Transfusion Status in Liver and Kidney Transplantation Recipients—Results from Nationwide Claims Database
Abstract
1. Introduction
2. Materials and Methods
3. Results
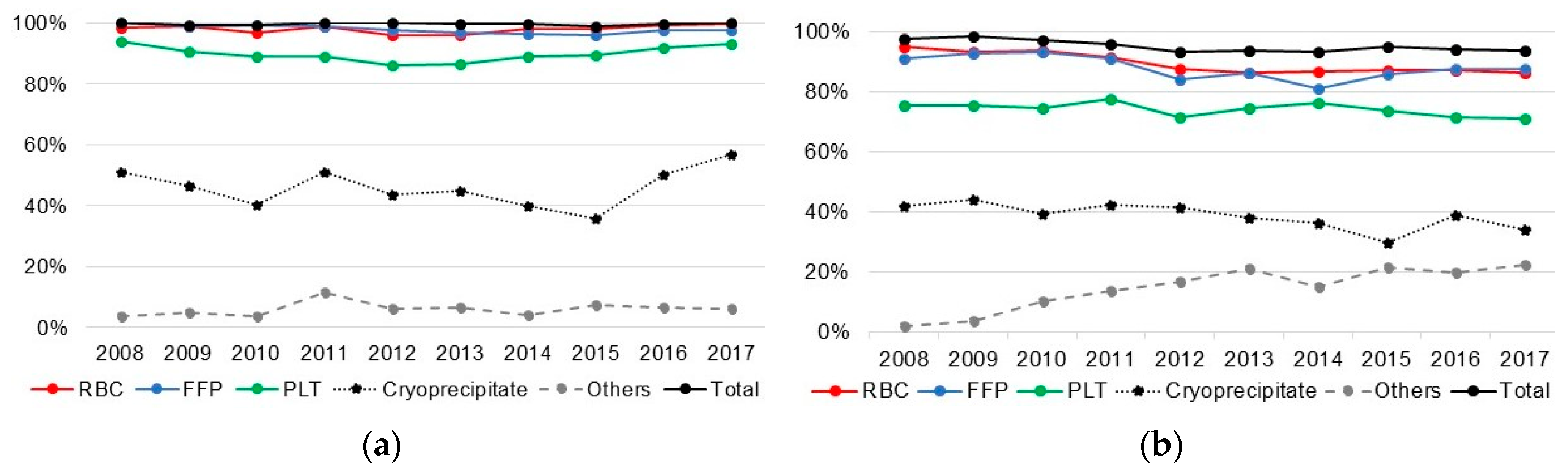
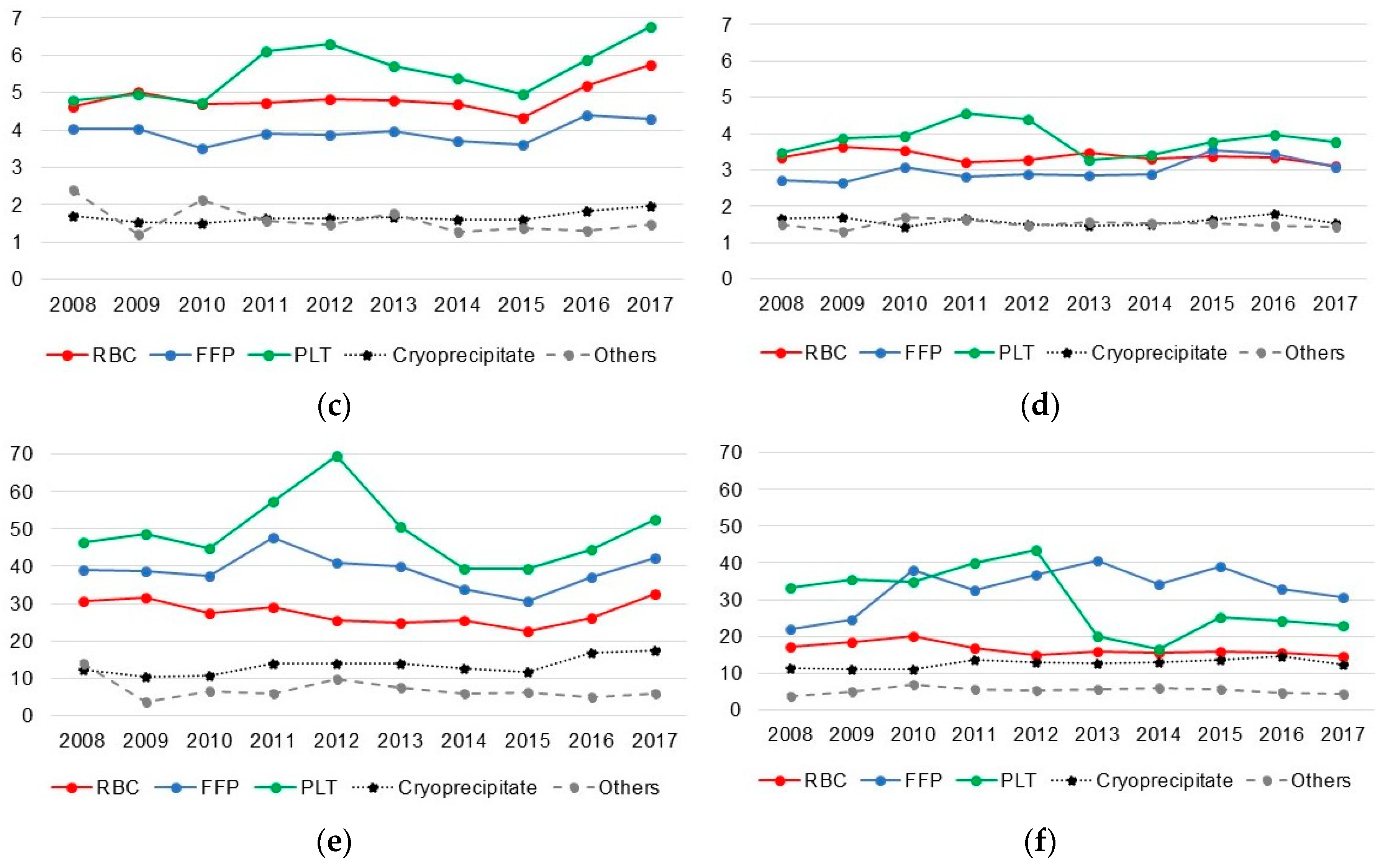
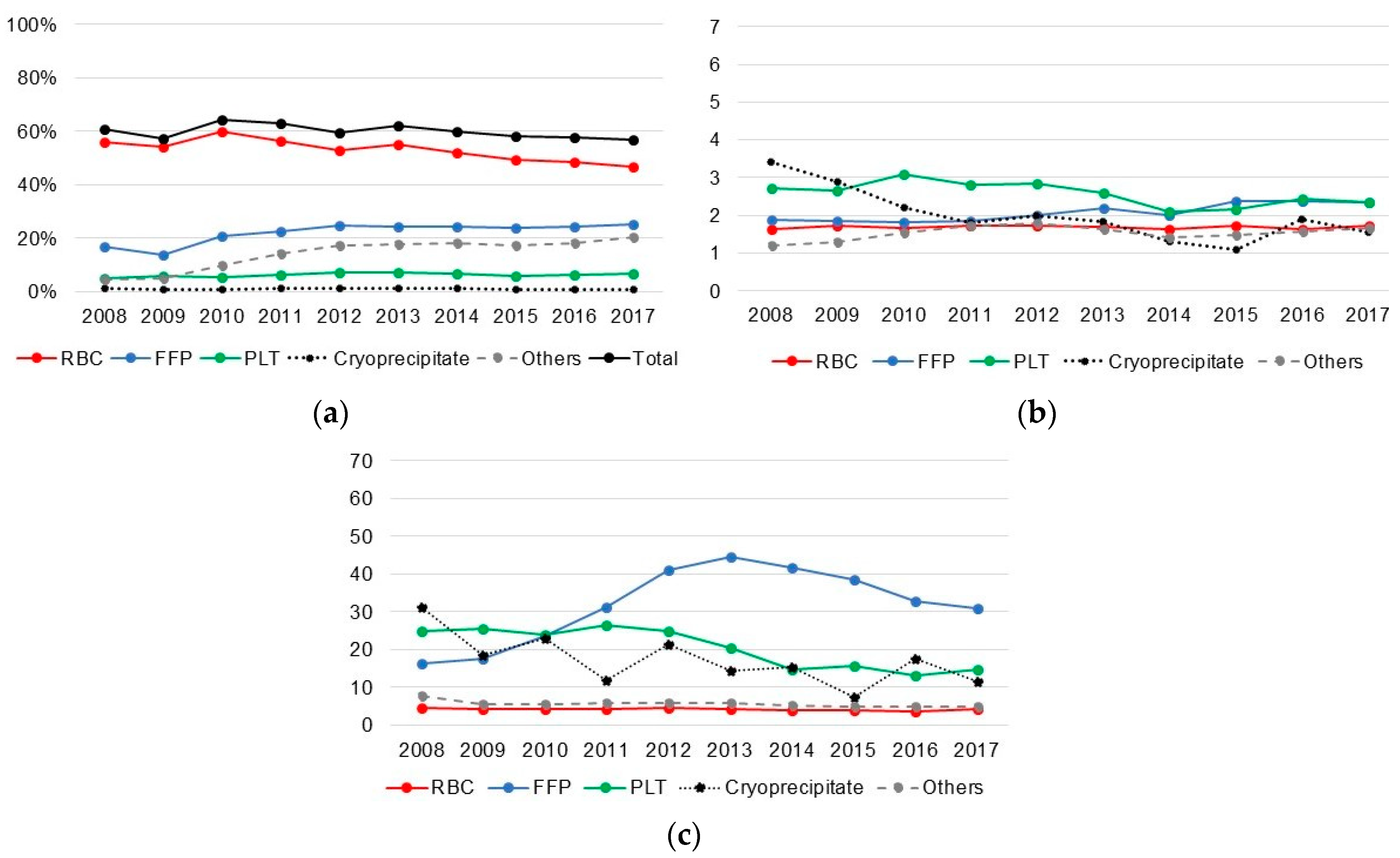
3.1. Transfusion in Liver Recipients
3.2. Transfusion in Kidney Recipients
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Black, C.K.; Termanini, K.M.; Aguirre, O.; Hawksworth, J.S.; Sosin, M. Solid organ transplantation in the 21(st) century. Ann. Transl. Med. 2018, 6, 409. [Google Scholar] [CrossRef] [PubMed]
- Cleland, S.; Corredor, C.; Ye, J.J.; Srinivas, C.; McCluskey, S.A. Massive haemorrhage in liver transplantation: Consequences, prediction and management. World J. Transplant. 2016, 6, 291–305. [Google Scholar] [CrossRef] [PubMed]
- Hart, A.; Smith, J.M.; Skeans, M.A.; Gustafson, S.K.; Wilk, A.R.; Robinson, A.; Wainright, J.L.; Haynes, C.R.; Snyder, J.J.; Kasiske, B.L.; et al. OPTN/SRTR 2016 Annual Data Report: Kidney. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2018, 18 (Suppl. S1), 18–113. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.R.; Lake, J.R.; Smith, J.M.; Schladt, D.P.; Skeans, M.A.; Harper, A.M.; Wainright, J.L.; Snyder, J.J.; Israni, A.K.; Kasiske, B.L. OPTN/SRTR 2016 Annual Data Report: Liver. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2018, 18 (Suppl. S1), 172–253. [Google Scholar] [CrossRef] [PubMed]
- Akalin, E. A New Treatment Option for Highly Sensitized Patients Awaiting Kidney Transplantation. Am. J. Kidney Dis. Off. J. Natl. Kidney Found. 2018, 71, 458–460. [Google Scholar] [CrossRef]
- Scornik, J.C.; Meier-Kriesche, H.U. Blood transfusions in organ transplant patients: Mechanisms of sensitization and implications for prevention. Am. J. Transplant. Off. J. Am. Soc. Transplant. Am. Soc. Transpl. Surg. 2011, 11, 1785–1791. [Google Scholar] [CrossRef]
- Han, S.; Kwon, J.H.; Jung, S.H.; Seo, J.Y.; Jo, Y.J.; Jang, J.S.; Yeon, S.M.; Jung, S.H.; Ko, J.S.; Gwak, M.S.; et al. Perioperative Fresh Red Blood Cell Transfusion May Negatively Affect Recipient Survival After Liver Transplantation. Ann. Surg. 2018, 267, 346–351. [Google Scholar] [CrossRef]
- Cho, W.-H. Organ donation in Korea in 2018 and an introduction of the Korea national organ donation system. Korean J. Transplant. 2019, 33, 83–97. [Google Scholar] [CrossRef]
