Endothelial Progenitor Cells as a Potential Biomarker in Interstitial Lung Disease Associated with Rheumatoid Arthritis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. EPC Quantification by Flow Cytometry
2.3. Statistical Analyses
3. Results
3.1. Demographic and Clinical Features of Patients and Controls
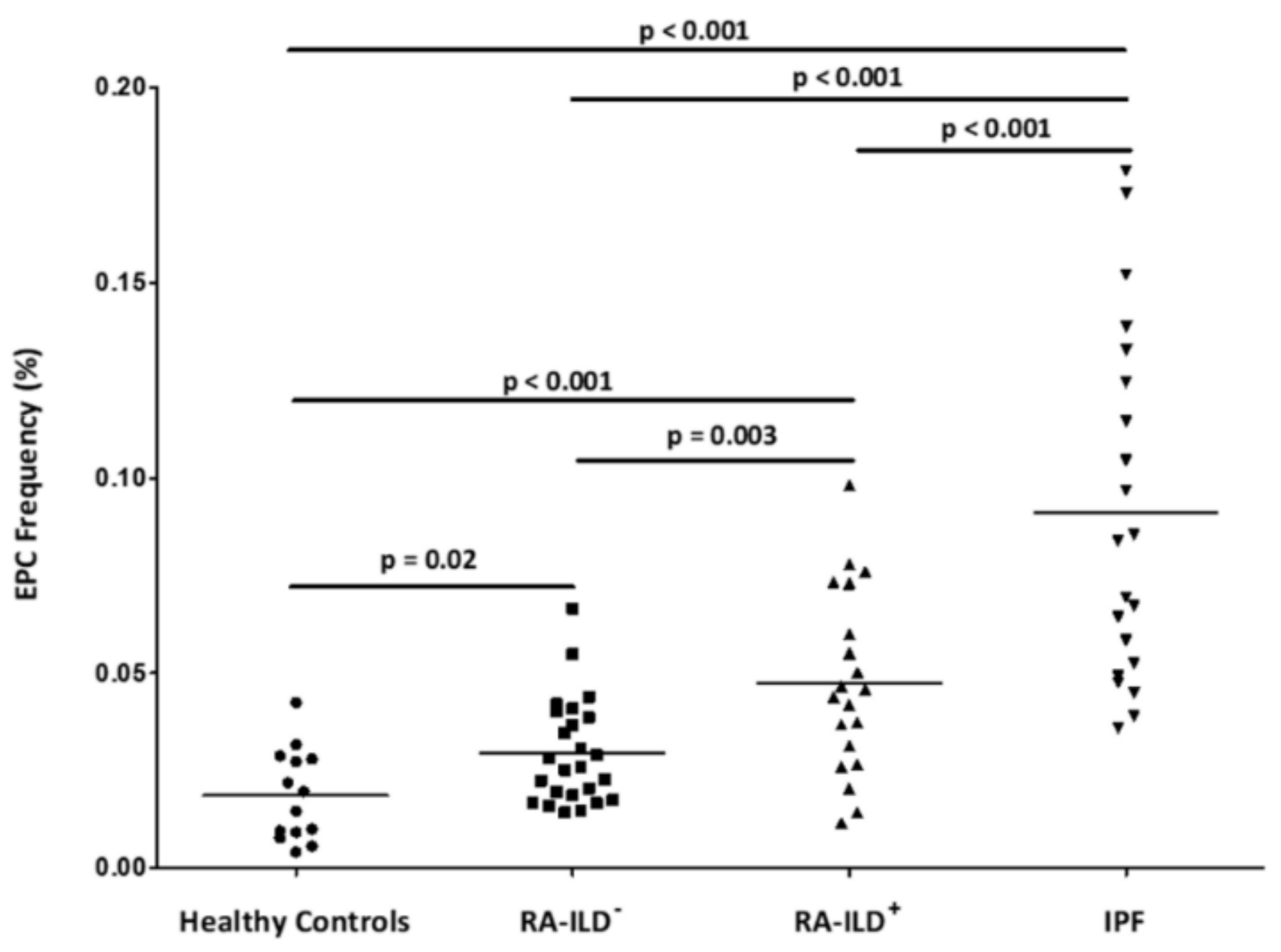
3.2. Differences of EPC Frequency between RA-ILD+ Patients and the Comparative Groups
3.3. Relationship of EPC Frequency with Clinical Features
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Bendstrup, E.; Moller, J.; Kronborg-white, S.; Prior, T.S.; Hyldgaard, C. Interstitial Lung Disease in Rheumatoid Arthritis Remains a Challenge for Clinicians. J. Clin. Med. 2019, 8, 2038. [Google Scholar] [CrossRef] [PubMed]
- Mathai, S.C.; Danoff, S.K. Management of interstitial lung disease associated with connective tissue disease. BMJ 2016, 352, h6819. [Google Scholar] [CrossRef] [PubMed]
- Paulin, F.; Doyle, T.J.; Fletcher, E.A.; Ascherman, D.P.; Rosas, I.O. Rheumatoid Arthritis-Associated Interstitial Lung Disease and Idiopathic Pulmonary Fibrosis: Shared Mechanistic and Phenotypic Traits Suggest Overlapping Disease Mechanisms. Rev. Investig. Clín. 2015, 67, 280–286. [Google Scholar]
- Atienza-Mateo, B.; Remuzgo-Martínez, S.; Mora-Cuesta, V.M.; Iturbe-Fernández, D.; Fernández-Rozas, S.; Prieto-Peña, D.; Calderón-Goercke, M.; Corrales, A.; Blanco-Rodriguez, G.; Gómez-Román, J.J.; et al. The Spectrum of Interstitial Lung Disease Associated with Autoimmune Diseases: Data of a 3.6-Year Prospective Study from a Referral Center of Interstitial Lung Disease and Lung Transplantation. J. Clin. Med. 2020, 9, 1606. [Google Scholar] [CrossRef]
- Alvarez, D.F.; Huang, L.; King, J.A.; Elzarrad, M.K.; Yoder, M.C.; Stevens, T. Lung microvascular endothelium is enriched with progenitor cells that exhibit vasculogenic capacity. Lung. Cell Mol. Physiol. 2008, 294, 419–430. [Google Scholar] [CrossRef] [PubMed]
- Asahara, T.; Murohara, T.; Sullivan, A.; Silver, M.; Van der Zee, R.; Li, T.; Witzenbichler, B.; Schatteman, G.; Isner, J.M. Isolation of Putative Progenitor Endothelial Cells for Angiogenesis. Sci. New Ser. 1997, 275, 964–967. [Google Scholar] [CrossRef] [PubMed]
