Tissue Viability of Free Flaps after Extracorporeal Perfusion Using a Modified Hydroxyethyl Starch Solution
Abstract
1. Introduction
2. Methods
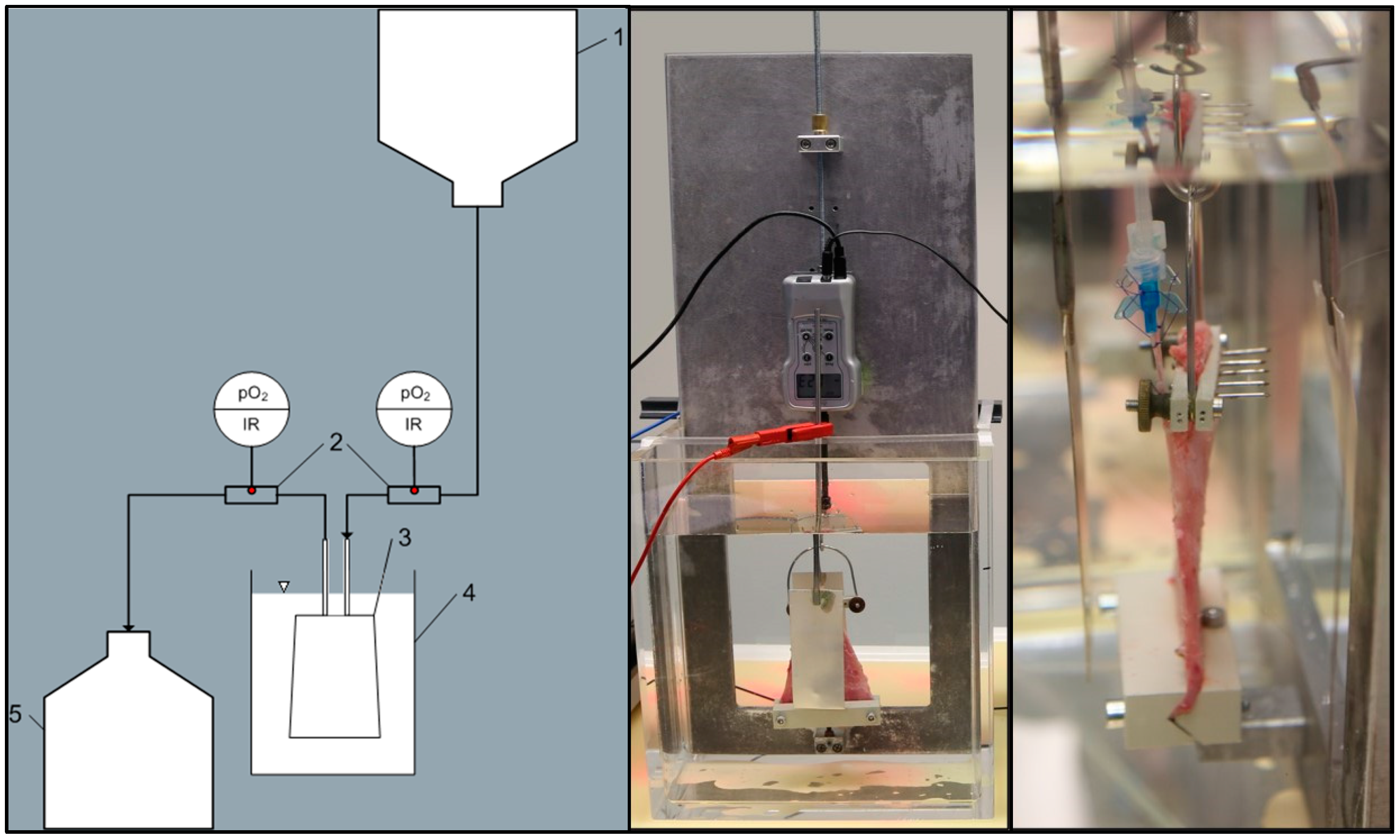
2.1. Animals, Surgical Protocol, and Experimental Setup
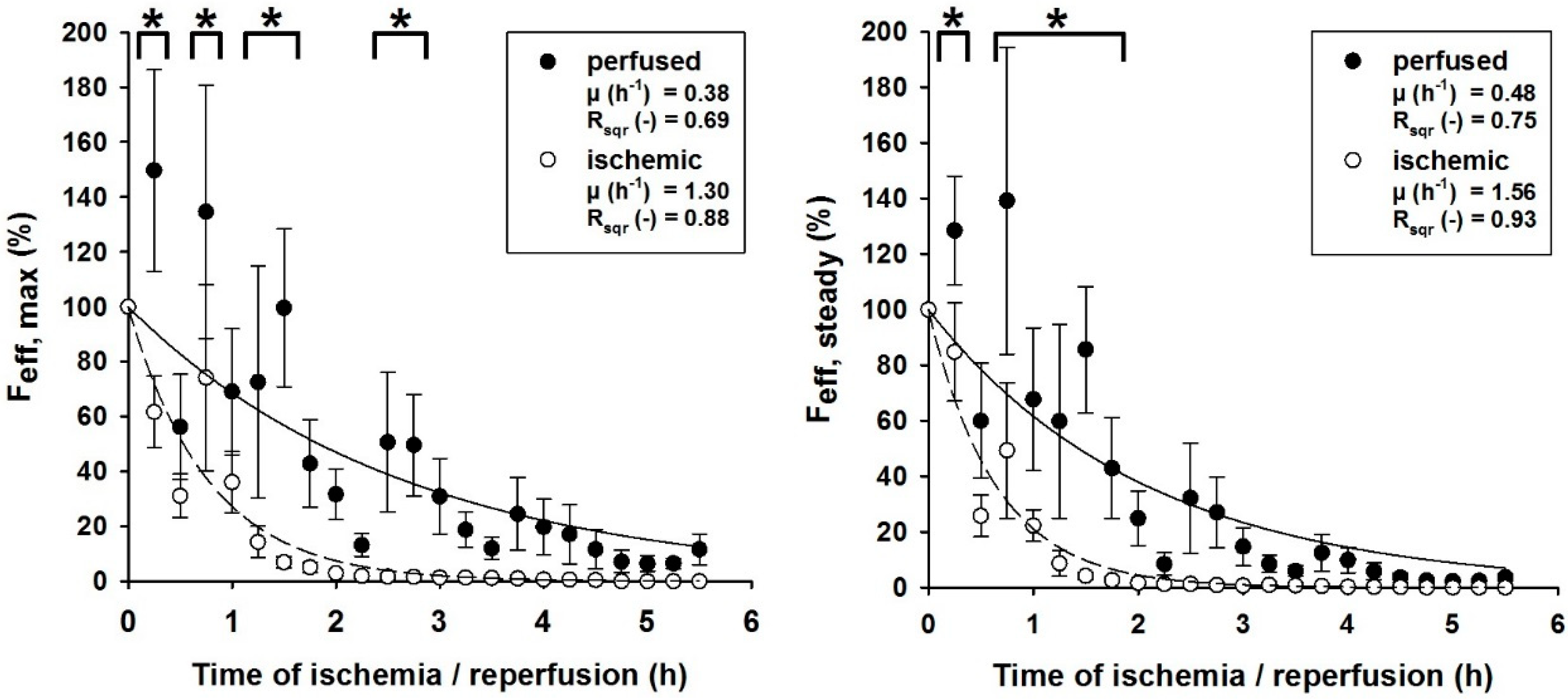
2.2. Extracorporeal Perfusion Parameters and Functionality Monitoring
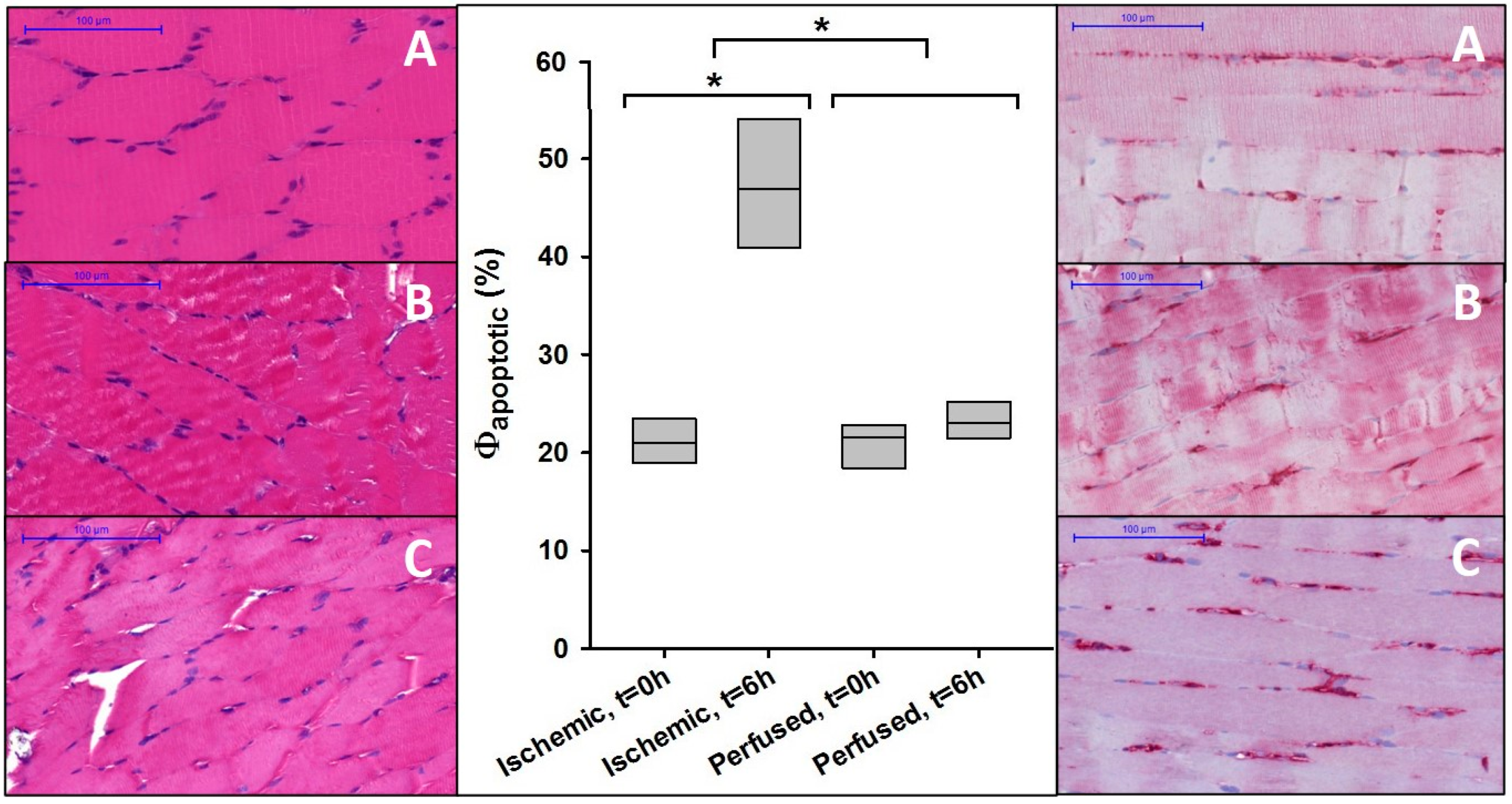
2.3. Histology and Immunohistochemistry
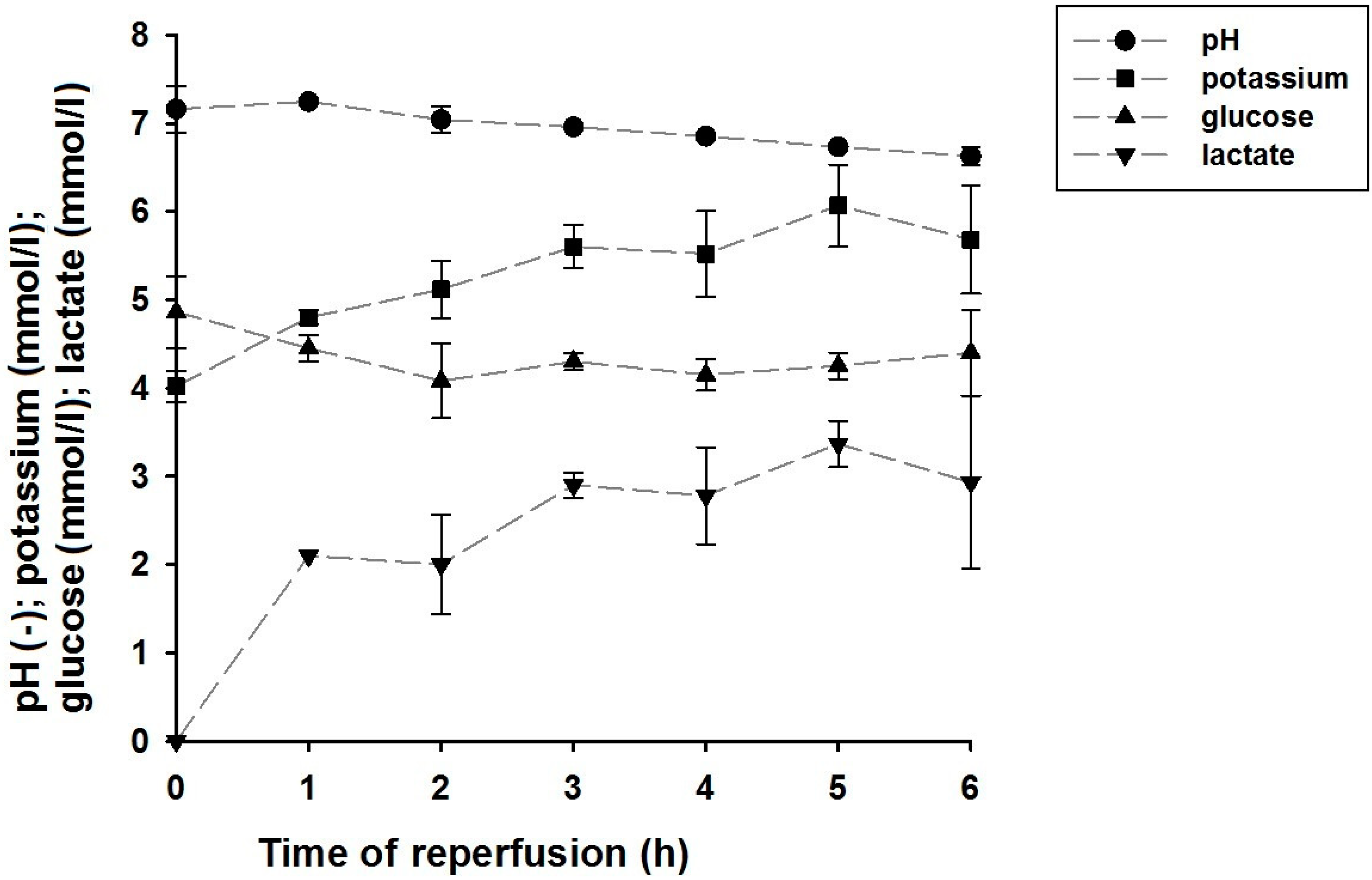
2.4. Perfusate Analysis
2.5. Statistical Analysis
3. Results
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Hao, Y.; Dong, X.; Liu, H.; Wang, Y. Preconditioning with one-time hydrogen gas does not attenuate skin flap ischemia-reperfusion injury in rat models. J. Plast. Reconstr. Aesthetic Surg. 2019, 72, 1661–1668. [Google Scholar] [CrossRef] [PubMed]
- Matsumoto, M.; Makino, Y.; Tanaka, T.; Tanaka, H.; Ishizaka, N.; Noiri, E.; Fujita, T.; Nangaku, M. Induction of renoprotective gene expression by cobalt ameliorates ischemic injury of the kidney in rats. J. Am. Soc. Nephrol. 2003, 14, 1825–1832. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Tuo, Z.; Zhang, J.; Guo, P.; Song, B. Hyperoxygenated solution improves tissue viability in an avulsion injury flap model. J. Plast. Reconstr. Aesthetic Surg. 2019. [Google Scholar] [CrossRef] [PubMed]
- Dengu, F.; Abbas, S.H.; Ebeling, G.; Nasralla, D. Normothermic Machine Perfusion (NMP) of the Liver as a Platform for Therapeutic Interventions during Ex-Vivo Liver Preservation: A Review. J. Clin. Med. 2020, 9, 1046. [Google Scholar] [CrossRef] [PubMed]
