Life Expectancy after Surgery for Ascending Aortic Aneurysm
Abstract
1. Introduction
2. Experimental Section
2.1. Sample and Data Collection
2.2. Objectives
2.3. Statistical Analysis
3. Results
3.1. Patients, Type of Surgery and Postoperative Outcomes.
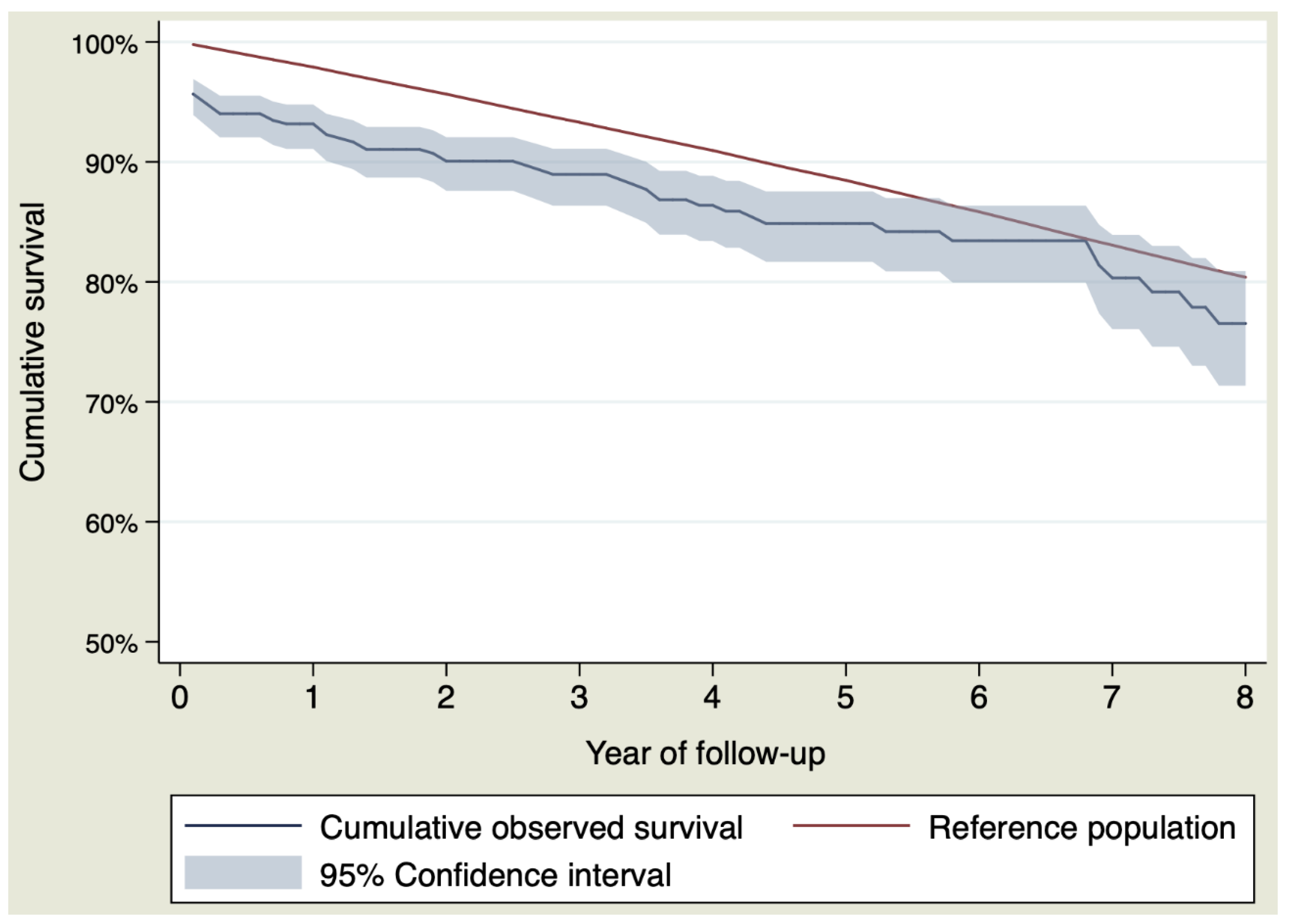
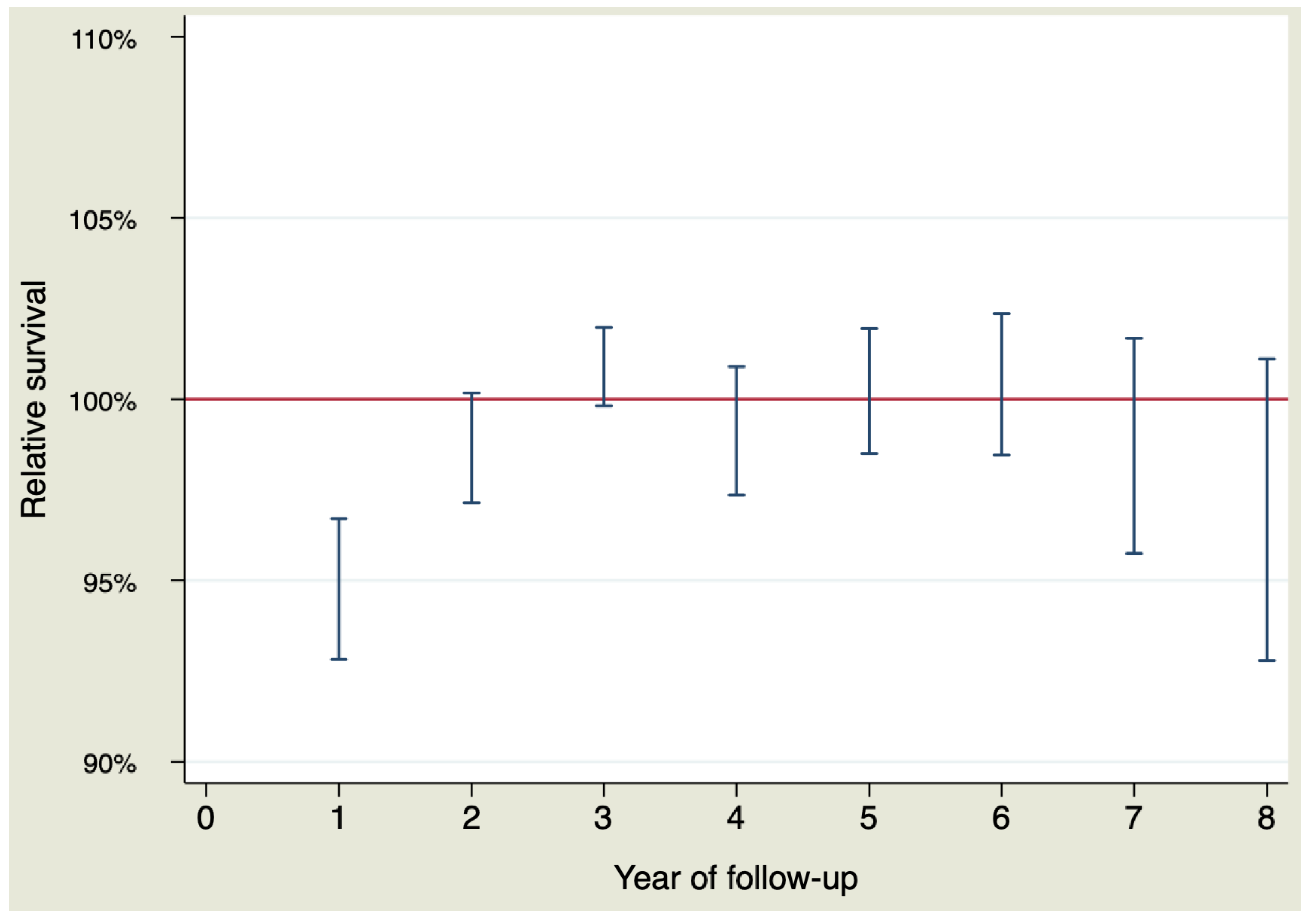
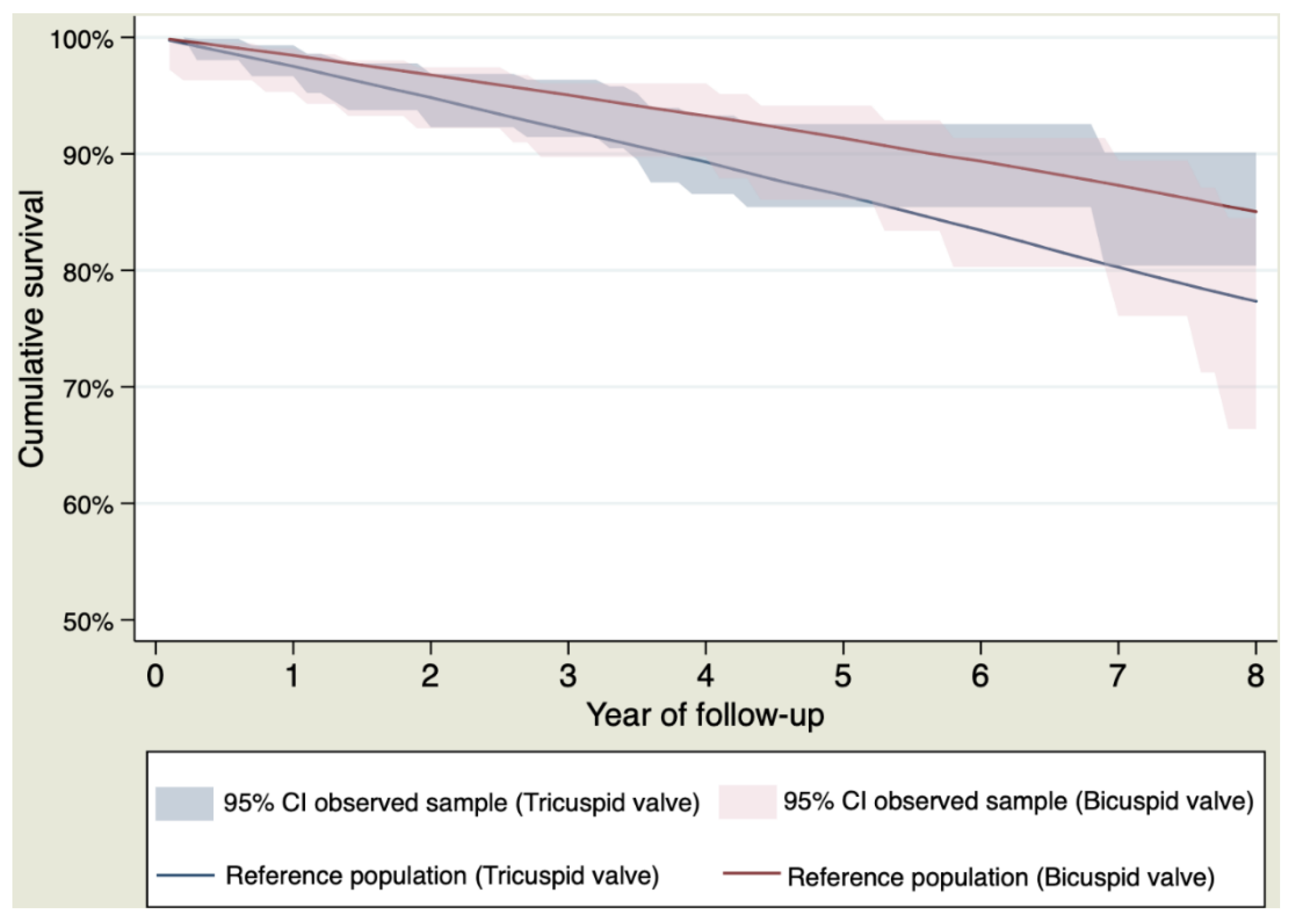
3.2. Life Expectancy of the Whole Sample
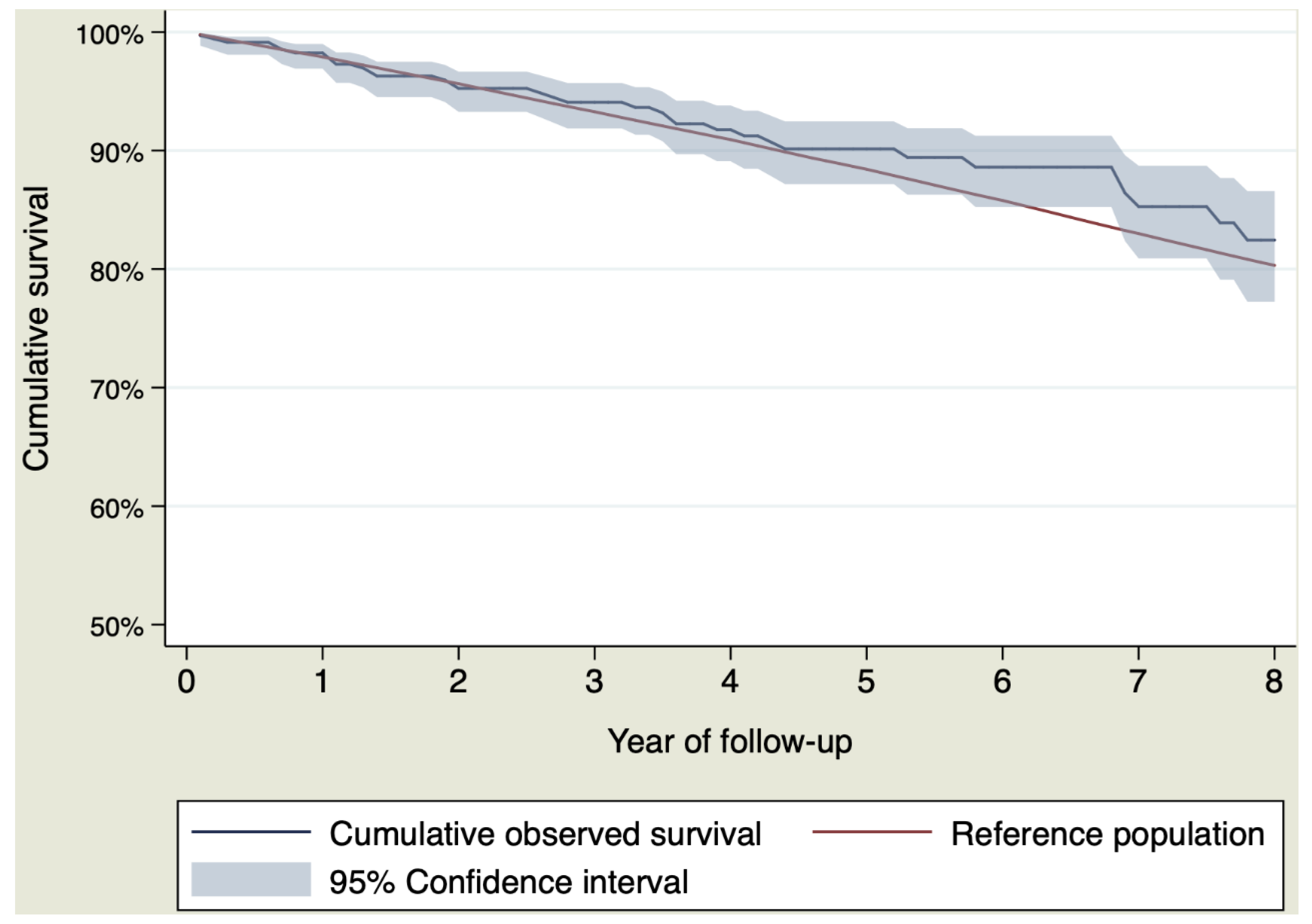
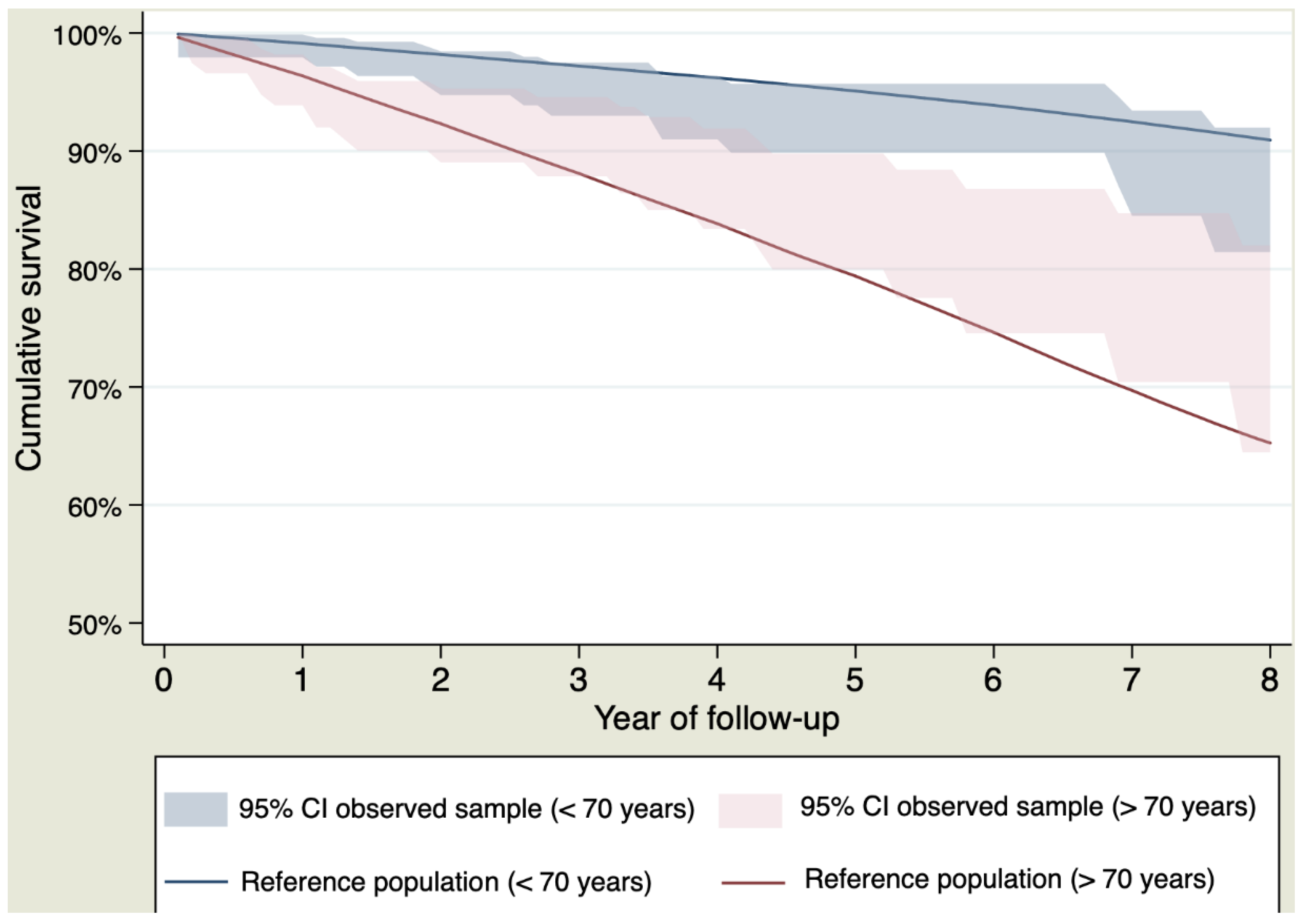
3.3. Life Expectancy for Patients who Survive the Postoperative Period
3.4. Causes of Death During the Follow-up, Risk Factors and Late Complications
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Conflicts of Interest
References
- Erbel, R.; Aboyans, V.; Boileaul, C.; Bossone, E.; Bartolomeo, R.D.; Eggebrecht, H.; Evangelista, A.; Falk, V.; Frank, H.; Gaemperli, O.; et al. ESC Guidelines on the diagnosis and treatment of aortic diseases. Eur. Heart J. 2014, 35, 2873–2926. [Google Scholar] [PubMed]
