Is There Any Difference in the Outcome of Geriatric and Non-Geriatric Severely Injured Patients?—A Seven-Year, Retrospective, Observational Cohort Study with Matched-Pair Analysis
Abstract
1. Introduction
2. Methods
2.1. Patients
2.2. Outcome
2.3. Case-Matched Design
2.4. Statistical Analysis
2.5. Ethics Approval and Consent to Participate
3. Results
4. Discussion
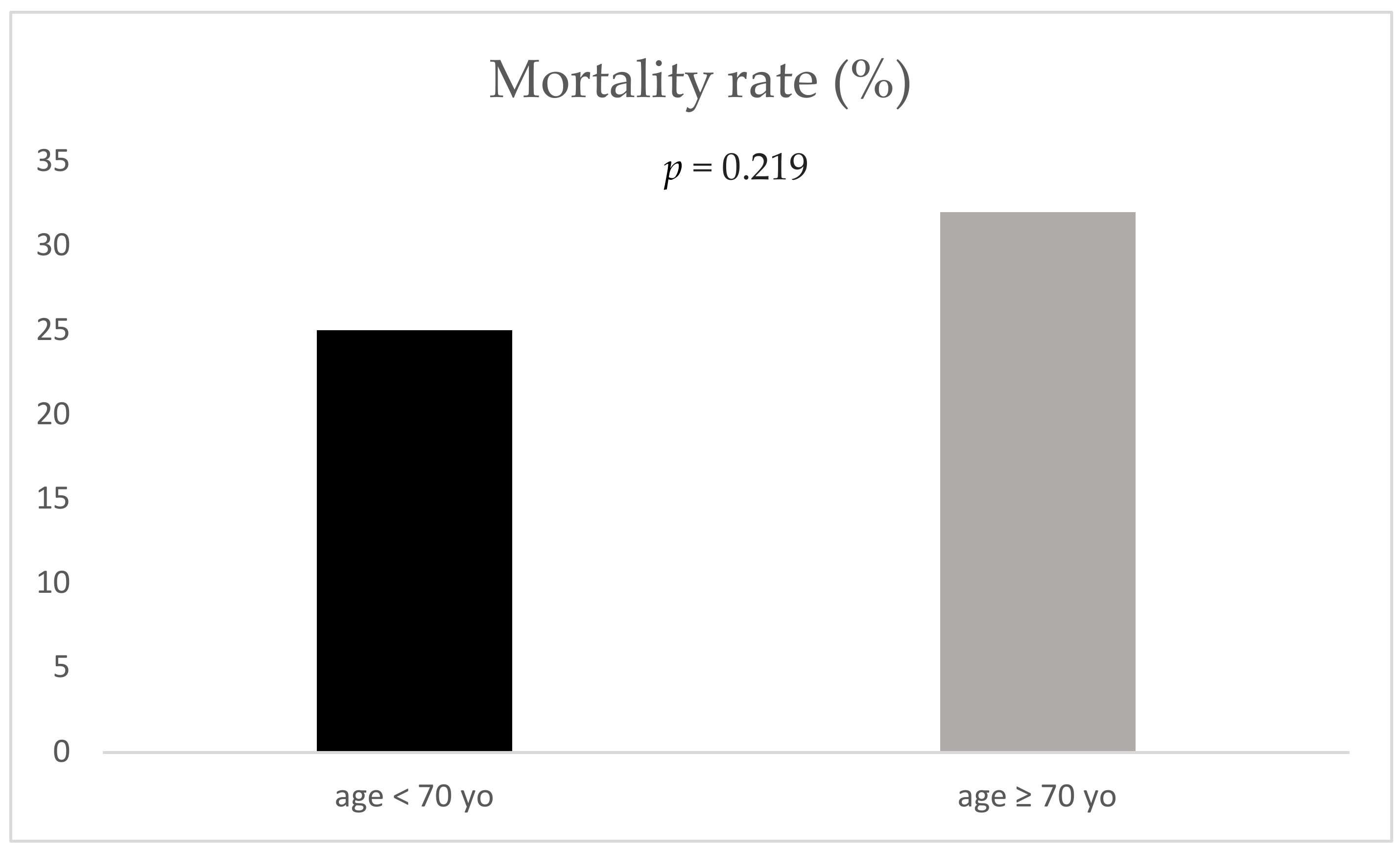
- Mortality demonstrated no significant difference between geriatric and non-geriatric patients.
