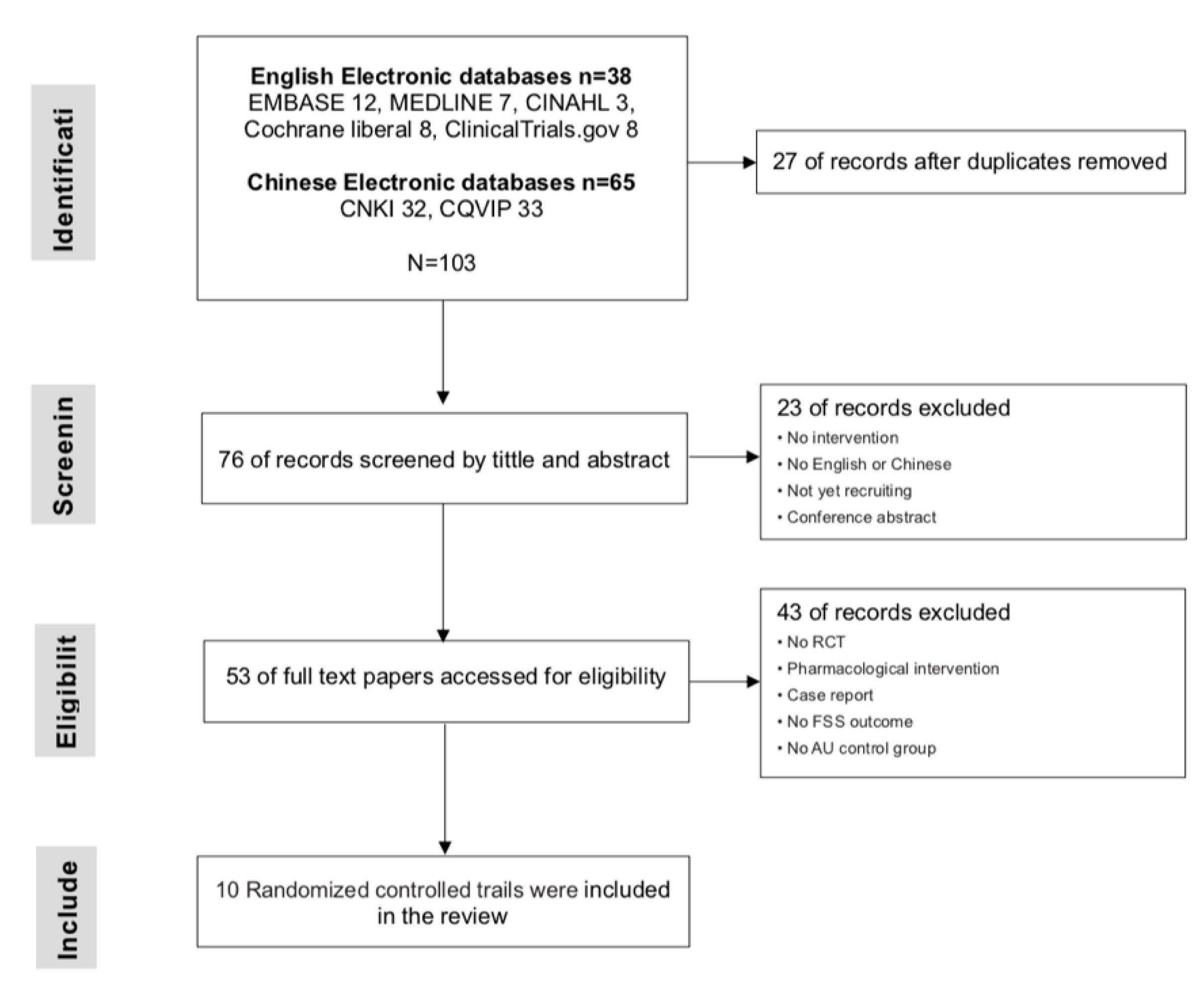
2. Materials and Methods
2.1. Inclusion and Exclusion Criteria
2.2. Data Search and Selection
2.3. Data Extraction and Quality Assessment
2.4. Statistical Analysis
3. Results
3.1. Type of Intervention
3.1.1. Community Health Management (CHM)
3.1.2. Traditional Chinese Medicine (TCM)
3.1.3. Cognitive Behavioral Therapy (CBT)
3.1.4. Respiratory Therapy (RT) and Music Therapy (MT)
3.1.5. Circuit Training (CT)
3.1.6. Hyperbaric Oxygen Therapy (HOT)
3.2. Assessment of Risk of Bias
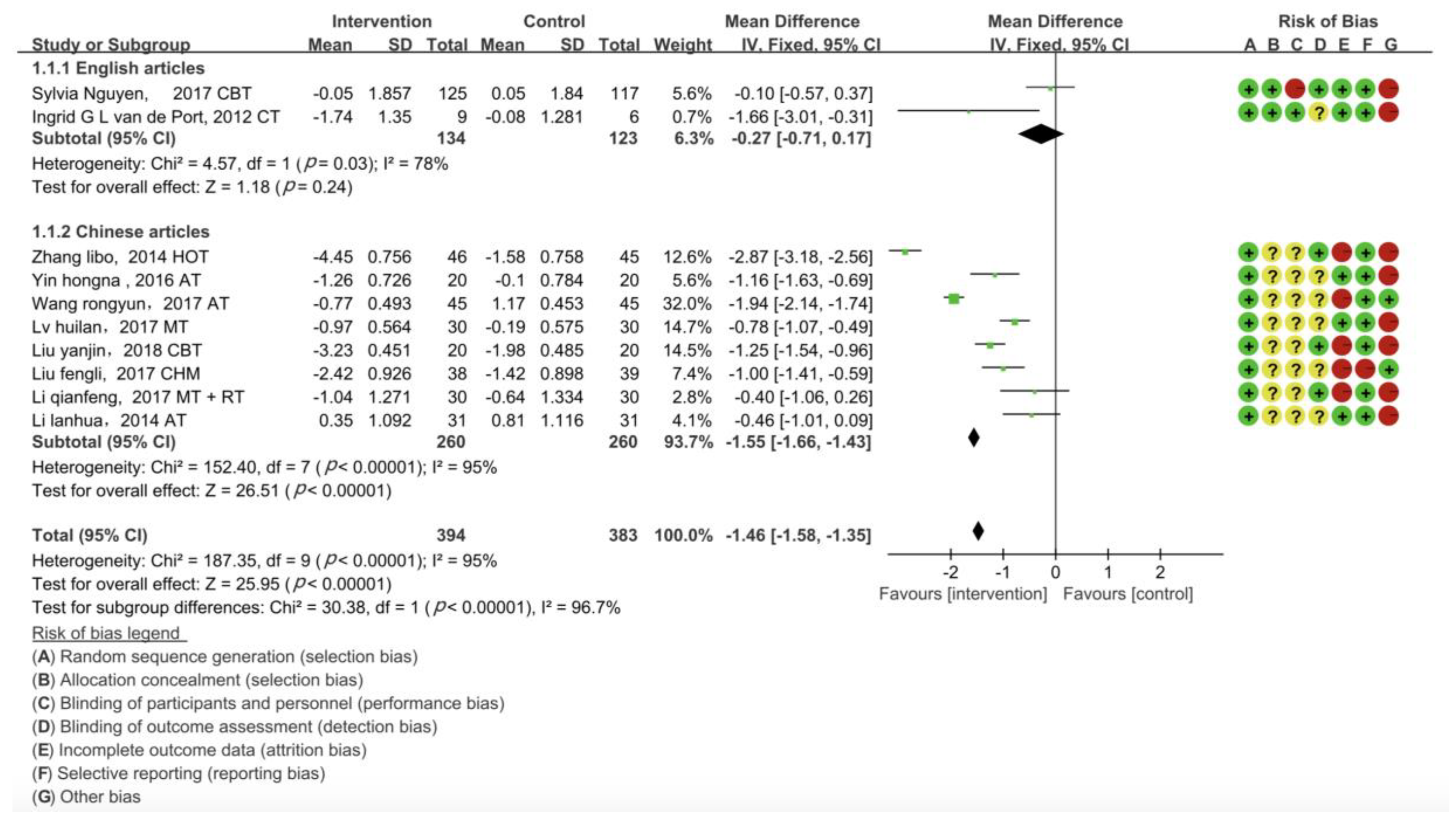
3.3. Pair-Wise Meta-Analysis
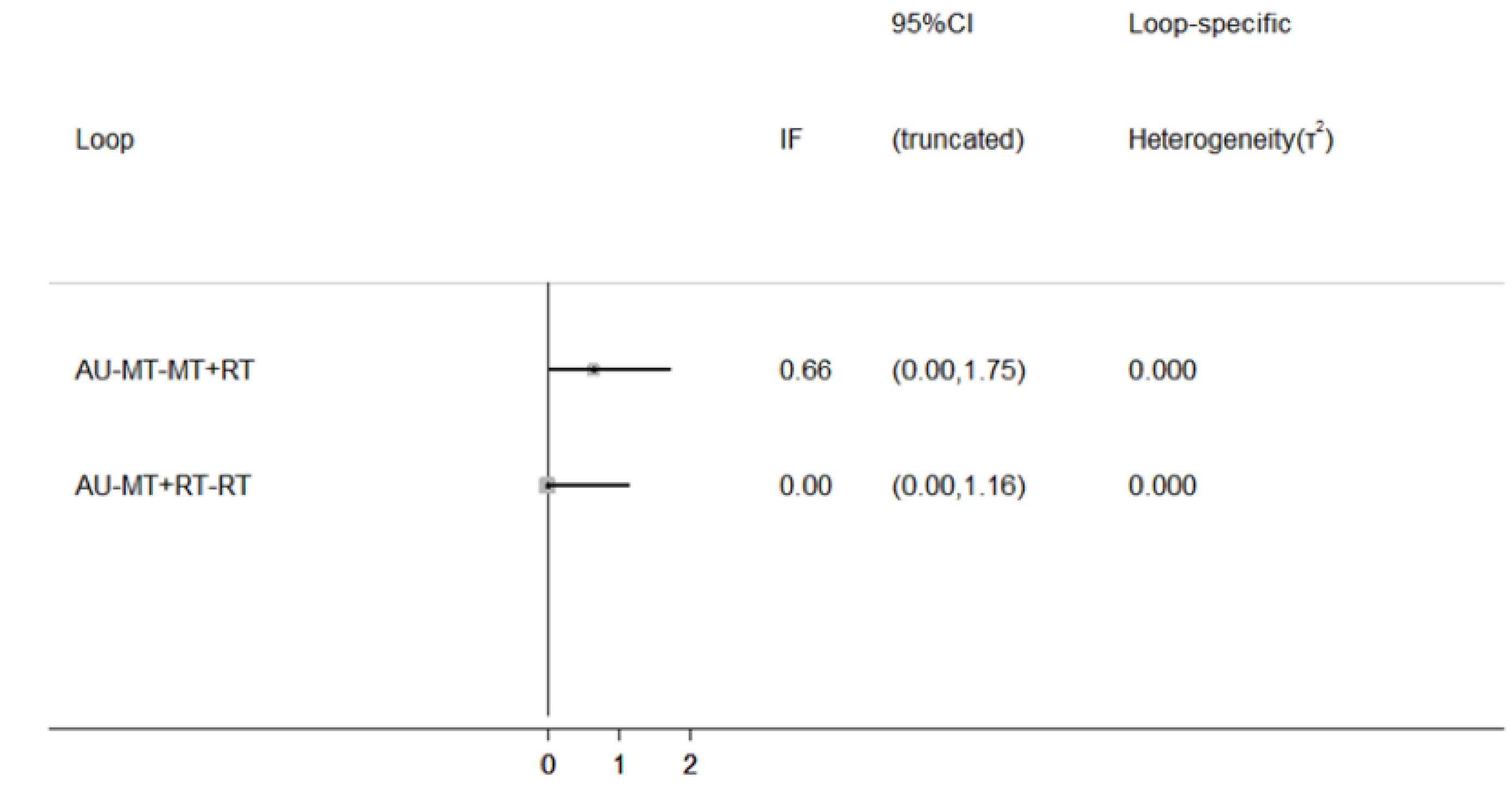
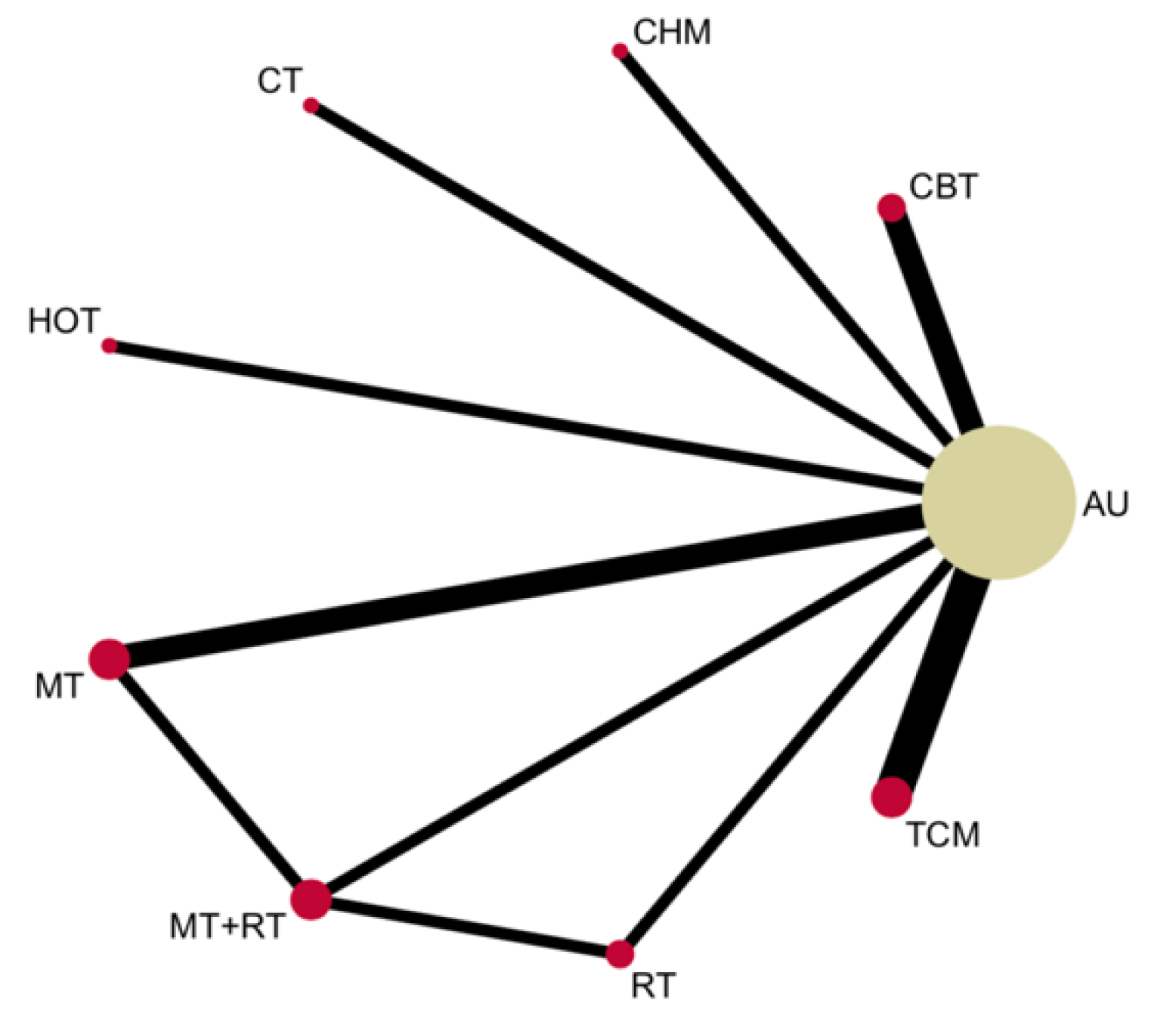
3.4. Network Meta-Analyses for Interventions
3.5. Rank Probability of Interventions
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| S1 | TI stroke or cerebrovascular accident or cva or cerebral vascular event or cve or transient ischemic attack or tia | 89,994 |
| S2 | TI fatigue or exhaustion or tiredness or lethargy | 24,958 |
| S3 | TI fatigue after stroke OR TI post stroke fatigue | 99 |
| S4 | S1 AND S2 | 195 |
| S5 | AB treatment or intervention or therapy or management or rehabilitation | 7,697,803 |
| S6 | TI controlled clinical trial or randomized controlled trail or randomized or placebo or randomly or trial or groups | 478,666 |
| S7 | S3 OR S4 | 195 |
| S8 | S5 AND S6 AND S7 | 7 |
| Author/Year | Country | Type of Stroke | Intervention | N | Mean Age (Years) | Time | p-Value | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Gender (Male) | Intervention | Control | Intervention | Control | Post-Incident Stroke | Endpoint | Baseline vs. Post | Baseline vs. Follow-Up | ||||
| Ingrid G L van de Port, 2012 | Netherlands | Ischemic and Haemorrhagic | CT | 162 | CT = 125 | AU = 117 | 56 | 58 | N/A | 24 weeks | >0.05 | >0.05 |
| Sylvia Nguyen, 2017 | Australia | Ischemic and Haemorrhagic | CBT | 11 | CBT = 9 | AU = 6 | 47 | 51 | 27 months | 16 weeks | <0.05 | <0.05 |