- Jodon de Villeroché, V.; Avouac, J.; Ponceau, A.; Ruiz, B.; Kahan, A.; Boileau, C.; Uzan, G.; Allanore, Y. Enhanced late-outgrowth circulating endothelial progenitor cell levels in rheumatoid arthritis and correlation with disease activity. Arthritis Res. Ther. 2010, 12, R27. [Google Scholar] [CrossRef]
- Rodríguez-Carrio, J.; Prado, C.; De Paz, B.; López, P.; Gómez, J.; Alperi-López, M.; Ballina-García, F.J.; Suárez, A. Circulating endothelial cells and their progenitors in systemic lupus erythematosus and early rheumatoid arthritis patients. Rheumatology 2012, 51, 1775–1784. [Google Scholar] [CrossRef]
- Distler, H.W.; Beyer, C.; Schett, G.; Luscher, T.F.; Gay, S.; Distler, O. Endothelial Progenitor Cells Novel Players in the Pathogenesis of Rheumatic Diseases. Arthritis Rheum. 2009, 60, 3168–3179. [Google Scholar] [CrossRef]
- Avouac, J.; Uzan, G.; Kahan, A.; Boileau, C.; Allanore, Y. Endothelial progenitor cells and rheumatic disorders. Jt. Bone Spine 2008, 75, 131–137. [Google Scholar] [CrossRef]
- De Biasi, S.; Cerri, S.; Bianchini, E.; Gibellini, L.; Persiani, E.; Montanari, G.; Luppi, F.; Carbonelli, C.M.; Zucchi, L.; Bocchino, M.; et al. Levels of circulating endothelial cells are low in idiopathic pulmonary fibrosis and are further reduced by anti-fibrotic treatments. BMC Med. 2015, 13, 277. [Google Scholar] [CrossRef] [PubMed]
- Smadja, D.M.; Mauge, L.; Nunes, H.; D’Audigier, C.; Juvin, K.; Borie, R.; Carton, Z.; Bertil, S.; Blanchard, A.; Crestani, B.; et al. Imbalance of circulating endothelial cells and progenitors in idiopathic pulmonary fibrosis. Angiogenesis 2013, 16, 147–157. [Google Scholar] [CrossRef] [PubMed]
- Aletaha, D.; Neogi, T.; Silman, A.J.; Funovits, J.; Felson, D.T.; Bingham, C.O., 3rd; Birnbaum, N.S.; Burmester, G.R.; Bykerk, V.P.; Cohen, M.D.; et al. 2010 Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010, 62, 2569–2581. [Google Scholar] [CrossRef] [PubMed]
- Travis, W.D.; Costabel, U.; Hansell, D.M.; King, T.E.; Lynch, D.A.; Nicholson, A.G.; Ryerson, C.J.; Ryu, J.H.; Selman, M.; Wells, A.U.; et al. An official American Thoracic Society/European Respiratory Society statement: Update of the international multidisciplinary classification of the idiopathic interstitial pneumonias. Am. J. Respir. Crit. Care Med. 2013, 188, 733–748. [Google Scholar] [CrossRef] [PubMed]