- Cheol Seong, S.; Kim, Y.Y.; Khang, Y.H.; Heon Park, J.; Kang, H.J.; Lee, H.; Do, C.H.; Song, J.S.; Hyon Bang, J.; Ha, S.; et al. Data Resource Profile: The National Health Information Database of the National Health Insurance Service in South Korea. Int. J. Epidemiol. 2017, 46, 799–800. [Google Scholar] [CrossRef]
- Massicotte, L.; Denault, A.Y.; Beaulieu, D.; Thibeault, L.; Hevesi, Z.; Nozza, A.; Lapointe, R.; Roy, A. Transfusion rate for 500 consecutive liver transplantations: Experience of one liver transplantation center. Transplantation 2012, 93, 1276–1281. [Google Scholar] [CrossRef]
- Massicotte, L.; Thibeault, L.; Roy, A. Classical Notions of Coagulation Revisited in Relation with Blood Losses, Transfusion Rate for 700 Consecutive Liver Transplantations. Semin. Thromb. Hemost. 2015, 41, 538–546. [Google Scholar] [PubMed]
- Massicotte, L.; Carrier, F.M.; Denault, A.Y.; Karakiewicz, P.; Hevesi, Z.; McCormack, M.; Thibeault, L.; Nozza, A.; Tian, Z.; Dagenais, M.; et al. Development of a Predictive Model for Blood Transfusions and Bleeding During Liver Transplantation: An Observational Cohort Study. J. Cardiothorac. Vasc. Anesth. 2018, 32, 1722–1730. [Google Scholar] [CrossRef] [PubMed]
- Marzouk, K.; Lawen, J.; Kiberd, B.A. Blood transfusion in deceased donor kidney transplantation. Transplant. Res. 2013, 2, 4. [Google Scholar] [CrossRef] [PubMed]
- Mazzeffi, M.; Jonna, S.; Blanco, N.; Mavrothalassitis, O.; Odekwu, O.; Fontaine, M.; Rock, P.; Tanaka, K.; Thom, K. Intraoperative red blood cell transfusion, delayed graft function, and infection after kidney transplant: An observational cohort study. J. Anesth. 2018, 32, 368–374. [Google Scholar] [CrossRef]
- Cywinski, J.B.; Alster, J.M.; Miller, C.; Vogt, D.P.; Parker, B.M. Prediction of intraoperative transfusion requirements during orthotopic liver transplantation and the influence on postoperative patient survival. Anesth. Analg. 2014, 118, 428–437. [Google Scholar] [CrossRef]
- McCluskey, S.A.; Karkouti, K.; Wijeysundera, D.N.; Kakizawa, K.; Ghannam, M.; Hamdy, A.; Grant, D.; Levy, G. Derivation of a risk index for the prediction of massive blood transfusion in liver transplantation. Liver Transplant. Off. Publ. Am. Assoc. Study Liver Dis. Int. Liver Transplant. Soc. 2006, 12, 1584–1593. [Google Scholar] [CrossRef]
- Solves, P.; Carpio, N.; Moscardo, F.; Lancharro, A.; Cano, I.; Moya, A.; López-Andujar, R.; Ángel Sanz, M. Transfusion Management and Immunohematologic Complications in Liver Transplantation: Experience of a Single Institution. Transfus. Med. Hemotherapy 2015, 42, 8–14. [Google Scholar] [CrossRef]