| Lv Huila, 2017 | China | Ischemic and Haemorrhagic | MT | 24 | MT = 20 | AU = 20 | 62 | 62 | 2.28 months | 8 weeks | <0.05 | N/A |
| Yin Hongna, 2016 | China | Ischemic and Haemorrhagic | TCM | 33 | AT = 30 | AU = 30 | 62 | 62 | 2.95 months | 4 weeks | <0.05 | N/A |
| Wang Rongyun, 2017 | China | Ischemic and Haemorrhagic | TCM | 45 | AT = 38 | AU = 39 | 67 | 67 | 2 weeks | 2 weeks | <0.05 | N/A |
| Li Lanhua, 2014 | China | Ischemic and Haemorrhagic | TCM | 51 | AT = 46 | AU = 45 | 51 | 51 | 27days- 20 months | 4 weeks | <0.05 | N/A |
| Liu Vanjin, 2018 | China | Ischemic and Haemorrhagic | CBT | N/A | CBT = 30 | AU = 30 | N/A | N/A | N/A | 8 weeks | <0.05 | N/A |
| Li Qianfeng, 2017 | China | Ischemic | MT RT MT+RT | 47 | MT = 20 RT = 20 MT + RT = 20 | AU = 20 | 57 | 57 | N/A | 8 weeks | <0.05 | N/A |
| Liu Fengli, 2017 | China | Ischemic and Haemorrhagic | CHM | 43 | CHM = 45 | AU = 45 | 47 | 49 | N/A | 12 weeks | <0.05 | N/A |
| Zhang Libo, 2014 | China | Ischemic and Haemorrhagic | HOT | N/A | HOT = 31 | AU = 31 | N/A | N/A | N/A | 4 weeks | <0.05 | N/A |
References
- Cumming, T.B.; Packer, M.; Kramer, S.F.; English, C. The prevalence of fatigue after stroke: A systematic review and meta-analysis. Int. J. Stroke Off. J. Int. Stroke Soc. 2016, 11, 968–977. [Google Scholar] [CrossRef] [PubMed]
- Ingles, J.L.; Eskes, G.A.; Phillips, S.J. Fatigue after stroke. Arch. Phys. Med. Rehabil. 1999, 80, 173–178. [Google Scholar] [CrossRef]
- Lerdal, A.; Bakken, L.N.; Kouwenhoven, S.E.; Pedersen, G.; Kirkevold, M.; Finset, A.; Kim, H.S. Poststroke Fatigue—A Review. J. Pain Symptom Manag. 2009, 38, 928–949. [Google Scholar] [CrossRef] [PubMed]
- Glader, E.L.; Stegmayr, B.; Asplund, K. Poststroke fatigue: A 2-year follow-up study of stroke patients in Sweden. Stroke 2002, 33, 1327–1333. [Google Scholar] [CrossRef]