- Wagh, M.; Pantazi, G.; Romeo, R.; Hurley, J.V.; Morrison, W.A.; Knight, K.R. Cold storage of rat skeletal muscle free flaps and pre-ischemic perfusion with modified UW solution. Microsurgery 2000, 20, 343–349. [Google Scholar] [CrossRef]
- Blaisdell, F.W. The pathophysiology of skeletal muscle ischemia and the reperfusion syndrome: A review. Cardiovasc. Surg. 2002, 10, 620–630. [Google Scholar] [CrossRef]
- Lloyd, M.S.; Teo, T.C.; Pickford, M.A.; Arnstein, P.M. Preoperative management of the amputated limb. Emerg. Med. J. 2005, 22, 478–480. [Google Scholar] [CrossRef][Green Version]
- Woo, M.; Hakem, R.; Soengas, M.S.; Duncan, G.S.; Shahinian, A.; Kagi, D.; Hakem, A.; McCurrach, M.; Khoo, W.; Kaufman, S.A.; et al. Essential contribution of caspase 3/CPP32 to apoptosis and its associated nuclear changes. Genes Dev. 1998, 12, 806–819. [Google Scholar] [CrossRef]
- Hickey, M.J.; Knight, K.R.; Hurley, J.V.; Lepore, D.A. Phosphoenolpyruvate/adenosine triphosphate enhances post-ischemic survival of skeletal muscle. J. Reconstr. Microsurg. 1995, 11, 415–422. [Google Scholar] [CrossRef]
- Suzuki, H.; Poole, D.C.; Zweifach, B.W.; Schmid-Schonbein, G.W. Temporal correlation between maximum tetanic force and cell death in postischemic rat skeletal muscle. J. Clin. Investig. 1995, 96, 2892–2897. [Google Scholar] [CrossRef]
