COVID-19 and Adverse Pregnancy Outcome: A Systematic Review of 104 Cases
Abstract
1. Introduction
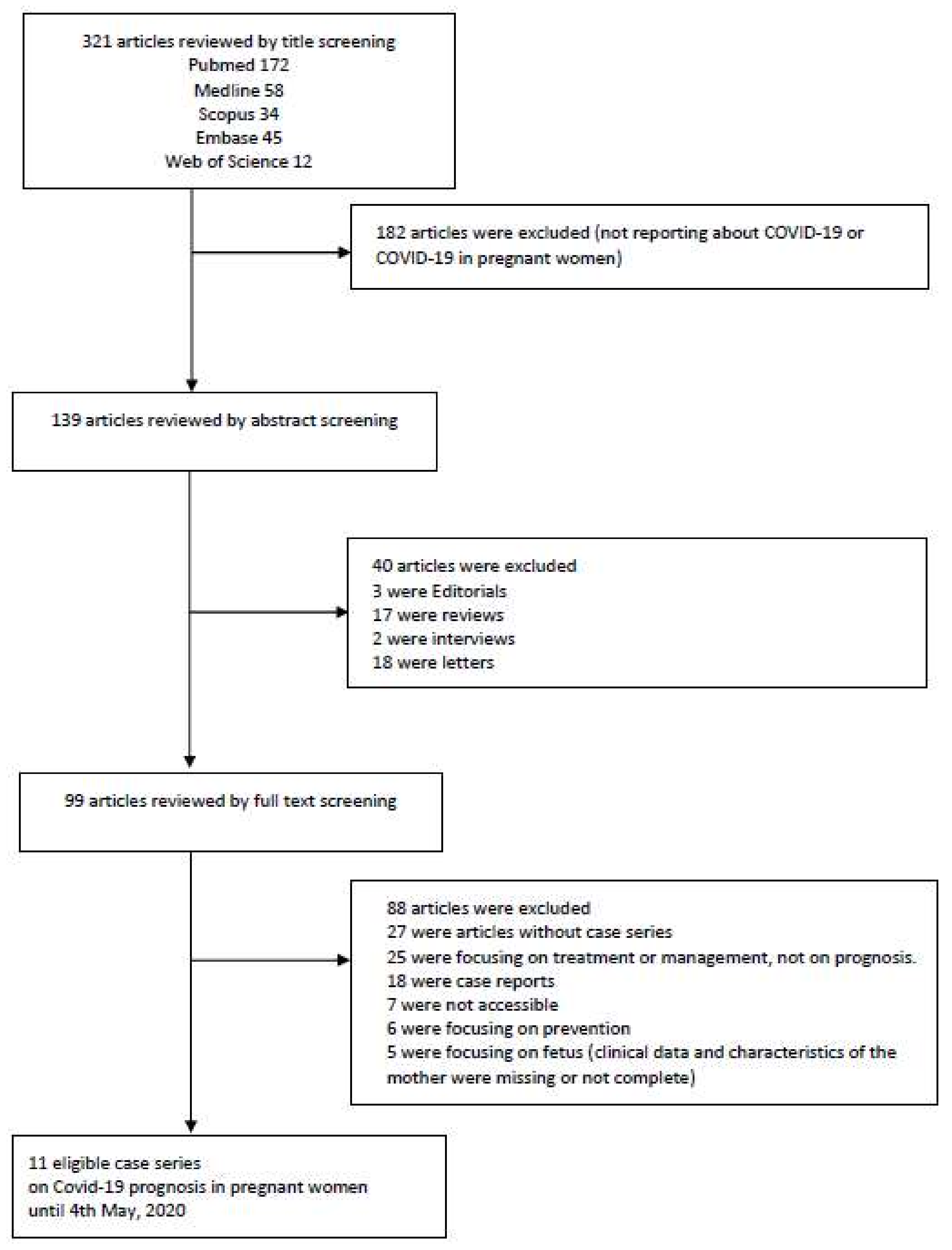
2. Materials and Methods
Literature Search Strategy and Selection Criteria
3. Results
3.1. Summary of Previously Published Meta-Analyses
3.2. Study Selection and Maternal Characteristics
3.3. Maternal Findings and Outcomes
3.4. Neonatal Findings and Outcomes
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Cucinotta, D.; Vanelli, M. Who Declares covid-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506. [Google Scholar] [CrossRef]
- Guan, W.-J.; Ni, Z.-Y.; Hu, Y.; Liang, W.-H.; Ou, C.-Q.; He, J.-X.; Liu, L.; Shan, H.; Lei, C.-L.; Hui, D.S.; et al. Clinical Characteristics of Coronavirus Disease 2019 in China. N. Engl. J. Med. 2020, 382, 1708–1720. [Google Scholar] [CrossRef] [PubMed]
- Verity, R.; Okell, L.C.; Dorigatti, I.; Winskill, P.; Whittaker, C.; Imai, N.; Cuomo-Dannenburg, G.; Thompson, H.; Walker, P.G.T.; Fu, H.; et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect. Dis. 2020, 20, 669–677. [Google Scholar] [CrossRef]
- Mehta, N.; Chen, K.; Hardy, E.; Powrie, R. Respiratory disease in pregnancy. Best Pract. Res. Clin. Obstet. Gynaecol. 2015, 29, 598–611. [Google Scholar] [CrossRef]
- Kourtis, A.P.; Read, J.S.; Jamieson, D.J. Pregnancy and Infection. N. Engl. J. Med. 2014, 370, 2211–2218. [Google Scholar] [CrossRef]
- Maxwell, C.; McGeer, A.; Tai, K.F.Y.; Sermer, M.; McGeer, A. No. 225-Management Guidelines for Obstetric Patients and Neonates Born to Mothers With Suspected or Probable Severe Acute Respiratory Syndrome (SARS). J. Obstet. Gynaecol. Can. 2017, 39, e130–e137. [Google Scholar] [CrossRef] [PubMed]
- Goodnight, W.H.; Soper, D.E. Pneumonia in pregnancy. Crit. Care Med. 2005, 33, S390–S397. [Google Scholar] [CrossRef]
- Madinger, N.E.; Greenspoon, J.S.; Ellrodt, A.G. Pneumonia during pregnancy: Has modern technology improved maternal and fetal outcome? Am. J. Obstet. Gynecol. 1989, 161, 657–662. [Google Scholar] [CrossRef]
- Piccinni, M.P.; Giudizi, M.G.; Biagiotti, R.; Beloni, L.; Giannarini, L.; Sampognaro, S.; Parronchi, P.; Manetti, R.; Annunziato, F.; Livi, C. Progesterone favors the development of human T helper cells producing Th2-type cytokines and promotes both IL-4 production and membrane CD30 expression in established Th1 cell clones. J. Immunol. 1995, 155, 128–133. [Google Scholar]
- Wegmann, T.G.; Lin, H.; Guilbert, L.; Mosmann, T.R. Bidirectional cytokine interactions in the maternal-fetal relationship: Is successful pregnancy a TH2 phenomenon? Immunol. Today 1993, 14, 353–356. [Google Scholar] [CrossRef]