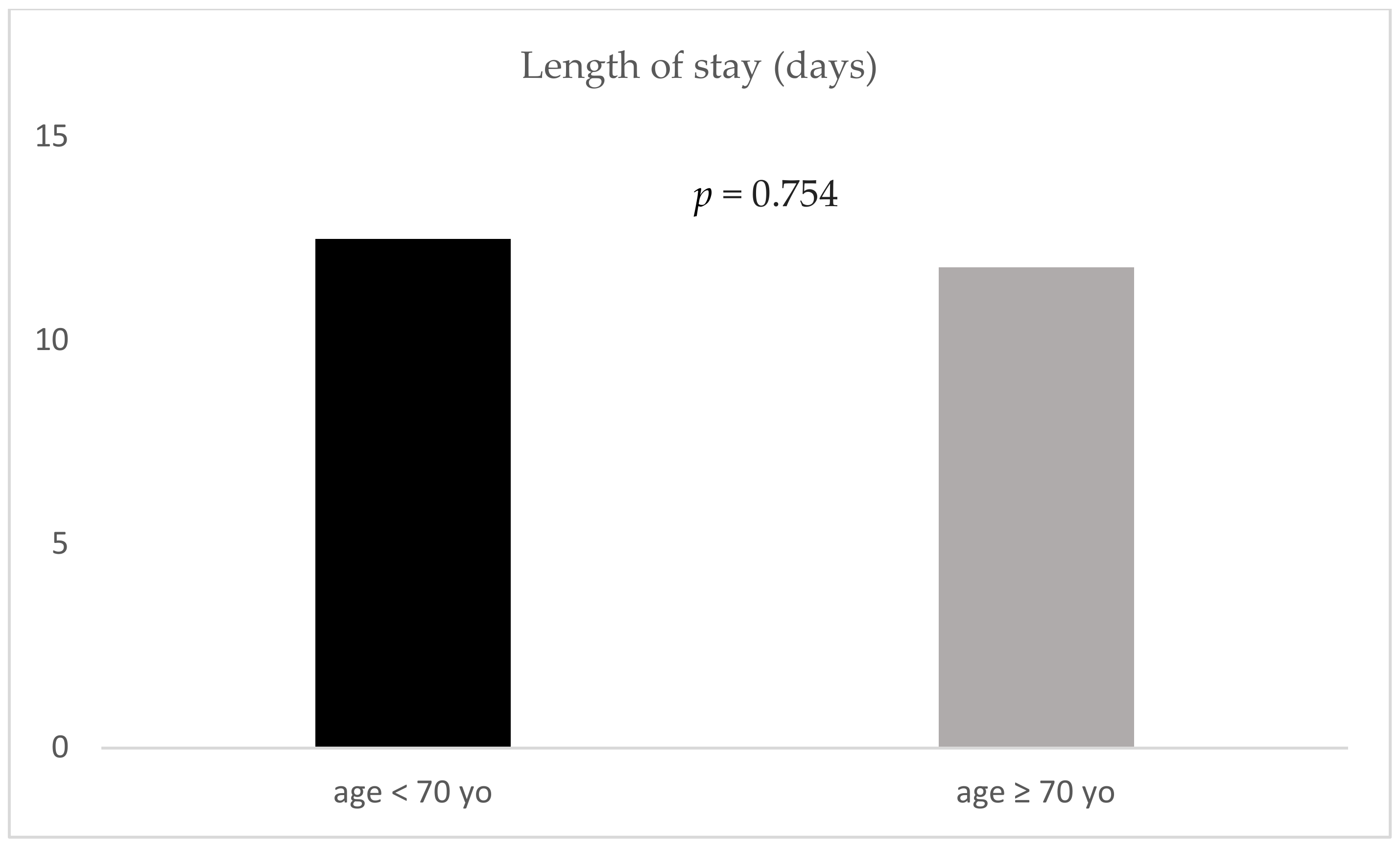
- Length of stay demonstrated no significant difference between geriatric and non-geriatric patients.
