Outcomes After Transjugular Intrahepatic Portosystemic Shunt in Cirrhotic Patients 70 Years and Older
Abstract
1. Introduction
2. Experimental Section
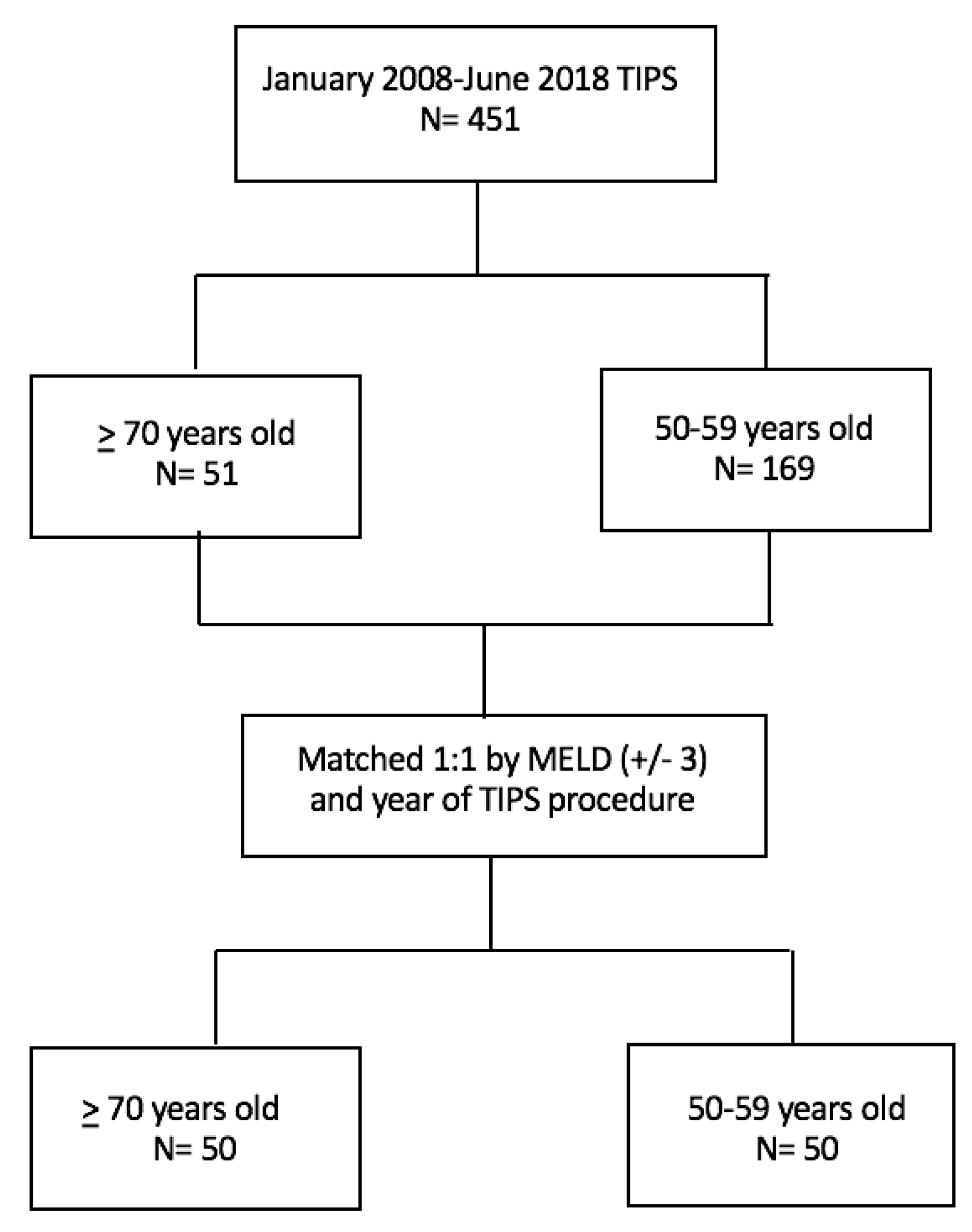
2.1. Patient Selection
2.2. Objectives of the Study
2.3. Data Collection
2.4. TIPS Indications
2.5. TIPS Technique
2.6. Statistics
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Kim, W.R.; Lake, J.R.; Smith, J.M.; Schladt, D.P.; Skeans, M.A.; Noreen, S.M.; Robinson, A.M.; Miller, E.; Snyder, J.J.; Israni, A.K.; et al. OPTN/SRTR 2017 Annual Data Report: Liver. Am. J. Transplant. 2019, 19, 184–283. [Google Scholar] [CrossRef]
- Vincent, G.K.; Velkoff, V.A. The next four decades: The Older Population in the United States: 2010 to 2050; US Department of Commerce, Economics and Statistics Administration, US Census Bureau: Washington DC, USA, 2010; pp. 25–1138.