- McClure, R.S.; Brogly, S.B.; Lajkosz, K.; Payne, D.; Hall, S.F.; Johnson, A.P. Epidemiology and management of thoracic aortic dissections and thoracic aortic aneurysms in Ontario, Canada: A population-based study. J. Thorac. Cardiovasc. Surg. 2018, 155, 2254–2264. [Google Scholar] [CrossRef] [PubMed]
- Ahmad, M.M.; Kiani, I.A.; Amma, K.A.; Ahmad, M.N.; Khandheria, B.K.; Paterick, T.E.; Jain, R.; Tajik, A.J. Ascending Aortic Aneurysm Is an Inherited Disease: A Contemporary Literature Review Based on Hill’s Criteria of Specificity, Strength of Association, and Biological Coherence. Cardiol. Rev. 2017, 25, 268–278. [Google Scholar] [CrossRef] [PubMed]
- González-Santos, J.M.; Arnáiz-García, M.E. Wrapping of the ascending aorta revisited—Is there any role left for conservative treatment of ascending aortic aneurysm? J. Thorac. Dis. 2017, 9 (Suppl. S6), S488–S497. [Google Scholar] [CrossRef] [PubMed]
- Freiberg, M.S.; Arnold, A.M.; Newman, A.B.; Edwards, M.S.; Kraemer, K.L.; Kuller, L.H. Abdominal aortic aneurysms, increasing infrarenal aortic diameter, and risk of total mortality and incident cardiovascular disease events: 10-year follow-up data from the Cardiovascular Health Study. Circulation 2008, 117, 1010–1017. [Google Scholar] [CrossRef] [PubMed]
- Abdulkareem, N.; Soppa, G.; Jones, S.; Valencia, O.; Smelt, J.; Jahangiri, M. Dilatation of the remaining aorta after aortic valve or aortic root replacement in patients with bicuspid aortic valve: A 5-year follow-up. Ann. Thorac. Surg. 2013, 96, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Van Duffel, D.; Van Gemert, R.; Starinieri, P.; Pauwels, J.L.; Natukunda, A.; Rakhmawati, T.W.; Chirehwa, M.T.; Orwa, J.; Thys, H.; Deboosere, P.; et al. Elective reconstruction of the ascending aorta for aneurysmal disease restores normal life expectancy. An analysis of risk factors for early and late mortality. Acta Cardiol. 2013, 68, 349–353. [Google Scholar] [CrossRef] [PubMed]