- Eskes, G.A.; Lanctôt, K.L.; Herrmann, N.; Lindsay, P.; Bayley, M.; Bouvier, L.; Dawson, D.; Egi, S.; Gilchrist, E.; Green, T. Canadian Stroke Best Practice Recommendations: Mood, Cognition and Fatigue Following Stroke practice guidelines, update 2015. Int. J. Stroke 2015, 10, 1130–1140. [Google Scholar] [CrossRef]
- Rowat, A.; Pollock, A.; St George, B.; Cowey, E.; Booth, J.; Lawrence, M.; Scottish Stroke Nurses Forum (SSNF). Top 10 research priorities relating to stroke nursing: A rigorous approach to establish a national nurse-led research agenda. J. Adv. Nurs. 2016, 72, 2831–2843. [Google Scholar] [CrossRef] [Green Version]
- Jason, L.A.; Evans, M.; Brown, M. What is fatigue? Pathological and non-pathological fatigue. PMR 2010, 2, 327–331. [Google Scholar] [CrossRef]
- De Groot, M.H.; Phillips, S.J.; Eskes, G.A. Fatigue Associated with Stroke and Other Neurologic Conditions: Implications for Stroke Rehabilitation. Arch. Phys. Med. Rehabil. 2003, 84, 1714–1720. [Google Scholar] [CrossRef]
- Lynch, J.; Mead, G.; Greig, C.; Young, A.; Lewis, S.; Sharpe, M. Fatigue after stroke: The development and evaluation of a case definition. J. Psychosom. Res. 2007, 63, 539–544. [Google Scholar] [CrossRef]
- McNair, D.M.; Lorr, M.; Droppleman, L.F. Manual for the Profile of Mood States; Educational and Industrial Testing Services: San Diego, CA, USA, 1971. [Google Scholar]
- Krupp, L.B.; Alvarez, L.A.; Larocca, N.G.; Scheinberg, L.C. Fatigue in multiple sclerosis. Arch. Neurol. 1988, 45, 435–437. [Google Scholar] [CrossRef] [PubMed]
- Fisk, J.D.; Ritvo, P.G.; Ross, L.; Haase, D.A.; Marrie, T.J.; Schlech, W.F. Measuring the functional impact of fatigue: Initial validation of the Fatigue Impact Scale. Clin. Infect. Dis. 1994, 18 (Suppl. 1), S79–S83. [Google Scholar] [CrossRef]
- Vercoulen, J.H.M.M.; Swanink, C.M.A.; Fennis, J.F.M.; Galama, J.M.D.; van der Meer, J.W.M.; Bleijenberg, G. Dimensional assessment of chronic fatigue syndrome. J. Psychosom. Res. 1994, 38, 383–392. [Google Scholar] [CrossRef] [Green Version]