- Czigany, Z.; Lurje, I.; Schmelzle, M.; Schoning, W.; Ollinger, R.; Raschzok, N.; Sauer, I.M.; Tacke, F.; Strnad, P.; Trautwein, C.; et al. Ischemia-Reperfusion Injury in Marginal Liver Grafts and the Role of Hypothermic Machine Perfusion: Molecular Mechanisms and Clinical Implications. J. Clin. Med. 2020, 9, 846. [Google Scholar] [CrossRef] [PubMed]
- Dragu, A.; Birkholz, T.; Kleinmann, J.A.; Schnurer, S.; Munch, F.; Cesnjevar, R.; Schmidt, J.; Taeger, C.; Kneser, U.; Horch, R.E. Extracorporeal perfusion of free muscle flaps in a porcine model using a miniaturized perfusion system. Arch. Orthop. Trauma Surg. 2011, 131, 849–855. [Google Scholar] [CrossRef] [PubMed]
- Dragu, A.; Kleinmann, J.A.; Taeger, C.D.; Birkholz, T.; Schmidt, J.; Geppert, C.I.; Prabst, K.; Unglaub, F.; Munch, F.; Weyand, M.; et al. Immunohistochemical evaluation after ex vivo perfusion of rectus abdominis muscle flaps in a porcine model. Plast. Reconstr. Surg. 2012, 130, 265e–273e. [Google Scholar] [CrossRef] [PubMed]
- Dragu, A.; Taeger, C.D.; Buchholz, R.; Sommerfeld, B.; Hubner, H.; Birkholz, T.; Kleinmann, J.A.; Munch, F.; Horch, R.E.; Prabst, K. Online oxygen measurements in ex vivo perfused muscle tissue in a porcine model using dynamic quenching methods. Arch. Orthop. Trauma Surg. 2012, 132, 655–661. [Google Scholar] [CrossRef]
- Fichter, A.M.; Ritschl, L.M.; Borgmann, A.; Humbs, M.; Luppa, P.B.; Wolff, K.D.; Mucke, T. Development of an Extracorporeal Perfusion Device for Small Animal Free Flaps. PLoS ONE 2016, 11, e0147755. [Google Scholar] [CrossRef]