- Lynch, D.A.; Sverzellati, N.; Travis, W.D.; Brown, K.K.; Colby, T.V.; Galvin, J.R.; Goldin, J.G.; Hansell, D.M.; Inoue, Y.; Johkoh, T.; et al. Diagnostic criteria for idiopathic pulmonary fibrosis: A Fleischner Society White Paper. Lancet Respir. Med. 2018, 6, 138–153. [Google Scholar] [CrossRef]
- Distler, J.H.W.; Allanore, Y.; Avouac, J.; Giacomelli, R.; Guiducci, S.; Moritz, F.; Akhmetshina, A.; Walker, U.A.; Gabrielli, A.; Müller-Ladner, U.; et al. EULAR Scleroderma Trials and Research group statement and recommendations on endothelial precursor cells EUSTAR statement and recommendations on endothelial precursor cells. Ann. Rheum. Dis. 2009, 68, 163–168. [Google Scholar] [CrossRef]
- Schmidt-Lucke, C.; Fichtlscherer, S.; Aicher, A.; Tschöpe, C.; Schultheiss, H.-P.; Zeiher, A.M.; Dimmeler, S. Quantification of Circulating Endothelial Progenitor Cells Using the Modified ISHAGE Protocol. PLoS ONE 2010, 5, e13790. [Google Scholar] [CrossRef]
- Van Craenenbroeck, E.M.; Van Craenenbroeck, A.H.; Van Ierssel, S.; Bruyndonckx, L.; Hoymans, V.Y.; Vrints, C.J.; Conraads, V.M. Quantification of circulating CD34 +/KDR +/CD45 dim endothelial progenitor cells: Analytical considerations. Int. J. Cardiol. 2013, 167, 1688–1695. [Google Scholar] [CrossRef]
- Aragona, C.O.; Imbalzano, E.; Mamone, F.; Cairo, V.; Gullo, A.L.; D’Ascola, A.; Sardo, M.A.; Scuruchi, M.; Basile, G.; Saitta, A.; et al. Endothelial Progenitor Cells for Diagnosis and Prognosis in Cardiovascular Disease. Stem Cells Int. 2016, 2016, 8043792. [Google Scholar] [CrossRef]
- Huertas, A.; Palange, P. Circulating endothelial progenitor cells and chronic pulmonary diseases. Eur. Respir. J. 2011, 37, 426–431. [Google Scholar] [CrossRef]
- Ghiadoni, L.; Mosca, M.; Tani, C.; Virdis, A.; Taddei, S.; Bombardieri, S. Clinical and methodological aspects of endothelial function in patients with systemic autoimmune diseases. Clin. Exp. Rheumatol. 2008, 26, 680. [Google Scholar] [PubMed]
- Heiss, C.; Keymel, S.; Niesler, U.; Ziemann, J.; Kelm, M.; Kalka, C. Impaired progenitor cell activity in age-related endothelial dysfunction. J. Am. Coll. Cardiol. 2005, 45, 1441–1448. [Google Scholar] [CrossRef] [PubMed]
| Healthy Controls n = 14 | RA-ILD+ Patients n = 20 | RA-ILD− Patients n = 25 | IPF Patients n = 21 | * p | |
|---|---|---|---|---|---|