- Goldacre, M.J. Demography of aging and the epidemiology of gastrointestinal disorders in the elderly. Best Pract. Res. Clin. Gastroenterol. 2009, 23, 793–804. [Google Scholar] [CrossRef] [PubMed]
- Summary Health Statistics: National Health Interview Survey; Centers for Disease Control and Prevention: Atlanta, GA, USA, 2017; Table A-4b; pp. 1–9.
- Adams, L.A.; Lymp, J.F.; Sauver, J.S.; Sanderson, S.O.; Lindor, K.D.; Feldstein, A.; Angulo, P. The Natural History of Nonalcoholic Fatty Liver Disease: A Population-Based Cohort Study. Gastroenterology 2005, 129, 113–121. [Google Scholar] [CrossRef] [PubMed]
- Runyon, B.A. Management of adult patient with ascites due to cirrhosis: An update. Hepatology 2009, 46, 2087–2107. [Google Scholar]
- Garcia-Tsao, G.; Abraldes, J.G.; Berzigotti, A.; Bosch, J. Portal hypertensive bleeding in cirrhosis: Risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the study of liver diseases. Hepatology 2017, 65, 310–335. [Google Scholar] [CrossRef] [PubMed]
- Laberge, J.M.; Somberg, K.A.; Lake, J.R.; Gordon, R.L.; Kerlan, R.K., Jr.; Ascher, N.L.; Roberts, J.P.; Simor, M.M.; Doherty, C.A.; Hahn, J.; et al. Two year outcome following transjugular intrahepatic portosystemic stent-shunt for variceal bleeding: Results in 90 patients. Gastroenterology 1995, 108, 1143–1151. [Google Scholar] [CrossRef]
- Boyer, T.D.; Haskal, Z.J. The role of transjugular intrahepatic portosystemic shunt (TIPS) in the management of portal hypertension: Update 2009. Hepatology 2010, 51, 306. [Google Scholar] [CrossRef]
- Gaba, R.C.; Bui, J.T.; Cotler, S.J.; Kallwitz, E.R.; Mengin, O.T.; Martinez, B.K.; Berkes, J.L.; Carrillo, T.C.; Knuttinen, M.G.; Owens, C.A. Rebleeding rates following TIPS for variceal hemorrhage in the Viatorr era: TIPS alone versus TIPS with variceal embolization. Hepatol. Int. 2010, 4, 749–756. [Google Scholar] [CrossRef]
- Gaba, R.C.; Omene, B.O.; Podczerwinski, E.S.; Knuttinen, M.G.; Cotler, S.J.; Kallwitz, E.R.; Berkes, J.L.; Walzwe, N.M.; Bui, J.T.; Owens, C.A. TIPS for Treatment of Variceal Hemorrhage: Clinical Outcomes in 128 Patients at a Single Institution over a 12-Year Period. J. Vasc. Interv. Radiol. 2012, 23, 227–235. [Google Scholar] [CrossRef]
- Casadaban, L.C.; Parvinian, A.; Minocha, J.; Lakhoo, J.; Grant, C.W.; Ray, C.E., Jr.; Knuttinen, M.G.; Bui, J.T.; Gaba, R.C. Clearing the Confusion over Hepatic Encephalopathy After TIPS Creation: Incidence, Prognostic Factors, and Clinical Outcomes. Dig. Dis. Sci. 2015, 60, 1059. [Google Scholar] [CrossRef]
- Somberg, K.A.; Riegler, J.L.; LaBerg, J.M.; Doherty-Simor, M.M.; Bachetti, P.; Roberts, J.P.; Lake, J.R. Hepatic Encephalopathy after Transjugular Intrahepatic Portosystemic Shunts: Incidence and Risk Factors. Am. J. Gastroenterol. 1995, 90, 549–555. [Google Scholar]