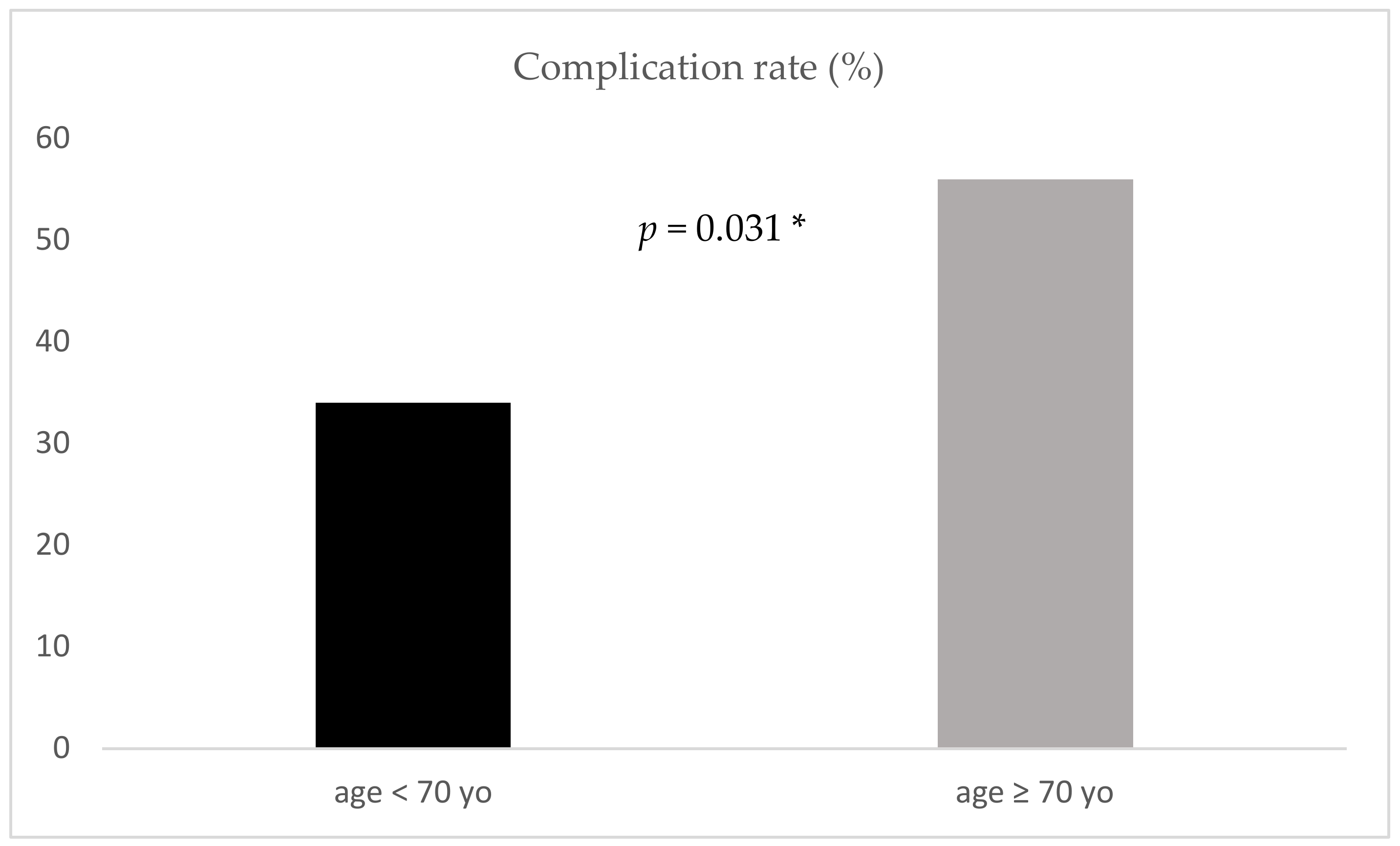
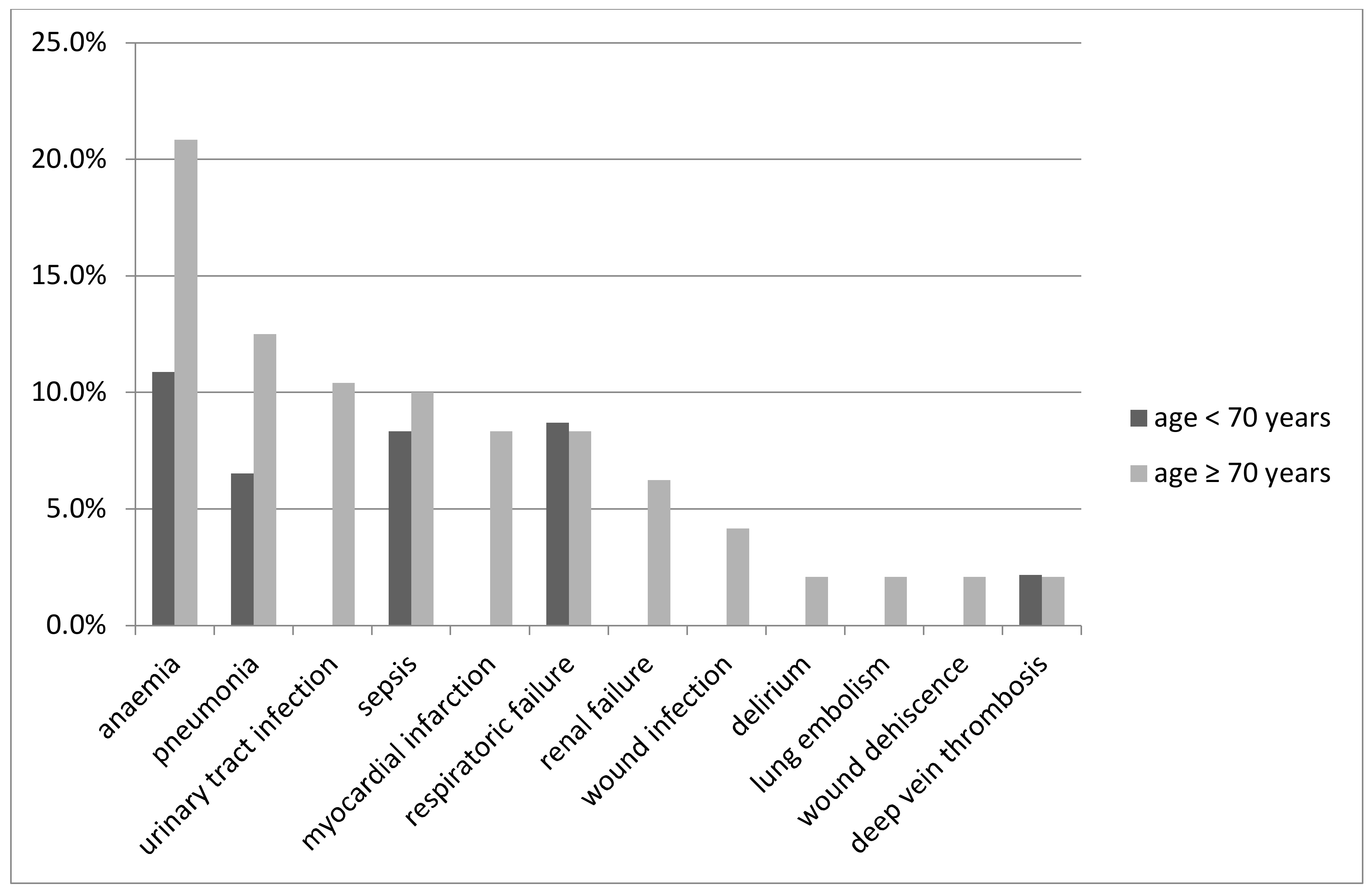
- Geriatric trauma patients had a significantly higher rate of complications.