- Ware, J.E.; Gandek, B.; The IQOLA Project Group. The SF-36 health survey: Development and use in mental health research and the IQOLA project. Int. J. Mental Health 1994, 23, 49. [Google Scholar] [CrossRef]
- Smets, E.M.; Garssen, B.; Bonke, B.; De Haes, J.C. The multidimensional fatigue inventory (MFI) psychometric qualities of an instrument to assess fatigue. J. Psychosom. Res. 1995, 39, 315–325. [Google Scholar] [CrossRef] [Green Version]
- Cella, D. Manual of the Functional Assessment of Chronic Illness Therapy (FACIT) Measurement System; Version 4; Center on Outcomes, Research and Education (CORE), Evanston Northwestern Healthcare and Northwestern University: Evanston, IL, USA, 1997. [Google Scholar]
- Stein, K.D.; Martin, S.C.; Hann, D.M.; Jacobsen, P.B. A multidimensional measure of fatigue for use with cancer patients. Cancer Pract. 1998, 6, 143–152. [Google Scholar] [CrossRef] [PubMed]
- Mendoza, T.R.; Wang, X.S.; Cleeland, C.S.; Morrissey, M.; Johnson, B.A.; Wendt, J.K.; Huber, S.L. The rapid assessment of fatigue severity in cancer patients: Use of the Brief Fatigue Inventory. Cancer 1999, 85, 1186–1196. [Google Scholar] [CrossRef]
- Michielsen, H.J.; De Vries, J.; Van Heck, G.L. Psychometric qualities of a brief self-rated fatigue measure: The Fatigue Assessment Scale. J. Psychosom. Res. 2003, 54, 345–352. [Google Scholar] [CrossRef]
- Badaru, U.M.; Ogwumike, O.O.; Adeniyi, A.F.; Olowe, O.O. Variation in functional independence among stroke survivors having fatigue and depression. Neurol. Res. Int. 2013, 2013, 842980. [Google Scholar] [CrossRef] [Green Version]
- Kruithof, N.; Van Cleef, M.H.; Rasquin, S.M.; Bovend’Eerdt, T.J. Screening poststroke fatigue; feasibility and validation of an instrument for the screening of poststroke fatigue throughout the rehabilitation process. J. Stroke Cerebrovasc. Dis. 2016, 25, 188–196. [Google Scholar] [CrossRef]