- Suraweera, D.; Jimenez, M.; Viramontes, M.; Jamal, N.; Grotts, J.; Elashoff, D.; Lee, E.W.; Saab, S. Age-related Morbidity and Mortality After Transjugular Intrahepatic Portosystemic Shunts. J. Clin. Gastroenterol. 2017, 51, 360–363. [Google Scholar] [CrossRef] [PubMed]
- Syed, M.I.; Karsan, H.; Ferral, H.; Shaikh, A.; Waheed, U.; Akhter, T.; Gabbard, A.; Morar, K.; Tyrrell, R. Transjugular intrahepatic porto-systemic shunt in the elderly: Palliation for complications of portal hypertension. World J. Hepatol. 2012, 4, 35–42. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Wang, F.; Chen, X.; Li, B.; Meng, W.; Qin, C. Short outcome comparison of elderly patients versus nonelderly patients treated with transjugular intrahepatic portosystemic stent shunt: A propensity score matched cohort study. Medicine 2017, 96, e7551. [Google Scholar] [CrossRef] [PubMed]
- Pan, J.J.; Chen, C.; Caridi, J.G.; Geller, B.; Firpi, R.; Machicao, V.I.; Hawkins, I.F., Jr.; Soldevila-Pico, C.; Nelson, D.R.; Morelli, G. Factors predicting survival after transjugular intrahepatic portosystemic shunt creation: 15 years’ experience from a single tertiary medical center. J. Vasc. Interv. Radiol. 2008, 19, 1576–1581. [Google Scholar] [CrossRef]
- Russo, M.W.; Sood, A.; Jacobson, I.M.; Brown, R.S., Jr. Transjugular intrahepatic portosystemic shunt for refractory ascites: An analysis of the literature on efficacy, morbidity, and mortality. Am. J. Gastroenterol. 2003, 98, 2521–2527. [Google Scholar]
- Riggio, O.; Angeloni, S.; Salvatori, F.M.; De Santis, A.; Cerini, F.; Farcomeni, A.; Attili, A.F.; Merli, M. Incidence, Natural History, and Risk Factors of Hepatic Encephalopathy After Transjugular Intrahepatic Portosystemic Shunt With Polytetrafluoroethylene-Covered Stent Grafts. Am. J. Gastroenterol. 2008, 3, 2738–2746. [Google Scholar] [CrossRef]
- Parvinian, A.; Shah, K.D.; Couture, P.M.; Minocha, J.; Knuttinen, M.G.; Bui, J.T.; Gaba, R.C. Older Patient Age May Predict Early Mortality after Transjugular Intrahepatic Portosystemic Shunt Creation in Individuals at Intermediate Risk. J. Vasc. Interv. Radiol. 2013, 24, 941–946. [Google Scholar] [CrossRef]
- Lee, E.W.; Kuei, A.; Saab, S.; Busuttil, R.W.; Durazo, F.; Han, S.H.; El-Kabany, M.M.; McWilliams, J.; Kee, S.T. Nationwide Trends of Mortality in 83884 TIPS in United States. World J. Gastroenterol. 2016, 22, 5780–5789. [Google Scholar] [CrossRef]
- Tan, H.K.; James, P.D.; Sniderman, K.W.; Wong, F. Long-term clinical outcome of patients with cirrhosis and refractory ascites treated with transjugular intrahepatic portosystemic shunt insertion. J. Gastroenterol. Hepatol. 2015, 30, 389–395. [Google Scholar] [CrossRef]
- Deschênes, M.; Dufresne, M.P.; Bui, B.; Fenyves, D.; Spahr, L.; Roy, L.; Lafortune, M.; Pomier-Layrargues, G. Predictors of clinical response to transjugular intrahepatic portosystemic shunt (TIPS) in cirrhotic patients with refractory ascites. Am. J. Gastroenterol. 1999, 94, 1361–1365. [Google Scholar]