- Peterss, S.; Mansour, A.M.; Zafar, M.A.; Thombre, K.; Rizzo, J.A.; Ziganshin, B.A.; Darr, U.M.; Elefteriades, J.A. Elective surgery for ascending aortic aneurysm in the elderly: Should there be an age cut-off? Eur. J. Cardiothorac. Surg. 2017, 51, 965–970. [Google Scholar] [CrossRef] [PubMed]
- Idrees, J.J.; Roselli, E.E.; Lowry, A.M.; Reside, J.M.; Javadikasgari, H.; Johnson, D.J.; Soltesz, E.G.; Johnston, D.R.; Pettersson, G.B.; Blackstone, E.H.; et al. Outcomes After Elective Proximal Aortic Replacement: A Matched Comparison of Isolated Versus Multicomponent Operations. Ann. Thorac. Surg. 2016, 101, 2185–2192. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Narayan, P.; Caputo, M.; Rogers, C.A.; Alwair, H.; Mahesh, B.; Angelini, G.D.; Bryan, A.J. Early and mid-term outcomes of surgery of the ascending aorta/arch: Is there a relationship with caseload? Eur. J. Cardiothorac. Surg. 2004, 25, 676–682. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Wanamaker, K.M.; Hirji, S.A.; Del Val, F.R.; Yammine, M.; Lee, J.; McGurk, S.; Shekar, P.; Kaneko, T. Proximal aortic surgery in the elderly population: Is advanced age a contraindication for surgery? J. Thorac. Cardiovasc. Surg. 2019, 157, 53–63. [Google Scholar] [CrossRef] [PubMed]
- Pan, E.; Kytö, V.; Savunen, T.; Gunn, J. Early and late outcomes after open ascending aortic surgery: 47-year experience in a single centre. Heart Vessels 2018, 33, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Park, C.B.; Greason, K.L.; Suri, R.M.; Michelena, H.I.; Schaff, H.V.; Sundt, T.M., 3rd. Should the proximal arch be routinely replaced in patients with bicuspid aortic valve disease and ascending aortic aneurysm? J. Thorac. Cardiovasc. Surg. 2011, 142, 602–607. [Google Scholar] [CrossRef] [PubMed]
- Ballester, J.; Robine, J.M.; Herrmann, F.R.; Rodó, X. Effect of the Great Recession on regional mortality trends in Europe. Nat. Commun. 2019, 8, 679. [Google Scholar] [CrossRef] [PubMed]
- The Organisation for Economic Co-operation and Development (OECD). Data. Life Expectancy at 65. Available online: https://data.oecd.org/healthstat/life-expectancy-at-65.htm (accessed on 1 September 2019).
