First Report of Sublingual Gland Ducts: Visualization by Dynamic MR Sialography and Its Clinical Application
Abstract
1. Introduction
2. Materials and Methods
3. Results
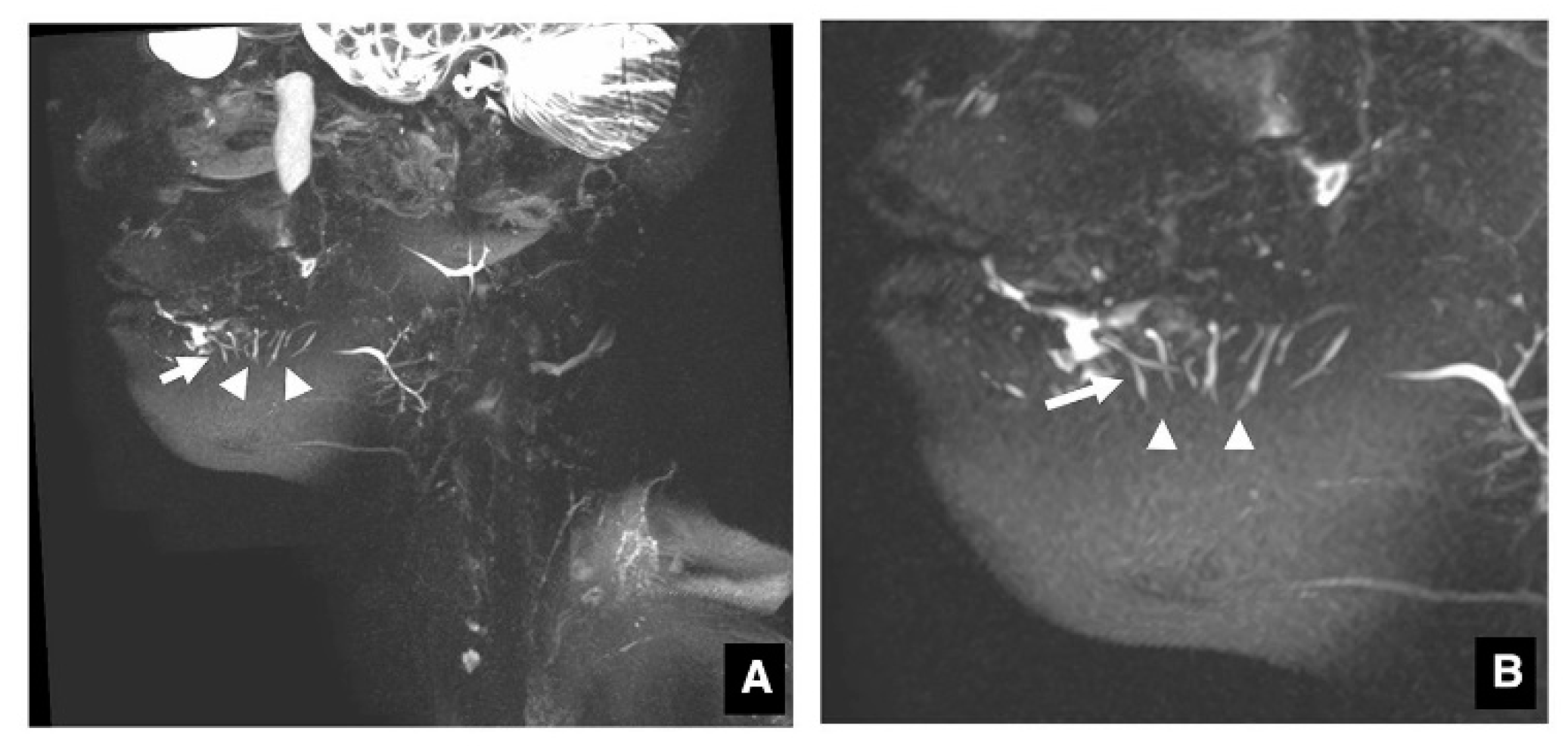
3.1. Visualization of Sublingual Gland Ducts by MR Sialography
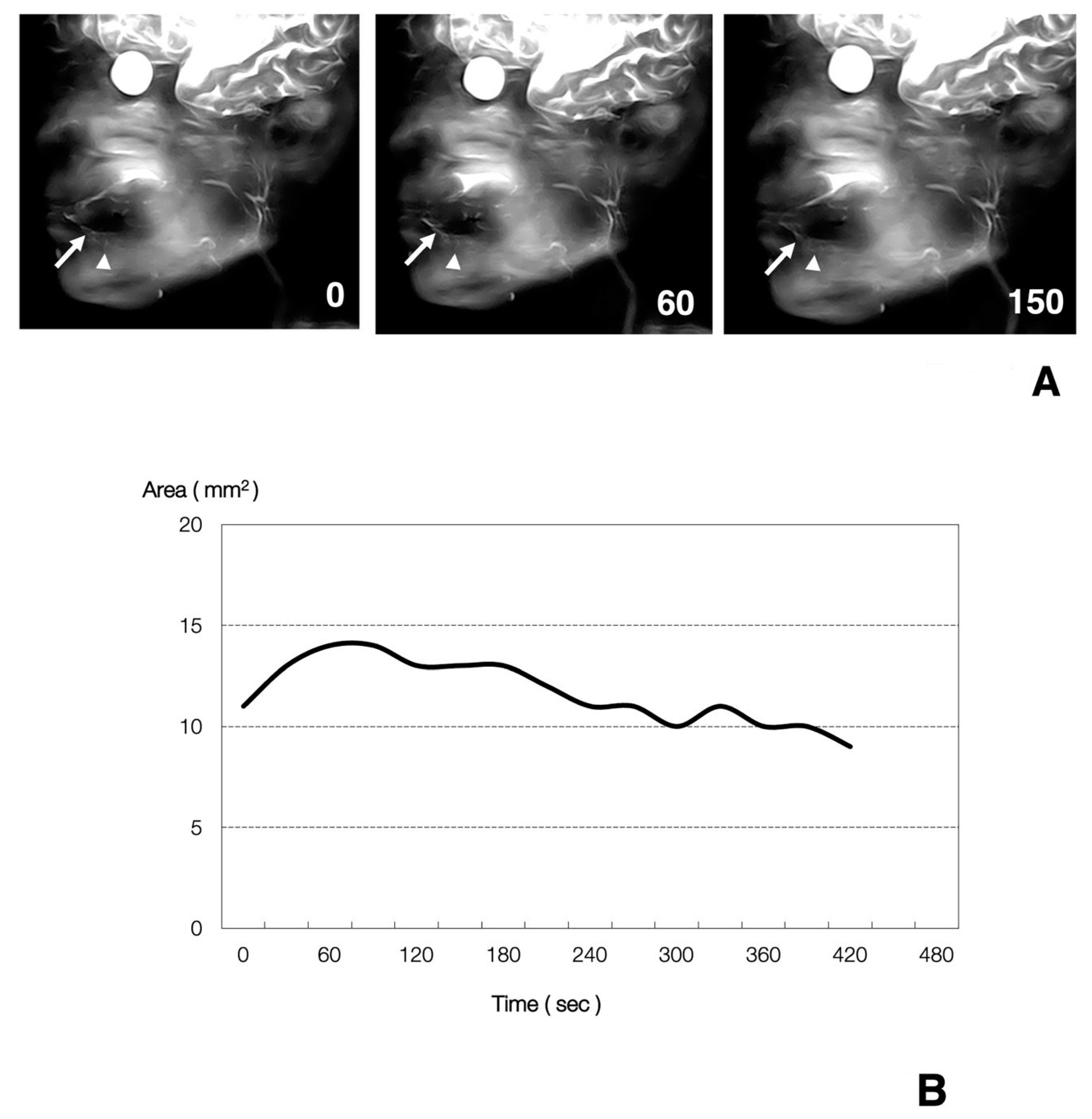
3.2. Function of Sublingual Gland Ducts Evaluated by Dynamic MR Sialography
3.3. Clinical Application of MR Sialography for Patients with Sublingual Gland Diseases
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Morimoto, Y.; Ono, K.; Tanaka, T.; Kito, S.; Inoue, H.; Seta, Y.; Yokota, M.; Inenaga, K.; Ohba, T. The functional evaluation of salivary glands using dynamic MR sialography following citric acid stimulation: A preliminary study. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2005, 100, 357–364. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, Y.; Tanaka, T.; Kito, S.; Tominaga, K.; Yoshioka, I.; Yamashita, Y.; Shibuya, T.; Matsufuji, Y.; Kodama, M.; Takahashi, T.; et al. Utility of three dimension fast asymmetric spin-echo (3D-FASE) sequences in MR sialographic sequences: Model and volunteer studies. Oral Dis. 2005, 11, 35–43. [Google Scholar] [CrossRef] [PubMed]
- Dirix, P.; De Keyzer, F.; Vandecaveye, V.; Stroobants, S.; Hermans, R.; Nuyts, S. Diffusion-weighted magnetic resonance imaging to evaluate major salivary gland function before and after radiotherapy. Int. J. Radiat. Oncol. Biol. Phys. 2008, 71, 1365–1371. [Google Scholar] [CrossRef]
- Wada, A.; Uchida, N.; Yokokawa, M.; Yoshizako, T.; Kitagaki, H. Radiation-induced xerostomia: Objective evaluation of salivary gland injury using MR sialography. AJNR Am. J. Neuroradiol. 2009, 30, 53–58. [Google Scholar] [CrossRef] [PubMed]
- Becker, M.; Marchal, F.; Becker, C.D.; Dulguerov, P.; Georgakopoulos, G.; Lehmann, W.; Terrier, F. Sialolithiasis and salivary ductal stenosis: Diagnostic accuracy of MR sialography with a three-dimensional extended-phase conjugate-symmetry rapid spin-echo sequence. Radiology 2000, 217, 347–358. [Google Scholar] [CrossRef]