- Thuluvuth, P.J.; Bal, J.S.; Mitchell, S.; Lund, G.; Venbrux, A. TIPS for Management of Refractory Ascites: Response and Survival Are Both Unpredictable. Dig. Dis. Sci. 2003, 48, 542–550. [Google Scholar] [CrossRef]
- Rees, C.J.; Rose, J.D.; Record, C.O.; Bassendine, M.F.; James, O.F.; Hudson, M. Transjugular intrahepatic portosystemic shunt: A limited role in refractory ascites. Eur. J. Gastroenterol. Hepatol. 1997, 9, 969–973. [Google Scholar] [CrossRef] [PubMed]
- Ferral, H.; Patel, N.H. Selection Criteria for Patients Undergoing Transjugular Intrahepatic Portosystemic Shunt Procedures: Current Status. J. Vasc. Interv. Radiol. 2005, 16, 449–455. [Google Scholar] [CrossRef] [PubMed]
- Saad, N.; Rude, M.K.; Darcy, M.; Hanin, J.B.; Wentworth, A.; Korenblat, K.M. Older age is associated with increased mortality after transjugular intrahepatic portosystemic shunt. Ann. Hepatol. 2016, 15, 215–221. [Google Scholar] [PubMed]
- Popovic, P.; Zore, A.; Surlan Popovic, K.; Garbajs, M.; Skok, P. Hepatic Encephalopathy after Transjugular Intrahepatic Portosystemic Shunt in Patients with Recurrent Variceal Hemorrhage. Gastroenterol Res. Pract. 2013, 2013, 398172. [Google Scholar]
- Bai, M.; Qi, X.; Yang, Z.; Yin, Z.; Nie, Y.; Yuan, S.; Wu, K.; Han, G.; Fan, D. Predictors of hepatic encephalopathy after transjugular intrahepatic portosystemic shunt in cirrhotic patients: A systematic review. J. Gastroenterol. Hepatol. 2011, 26, 943–951. [Google Scholar] [CrossRef]
| Total n = 100 | Age 50–59 | Age ≥ 70–84 | |
| n (%) | |||
| Age, median (IQR) | 65 (18) | 55 (4) | 73 (6) |
| Female | 40 (40) | 18 (36) | 22 (44) |
| White | 89 (89) | 43 (86) | 46 (92) |
| Black | 7 (7) | 6 (12) | 1 (2) |
| Asian | 2 (2) | 0 | 2 (2) |
| Other | 2 (2) | 1 (2) | 1 (1) |
| Hispanic | 1 (1) | 1 (2) | 0 |
| Etiology of liver disease | n (%) | ||
| Alcohol | 21 (21) | 13 (26) | 8 (16) |
| Nonalcoholic fatty liver disease (NAFLD) | 33 (33) | 5 (10) | 28 (56) |
| Hepatitis C | 27 (27) | 26 (52) | 2 (1) |
| Autoimmune | 3 (3) | 1 (2) | 2 (4) |
| Cryptogenic | 12 (12) | 3 (6) | 9 (18) |
| Value (Median IQR) | |||
| Median MELD-Na | 12 (7) | 12 (7) | 12 (7) |
| Median MELD | 11 (5) | 11 (6) | 11 (5) |
| Total bilirubin mg/dL | 1.3 (0.8) | 1.3 (1) | 1.3 (0.8) |
| INR | 1.2 (0.2) | 1.3 (1.2) | 1.2 (1.1) |
| Creatinine mg/dL | 1.1 (0.5) | 1.1 (0.7) | 1.3 (0.7) |
| Sodium mmol/L | 138 (9) | 138 (6) | 138 (6) |
| Albumin mg/dL | 2.8 (1) | 2.8 (1.1) | 2.9 (1) |
| Child–Pugh–Turcotte | n | ||
| A/B/C | 12/78/10 | 4/40/6 | 8/38/4 |
| On hepatic encephalopathy (HE) treatment pre transjugular intrahepatic portosystemic shunt (TIPS) (lactulose +/- rifaximin) | 26 (26) | 15 (30) | 11 (22) |
| Age 50–59 | Age70–84 | |
|---|---|---|
| Indication N (%) | ||
| Ascites | 16 (32) | 26 (52) p = 0.07 |
| Variceal bleed | 28 (56) | 22 (44) p = 0.3 |
| Acute variceal bleed | 17 (34) | 16 (32) |