4.1. Strengths/Limitations
4.2. Mortality
4.3. Complications
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Schneider-Schneiter BdBiEdP. Demografischer Wandel in der Schweiz: Handlungsfelder auf Bundesebene; Schneider-Schneiter BdBiEdP: Basel, Switzerland, 2016. [Google Scholar]
- Carone, G.; Costello, D. Can Europe Afford to Grow Old? Financ. Dev. 2006, 43, 28–31, Swiss confederation, Bern, Switzerland. [Google Scholar]
- Thompson, H.J.; McCormick, W.C.; Kagan, S.H. Traumatic Brain Injury in Older Adults: Epidemiology, Outcomes, and Future Implications. J. Am. Geriatr. Soc. 2006, 54, 1590–1595. [Google Scholar] [CrossRef] [PubMed]
- Keller, J.M.; Sciadini, M.F.; Sinclair, E.; O’Toole, R.V. Geriatric trauma: Demographics, injuries, and mortality. J. Orthop. Trauma 2012, 26, e161–e165. [Google Scholar] [CrossRef]
- Battistella, F.D.; Din, A.M.; Perez, L. Trauma Patients 75 Years and Older. J. Trauma Inj. Infect. Crit. Care 1998, 44, 618–624. [Google Scholar] [CrossRef]
- Grossman, M.D.; Miller, D.; Scaff, D.W.; Arcona, S. When Is an Elder Old? Effect of Preexisting Conditions on Mortality in Geriatric Trauma. J. Trauma 2002, 52, 242–246. [Google Scholar] [CrossRef]
- McMahon, D.J.; Schwab, C.W.; Kauder, D. Comorbidity and the Elderly Trauma Patient. World J. Surg. 1996, 20, 1113–1120. [Google Scholar] [CrossRef]
- Shorr, R.M.; Rodriguez, A.; Indeck, M.C.; Crittenden, M.D.; Hartunian, S.; Cowley, R.A. Blunt Chest Trauma in the Elderly. J. Trauma 1989, 29, 234–237. [Google Scholar] [CrossRef] [PubMed]
- Peterer, L.; Ossendorf, C.; Jensen, K.O.; Osterhoff, G.; Mica, L.; Seifert, B.; Werner, C.M.L.; Simmen, H.-P.; Pape, H.; Sprengel, K. Implementation of new standard operating procedures for geriatric trauma patients with multiple injuries: A single level I trauma centre study. BMC Geriatr. 2019, 19, 359. [Google Scholar] [CrossRef]
- Bonne, S.; Schuerer, D.J. Trauma in the older adult: Epidemiology and evolving geriatric trauma principles. Clin. Geriatr. Med. 2013, 29, 137–150. [Google Scholar] [CrossRef] [PubMed]
- De Vries, R.; Reininga, I.H.F.; De Graaf, M.W.; Heineman, E.; El Moumni, M.; Wendt, K.W. Older polytrauma: Mortality and complications. Injury 2019, 50, 1440–1447. [Google Scholar] [CrossRef] [PubMed]
- Cox, G.; Jones, E.; McGonagle, D.; Giannoudis, P.V. Reamer-irrigator-aspirator indications and clinical results: A systematic review. Int. Orthop. 2011, 35, 951–956. [Google Scholar] [CrossRef]
- Giannoudis, P.V.; Harwood, P.J.; Court-Brown, C.; Pape, H. Severe and multiple trauma in older patients; incidence and mortality. Injury 2009, 40, 362–367. [Google Scholar] [CrossRef]
- Demetriades, D.; Sava, J.; Alo, K.; Newton, E.; Velmahos, G.C.; Murray, J.A.; Belzberg, H.; Asensio, J.A.; Berne, T.V. Old Age as a Criterion for Trauma Team Activation. J. Trauma Acute Care Surg. 2001, 51, 754–757. [Google Scholar] [CrossRef] [PubMed]
- Champion, H.R.; Copes, W.S.; Sacco, W.J.; Lawnick, M.M.; Keast, S.L.; Bain, L.W., Jr.; E Flanagan, M.; Frey, C.F. The Major Trauma Outcome Study: Establishing national norms for trauma care. J. Trauma Acute Care Surg. 1990, 30, 1356–1365. [Google Scholar] [CrossRef]
- Oreskovich, M.R.; Howard, J.D.; Copass, M.K.; Carrico, C.J. Geriatric trauma: Injury patterns and outcome. J. Trauma 1984, 24, 565–572. [Google Scholar] [CrossRef]