- Roullet, S.; Biais, M.; Millas, E.; Revel, P.; Quinart, A.; Sztark, F. Risk factors for bleeding and transfusion during orthotopic liver transplantation. Ann. Fr. Anesth. Reanim. 2011, 30, 349–352. [Google Scholar] [CrossRef]
- Richards, K.M.; Spicer, R.A.; Craig, E.; Kennedy, S.E. Prevalence and predictors of blood transfusion after pediatric kidney transplantation. Pediatric Nephrol. (Berl. Ger.) 2018, 33, 2177–2184. [Google Scholar] [CrossRef]
- Scornik, J.C.; Schold, J.D.; Bucci, M.; Meier-Kriesche, H.-U. Effects of blood transfusions given after renal transplantation. Transplantation 2009, 87, 1381–1386. [Google Scholar] [CrossRef]
- Murphy, W.G. The sex difference in haemoglobin levels in adults—mechanisms, causes, and consequences. Blood Rev. 2014, 28, 41–47. [Google Scholar] [CrossRef] [PubMed]
- Marroni, C.A.; Fleck, A.M., Jr.; Fernandes, S.A.; Galant, L.H.; Mucenic, M.; de Mattos Meine, M.H.; Mariante-Neto, G.; de Mello Brandão, A.B. Liver transplantation and alcoholic liver disease: History, controversies, and considerations. World J. Gastroenterol. 2018, 24, 2785–2805. [Google Scholar] [CrossRef] [PubMed]
- Kang, E.; Han, M.; Kim, H.; Park, S.K.; Lee, J.; Hyun, Y.Y.; Kim, Y.-S.; Chung, W.; Kim, H.J.; Oh, Y.K.; et al. Baseline General Characteristics of the Korean Chronic Kidney Disease: Report from the KoreaN Cohort Study for Outcomes in Patients With Chronic Kidney Disease (KNOW-CKD). J. Korean Med. Sci. 2017, 32, 221–230. [Google Scholar] [CrossRef] [PubMed]
- Humar, A.; Ganesh, S.; Jorgensen, D.; Tevar, A.; Ganoza, A.; Molinari, M.; Hughes, C. Adult Living Donor Versus Deceased Donor Liver Transplant (LDLT Versus DDLT) at a Single Center: Time to Change Our Paradigm for Liver Transplant. Ann. Surg. 2019, 270, 444–451. [Google Scholar] [CrossRef] [PubMed]
- Scornik, J.C.; Bromberg, J.S.; Norman, D.J.; Bhanderi, M.; Gitlin, M.; Petersen, J. An update on the impact of pre-transplant transfusions and allosensitization on time to renal transplant and on allograft survival. BMC Nephrol. 2013, 14, 217. [Google Scholar] [CrossRef] [PubMed]
- Donohue, C.I.; Mallett, S.V. Reducing transfusion requirements in liver transplantation. World J. Transplant. 2015, 5, 165–182. [Google Scholar] [CrossRef]