- Krezdorn, N.; Macleod, F.; Tasigiorgos, S.; Turk, M.; Wo, L.; Kiwanuka, H.; Lopdrup, B.I.D.R.; Kollar, B.; Edelman, E.R.; Pomahac, B. Twenty-Four-Hour Ex Vivo Perfusion with Acellular Solution Enables Successful Replantation of Porcine Forelimbs. Plast. Reconstr. Surg. 2019, 144, 608e–618e. [Google Scholar] [CrossRef]
- Kueckelhaus, M.; Dermietzel, A.; Alhefzi, M.; Aycart, M.A.; Fischer, S.; Krezdorn, N.; Wo, L.; Maarouf, O.H.; Riella, L.V.; Abdi, R.; et al. Acellular Hypothermic Extracorporeal Perfusion Extends Allowable Ischemia Time in a Porcine Whole Limb Replantation Model. Plast. Reconstr. Surg. 2017, 139, 922e–932e. [Google Scholar] [CrossRef]
- Kueckelhaus, M.; Fischer, S.; Sisk, G.; Kiwanuka, H.; Bueno, E.M.; Dermietzel, A.; Alhefzi, M.; Aycart, M.; Diehm, Y.; Pomahac, B. A Mobile Extracorporeal Extremity Salvage System for Replantation and Transplantation. Ann. Plast. Surg. 2016, 76, 355–360. [Google Scholar] [CrossRef]
- Kueckelhaus, M.; Puscz, F.; Dermietzel, A.; Dadras, M.; Fischer, S.; Krezdorn, N.; Pomahac, B.; Hirsch, T. Extracorporeal Perfusion in Vascularized Composite Allotransplantation: Current Concepts and Future Prospects. Ann. Plast. Surg. 2018, 80, 669–678. [Google Scholar] [CrossRef]
- Muller, S.; Constantinescu, M.A.; Kiermeir, D.M.; Gajanayake, T.; Bongoni, A.K.; Vollbach, F.H.; Meoli, M.; Plock, J.; Jenni, H.; Banic, A.; et al. Ischemia/reperfusion injury of porcine limbs after extracorporeal perfusion. J. Surg. Res. 2013, 181, 170–182. [Google Scholar] [CrossRef]