- Hinkle, J.L.; Becker, K.J.; Kim, J.S.; McNair, N.; Choi-Kwon, S.; Saban, K.L.; Mead, G.E.; American Heart Association Council on Cardiovascular and Stroke Nursing and Stroke Council. Poststroke fatigue: Emerging evidence and approaches to management: A scientific statement for healthcare professionals from the American Heart Association. Stroke 2017, 48, e159–e170. [Google Scholar] [CrossRef] [Green Version]
- Catalá-López, F.; Tobías, A.; Cameron, C.; Moher, D.; Hutton, B. Network meta-analysis for comparing treatment effects of multiple interventions: An introduction. Rheumatol. Int. 2014, 34, 1489–1496. [Google Scholar] [CrossRef] [PubMed]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: Checklist and explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, F.; Li, Y.; Jiao, L.; Wang, P.; Zhao, C.; Zhou, Y.; Cheng, R. Effect of community health management on post-stroke fatigue. Chin. J. Prev. Contr. Chron. Dis. 2017, 25, 396–398. [Google Scholar]
- Yin, H.; Guo, Y.; Li, Q. Clinical Observation of Acupuncture at Baihui (GV20) and Sishencong (Ex-hn1) Combined with Rehabilitation Training on Patients of Post Stroke Fatigue. JETCM 2016, 25, 1746–1748. [Google Scholar]
- Li, L.; Zheng, J. Observation on integrated traditional Chinese and Western medicine in post-stroke fatigue rehabilitation. World Chin. Med. 2014, 9, 1155–1157. [Google Scholar]
- Wang, R.; Lin, X.; Sun, Q. Clinical Study on Transcutaneous Acupoint Electrical Nerve Stimulation for Post-stroke Fatigue. Shanghai J. Acupunct. Moxibustion 2017, 36, 14–16. [Google Scholar]
- Nguyen, S.; Wong, D.; McKay, A.; Rajaratnam, S.M.W.; Spitz, G.; Williams, G.; Mansfield, D.; Ponsford, J.L. Cognitive behavioural therapy for post-stroke fatigue and sleep disturbance: A pilot randomised controlled trial with blind assessment. Neuropsychol. Rehabil. 2019, 29, 723–738. [Google Scholar] [CrossRef]