- Van Well, G.; Daalderop, L.A.; Wolfs, T.G.A.M.; Kramer, B.W. Human perinatal immunity in physiological conditions and during infection. Mol. Cell. Pediatr. 2017, 4, 4. [Google Scholar] [CrossRef]
- Regal, J.F.; Gilbert, J.S.; Burwick, R.M. The complement system and adverse pregnancy outcomes. Mol. Immunol. 2015, 67, 56–70. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.-H.; Keller, J.; Wang, I.-T.; Lin, C.-C.; Lin, H.-C. Pneumonia and pregnancy outcomes: A nationwide population-based study. Am. J. Obstet. Gynecol. 2012, 207, 288.e1–288.e7. [Google Scholar] [CrossRef] [PubMed]
- Wong, S.F.; Chow, K.M.; De Swiet, M. Severe acute respiratory syndrome and pregnancy. BJOG 2003, 110, 641–642. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.-P.; Wang, Y.-H.; Chen, L.-N.; Zhang, R.; Xie, Y.-F. Clinical analysis of pregnancy in second and third trimesters complicated severe acute respiratory syndrome. Zhonghua Fu Chan Ke Za Zhi 2003, 38, 516–520. [Google Scholar]
- Wong, S.F.; Chow, K.M.; Leung, T.N.; Ng, W.F.; Ng, T.K.; Shek, C.C.; Ng, P.C.; Lam, P.W.; Ho, L.C.; To, W.W.; et al. Pregnancy and perinatal outcomes of women with severe acute respiratory syndrome. Am. J. Obstet. Gynecol. 2004, 191, 292–297. [Google Scholar] [CrossRef]
- Alfaraj, S.H.; Al-Tawfiq, J.A.; Memish, Z.A. Middle East Respiratory Syndrome Coronavirus (MERS-CoV) infection during pregnancy: Report of two cases & review of the literature. J. Microbiol. Immunol. Infect. 2018, 52, 501–503. [Google Scholar] [CrossRef]
- Sade, S.; Sheiner, E.; Wainstock, T.; Hermon, N.; Salem, S.Y.; Kosef, T.; Battat, T.L.; Oron, S.; Pariente, G. Risk for Depressive Symptoms among Hospitalized Women in High-Risk Pregnancy Units during the COVID-19 Pandemic. J. Clin. Med. 2020, 9, 2449. [Google Scholar] [CrossRef]
- Murad, M.H.; Sultan, S.; Haffar, S.; Bazerbachi, F. Methodological quality and synthesis of case series and case reports. BMJ Evid. Based Med. 2018, 23, 60–63. [Google Scholar] [CrossRef]
- Di Mascio, D.; Khalil, A.; Saccone, G.; Rizzo, G.; Buca, D.; Liberati, M.; Vecchiet, J.; Nappi, L.; Scambia, G.; Berghella, V.; et al. Outcome of coronavirus spectrum infections (sars, mers, covid-19) during pregnancy: A systematic review and meta-analysis. Am. J. Obstet. Gynecol. MFM 2020, 2, 100107. [Google Scholar] [CrossRef] [PubMed]
- Kasraeian, M.; Zare, M.; Vafaei, H.; Asadi, N.; Faraji, A.; Bazrafshan, K.; Roozmeh, S. COVID-19 pneumonia and pregnancy; a systematic review and meta-analysis. J. Matern. Neonatal Med. 2020, 19, 1–8. [Google Scholar] [CrossRef]