| Sex (women), n (%) | 7 (50) | 9 (45.0) | 15 (60.0) | 7 (33.3) | 0.32 |
| Age at study, mean ± SD, years | 41.8 ± 13.7 | 66.8 ± 10.2 | 60.1 ± 11.8 | 69.2 ± 10.0 | 0.05 |
| Smoking ever, n (%) | 3 (27.3) | 13 (65.0) | 13 (52.0) | 16 (76.2) | 0.38 |
| Duration of RA disease, mean ± SD, years | − | 9.2 ± 10.2 | 4.1 ± 7.4 | − | 0.06 |
| RF positive, n (%) | − | 16 (80.0) | 11 (44.0) | − | 0.01 |
| ACPA positive, n (%) | − | 18 (90.0) | 15 (60.0) | − | 0.02 |
| CRP (mg/dL), mean ± SD | − | 1.1 ± 1.1 | 0.5 ± 0.5 | − | 0.04 |
| ESR (mm/1st hour), mean ± SD | − | 22.8 ± 27.2 | 14.4 ± 12.4 | − | 0.24 |
| Pulmonary function tests | |||||
| FVC (% predicted), mean ± SD | − | 95.1 ± 24.7 | 99.2 ± 16.0 | 84.9 ± 14.7 | 0.58 |
| FEV1 (% predicted), mean ± SD | − | 91.7 ± 21.5 | 94.9 ± 22.0 | 87.3 ± 19.6 | 0.67 |
| FEV1/FVC (% predicted), mean ± SD | − | 77.6 ± 9.3 | 93.6 ± 12.3 | 79.7 ± 7.8 | <0.001 |
| DLCO (% predicted), mean ± SD | − | 40.9 ± 13.9 | 79.9 ± 20.0 | 43.6 ± 18.4 | <0.001 |
| HRCT pattern | |||||
| UIP pattern, n (%) | − | 11 (55.0) | − | 21 (100.0) | − |
| Probable UIP pattern, n (%) | − | 1 (5.0) | − | − | − |
| NSIP pattern, n (%) | − | 7 (35.0) | − | − | − |
| Non-NSIP pattern, n (%) | − | 1 (5.0) | − | − | − |
| Therapies received by RA patients | |||||
| csDMARDs, n (%) | − | 17 (85) | 13 (52) | − | 0.02 |
| bDMARDs, n (%) | − | 15 (75) | 2 (8) | − | <0.001 |
| RA-ILD+ Patients | RA-ILD− Patients | IPF Patients | ||||
|---|---|---|---|---|---|---|
| r | p | r | p | r | p | |
| Duration of RA disease (years) | −0.19 | 0.42 | −0.04 | 0.87 | − | − |
| CRP (mg/dL) | −0.06 | 0.79 | −0.30 | 0.20 | − | − |
| ESR (mm/1st hour) | −0.34 | 0.10 | −0.06 | 0.82 | − | − |
| FVC (% predicted) | 0.07 | 0.76 | 0.26 | 0.34 | −0.21 | 0.35 |
| FEV1 (% predicted) | −0.07 | 0.77 | 0.29 | 0.29 | −0.19 | 0.40 |
| FEV1/FVC (% predicted) | −0.03 | 0.89 | 0.24 | 0.40 | −0.05 | 0.83 |
| DLCO (% predicted) | 0.38 | 0.22 | 0.07 | 0.81 | −0.23 | 0.40 |
| Variable | Category | RA-ILD+ Patients | RA-ILD− Patients | IPF Patients | |||
|---|---|---|---|---|---|---|---|
| Mean ± SD | p | Mean ± SD | p | Mean ± SD | p | ||
| Smoking ever | No | 0.059 ± 0.020 | 0.20 | 0.028 ± 0.010 | 0.53 | 0.092 ± 0.048 | 0.93 |
| Yes | 0.043 ± 0.024 | 0.031 ± 0.016 | 0.091 ± 0.045 | ||||
| RF | No | 0.061 ± 0.034 | 0.31 | 0.026 ± 0.009 | 0.18 | − | − |