- Liu, Y.; Wang, L.; Dong, X. Influence of cognitive behavioral intervention on health behavior and treatment compliance of patients with post stroke fatigue based on problem solving method. Chin. Nurs. Res. 2018, 32, 327–329. [Google Scholar]
- Lv, H.; Liang, W.; Liu, S.; Wang, Y.; Wang, Y. Effect of music therapy combined with nursing intervention on post-stroke fatigue. Nurs. Pract. Res. 2017, 14, 154–155. [Google Scholar]
- Li, Q.; Wang, Y.; Yang, W. Effect of respiratory training instrument combined with music therapy on rehabilitation of post-stroke fatigue. Chin. J. Integr. Med. Cardio-Cerebrovasc. Dis. 2017, 15, 3207–3210. [Google Scholar]
- van de Port, I.G.; Wevers, L.E.; Lindeman, E.; Kwakkel, G. Effects of circuit training as alternative to usual physiotherapy after stroke: Randomised controlled trial. BMJ 2012, 344, e2672. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Libo, Z.; Xiutang, M.; Yang, W.; Xi, H.; Jie, L.; Tao, L.; Xinnian, D. The influence of hyperbaric oxygen therapy on post-stroke fatigue. Chin. J. Conval. Med. 2014, 23, 503–504. [Google Scholar]
- Lanctôt, K.L.; Lindsay, M.P.; Smith, E.E.; Sahlas, D.J.; Foley, N.; Gubitz, G.; Austin, M.; Ball, K.; Bhogal, S.; Blake, T.; et al. Canadian Stroke Best Practice Recommendations: Mood, Cognition and Fatigue following Stroke, 6th edition update 2019. Int. J. Stroke 2019, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zedlitz, A.M.; Rietveld, T.C.; Geurts, A.C.; Fasotti, L. Cognitive and graded activity training can alleviate persistent fatigue after stroke: A randomized, controlled trial. Stroke 2012, 43, 1046–1051. [Google Scholar] [CrossRef] [Green Version]
- Renner, C.; Outermans, J.; Ludwig, R.; Brendel, C.; Kwakkel, G.; Hummelsheim, H. Group therapy task training versus individual task training during inpatient stroke rehabilitation: A randomised controlled trial. Clin. Rehabil. 2016, 30, 637–648. [Google Scholar] [CrossRef]
- Clarke, A.; Barker-Collo, S.L.; Feigin, V.L. Poststroke Fatigue: Does Group Education Make a Difference? A Randomized Pilot Trial. Top. Stroke Rehabil. 2012, 19, 32–39. [Google Scholar] [CrossRef]