- Suh, Y.S.; Lee, J.J.; Nho, J.H.; Lee, J.J.; Won, S.H.; Yang, H.J. Transfusion trends in hip arthroplasty in Korea: A nationwide study by the Korean National Health Insurance Service. Transfusion 2019, 59, 2324–2333. [Google Scholar] [CrossRef]
- Lee, J.; Lee, J.G.; Jung, I.; Joo, D.J.; Kim, S.I.; Kim, M.S. Development of a Korean Liver Allocation System using Model for End Stage Liver Disease Scores: A Nationwide, Multicenter study. Sci. Rep. 2019, 9, 7495. [Google Scholar] [CrossRef]
| Liver Transplantation (N = 10858) | Kidney Transplantation (N = 16191) | |||||
|---|---|---|---|---|---|---|
| Not Transfused | Transfused | pa | Not Transfused | Transfused | pa | |
| Sex | ||||||
| Male | 359 (4.7%) | 7363 (95.4%) | <0.001 | 4282 (44.6%) | 5325 (55.4%) | <0.001 |
| Female | 37 (1.2%) | 3099 (98.8%) | 2248 (34.1%) | 4336 (65.9%) | ||
| Age group (years) | ||||||
| <20 | 7 (1.5%) | 457 (98.5%) | 0.026 | 183 (43.3%) | 240 (56.7%) | 0.001 |
| 20–39 | 27 (3.5%) | 744 (96.5%) | 1650 (42.3%) | 2249 (57.7%) | ||
| 40–49 | 73 (3.1%) | 2309 (96.9%) | 1831 (40.9%) | 2641 (59.1%) | ||
| 50–59 | 197 (4.1%) | 4653 (95.9%) | 2029 (39.3%) | 3135 (60.7%) | ||
| ≥60 | 92 (3.9%) | 2299 (96.2%) | 837 (37.5%) | 1396 (62.5%) | ||
| Income (quartile) | ||||||
| 1st | 54 (3.2%) | 1614 (96.8%) | <0.001 | 1045 (41.0%) | 1505 (59.0%) | 0.183 |
| 2nd | 54 (2.9%) | 1826 (97.1%) | 1013 (40.0%) | 1521 (60.0%) | ||
| 3rd | 75 (2.9%) | 2491 (97.1%) | 1447 (40.4%) | 2131 (59.6%) | ||
| 4th | 198 (5.0%) | 3781 (95.0%) | 2113 (41.1%) | 3030 (58.9%) | ||
| Missing | 15 (2.0%) | 750 (98.0%) | 912 (38.2%) | 1474 (61.8%) | ||
| Disability | ||||||
| No | 364 (3.7%) | 9418 (96.3%) | 0.215 | 2439 (40.8%) | 3547 (59.3%) | 0.411 |
| Yes | 32 (3.0%) | 1044 (97.0%) | 4091 (40.1%) | 6114 (59.9%) | ||
| Residential area | ||||||
| Seoul | 82 (4.0%) | 1992 (96.1%) | 0.693 | 1317 (41.4%) | 1867 (58.6%) | <0.001 |
| Busan | 24 (3.4%) | 685 (96.6%) | 417 (32.0%) | 887 (68.0%) | ||
| Incheon | 13 (2.1%) | 610 (97.9%) | 337 (37.0%) | 575 (63.1%) | ||
| Daegu | 19 (3.2%) | 579 (96.8%) | 347 (39.3%) | 535 (60.7%) | ||
| Gwangju | 10 (3.2%) | 307 (96.9%) | 202 (45.6%) | 241 (54.4%) | ||
| Daejeon | 10 (3.4%) | 284 (96.6%) | 186 (37.6%) | 309 (62.4%) | ||
| Ulsan | 10 (3.7%) | 259 (96.3%) | 217 (51.4%) | 205 (48.6%) | ||
| Sejong | 1 (6.7%) | 14 (93.3%) | 12 (52.2%) | 11 (47.8%) | ||
| Gyeonggi-do | 93 (3.7%) | 2453 (96.4%) | 1598 (41.5%) | 2257 (58.6%) | ||
| Gangwon-do | 12 (3.4%) | 346 (96.7%) | 177 (38.6%) | 282 (61.4%) | ||