- Yang, Z.; Wang, M.; Zhu, Z.; Liu, Y. Coronavirus disease 2019 (COVID-19) and pregnancy: A systematic review. J. Matern. Neonatal Med. 2020, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Della Gatta, A.N.; Rizzo, R.; Pilu, G.; Simonazzi, G. Coronavirus disease 2019 during pregnancy: A systematic review of reported cases. Am. J. Obstet. Gynecol. 2020, 223, 36–41. [Google Scholar] [CrossRef] [PubMed]
- Zaigham, M.; Andersson, O. Maternal and perinatal outcomes with COVID-19: A systematic review of 108 pregnancies. Acta Obstet. Gynecol. Scand. 2020, 99, 823–829. [Google Scholar] [CrossRef]
- Matar, R.; Alrahmani, L.; Monzer, N.; Debiane, L.G.; Berbari, E.; Fares, J.; Fitzpatrick, F.; Murad, M.H. Clinical Presentation and Outcomes of Pregnant Women With Coronavirus Disease 2019: A Systematic Review and Meta-analysis. Clin. Infect. Dis. 2020. [Google Scholar] [CrossRef] [PubMed]
- Abdollahpour, S.; Khadivzadeh, T. Improving the quality of care in pregnancy and childbirth with coronavirus (COVID-19): A systematic review. J. Matern. Neonatal Med. 2020, 1–9. [Google Scholar] [CrossRef]
- Chen, S.; Liao, E.; Cao, D.; Gao, Y.; Sun, G.; Shao, Y. Clinical analysis of pregnant women with 2019 novel coronavirus pneumonia. J. Med. Virol. 2020. [Google Scholar] [CrossRef]
- Liao, J.; He, X.; Gong, Q.; Yang, L.; Zhou, C.; Li, J. Analysis of vaginal delivery outcomes among pregnant women in Wuhan, China during the COVID-19 pandemic. Int. J. Gynecol. Obstet. 2020, 150, 53–57. [Google Scholar] [CrossRef]
- Xu, L.; Yang, Q.; Shi, H.; Lei, S.; Liu, X.; Zhu, Y.; Wu, Q.; Ding, X.; Tian, Y.; Hu, Q.; et al. Clinical presentations and outcomes of SARS-CoV-2 infected pneumonia in pregnant women and health status of their neonates. Sci. Bull. 2020. [Google Scholar] [CrossRef]
- Buonsenso, D.; Raffaelli, F.; Tamburrini, E.; Biasucci, D.G.; Salvi, S.; Smargiassi, A.; Inchingolo, R.; Scambia, G.; Lanzone, A.; Testa, A.C.; et al. Clinical role of lung ultrasound for the diagnosis and monitoring of COVID-19 pneumonia in pregnant women. Ultrasound Obstet. Gynecol. 2020. [Google Scholar] [CrossRef]
- Cao, D.; Yin, H.; Chen, J.; Tang, F.; Peng, M.; Li, R.; Xie, H.; Wei, X.; Zhao, Y.; Sun, G.-Q. Clinical analysis of ten pregnant women with COVID-19 in Wuhan, China: A retrospective study. Int. J. Infect. Dis. 2020, 95, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.; Yang, W.; Wu, X.; Zhang, T.; Zhao, Y.; Ren, W.; Xia, J. Clinical Manifestation and Laboratory Characteristics of SARS-CoV-2 Infection in Pregnant Women. Virol. Sin. 2020, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Yang, P.; Wang, X.; Liu, P.; Wei, C.; He, B.; Zheng, J.; Zhao, D. Clinical characteristics and risk assessment of newborns born to mothers with COVID-19. J. Clin. Virol. 2020, 127, 104356. [Google Scholar] [CrossRef]