- Norden, M.A.; Rao, V.K.; Southard, J.H. Improved preservation of rat hindlimbs with the University of Wisconsin solution and butanedione monoxime. Plast. Reconstr. Surg. 1997, 100, 957–965. [Google Scholar] [CrossRef] [PubMed]
- Taeger, C.D.; Friedrich, O.; Dragu, A.; Weigand, A.; Hobe, F.; Drechsler, C.; Geppert, C.I.; Arkudas, A.; Munch, F.; Buchholz, R.; et al. Assessing viability of extracorporeal preserved muscle transplants using external field stimulation: A novel tool to improve methods prolonging bridge-to-transplantation time. Sci. Rep. 2015, 5, 11956. [Google Scholar] [CrossRef] [PubMed]
- Taeger, C.D.; Friedrich, O.; Drechsler, C.; Weigand, A.; Hobe, F.; Geppert, C.I.; Munch, F.; Birkholz, T.; Buchholz, R.; Horch, R.E.; et al. Hydroxyethyl starch solution for extracorporeal tissue perfusion. Clin. Hemorheol. Microcirc. 2016, 64, 91–103. [Google Scholar] [CrossRef] [PubMed]
- Taeger, C.D.; Friedrich, O.; Horch, R.E.; Drechsler, C.; Weigand, A.; Hopf, F.; Geppert, C.I.; Munch, F.; Birkholz, T.; Wenzel, C.; et al. Extracorporeal perfusion—Reduced to a one-way infusion. Clin. Hemorheol. Microcirc. 2017. [Google Scholar] [CrossRef] [PubMed]
- Taeger, C.D.; Lamby, P.; Dolderer, J.; Philipp, A.; Kehrer, A.; Horch, R.E.; Prabst, K.; Prantl, L. Extracorporeal Perfusion for Salvage of Major Amputates. Ann. Surg. 2019, 270, e5–e6. [Google Scholar] [CrossRef] [PubMed]