| Chungcheongbuk-do | 12 (3.7%) | 309 (96.3%) | 211 (46.6%) | 242 (53.4%) | ||
| Chungcheongnam-do | 17 (4.1%) | 399 (95.9%) | 234 (40.1%) | 350 (59.9%) | ||
| Jeollabuk-do | 14 (3.8%) | 359 (96.3%) | 233 (43.2%) | 307 (56.9%) | ||
| Jeollanam-do | 21 (4.6%) | 440 (95.4%) | 226 (40.3%) | 335 (59.7%) | ||
| Gyeongsangbuk-do | 27 (3.9%) | 669 (96.1%) | 327 (39.0%) | 512 (61.0%) | ||
| Gyeongsangnam-do | 30 (4.6%) | 619 (95.4%) | 390 (38.4%) | 625 (61.6%) | ||
| Jeju-do | 1 (0.7%) | 138 (99.3%) | 99 (45.0%) | 121 (55.0%) | ||
| Year of transplantation | ||||||
| 2008 | 15 (1.8%) | 844 (98.3%) | <0.001 | 435 (39.3%) | 673 (60.7%) | <0.001 |
| 2009 | 13 (1.5%) | 883 (98.6%) | 499 (42.1%) | 687 (57.9%) | ||
| 2010 | 23 (2.4%) | 935 (97.6%) | 440 (35.9%) | 787 (64.1%) | ||
| 2011 | 33 (3.1%) | 1031 (96.9%) | 584 (37.2%) | 984 (62.8%) | ||
| 2012 | 54 (4.9%) | 1047 (95.1%) | 691 (40.6%) | 1012 (59.4%) | ||
| 2013 | 47 (4.6%) | 977 (95.4%) | 636 (38.0%) | 1038 (62.0%) | ||
| 2014 | 53 (4.8%) | 1063 (95.3%) | 700 (40.3%) | 1039 (59.8%) | ||
| 2015 | 48 (3.9%) | 1199 (96.2%) | 759 (42.0%) | 1048 (58.0%) | ||
| 2016 | 52 (4.0%) | 1244 (96.0%) | 897 (42.3%) | 1224 (57.7%) | ||
| 2017 | 58 (4.5%) | 1239 (95.5%) | 889 (43.2%) | 1169 (56.8%) | ||
| Type of donor | ||||||
| Deceased | 10 (0.3%) | 3110 (99.7%) | <0.001 | - | - | |
| Living | 386 (5.0%) | 7352 (95.0%) | - | - | ||
| Total | RBC | FFP | PLT | Cryoprecipitate | |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Female | 3.81 (2.70–5.39) | 3.33 (2.67–4.15) | 1.63 (1.38–1.92) | 1.46 (1.30–1.63) | 1.11 (1.02–1.21) |
| Age group (years) | |||||
| <20 | 1.38 (0.64–3.00) | 1.76 (1.03–3.01) | 0.45 (0.33–0.60) | 0.15 (0.12–0.19) | 0.78 (0.64–0.96) |
| 20–39 | 0.63 (0.41–0.97) | 1.05 (0.75–1.46) | 1.02 (0.75–1.39) | 0.66 (0.55–0.80) | 1.32 (1.13–1.54) |
| 40–49 | 1.06 (0.80–1.40) | 1.08 (0.90–1.30) | 1.13 (0.94–1.36) | 1.08 (0.95–1.23) | 1.16 (1.05–1.29) |
| 50–59 | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| ≥60 | 0.95 (0.73–1.23) | 1.09 (0.91–1.31) | 0.96 (0.81–1.14) | 0.98 (0.86–1.11) | 1.02 (0.92–1.13) |
| Income (quartile) | |||||
| 1st | 1.42 (1.04–1.94) | 1.33 (1.07–1.65) | 1.35 (1.10–1.66) | 1.32 (1.13–1.53) | 1.02 (0.91–1.15) |
| 2nd | 1.66 (1.21–2.27) | 1.46 (1.18–1.81) | 1.37 (1.13–1.67) | 1.25 (1.09–1.44) | 0.95 (0.85–1.07) |
| 3rd | 1.59 (1.21–2.10) | 1.34 (1.11–1.62) | 1.34 (1.13–1.60) | 1.10 (0.97–1.24) | 1.03 (0.93–1.14) |