- Adams, S.D.; Cotton, B.A.; McGuire, M.F.; Dipasupil, E.; Podbielski, J.M.; Zaharia, A.; Ware, D.N.; Gill, B.S.; Albarado, R.; Kozar, R.A.; et al. Unique pattern of complications in elderly trauma patients at a Level I trauma center. J. Trauma Acute Care Surg. 2012, 72, 112–118. [Google Scholar] [CrossRef]
- Schiller, W.R.; Knox, R.; Chleborad, W. A five-year experience with severe injuries in elderly patients. Accid. Anal. Prev. 1995, 27, 167–174. [Google Scholar] [CrossRef]
- Pudelek, B. Geriatric Trauma: Special Needs for a Special Population. AACN Adv. Crit. Care 2002, 13, 61–72. [Google Scholar] [CrossRef]
- Pape, H.C.; Lefering, R.; Butcher, N.; Peitzman, A.B.; Leenen, L.; Marzi, I.; Lichte, P.; Josten, C.; Bouillon, B.; Schmucker, U.; et al. The definition of polytrauma revisited: An international consensus process and proposal of the new ‘Berlin definition’. J. Trauma Acute Care Surg. 2014, 77, 780–786. [Google Scholar] [CrossRef]
- Bala, M.; Willner, D.; Klauzni, D.; Bdolah-Abram, T.; I Rivkind, A.I.; Gazala, M.A.; Elazary, R.; Almogy, G. Pre-hospital and admission parameters predict in-hospital mortality among patients 60 years and older following severe trauma. Scand. J. Trauma Resusc. Emerg. Med. 2013, 21, 91. [Google Scholar] [CrossRef]
- Pfeifer, R.; Teuben, M.; Andruszkow, H.; Barkatali, B.M.; Pape, H.-C. Mortality Patterns in Patients with Multiple Trauma: A Systematic Review of Autopsy Studies. PLoS ONE 2016, 11, e0148844. [Google Scholar] [CrossRef]
- Clement, N.D.; Tennant, C.; Muwanga, C. Polytrauma in the elderly: Predictors of the cause and time of death. Scand. J. Trauma Resusc. Emerg. Med. 2010, 18, 26. [Google Scholar] [CrossRef] [PubMed]
- Hollis, S.; Lecky, F.; Yates, D.W.; Woodford, M. The effect of pre-existing medical conditions and age on mortality after injury. J. Trauma Acute Care Surg. 2006, 61, 1255–1260. [Google Scholar] [CrossRef]
- Baker, S.P.; O’Neill, B.; Haddon, W., Jr.; Long, W.B. The injury severity score: A method for describing patients with multiple injuries and evaluating emergency care. J. Trauma Acute Care Surg. 1974, 14, 187–196. [Google Scholar] [CrossRef]
- Teasdale, G.; Jennett, B. Assessment of coma and impaired consciousness. A practical scale. Lancet 1974, 304, 81–84. [Google Scholar] [CrossRef]
- States, J.D. The Abbreviated and the Comprehensive Research Injury Scales. SAE Trans. 1969, 78, 2625–2634. [Google Scholar] [CrossRef]
- Saklad, M. Grading of Patients for Surgical Procedures. Anesthesiol. J. Am. Soc. Anesthesiol. 1941, 2, 281–284. [Google Scholar] [CrossRef]
- BBone, R.C.; Balk, R.A.; Cerra, F.B.; Dellinger, R.P.; Fein, A.M.; Knaus, W.A.; Schein, R.M.; Sibbald, W.J. Definitions for Sepsis and Organ Failure and Guidelines for the Use of Innovative Therapies in Sepsis. Chest 1992, 101, 1644–1655. [Google Scholar] [CrossRef]
- Bellomo, R.; Ronco, C.; Kellum, J.A.; Mehta, R.L.; Palevsky, P. Acute Dialysis Quality Initiative workgroup. Acute renal failure-definition, outcome measures, animal models, fluid therapy and information technology needs: The Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Crit. Care 2004, 8, R204–R212. [Google Scholar] [PubMed]