- Murakami, R.; Baba, Y.; Nishimura, R.; Baba, T.; Matsumoto, N.; Yamashita, Y.; Ishikawa, T.; Takahashi, M. MR sialography using half-Fourier acquisition single-shot turbo spin-echo (HASTE) sequences. Am. J. Neuroradiol. 1998, 19, 959–961. [Google Scholar]
- Gadodia, A.; Seith, A.; Sharma, R.; Thakar, A.; Parshad, R. Magnetic resonance sialography using CISS and HASTE sequences in inflammatory salivary gland diseases: Comparison with digital sialography. Acta Radiol. 2010, 51, 156–163. [Google Scholar] [CrossRef]
- Ohbayashi, N.; Yamada, I.; Yoshino, N.; Sasaki, T. Sjögren syndrome: Comparison of assessments with MR sialography and conventional sialography. Radiology 1998, 209, 683–688. [Google Scholar] [CrossRef]
- Morimoto, Y.; Habu, M.; Tomoyose, T.; Ono, K.; Tanaka, T.; Yoshioka, I.; Tominaga, K.; Yamashita, Y.; Ansai, T.; Kito, S.; et al. Dynamic MR sialography as a new diagnostic technique for patients with Sjögren syndrome. Oral Dis. 2006, 12, 408–414. [Google Scholar] [CrossRef]
- Tanaka, T.; Ono, K.; Ansai, T.; Yoshioka, I.; Habu, M.; Tomoyose, T.; Yamashita, Y.; Nishida, I.; Oda, M.; Kuroiwa, H.; et al. Dynamic magnetic resonance sialography for patients with xerostomia. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2008, 106, 115–123. [Google Scholar] [CrossRef]
- Habu, M.; Tanaka, T.; Tomoyose, T.; Ono, K.; Ansai, T.; Ozaki, Y.; Yoshioka, I.; Yamashita, Y.; Kodama, M.; Yamamoto, N.; et al. Significance of dynamic magnetic resonance sialography in prognostic evaluation of saline solution irrigation of the parotid gland for the treatment of xerostomia. J. Oral Maxillofac. Surg. 2010, 68, 768–776. [Google Scholar] [CrossRef]
- Tanaka, T.; Ono, K.; Habu, M.; Inoue, H.; Tominaga, K.; Okabe, S.; Kito, S.; Yokota, M.; Fukuda, J.; Inenaga, K.; et al. Functional evaluations of the parotid and submandibular glands using dynamic magnetic resonance sialography. Dentomaxillofac. Radiol. 2007, 36, 218–223. [Google Scholar] [CrossRef] [PubMed]