- Taeger, C.D.; Muller-Seubert, W.; Horch, R.E.; Prabst, K.; Munch, F.; Geppert, C.I.; Birkholz, T.; Dragu, A. Ischaemia-related cell damage in extracorporeal preserved tissue—New findings with a novel perfusion model. J. Cell. Mol. Med. 2014, 18, 885–894. [Google Scholar] [CrossRef]
- Taeger, C.D.; Prabst, K.; Beier, J.P.; Meyer, A.; Horch, R.E. Extracorporeal Free Flap Perfusion in Case of Prolonged Ischemia Time. Plast. Reconstr. Surg. Glob. Open 2016, 4, e682. [Google Scholar] [CrossRef]
- Slater, N.J.; Zegers, H.J.H.; Kusters, B.; Beune, T.; van Swieten, H.A.; Ulrich, D.J.O. Ex-vivo oxygenated perfusion of free flaps during ischemia time: A feasibility study in a porcine model and preliminary results. J. Surg. Res. 2016, 205, 292–295. [Google Scholar] [CrossRef]
- Allen, D.G.; Lamb, G.D.; Westerblad, H. Skeletal muscle fatigue: Cellular mechanisms. Physiol. Rev. 2008, 88, 287–332. [Google Scholar] [CrossRef]
- Wolff, K.D.; Mucke, T.; von Bomhard, A.; Ritschl, L.M.; Schneider, J.; Humbs, M.; Fichter, A.M. Free flap transplantation using an extracorporeal perfusion device: First three cases. J. Cranio Maxillofac. Surg. 2016, 44, 148–154. [Google Scholar] [CrossRef]
- Karle, W.E.; Anand, S.M.; Clain, J.B.; Scherl, S.; Buchbinder, D.; Smith, M.L.; Urken, M.L. Use of a combined latissimus dorsi scapular free flap revascularized with vein grafting to the internal mammary artery in a vessel-depleted and previously irradiated neck. Head Neck 2013, 35, E328–E332. [Google Scholar] [CrossRef] [PubMed]