- Wu, X.; Sun, R.; Chen, J.; Xie, Y.; Zhang, S.; Wang, X. Radiological findings and clinical characteristics of pregnant women with COVID -19 pneumonia. Int. J. Gynecol. Obstet. 2020, 150, 58–63. [Google Scholar] [CrossRef] [PubMed]
- Zhu, H.; Wang, L.; Fang, C.; Peng, S.; Zhang, L.; Chang, G.; Xia, S.; Zhou, W. Clinical analysis of 10 neonates born to mothers with 2019-nCoV pneumonia. Transl. Pediatr. 2020, 9, 51–60. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Chen, H.; Tang, K.; Guo, Y. Clinical manifestations and outcome of SARS-CoV-2 infection during pregnancy. J. Infect. 2020. [Google Scholar] [CrossRef]
- Hantoushzadeh, S.; Shamshirsaz, A.A.; Aleyasin, A.; Seferovic, M.D.; Aski, S.K.; Arian, S.E.; Pooransari, P.; Ghotbizadeh, F.; Aalipour, S.; Soleimani, Z.; et al. Maternal Death Due to COVID-19 Disease. Am. J. Obstet. Gynecol. 2020, 223. [Google Scholar] [CrossRef]
- Ottestad, W.; Søvik, S. COVID-19 patients with respiratory failure: What can we learn from aviation medicine? Br. J. Anaesth. 2020, 125, E280–E281. [Google Scholar] [CrossRef]
- Sutton, D.; Fuchs, K.; D’Alton\, M.; Goffman, D. Universal Screening for SARS-CoV-2 in Women Admitted for Delivery. N. Engl. J. Med. 2020, 382, 2163–2164. [Google Scholar] [CrossRef]
| Authors | Included Studies, n | Sample Size | Study Period | Description | Comment |
|---|---|---|---|---|---|
| Mascio et al. 2020 [21] | 19 | 79 | Until 13 March 2020 | In mothers infected with coronavirus infections, including COVID-19, >90% of whom also had pneumonia, preterm birth is the most common adverse pregnancy outcome. Miscarriage, preeclampsia, cesarean, and perinatal death (7-11%) were also more common than in the general population. | A meta-analysis of pregnancy outcomes of patients with SARS, MERS and COVID-19—no significant results about CT findings and neonatal outcomes. |
| Kasraeian et al. 2020 [22] | 9 | 87 | Until 18 March 2020 | Most pregnant patients suffered from mild or moderate COVID-19 pneumonia with no pregnancy loss, proposing a similar pattern of the clinical characteristics of COVID-19 pneumonia to that of other adult populations. | Summarized the overall outcomes especially including vertical transmission and successful termination—there are no results about CT findings and treatment modalities. |