- Harold, E. Clinical Anatomy, 11th ed.; Blackwell Publishing: Hoboken, NJ, USA, 2018; pp. 272–274. [Google Scholar]
- Oda, M.; Tanaka, T.; Habu, M.; Ono, K.; Kodama, M.; Kokuryo, S.; Yamamoto, N.; Kito, S.; Wakasugi-Sato, N.; Matsumoto-Takeda, S.; et al. Diagnosis and prognostic evaluation for xerostomia using dynamic MR sialography. Curr. Med. Imaging Rev. 2014, 10, 84–94. [Google Scholar] [CrossRef]
- Morimoto, Y.; Tanaka, T.; Yoshioka, I.; Masumi, S.; Yamashita, M.; Ohba, T. Virtual endoscopic view of salivary gland ducts using MR sialography data from three dimension fast asymmetric spin-echo (3D-FASE) sequences: A preliminary study. Oral Dis. 2002, 8, 268–274. [Google Scholar] [CrossRef] [PubMed]
- Morimoto, Y.; Tanaka, T.; Tominaga, K.; Yoshioka, I.; Kito, S.; Ohba, T. Clinical application of MR sialographic 3D-reconstruction imaging and MR virtual endoscopy for salivary gland duct analysis. J. Oral Maxillofac. Surg. 2004, 62, 1236–1244. [Google Scholar] [CrossRef]
- Yang, D.; Kodama, T.; Tamura, S.; Watanabe, K. Evaluation of inner ear by 3D fast asymmetric spin echo (FASE) MR imaging: Phantom and volunteer studies. Magn. Reson. Imaging 1999, 17, 171–182. [Google Scholar] [CrossRef]
- Markopoulos, A.K. A Handbook of Oral Physiology and Oral Biology; Bentham Science Publishers: Sharjah, UAE, 2010; pp. 44–50. [Google Scholar]
- Moore, K.L. Essential Clinical Anatomy; Lippincott Williams and Wilkins Publishers: Philadelphia, PA, USA, 2010; pp. 560–570. [Google Scholar]
- Carbognin, G.; Girardi, V.; Biasiutti, C.; Manfredi, R.; Frulloni, R.L.; Hermans, J.J.; Mucelli, R.P. Autoimmune pancreatitis: Imaging findings on contrast-enhanced MR, MRCP and dynamic secretin-enhanced MRCP. Radiol. Med. 2009, 114, 1214–1231. [Google Scholar] [CrossRef]