- Meyer, A.; Goller, K.; Horch, R.E.; Beier, J.P.; Taeger, C.D.; Arkudas, A.; Lang, W. Results of combined vascular reconstruction and free flap transfer for limb salvage in patients with critical limb ischemia. J. Vasc. Surg. 2015, 61, 1239–1248. [Google Scholar] [CrossRef] [PubMed]
- Meyer, A.; Horch, R.E.; Schoengart, E.; Beier, J.P.; Taeger, C.D.; Arkudas, A.; Lang, W. Results of combined vascular reconstruction by means of AV loops and free flap transfer in patients with soft tissue defects. J. Plast. Reconstr. Aesthetic Surg. 2016, 69, 545–553. [Google Scholar] [CrossRef] [PubMed]
- Taeger, C.D.; Arkudas, A.; Beier, J.P.; Horch, R.E. Emergency arterio-venous loop for free-flap defect reconstruction of the lower thigh with a post-irradiated and heavily infected wound. Int. Wound J. 2015, 12, 598–600. [Google Scholar] [CrossRef] [PubMed]
- Constantinescu, M.A.; Knall, E.; Xu, X.; Kiermeir, D.M.; Jenni, H.; Gygax, E.; Rieben, R.; Banic, A.; Vogelin, E. Preservation of amputated extremities by extracorporeal blood perfusion; a feasibility study in a porcine model. J. Surg. Res. 2011, 171, 291–299. [Google Scholar] [CrossRef]
- O’Donovan, M.J.; Rowlerson, A.; Taylor, A. Proceedings: The perfused isolated human limb: An assessment of its viability. J. Physiol. 1976, 256, 27P–28P. [Google Scholar]

| Component | Concentration |
|---|---|
| Na+ | 137.0 mmol/L |
| K+ | 4.0 mmol/L |
| Ca++ | 2.3 mmol/L |