| Yes | 0.047 ± 0.020 | 0.034 ± 0.017 | − | ||||
| ACPA | No | 0.046 | 0.88 | 0.026 ± 0.009 | 0.34 | − | − |
| Yes | 0.049 ± 0.023 | 0.031 ± 0.015 | − | ||||
| HRCT pattern | UIP | 0.043 ± 0.020 | 0.15 | − | − | 0.091 ± 0.045 | − |
| NSIP | 0.059 ± 0.025 | − | − | ||||
| csDMARDs | No | 0.036 ± 0.099 | 0.39 | 0.033 ± 0.016 | 0.25 | − | − |
| Yes | 0.049 ± 0.025 | 0.027 ± 0.011 | |||||
| bDMARDs | No | 0.047 ± 0.034 | 0.99 | 0.030 ± 0.014 | 0.31 | − | − |
| Yes | 0.047 ± 0.020 | 0.020 ± 0.004 | |||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pulito-Cueto, V.; Remuzgo-Martínez, S.; Genre, F.; Mora-Cuesta, V.M.; Iturbe-Fernández, D.; Fernández-Rozas, S.; Atienza-Mateo, B.; Lera-Gómez, L.; Alonso-Lecue, P.; Rodríguez-Carrio, J.; et al. Endothelial Progenitor Cells as a Potential Biomarker in Interstitial Lung Disease Associated with Rheumatoid Arthritis. J. Clin. Med. 2020, 9, 4098. https://doi.org/10.3390/jcm9124098
Pulito-Cueto V, Remuzgo-Martínez S, Genre F, Mora-Cuesta VM, Iturbe-Fernández D, Fernández-Rozas S, Atienza-Mateo B, Lera-Gómez L, Alonso-Lecue P, Rodríguez-Carrio J, et al. Endothelial Progenitor Cells as a Potential Biomarker in Interstitial Lung Disease Associated with Rheumatoid Arthritis. Journal of Clinical Medicine. 2020; 9(12):4098. https://doi.org/10.3390/jcm9124098
Chicago/Turabian StylePulito-Cueto, Verónica, Sara Remuzgo-Martínez, Fernanda Genre, Víctor M. Mora-Cuesta, David Iturbe-Fernández, Sonia Fernández-Rozas, Belén Atienza-Mateo, Leticia Lera-Gómez, Pilar Alonso-Lecue, Javier Rodríguez-Carrio, and et al. 2020. "Endothelial Progenitor Cells as a Potential Biomarker in Interstitial Lung Disease Associated with Rheumatoid Arthritis" Journal of Clinical Medicine 9, no. 12: 4098. https://doi.org/10.3390/jcm9124098
APA StylePulito-Cueto, V., Remuzgo-Martínez, S., Genre, F., Mora-Cuesta, V. M., Iturbe-Fernández, D., Fernández-Rozas, S., Atienza-Mateo, B., Lera-Gómez, L., Alonso-Lecue, P., Rodríguez-Carrio, J., Prieto-Peña, D., Portilla, V., Blanco, R., Corrales, A., Gualillo, O., Cifrián, J. M., López-Mejías, R., & González-Gay, M. A. (2020). Endothelial Progenitor Cells as a Potential Biomarker in Interstitial Lung Disease Associated with Rheumatoid Arthritis. Journal of Clinical Medicine, 9(12), 4098. https://doi.org/10.3390/jcm9124098