- Haider, A.H.; Saleem, T.; Leow, J.J.; Villegas, C.V.; Kisat, M.; Schneider, E.B.; Haut, E.R.; Stevens, K.A.; Cornwell, E.E.; MacKenzie, E.J.; et al. Influence of the National Trauma Data Bank on the study of trauma outcomes: Is it time to set research best practices to further enhance its impact? J. Am. Coll. Surg. 2012, 214, 756–768. [Google Scholar] [CrossRef]
- Saad, S.; Mohamed, N.; Moghazy, A.; Ellabban, G.; El-Kamash, S. Venous glucose, serum lactate and base deficit as biochemical predictors of mortality in patients with polytrauma. Ulus Travma Acil Cerrahi Derg 2016, 22, 29–33. [Google Scholar]
- Palmer, C.S.; Gabbe, B.J.; Cameron, P.A. Defining major trauma using the 2008 Abbreviated Injury Scale. Injury 2016, 47, 109–115. [Google Scholar] [CrossRef]
- Gitajn, I.L.; Castillo, R.; Breazeale, S.; Schoonover, C.; Berger, P.; Huang, Y.; O’Hara, N.; O’Toole, R.V.; Sciadini, M.F. Survivorship After High-Energy Geriatric Trauma. J. Orthop. Trauma 2017, 31, e230–e235. [Google Scholar] [CrossRef]
- Cohen, M.J.; Christie, S.A. Coagulopathy of Trauma. Crit. Care Clin. 2017, 33, 101–118. [Google Scholar] [CrossRef]
- Erdue, P.W.; Watts, D.; Kaufmann, C.R.; Trask, A.L. Differences in mortality between elderly and younger adult trauma patients: Geriatric status increases risk of delayed death. J. Trauma Acute Care Surg. 1998, 45, 805–810. [Google Scholar]
- Trunkey, D.D. Trauma. Accidental and intentional injuries account for more years of life lost in the U.S. than cancer and heart disease. Among the prescribed remedies are improved preventive efforts, speedier surgery and further research. Sci. Am. 1983, 249, 28–35. [Google Scholar] [CrossRef] [PubMed]
- Pellicane, J.V.; Byrne, K.; DeMaria, E.J. Preventable complications and death from multiple organ failure among geriatric trauma victims. J. Trauma 1992, 33, 440–444. [Google Scholar] [CrossRef]
- McMahon, D.J.; Shapiro, M.B.; Kauder, D.R. The injured elderly in the trauma intensive care unit. Surg. Clin. N. Am. 2000, 80, 1005–1019. [Google Scholar] [CrossRef]
- Dimitriou, R.; Calori, G.M.; Giannoudis, P.V. Polytrauma in the elderly: Specific considerations and current concepts of management. Eur. J. Trauma Emerg. Surg. 2011, 37, 539–548. [Google Scholar] [CrossRef]
- Morley, J.E.; Vellas, B.; van Kan, G.A.; Anker, S.D.; Bauer, J.M.; Bernabei, R.; Cesari, M.; Chumlea, W.; Doehner, W.; Evans, J.; et al. Frailty Consensus: A Call to Action. J. Am. Med. Dir. Assoc. 2013, 14, 392–397. [Google Scholar] [CrossRef]
- Cesari, M.; Calvani, R.; Marzetti, E. Frailty in Older Persons. Clin. Geriatr. Med. 2017, 33, 293–303. [Google Scholar] [CrossRef]
- Collard, R.M.; Boter, H.; Schoevers, R.A.; Oude Voshaar, R.C. Prevalence of Frailty in Community-Dwelling Older Persons: A Systematic Review. J. Am. Geriatr. Soc. 2012, 60, 1487–1492. [Google Scholar] [CrossRef]
- Gaskell, H.; Derry, S.; Moore, R.A.; McQuay, H.J. Prevalence of anaemia in older persons: Systematic review. BMC Geriatr. 2008, 8, 1. [Google Scholar] [CrossRef]
- Veerasamy, M.; Edwards, R.; Ford, G.; Kirkwood, T.; Newton, J.; Jones, D.; Kunadian, V. Acute coronary syndrome among older patients: A review. Cardiol. Rev. 2015, 23, 26–32. [Google Scholar] [CrossRef]
- Cabre, M. Pneumonia in the elderly. Curr. Opin. Pulm. Med. 2009, 15, 223–229. [Google Scholar] [CrossRef]
- Tessler, R.A.; Rangel, M.M.; Rosser, M.L.; Rivara, F.P.; Bulger, E.; Vavilala, M.S.; Reed, M.J.; Arbabi, S. Complications in low-risk older adult trauma patients: A case-control study. J. Trauma Acute Care Surg. 2019, 86, 858–863. [Google Scholar] [CrossRef]