- Emery, C.E. Relieving Post-Stroke Fatigue Using a Group-Based Educational Training Approach. Ph.D. Thesis, Virginia Commonwealth University Richmond, Richmond, VA, USA, April 2015. [Google Scholar]
- Wu, S.; Kutlubaev, M.A.; Chun, H.Y.; Cowey, E.; Pollock, A.; Macleod, M.R.; Dennis, M.; Keane, E.; Sharpe, M.; Mead, G.E. Interventions for post-stroke fatigue. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [Green Version]
- Christensen, D.; Johnsen, S.P.; Watt, T.; Harder, I.; Kirkevold, M.; Andersen, G. Dimensions of Post-Stroke Fatigue: A Two-Year Follow-Up Study. Cerebrovasc. Dis. 2008, 26, 134–141. [Google Scholar] [CrossRef]
- Snaphaan, L.; van der Werf, S.; de Leeuw, F.E. Time course and risk factors of post-stroke fatigue: A prospective cohort study. Eur. J. Neurol. 2011, 18, 611–617. [Google Scholar] [CrossRef]

| Scale | Developed By | Target Population | Items |
|---|---|---|---|
| Profile of Mood States—fatigue subscale (POMS) | McNair et al., 1971 [10] | Psychiatric patients | 65 |
| Fatigue Severity Scale (FSS) | Krupp et al., 1989 [11] | MS, SLE | 9 |
| Fatigue Impact Scale (FIS) | Fisk et al., 1994 [12] | MS, CFS | 40 |
| Checklist of Individual Strength (CIS) | Vercoulen et al., 1994 [13] | CFS | 24 |
| SF-36 (Vitality subscale) | Ware et al., 1994 [14] | Chronic disease patients | 4 |
| Multidimensional Fatigue Inventory (MFI-20) | Smets et al., 1995 [15] | Cancer, CFS, General clinical populations | 20 |
| FACIT (Fatigue Scale) | David Cella, et al., 1997 [16] | Chronic Illness | 13 |
| Multidimensional Fatigue Symptom Inventory (MFIS) | Stein et al., 1998 [17] | Cancer-related fatigue | 6 |
| Brief Fatigue Inventory (BFI) | Tito R et al., 1999 [18] | Cancer-related fatigue | 4 |
| Fatigue Assessment Scale (FAS) | Michielsen et al., 2003 [19] | Workers | 10 |
| Neurological fatigue index-MS (NFI-MS) in stroke | Mills et al., 2012 [20] | MS | 23 |