| Yang et al. (2020) [23] | 18 | 114 | 1 January 2020 to 26 March 2020 | The clinical characteristics of pregnant women with COVID-19 are similar to those of nonpregnant adults. Fetal and neonatal outcomes appear good in most cases, but available data only include pregnant women infected in their third trimesters. | Summarized the clinical characteristics and neonatal or pregnancy outcomes—no significant results about CT findings and neonatal outcomes. |
| Gatta et al. (2020) [24] | 6 | 51 | Until 14 March 2020 | 3 pregnancies were ongoing; of the remaining 48 pregnant women, 46 gave birth by cesarean delivery, and 2 gave birth vaginally; in this study, 1 stillbirth and 1 neonatal death were reported. | Summarized the pregnancy outcomes—there are no results about CT findings and treatment modalities. |
| Zaigham et al. (2020) [25] | 18 | 108 | 12 Feburary 2020 to 4 April 2020 | Most reports described women presenting in the third trimester with fever (68%) and coughing (34%). Lymphocytopenia (59%) with elevated CRP (70%) was observed and 91% of the women were delivered by cesarean section. Three maternal intensive care unit admissions were noted but no maternal deaths. One neonatal death and one intrauterine death were also reported. | Summarized the clinical presentations, laboratory findings and outcomes—there are no results about CT findings and treatment modalities. |
| Matar et al. (2020) [26] | 24 | 136 | Until 30 April 2020 | Most common symptoms were fever (62.9%) and cough (36.8%). Laboratory findings included elevated C-Reactive Protein (57%) and lymphocytopenia (50%). GGO was the most common radiological finding (81.7%). Preterm birth rate was 37.7% and cesarean delivery rate was 76%. There was one maternal death. There were two fetal COVID-19 cases. | A meta-analysis of pregnancy outcomes of patients—treatment modalities were not fully described. |
| Abdollahpour et al. (2020) [27] | 29 | NA | Until 25 March 2020 | In conclusion, improving quality of care in maternal health, as well as educating, training, and supporting healthcare providers in infection management to be prioritized. | Described the previous published papers—there are no summarized data of clinical outcomes. |
| Variable | Number of Reported Cases/Total Number of Patients (n = 104) | |
|---|---|---|
| Age (years) | ||
| <20 | 0 | (0.0%) |
| 20–24 | 6 | (5.8%) |
| 25–29 | 32 | (30.8%) |
| 30–34 | 38 | (36.5%) |
| 35–39 | 17 | (16.3%) |
| 40–45 | 2 | (1.9%) |
| 50–54 | 1 | (1.0%) |
| No information | 8 | (7.7%) |