- Instituto Nacional de Estadística. Tables for Mortality. Available online: http://www.ine.es/jaxiT3/Tabla.htm?t=27154 (accessed on 1 September 2019).
- Hakulinen, T.; Seppä, K.; Lambert, P.C. Choosing the relative survival method for cancer survival estimation. Eur. J. Cancer 2011, 47, 2202–2210. [Google Scholar] [CrossRef] [PubMed]
- Mariotto, A.B.; Noone, A.M.; Howlader, N.; Cho, H.; Keel, G.E.; Garshell, J.; Woloshin, S.; Schwartz, L.M. Cancer Survival: An Overview of Measures, Uses, and Interpretation. J. Natl. Cancer Inst. Monogr. 2014, 49, 145–186. [Google Scholar] [CrossRef] [PubMed]
- Glaser, N.; Persson, M.; Jackson, V.; Holzmann, M.J.; Franco-Cereceda, A.; Sartipy, U. Loss in life expectancy after surgical aortic valve replacement. J. Am. Coll. Cardiol. 2019, 74, 26–33. [Google Scholar] [CrossRef] [PubMed]
- Dickman, P.W.; Coviello, E. Estimating and Modeling Relative Survival. Stata J. 2015, 15, 186–215. [Google Scholar] [CrossRef]
- Bilkhu, R.; Youssefi, P.; Soppa, G.; Theodoropoulos, P.; Phillips, S.; Liban, B.; Child, A.; Tome, M.; Nowell, J.; Sharma, R.; et al. Fate of the Aortic Arch Following Surgery on Aortic Root and Ascending Aorta in Bicuspid Aortic Valve. Ann. Thorac. Surg. 2018, 106, 771–776. [Google Scholar] [CrossRef] [PubMed]
| Variable | Value |
|---|---|
| Age (years) | 65.27 ± 13.09 |
| Women | 232 (31.44%) |
| Body mass index (kg/m2) | 28.15 ± 4.54 |
| Body surface area (m2) | 1.85 ± 0.20 |
| Hypertension | 492 (66.67%) |
| Diabetes mellitus | |
| Type 1 | 12 (1.63%) |
| Type 2 | 65 (8.81%) |
| Dyslipidaemia | 241 (32.66%) |
| Previous stroke | 28 (3.79%) |
| Previous acute myocardial infarction | 16 (2.27%) |
| Extracardiac arteriopathy | 26 (3.53%) |
| Renal impairment | |
| Creatinine clearance >85 mL/min | 520 (70.65%) |
| Creatinine clearance 50–85 mL/min | 164 (22.28%) |
| Creatinine clearance <50 mL/min | 52 (7.07%) |
| Chronic pulmonary disease | 108 (14.63%) |
| Poor mobility | 2 (0.27%) |
| EuroScore 2 | 3.68 ± 3.65 |
| Logistic EuroSCORE | 13.19 ± 9.86 |
| NYHA functional class: | |
| NYHA I/IV | 136 (18.43%) |
| NYHA II/IV | 374 (50.68%) |
| NYHA III/IV | 202 (27.37%) |
| NYHA IV/IV | 26 (3.52%) |
| Previous atrial fibrillation | |
| Paroxysmal atrial fibrillation | 34 (4.62%) |
| Persistent or permanent atrial fibrillation | 115 (15.63%) |
| PASP | |
| 31–55 mmHg | 156 (21.14%) |
| > 55 mmHg | 19 (2.57%) |
| LVEF (%) | |
| 31–50% | 164 (22.22%) |
| 21–30% | 29 (3.93%) |
| <20% | 2 (0.27%) |
| Grade of aortic stenosis | |
| I | 40 (5.42%) |
| II | 29 (3.93%) |
| III | 40 (5.42%) |
| IV | 233 (31.57%) |
| Grade of aortic regurgitation | |
| I | 74 (10.03%) |
| II | 83 (11.25%) |
| III | 134 (18.16%) |
| IV | 232 (31.44%) |
| Bicuspid aortic valve | 296 (40.11%) |
| Severe ventricular hypertrophy | 111 (15.22%) |
| Diameter of the aorta (mm) | |
| Sinus of Valsalva | 42.77 ± 7.07 |
| Ascending aorta | 50.93 ± 8.43 |
| Aortic arch | 40.6 ± 9.22 |
| Variable | Value |
|---|---|
| Intraoperative characteristics | |