| Detection List Fatigue (DLF) | Nena Kruithof et al., 2016 [21] | Post-stroke fatigue | 9 |
| TCM | ||||||||
| −1.40 (−3.15, 0.35) | AU | |||||||
| −0.27 (−3.05, 2.61) | 1.13 (−1.05, 3.42) | CBT | ||||||
| 0.46 (−3.02, 3.87) | 1.86 (−1.08, 4.87) | 0.71 (−3.09, 4.44) | CHM | |||||
| −1.61 (−5.19, 1.83) | −0.21 (−3.23, 2.81) | −1.34 (−5.20, 2.24) | −2.07 (−6.35, 2.08) | CT | ||||
| −1.54 (−5.03, 1.83) | −0.16 (−3.20, 2.85) | −1.29 (−5.09, 2.42) | −1.99 (−6.32, 2.15) | 0.05 (−4.24, 4.32) | HOT | |||
| −0.59 (−3.28, 2.16) | 0.80 (−1.30, 2.95) | −0.32 (−3.46, 2.73) | −1.05 (−4.64, 2.68) | 1.01 (−2.62, 4.69) | 0.96 (−2.65, 4.80) | MT | ||
| −0.39 (−3.64, 2.96) | 1.02 (−1.83, 3.94) | −0.08 (−3.94, 3.45) | −0.82 (−5.06, 3.27) | 1.23 (−2.95, 5.38) | 1.17 (−2.92, 5.37) | 0.20 (−2.66, 3.03) | MT + RT | |
| −0.61 (−3.87, 2.71) | 0.78 (−2.00, 3.63) | −0.35 (−3.98, 3.25) | −1.08 (−5.16, 3.15) | 0.99 (−3.09, 5.13) | 0.92 (−3.17, 5.10) | −0.03 (−2.85, 2.80) | −0.24 (−3.29, 2.79) | RT |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, Y.; Yuki, M.; Otsuki, M. Non-Pharmacological Interventions for Post-Stroke Fatigue: Systematic Review and Network Meta-Analysis. J. Clin. Med. 2020, 9, 621. https://doi.org/10.3390/jcm9030621
Su Y, Yuki M, Otsuki M. Non-Pharmacological Interventions for Post-Stroke Fatigue: Systematic Review and Network Meta-Analysis. Journal of Clinical Medicine. 2020; 9(3):621. https://doi.org/10.3390/jcm9030621
Chicago/Turabian StyleSu, Ya, Michiko Yuki, and Mika Otsuki. 2020. "Non-Pharmacological Interventions for Post-Stroke Fatigue: Systematic Review and Network Meta-Analysis" Journal of Clinical Medicine 9, no. 3: 621. https://doi.org/10.3390/jcm9030621
APA StyleSu, Y., Yuki, M., & Otsuki, M. (2020). Non-Pharmacological Interventions for Post-Stroke Fatigue: Systematic Review and Network Meta-Analysis. Journal of Clinical Medicine, 9(3), 621. https://doi.org/10.3390/jcm9030621