| Country | ||
| China | 91 | (87.5%) |
| Italy | 4 | (3.8%) |
| Iran | 9 | (8.7%) |
| SARS-CoV-2 Quantitative RT-PCR | ||
| Positive | 72 | (69.2%) |
| Negative | 7 | (6.7%) |
| Not done | 12 | (11.6%) |
| No information | 13 | (12.5%) |
| Survival Rate | ||
| Alive | 56 | (53.9%) |
| Death | 7 | (6.7%) |
| No information | 41 | (39.4%) |
| Initial Symptoms | Number of Reported Cases/Total Number of Patients (n = 104) | |
|---|---|---|
| General Condition | ||
| Fever | 61 | (58.6%) |
| Respiratory | ||
| Chest discomfort * | 4 | (3.9%) |
| Cough | 32 | (30.7%) |
| Dyspnea | 15 | (14.4%) |
| Sputum | 1 | (1.0%) |
| Sore throat | 3 | (2.9%) |
| Nasal obstruction | 1 | (1.0%) |
| CT Findings | Number of Reported Cases/Total Number of Patients (n = 104) | |
|---|---|---|
| Finding | ||
| Abnormal | 52 | (50.0%) |
| Normal | 1 | (1.0%) |
| No information | 51 | (49.0%) |
| GGO * | ||
| Bilateral | 23 | (22.1%) |
| Unilateral | 10 | (9.6%) |
| Positive | 23 | (22.1%) |
| Negative | 1 | (1.0%) |
| No information | 47 | (45.2%) |
| Variable | Number of Reported Cases/Total Number of Patients (n = 104) | |
|---|---|---|
| Antibiotics | 27 | (25.9%) |
| Antiviral | 18 | (17.3%) |
| Steroid | 3 | (2.9%) |
| Anti-coagulant | 8 | (7.7%) |
| Hydroxychloroquine | 10 | (9.6%) |
| Obstetrical Complications | Number of Reported Cases/Total Number of Patients (n = 104) | |
|---|---|---|
| Gestational Diabetes Mellitus | 3 | (2.9%) |
| Preeclampsia | 6 | (5.8%) |
| PROM | 10 | (9.6%) |
| Fetal distress | 14 | (13.5%) |
| Abortion | 3 | (2.9%) |
| Prematurity | 9 | (8.7%) |
| Pregnancy induced HTN | 4 | (3.8%) |
| Placental abruption | 1 | (1.0%) |
| Vaginal bleeding | 1 | (1.0%) |
| Fetal death * | 5 | (4.8%) |
| Variable | Number of Reported Cases (Total n = 104) | |||
|---|---|---|---|---|
| Survival or Unreported (n = 97) | Death (n = 7) | p Value | ||
| Mean age | 30 | 36 | 0.118 | |
| SARS-CoV-2 RT-PCR positive | 65 (67.0%) | 7 (100%) | 0.713 | |
| Initial symptoms | Cough | 25 (25.8%) | 7 (100%) | 0.000 |
| Fever | 54 (55.7%) | 7 (100%) | 0.021 | |
| Dyspnea | 8 (8.2%) | 7 (100%) | 0.000 | |
| Sputum | 1 (1.0%) | 0 (0%) | 0.933 | |
| Sore throat | 3 (3.1%) | 0 (0%) | 0.810 | |
| Nasal obstruction | 1 (1.0%) | 0 (0%) | 0.933 | |
| Abnormal CT findings | 45 (46.4%) | 7 (100%) | 0.055 | |
| GGO | Bilateral | 17 (17.5%) | 6 (85.7%) | 0.020 |
| Unilateral | 10 (10.3%) | 0 (0%) | ||
| Positive | 23 (23.7%) | 0 (0%) | ||
| Negative | 1 (1.0%) | 0 (0%) | ||
| Treatment | Antibiotics | 20 (20.6%) | 7 (100%) | 0.000 |
| Antivirals | 11 (11.3%) | 7 (100%) | 0.000 | |