- Janssens, J.-P.; Krause, K.-H. Pneumonia in the very old. Lancet Infect. Dis. 2004, 4, 112–124. [Google Scholar] [CrossRef]
| Age < 70 | Age ≥ 70 | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | Mean | Standard Deviation | n | % | Mean | Standard Deviation | ||
| gender | female | 276 | 24.8% | 159 | 46.0% | ||||
| male | 835 | 75.2% | 187 | 54.0% | |||||
| trauma mechanism | penetrating | 68 | 6.1% | 3 | 0.9% | ||||
| blunt | 1043 | 93.9% | 343 | 99.1% | |||||
| ISS (points) | 31 | 15 | 37 | 22 | |||||
| At admission | |||||||||
| heart rate (beats/min) | 91 | 23 | 85 | 21 | |||||
| systolic blood pressure (mmHg) | 125 | 26 | 133 | 29 | |||||
| base excess (mmol/L) | −4.1 | 4.8 | −3.6 | 4.4 | |||||
| lactate (mmol/L) | 2.5 | 2.3 | 2.2 | 2.1 | |||||
| haemoglobin (g/L) | 11.43 | 2.60 | 10.93 | 2.22 | |||||
| haematokrit (L/L) | 33.26 | 7.30 | 32.15 | 6.12 | |||||
| thrombocytes (103/µL) | 204 | 72 | 186 | 77 | |||||
| GCS (points) | 10 | 5 | 9 | 5 | |||||
| presence of coagulopathy (INR > 1.4) | 237 | 21.3% | 61 | 30.2% | |||||
| Outcome | |||||||||
| death during hospitalisation | 179 | 16.1% | 104 | 46.0% | |||||
| Length of stay (days) | 17 | 19 | 10 | 11 | |||||
| complications | 593 | 53.4% | 158 | 45.7% | |||||
| Group | Male (%) | Age (Years ± SD) | ISS (Points ± SD) | GCS (Points ± SD) | BE (mmol/L ± SD) | INR ≥ 1.4 (%) |
|---|---|---|---|---|---|---|
| n < 70 yo (n = 57) | 72 | 45 ± 16 | 33 ± 22 | 10 ± 6 | −2.6 ± 2.5 | 8.9 |
| n ≥ 70 yo (n = 57) | 72 | 79 ± 6 | 33 ± 22 | 10 ± 6 | −2.6 ± 2.7 | 8.9 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jensen, K.O.; Lempert, M.; Sprengel, K.; Simmen, H.P.; Pothmann, C.; Schlögl, M.; Bischoff-Ferrari, H.A.; Hierholzer, C.; Pape, H.C.; Neuhaus, V. Is There Any Difference in the Outcome of Geriatric and Non-Geriatric Severely Injured Patients?—A Seven-Year, Retrospective, Observational Cohort Study with Matched-Pair Analysis. J. Clin. Med. 2020, 9, 3544. https://doi.org/10.3390/jcm9113544
Jensen KO, Lempert M, Sprengel K, Simmen HP, Pothmann C, Schlögl M, Bischoff-Ferrari HA, Hierholzer C, Pape HC, Neuhaus V. Is There Any Difference in the Outcome of Geriatric and Non-Geriatric Severely Injured Patients?—A Seven-Year, Retrospective, Observational Cohort Study with Matched-Pair Analysis. Journal of Clinical Medicine. 2020; 9(11):3544. https://doi.org/10.3390/jcm9113544
Chicago/Turabian StyleJensen, Kai O., Maximilian Lempert, Kai Sprengel, Hans P. Simmen, Carina Pothmann, Mathias Schlögl, Heike A. Bischoff-Ferrari, Christian Hierholzer, Hans C. Pape, and Valentin Neuhaus. 2020. "Is There Any Difference in the Outcome of Geriatric and Non-Geriatric Severely Injured Patients?—A Seven-Year, Retrospective, Observational Cohort Study with Matched-Pair Analysis" Journal of Clinical Medicine 9, no. 11: 3544. https://doi.org/10.3390/jcm9113544
APA StyleJensen, K. O., Lempert, M., Sprengel, K., Simmen, H. P., Pothmann, C., Schlögl, M., Bischoff-Ferrari, H. A., Hierholzer, C., Pape, H. C., & Neuhaus, V. (2020). Is There Any Difference in the Outcome of Geriatric and Non-Geriatric Severely Injured Patients?—A Seven-Year, Retrospective, Observational Cohort Study with Matched-Pair Analysis. Journal of Clinical Medicine, 9(11), 3544. https://doi.org/10.3390/jcm9113544