- Park, H.S.; Lee, J.M.; Choi, H.K.; Hong, S.H.; Han, J.K.; Choi, B.I. Preoperative evaluation of pancreatic cancer: Comparison of gadolinium-enhanced dynamic MRI with MR cholangiopancreatography versus MDCT. J. Magn. Reson. Imaging 2009, 30, 586–595. [Google Scholar] [CrossRef]
- Schlaudraff, E.; Wagner, H.J.; Klose, K.J.; Heverhagen, J.T. Prospective evaluation of the diagnostic accuracy of secretin-enhanced magnetic resonance cholangiopancreaticography in suspected chronic pancreatitis. Magn. Reson. Imaging 2008, 26, 1367–1373. [Google Scholar] [CrossRef]
- Akisik, M.F.; Sandrasegaran, K.; Aisen, A.A.; Maglinte, D.D.; Sherman, S.; Lehman, G.A. Dynamic secretin-enhanced MR cholangiopancreatography. Radiographics 2006, 26, 665–677. [Google Scholar] [CrossRef][Green Version]
- Gillams, A.R.; Kurzawinski, T.; Lees, W.R. Diagnosis of duct disruption and assessment of pancreatic leak with dynamic secretin-stimulated MR cholangiopancreatography. Am. J. Roentgenol. 2006, 186, 499–506. [Google Scholar] [CrossRef] [PubMed]


| Male | Female | |||||
|---|---|---|---|---|---|---|
| Number | Age (Mean ± SD) | Age Range | Number | Age (Mean ± SD) | Age Range | |
| Adult volunteers | 9 | 46.5 ± 8.7 | 29–55 | 11 | 40.3 ± 12.9 | 18–56 |
| Elderly volunteers | 8 | 68.1 ± 5.5 | 61–79 | 11 | 67. 5 ± 6.5 | 60–80 |
| Patients | 3 | 37.3 ± 15.4 | 27–55 | 4 | 48.0 ± 24.3 | 19–76 |
| Sequence | ||||
|---|---|---|---|---|
| STIR | T1WI | 2D-FASE | 3D-FASE | |
| TR (ms) | 4700 | 820 | 6000 | 3.2 |
| TE (ms) | 75 | 15 | 250 | 1.6 |
| Flip angle (°) | 90 | 90 | 90 | 45 |
| FOV (mm) | 200 × 200 | 200 × 200 | 200 × 200 | 200 × 200 |
| Section thickness (mm) | 6 | 6 | 30–60 | 1.8 |
| Matrix (pixels) | 224 × 320 | 224 × 320 | 224 × 320 | 120 × 96 |
| Acquisition time (min: s) | 3:30 | 3:30 | 0:18 (12hase) | 4:30–5:30 |
| Sublingual Glands and Ducts Visualized | Only Sublingual Glands Visualized | |
|---|---|---|
| Adult volunteers (n = 20) | 16 | 2 |
| Elderly volunteers (n = 19) | 12 | 4 |
| Patients (n = 7) | 5 | 1 |