| 4th | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Disability | |||||
| No | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Yes | 1.06 (0.73–1.56) | 1.27 (0.97–1.67) | 2.07 (0.84–1.39) | 1.26 (1.06–1.52) | 1.14 (1.00–1.30) |
| Residential area | |||||
| Seoul | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Busan | 1.40 (0.88–2.25) | 1.27 (0.92–1.75) | 1.29 (0.95–1.77) | 1.46 (1.17–1.82) | 1.24 (1.04–1.48) |
| Incheon | 2.43 (1.33–4.42) | 0.96 (0.71–1.31) | 1.90 (1.31–2.74) | 1.06 (0.86–1.32) | 0.53 (0.44–0.66) |
| Daegu | 1.12 (0.67–1.88) | 1.31 (0.90–1.90) | 1.13 (0.80–1.59) | 1.10 (0.88–1.39) | 1.09 (0.90–1.31) |
| Gwangju | 1.64 (0.83–3.22) | 1.86 (1.13–3.05) | 1.40 (0.91–2.14) | 1.49 (1.10–2.01) | 1.64 (1.29–2.08) |
| Daejeon | 1.21 (0.61–2.38) | 1.40 (0.85–2.31) | 1.46 (0.90–2.34) | 1.49 (1.08–2.05) | 1.30 (1.01–1.66) |
| Ulsan | 1.23 (0.62–2.43) | 1.41 (0.85–2.33) | 0.85 (0.57–1.29) | 1.27 (0.92–1.75) | 2.40 (1.85–3.12) |
| Sejong | 0.88 (0.11–7.27) | 0.80 (0.17–3.83) | 2.11 (0.27–16.57) | 1.07 (0.32–3.61) | 2.04 (0.73–5.68) |
| Gyeonggi-do | 1.17 (0.86–1.6) | 1.15 (0.92–1.42) | 0.97 (0.79–1.19) | 1.40 (1.21–1.62) | 0.98 (0.87–1.11) |
| Gangwon-do | 1.35 (0.72–2.53) | 1.10 (0.73–1.67) | 0.91 (0.63–1.32) | 1.13 (0.86–1.49) | 1.16 (0.92–1.46) |
| Chungcheongbuk-do | 1.28 (0.69–2.41) | 1.12 (0.73–1.71) | 1.44 (0.92–2.23) | 1.21 (0.91–1.62) | 1.23 (0.97–1.56) |
| Chungcheongnam-do | 1.14 (0.67–1.97) | 1.47 (0.97–2.23) | 1.04 (0.73–1.49) | 1.37 (1.05–1.78) | 1.58 (1.28–1.96) |
| Jeollabuk-do | 1.25 (0.69–2.24) | 1.12 (0.75–1.67) | 0.74 (0.53–1.04) | 1.34 (1.01–1.77) | 0.84 (0.67–1.07) |
| Jeollanam-do | 1.13 (0.69–1.87) | 1.38 (0.95–2.02) | 1.24 (0.87–1.76) | 1.30 (1.01–1.67) | 1.64 (1.33–2.01) |
| Gyeongsangbuk-do | 1.26 (0.80–1.98) | 1.20 (0.88–1.65) | 1.48 (1.07–2.04) | 1.50 (1.20–1.87) | 0.92 (0.77–1.10) |
| Gyeongsangnam-do | 0.96 (0.62–1.48) | 0.99 (0.72–1.35) | 1.03 (0.76–1.39) | 1.26 (1.01–1.57) | 1.24 (1.03–1.48) |
| Jeju-do | 7.60 (1.04–55.42) | 2.25 (1.02–4.95) | 2.84 (1.23–6.57) | 1.80 (1.13–2.88) | 1.89 (1.33–2.67) |
| Year of transplantation | |||||
| 1–year increment | 0.89 (0.85–0.92) | 0.91 (0.88–0.93) | 0.92 (0.89–0.94) | 0.97 (0.95–0.99) | 0.97 (0.96–0.99) |
| Donor type | |||||
| Deceased | 16.67 (8.33–33.33) | 6.25 (0.55–7.69) | 6.25 (4.76–7.69) | 3.44 (3.03–4.00) | 1.39 (1.27–1.52) |