| Hepatic hydrothorax | 6 (12) | 2 (4) |
| Pre-TIPS gradient mmHg | 17 (7) | 16 (7) |
| Post-TIPS gradient mmHg | 5 (5) | 5 (3) |
| Age 50–59 | Age 70–84 | |
|---|---|---|
| 30 d mortality N (%) | 6 (12) | 12 (24) p = 0.19 |
| Length of stay (mean/median/IQR d) | 3/1/3 | 3/2/2 |
| Readmission N (%) | 6 (12) | 17 (34) p = 0.02 |
| Readmission for HE post TIPS N (%) | 5 (10) | 14 (28) p = 0.04 |
| On lactulose post TIPS N (%) | 43 (86) | 38 (76) |
| On rifaximin post TIPS N (%) | 18 (36) | 22 (44) |
| Age | MELD pre TIPS | Indication | Cause of Death | Days to Death |
|---|---|---|---|---|
| 50 | 27 | Acute variceal bleed | Multisystem organ failure (MOF), liver failure | 0 |
| 52 | 17 | Acute variceal bleed | MOF, liver failure | 1 |
| 53 | 14 | Acute variceal bleed | MOF, liver failure | 3 |
| 55 | 14 | Acute variceal bleed | MOF, liver failure | 8 |
| 58 | 12 | Acute variceal bleed | MOF, liver failure | 1 |
| 56 | 17 | Ascites | Sepsis, MOF, liver failure | 22 |
| 70 | 18 | Acute variceal bleed | Liver failure, hospice | 18 |
| 70 | 24 | Acute variceal bleed | MOF, liver failure | 1 |
| 71 | 11 | Ascites | HE, fell broke hip, home hospice | 25 |
| 72 | 27 | Acute variceal bleed | MOF, liver failure | 1 |
| 72 | 18 | Acute variceal bleed | In hospital | 3 |
| 74 | 10 | Acute variceal bleed | MOF, liver failure | 9 |
| 75 | 20 | Hepatic hydrothorax | MOF, liver failure | 9 |
| 77 | 11 | Ascites | MOF, liver failure | 15 |
| 79 | 18 | Acute variceal bleed | MOF, liver failure | 0 |
| 80 | 10 | Ascites | Home hospice, liver failure | 28 |
| 83 | 10 | Ascites | Unknown | 17 |
| 84 | 16 | Ascites | UTI, sepsis | 23 |
| Variable | OR (95% CI) |
|---|---|
| Age ≥ 70 years old | 5.3 (1.4–20.1) |
| Pre-TIPS encephalopathy | 1.4 (0.5–4.3) |
| Ascites as indication | 1.6 (0.3–10.5) |
| Variceal bleeding as indication | 1.2 (0.2–8.0) |
| Etiology: Alcohol | 1.4 (0.3–5.9) |
| NAFLD | 1.2 (0.4–4.2) |
| Viral hepatitis | 3.5 (0.7–17.1) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Adlakha, N.; Russo, M.W. Outcomes After Transjugular Intrahepatic Portosystemic Shunt in Cirrhotic Patients 70 Years and Older. J. Clin. Med. 2020, 9, 381. https://doi.org/10.3390/jcm9020381
Adlakha N, Russo MW. Outcomes After Transjugular Intrahepatic Portosystemic Shunt in Cirrhotic Patients 70 Years and Older. Journal of Clinical Medicine. 2020; 9(2):381. https://doi.org/10.3390/jcm9020381
Chicago/Turabian StyleAdlakha, Natasha, and Mark W. Russo. 2020. "Outcomes After Transjugular Intrahepatic Portosystemic Shunt in Cirrhotic Patients 70 Years and Older" Journal of Clinical Medicine 9, no. 2: 381. https://doi.org/10.3390/jcm9020381
APA StyleAdlakha, N., & Russo, M. W. (2020). Outcomes After Transjugular Intrahepatic Portosystemic Shunt in Cirrhotic Patients 70 Years and Older. Journal of Clinical Medicine, 9(2), 381. https://doi.org/10.3390/jcm9020381