| Type of Surgery Aortic valve replacement and ascending aorta replacement Aortic root remodelling with ascending aorta replacement Isolated ascending aorta replacement Bentall-Bonno procedures with ascending aorta replacement Ascending aorta and aortic arch replacement Ascending aorta replacement and aortic valve repair Aortic valve replacement, ascending aorta replacement and aortic arch replacement | 386 (52.30%) 140 (18.97%) 86 (11.65%) 57 (7.72%) 30 (4.07%) 23 (3.11%) 16 (2.17%) |
| Cardiopulmonary bypass time | 139 ± 60 |
| Cross-clamping time | 112 ± 52 |
| Surgery with circulatory arrest | 84 (11.38%) |
| Using deep hypothermia | 13 (15.48%) |
| Using moderate hypothermia with antegrade cerebral perfusion | 71 (84.52%) |
| Concomitant coronary surgery | 114 (15.44%) |
| Number of the prosthetic tube | |
| 26 | 75 (10.16%) |
| 28 | 209 (28.32%) |
| 30 | 340 (46.07%) |
| 32 | 91 (12.33%) |
| 34 | 21 (2.85%) |
| 36 | 2 (0.27%) |
| EuroScore 2 | 3.68 ± 3.65 |
| Logistic EuroSCORE | 13.19 ± 9.86 |
| Postoperative complications | |
| Permanent pacemaker | 46 (6.23%) |
| New atrial fibrillation | 144 (19.83%) |
| Reoperation for bleeding | 48 (6.50%) |
| Stroke | 33 (4.47%) |
| New renal failure | 25 (3.38%) |
| Medication at discharge | |
| Angiotensin II receptor blockers | 161 (21.82%) |
| Angiotensin-converting enzyme inhibitors | 155 (20.00%) |
| Beta blockers | 434 (59.78%) |
| Statins | 278 (38.29%) |
| Cause | Value |
|---|---|
| Causes of re-operation | |
| Aorta-related | |
| Treated by endovascular therapy | 10 (1.36%) |
| Aneurysm | 6 (0.81%) |
| Dissection | 5 (0.54%) |
| Treated by open cardiac surgery | |
| Pseudoaneurysm | 8 (1.08%) |
| New aneurysm | 2 (0.27%) |
| Non aorta-related | |
| Endocarditis | 10 (1.36%) |
| Prosthesis thrombosis | 2 (0.36%) |
| Periprosthetic aortic regurgitation | 3 (0.41%) |
| Prosthetic degeneration | 3 (0.41%) |
| Myxoma | 2 (0.36%) |
| Failed aortic repair | 7 (0.95%) |
| Causes of death | |
| Peri-operative period n = 44 | |
| Cardiogenic shock | 21 (2.85%) |
| Hemorrhagic shock | 6 (0.81%) |
| Infection/Sepsis | 11 (1.49%) |
| Others | 6 (0.81%) |
| Follow-up n = 86 (Between survivors of the postoperative period) | |
| Cancer | 24 (3.46%) |
| Cardiac failure | 18 (2.59%) |
| Infection or sepsis | 10 (1.44%) |
| Stroke | 6 (0.86%) |
| Acute aortic syndrome | 3 (0.43%) |
| Sudden death | 3 (0.43%) |
| Other cause | 22 (3.17%) |
| Year of Follow-up | Cumulative Survival in the Sample | Cumulative Survival in the Reference | Annual Relative Survival* |
|---|---|---|---|
| First year | 93.17% (CI 95% 91.08–94.78%) | 97.90% | 95.02% (CI 95% 92.82–96.71%) |
| Second year | 90.06% (CI 95% 87.59–92.05%) | 95.65% | 98.98% (CI 95% 97.15–100.18%) |
| Third year | 88.96% (CI 95% 86.35–91.10%) | 93.30% | 100.31% (CI 95% 99.82–101.99%) |
| Fourth year | 86.37% (CI 95% 83.41–88.85%) | 90.95% | 99.60% (CI 95% 97.36–100.90%) |
| Fifth year | 84.86% (CI 95% 81.67–87.53%) | 88.46% | 100.87% (CI 95% 98.50–101.96%) |
| Sixth year | 83.42% (CI 95% 79.95–86.35%) | 85.84% | 101.29% (CI 95% 98.46–102.37%) |
| Seventh year | 80.33% (CI 95% 76.05–83.92%) | 83.06% | 99.81% (CI 95% 95.75–101.69%) |
| Eighth year | 76.53% (CI 95% 71.35–80.91%) | 80.39% | 98.46% (CI 95% 92.79–101.12%) |
| Year of Follow-up | Cumulative Survival in the Sample | Cumulative Survival in the Reference | Annual Relative Survival* |