| Living | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Total | RBC | FFP | PLT | Cryoprecipitate | |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Female | 1.56 (1.47–1.67) | 1.62 (1.52–1.73) | 1.37 (1.27–1.48) | 1.47 (1.29–1.67) | 1.67 (1.23–2.28) |
| Age group (years) | |||||
| <20 | 0.83 (0.68–1.02) | 0.97 (0.79–1.19) | 0.63 (0.48–0.82) | 0.60 (0.36–1.01) | 0.62 (0.19–2.00) |
| 20–39 | 0.84 (0.77–0.91) | 0.83 (0.76–0.91) | 0.82 (0.74–0.91) | 0.83 (0.69–0.99) | 0.56 (0.35–0.89) |
| 40–49 | 0.90 (0.83–0.98) | 0.92 (0.84–0.99) | 0.95 (0.86–1.04) | 0.93 (0.78–1.10) | 0.90 (0.61–1.34) |
| 50–59 | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| ≥60 | 1.11 (1.00–1.23) | 1.15 (1.04–1.27) | 1.01 (0.89–1.13) | 1.35 (1.12–1.62) | 1.16 (0.73–1.84) |
| Income (quartile) | |||||
| 1st | 1.02 (0.92–1.13) | 1.02 (0.92–1.12) | 1.35 (1.10–1.66) | 0.80 (0.65–0.99) | 0.90 (0.52–1.54) |
| 2nd | 1.05 (0.95–1.16) | 1.06 (0.96–1.17) | 1.37 (1.13–1.67) | 0.92 (0.75–1.12) | 1.72 (1.11–2.67) |
| 3rd | 1.03 (0.94–1.12) | 1.03 (0.95–1.13) | 1.34 (1.13–1.60) | 0.98 (0.82–1.16) | 1.17 (0.75–1.80) |
| 4th | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Disability | |||||
| No | 1.00 (0.93–1.07) | 0.87 (0.81–0.93) | 1.42 (1.31–1.54) | 0.82 (0.71–0.94) | 1.27 (0.91–1.77) |
| Yes | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Residential area | |||||
| Seoul | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) | 1 (ref) |
| Busan | 1.51 (1.31–1.73) | 1.39 (1.21–1.58) | 2.00 (1.74–2.31) | 1.65 (1.31–2.09) | 2.59 (1.55–4.33) |
| Incheon | 1.23 (1.06–1.44) | 1.46 (1.26–1.7) | 0.66 (0.55–0.81) | 0.99 (0.73–1.35) | 1.24 (0.60–2.57) |
| Daegu | 1.12 (0.96–1.31) | 1.26 (1.08–1.47) | 0.75 (0.62–0.91) | 0.94 (0.68–1.3) | 0.77 (0.32–1.87) |
| Gwangju | 0.86 (0.70–1.05) | 0.92 (0.75–1.12) | 1.13 (0.89–1.43) | 1.30 (0.89–1.91) | 2.40 (1.12–5.13) |
| Daejeon | 1.21 (1.00–1.48) | 1.27 (1.05–1.54) | 0.80 (0.62–1.02) | 0.92 (0.61–1.39) | 1.65 (0.72–3.79) |
| Ulsan | 0.67 (0.55–0.83) | 0.66 (0.53–0.81) | 0.62 (0.47–0.82) | 0.52 (0.3–0.91) | 0.27 (0.04–1.96) |
| Sejong | 0.75 (0.33–1.71) | 0.64 (0.27–1.53) | 0.32 (0.07–1.36) | – | – |
| Gyeonggi-do | 1.01 (0.92–1.12) | 1.05 (0.95–1.15) | 0.95 (0.84–1.06) | 0.96 (0.79–1.17) | 0.86 (0.52–1.45) |
| Gangwon-do | 1.16 (0.95–1.42) | 1.17 (0.96–1.43) | 1.26 (1.01–1.59) | 0.83 (0.53–1.3) | 0.74 (0.22–2.44) |
| Chungcheongbuk-do | 0.83 (0.68–1.01) | 0.87 (0.71–1.06) | 1.07 (0.85–1.35) | 0.73 (0.46–1.18) | 1.23 (0.47–3.20) |