| Area (mm2) | Period to Occurrence of Maximum Area (s) | Period to Return to Its Pre-Citric Acid Stimulation 50% Level (s) | |||
|---|---|---|---|---|---|
| Before Citric Acid Stimulation | After Citric Acid Stimulation | Change Ratio | |||
| Adult volunteers (n = 16) | 10.0 ± 4.6 | 13.2 ± 5.3 | 1.3 ± 1.1 | 62 ± 28 | 110 ± 39 |
| Elderly volunteers (n = 12) | 9.0 ± 3.4 | 10.7 ± 4.4 | 1.2 ± 1.3 | 63 ± 26 | 117 ± 57 |
| Patients (n = 5) | 10.2 ± 5.5 | 11.0 ± 5.4 | 1.1 ± 1.0 | 54 ± 13 | 114 ± 25 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tanaka, T.; Oda, M.; Wakasugi-Sato, N.; Joujima, T.; Miyamura, Y.; Habu, M.; Kodama, M.; Takahashi, O.; Sago, T.; Matsumoto-Takeda, S.; et al. First Report of Sublingual Gland Ducts: Visualization by Dynamic MR Sialography and Its Clinical Application. J. Clin. Med. 2020, 9, 3676. https://doi.org/10.3390/jcm9113676
Tanaka T, Oda M, Wakasugi-Sato N, Joujima T, Miyamura Y, Habu M, Kodama M, Takahashi O, Sago T, Matsumoto-Takeda S, et al. First Report of Sublingual Gland Ducts: Visualization by Dynamic MR Sialography and Its Clinical Application. Journal of Clinical Medicine. 2020; 9(11):3676. https://doi.org/10.3390/jcm9113676
Chicago/Turabian StyleTanaka, Tatsurou, Masafumi Oda, Nao Wakasugi-Sato, Takaaki Joujima, Yuichi Miyamura, Manabu Habu, Masaaki Kodama, Osamu Takahashi, Teppei Sago, Shinobu Matsumoto-Takeda, and et al. 2020. "First Report of Sublingual Gland Ducts: Visualization by Dynamic MR Sialography and Its Clinical Application" Journal of Clinical Medicine 9, no. 11: 3676. https://doi.org/10.3390/jcm9113676
APA StyleTanaka, T., Oda, M., Wakasugi-Sato, N., Joujima, T., Miyamura, Y., Habu, M., Kodama, M., Takahashi, O., Sago, T., Matsumoto-Takeda, S., Nishida, I., Tsurushima, H., Otani, Y., Yoshiga, D., Sasaguri, M., & Morimoto, Y. (2020). First Report of Sublingual Gland Ducts: Visualization by Dynamic MR Sialography and Its Clinical Application. Journal of Clinical Medicine, 9(11), 3676. https://doi.org/10.3390/jcm9113676