|---|---|---|---|
| First year | 98.23% (CI 95% 96.91–98.99%) | 97.90% | 100.30% (CI 95% 98.92–101.09%) |
| Second year | 95.24% (CI 95% 93.26–96.65%) | 95.64% | 99.31% (CI 95% 97.53–100.45%) |
| Third year | 94.08% (CI 95% 91.87–95.70%) | 93.27% | 101.31% (CI 95% 99.81–101.99%) |
| Fourth year | 91.76% (CI 95% 89.10–93.80%) | 90.92% | 100.10% (CI 95% 97.96–101.26%) |
| Fifth year | 90.14% (CI 95% 87.17–92.46%) | 88.42% | 100.87% (CI 95% 98.48–101.96%) |
| Sixth year | 88.61% (CI 95% 85.24–91.25%) | 85.79% | 101.29% (CI 95% 98.44–102.38%) |
| Seventh year | 85.27% (CI 95% 80.90–88.72%) | 83.00% | 99.79% (CI 95% 95.68–101.69%) |
| Eighth year | 82.45% (CI 95% 77.24–86.57%) | 80.31% | 100.07% (CI 95% 94.79–102.12%) |
| Variable | HR | 95% CI | p Value |
|---|---|---|---|
| Women | 0.77 | 0.51–1.21 | 0.29 |
| Age | 1.03 | 1.01–1.05 | 0.002 |
| Type of surgery | |||
| Aortic valve replacement and ascending aorta replacement | 1.62 | 0.86–3.03 | 0.14 |
| Aortic root remodelling with ascending aorta replacement | 1.19 | 0.49–2.86 | 0.74 |
| Bentall-Bonno procedures with ascending aorta replacement | 1.93 | 0.81–4.76 | 0.14 |
| Ascending aorta and aortic arch replacement | 4.95 | 1.94–12.6 | 0.001 |
| Ascending aorta replacement and aortic valve repair | 2.55 | 0.76–8.56 | 0.13 |
| Aortic valve replacement, ascending aorta replacement and aortic arch replacement | 6.1 | 2.16–17.34 | 0.001 |
| Renal impairment | |||
| Creatinine clearance 50–85 mL/min | 1.39 | 0.90–2.17 | 0.14 |
| Creatinine clearance <50 mL/min | 1.73 | 0.98–3.07 | 0.059 |
| Diabetes | |||
| Type-2 | 0.89 | 0.45–1.72 | 0.85 |
| Type-1 | 2.22 | 0.98–5.14 | 0.06 |
| Extracardiac arteriopathy | 0.33 | 0.08–1.37 | 0.13 |
| Chronic pulmonary disease | 1.2 | 0.74–1.95 | 0.46 |
| PASP | |||
| 31–55 mmHg | 0.99 | 0.25–4.12 | 0.99 |
| >55 mmHg | 1.21 | 0.78–1.88 | 0.39 |
| LVEF (%) | |||
| 31–50% | 0.88 | 0.55–1.42 | 0.61 |
| 21–30% | 1.09 | 0.39–3.06 | 0.86 |
| <20% | 10.95 | 2.32–51.21 | 0.002 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hernandez-Vaquero, D.; Silva, J.; Escalera, A.; Álvarez-Cabo, R.; Morales, C.; Díaz, R.; Avanzas, P.; Moris, C.; Pascual, I. Life Expectancy after Surgery for Ascending Aortic Aneurysm. J. Clin. Med. 2020, 9, 615. https://doi.org/10.3390/jcm9030615
Hernandez-Vaquero D, Silva J, Escalera A, Álvarez-Cabo R, Morales C, Díaz R, Avanzas P, Moris C, Pascual I. Life Expectancy after Surgery for Ascending Aortic Aneurysm. Journal of Clinical Medicine. 2020; 9(3):615. https://doi.org/10.3390/jcm9030615
Chicago/Turabian StyleHernandez-Vaquero, Daniel, Jacobo Silva, Alain Escalera, Rubén Álvarez-Cabo, Carlos Morales, Rocío Díaz, Pablo Avanzas, Cesar Moris, and Isaac Pascual. 2020. "Life Expectancy after Surgery for Ascending Aortic Aneurysm" Journal of Clinical Medicine 9, no. 3: 615. https://doi.org/10.3390/jcm9030615
APA StyleHernandez-Vaquero, D., Silva, J., Escalera, A., Álvarez-Cabo, R., Morales, C., Díaz, R., Avanzas, P., Moris, C., & Pascual, I. (2020). Life Expectancy after Surgery for Ascending Aortic Aneurysm. Journal of Clinical Medicine, 9(3), 615. https://doi.org/10.3390/jcm9030615