| Chungcheongnam-do | 1.11 (0.92–1.32) | 1.07 (0.89–1.27) | 1.02 (0.82–1.26) | 0.96 (0.66–1.41) | 0.20 (0.03–1.46) |
| Jeollabuk-do | 0.96 (0.80–1.16) | 1.03 (0.85–1.24) | 0.66 (0.51–0.85) | 0.96 (0.65–1.42) | 1.32 (0.54–3.21) |
| Jeollanam-do | 1.10 (0.91–1.32) | 1.06 (0.89–1.27) | 1.08 (0.87–1.34) | 0.78 (0.51–1.19) | 0.64 (0.19–2.1) |
| Gyeongsangbuk-do | 1.14 (0.98–1.34) | 1.25 (1.07–1.46) | 0.87 (0.72–1.05) | 1.23 (0.91–1.66) | 0.54 (0.19–1.55) |
| Gyeongsangnam-do | 1.17 (1.01–1.35) | 1.10 (0.95–1.27) | 1.63 (1.39–1.90) | 1.47 (1.13–1.91) | 2.04 (1.12–3.69) |
| Jeju-do | 0.89 (0.68–1.18) | 1.12 (0.85–1.48) | 0.67 (0.46–0.98) | 0.52 (0.24–1.13) | 0.53 (0.07–3.92) |
| Year of transplantation | |||||
| 1–year increment | 0.98 (0.96–0.99) | 0.95 (0.94–0.96) | 1.05 (1.04–1.06) | 1.01 (0.99–1.03) | 0.96 (0.91–1.02) |
| Alive | Dead | p-Value | |
|---|---|---|---|
| Liver recipients | |||
| Not transfused | 333 (84.1) | 63 (15.9) | 0.054 |
| Transfused | 8388 (80.2) | 2074 (19.8) | |
| Deceased donor transplant recipients | |||
| Not transfused | 10 (100) | 0 (0) | 0.045 |
| Transfused | 2219 (71.4) | 891 (28.7) | |
| Living donor transplant recipients | |||
| Not transfused | 323 (83.7) | 63 (16.3) | 0.905 |
| Transfused | 6169 (83.9) | 1183 (16.1) | |
| Kidney recipients | |||
| Not transfused | 6319 (96.8) | 211 (3.2) | <0.001 |
| Transfused | 9034 (93.5) | 627 (6.5) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, B.; Yoon, J.; Kim, H.J.; Jung, Y.K.; Lee, K.G.; Choi, D. Transfusion Status in Liver and Kidney Transplantation Recipients—Results from Nationwide Claims Database. J. Clin. Med. 2020, 9, 3613. https://doi.org/10.3390/jcm9113613
Park B, Yoon J, Kim HJ, Jung YK, Lee KG, Choi D. Transfusion Status in Liver and Kidney Transplantation Recipients—Results from Nationwide Claims Database. Journal of Clinical Medicine. 2020; 9(11):3613. https://doi.org/10.3390/jcm9113613
Chicago/Turabian StylePark, Boyoung, Junghyun Yoon, Han Joon Kim, Yun Kyung Jung, Kyeong Geun Lee, and Dongho Choi. 2020. "Transfusion Status in Liver and Kidney Transplantation Recipients—Results from Nationwide Claims Database" Journal of Clinical Medicine 9, no. 11: 3613. https://doi.org/10.3390/jcm9113613
APA StylePark, B., Yoon, J., Kim, H. J., Jung, Y. K., Lee, K. G., & Choi, D. (2020). Transfusion Status in Liver and Kidney Transplantation Recipients—Results from Nationwide Claims Database. Journal of Clinical Medicine, 9(11), 3613. https://doi.org/10.3390/jcm9113613