| Mg++ | 1.5 mmol/L |
| CH3COO- | 34.0 mmol/L |
| Cl− | 110.0 mmol/L |
| C6H12O6 | 5 mmol/L |
| HES | 0.5 mmol/L |
| Heparin | 5000 IU/L |
| pH | 7.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Taeger, C.D.; Friedrich, O.; Horch, R.E.; Distler, C.; Kengelbach-Weigand, A.; Wenzel, C.; Prantl, L.; Präbst, K. Tissue Viability of Free Flaps after Extracorporeal Perfusion Using a Modified Hydroxyethyl Starch Solution. J. Clin. Med. 2020, 9, 3929. https://doi.org/10.3390/jcm9123929
Taeger CD, Friedrich O, Horch RE, Distler C, Kengelbach-Weigand A, Wenzel C, Prantl L, Präbst K. Tissue Viability of Free Flaps after Extracorporeal Perfusion Using a Modified Hydroxyethyl Starch Solution. Journal of Clinical Medicine. 2020; 9(12):3929. https://doi.org/10.3390/jcm9123929
Chicago/Turabian StyleTaeger, Christian D., Oliver Friedrich, Raymund E. Horch, Caroline Distler, Annika Kengelbach-Weigand, Carina Wenzel, Lukas Prantl, and Konstantin Präbst. 2020. "Tissue Viability of Free Flaps after Extracorporeal Perfusion Using a Modified Hydroxyethyl Starch Solution" Journal of Clinical Medicine 9, no. 12: 3929. https://doi.org/10.3390/jcm9123929
APA StyleTaeger, C. D., Friedrich, O., Horch, R. E., Distler, C., Kengelbach-Weigand, A., Wenzel, C., Prantl, L., & Präbst, K. (2020). Tissue Viability of Free Flaps after Extracorporeal Perfusion Using a Modified Hydroxyethyl Starch Solution. Journal of Clinical Medicine, 9(12), 3929. https://doi.org/10.3390/jcm9123929