| Steroid | 3 (3.1%) | 0 (0%) | 0.810 | |
| Anticoagulant | 2 (2.1%) | 6 (85.7%) | 0.000 | |
| Hydroxychloroquine | 5 (5.2%) | 5 (71.4%) | 0.000 | |
| Delivery method | NSVD | 21 (21.6%) | 1 (14.3%) | 0.003 |
| C/sec | 48 (49.4%) | 4 (57.1%) | ||
| Obstetrical complications | Gestational DM | 3 (3.1%) | 0 (0%) | 1.000 |
| Vaginal bleeding | 1 (1.0%) | 0 (0%) | 0.933 | |
| Preeclampsia | 6 (6.2%) | 0 (0%) | 1.000 | |
| PROM | 10 (10.3%) | 0 (0%) | 0.482 | |
| Fetal distress | 14 (14.4%) | 0 (0%) | 0.352 | |
| Abortion | 3 (3.1%) | 0 (0%) | 1.000 | |
| Prematurity | 9 (9.3%) | 0 (00%) | 0.520 | |
| Pregnancy-induced hypertension | 4 (4.1%) | 0 (0%) | 0.754 | |
| Placental abruption | 1 (1.0%) | 0 (0%) | 0.933 | |
| Fetal death | 1 (1.0%) | 4 (57.1%) | 0.000 | |
| Variable | Total Number of Pregnancies (n = 104) | |
|---|---|---|
| Survival Rate | ||
| Alive | 57 | (54.8%) |
| Fetal Death | 5 | (4.8%) |
| Neonatal Death | 1 | (1.0%) |
| No information | 41 | (39.4%) |
| Delivery Method | ||
| NSVD | 22 | (21.2%) |
| C/sec | 52 | (50.0%) |
| No information | 30 | (28.8%) |
| SARS-CoV-2 Quantitative RT-PCR | ||
| Positive | 0 | (0.0%) |
| Negative | 46 | (44.2%) |
| Not done | 35 | (33.6%) |
| No information | 23 | (22.2%) |
| Variable | Number of Reported Cases (Total n = 104) | |||
|---|---|---|---|---|
| Survival or Unreported (n =100) | Death (n = 4)* | p Value | ||
| Mean age | 31 | 36 | 0.312 | |
| SARS-CoV-2 RT-PCR positive | >0 (0.0%) | 0 (0.0%) | 1.000 | |
| Initial symptoms | Cough | 28 (28.0%) | 4 (100.0%) | 0.008 |
| Fever | 57 (57.0%) | 4 (100.0%) | 0.140 | |
| Dyspnea | 11 (11.0%) | 4 (100.0%) | 0.000 | |
| Sputum | 1 (1.0%) | 0 (0.0%) | 0.962 | |
| Sore throat | 3 (3.0%) | 0 (0.0%) | 0.888 | |
| Nasal obstruction | 1 (1.0%) | 0 (0.0%) | 0.933 | |
| Abnormal CT findings | 48 (48.0%) | 4 (100.0%) | 0.279 | |
| GGO | Bilateral | 10 (10.0%) | 3 (75.0%) | 0.301 |
| Unilateral | 10 (10.0%) | 0 (0.0%) | ||
| Positive | 23 (23.0%) | 0 (0.0%) | ||
| Negative | 1 (1.0%) | 0 (0.0%) | ||
| Treatment | Antibiotics | 23 (23.0%) | 4 (100.0%) | 0.004 |
| Antivirals | 14 (14.0%) | 4 (100.0%) | 0.001 | |
| Steroid | 3 (3.0%) | 0 (0.0%) | 0.888 | |
| Anticoagulant | 5 (5.0%) | 3 (75.0%) | 0.002 | |
| Hydroxychloroquine | 7 (7.0%) | 3 (75.0%) | 0.002 | |
| Delivery method | NSVD | 21 (21.0%) | 1 (25.0%) | 0.001 |
| C/sec | 51 (51.0%) | 1 (25.0%) | ||
| Obstetrical complications | Gestational DM | 3 (3.0%) | 0 (0.0%) | 1.000 |
| Vaginal bleeding | 1 (1.0%) | 0 (0.0%) | 0.962 | |
| Preeclampsia | 6 (6.0%) | 0 (0.0%) | 1.000 | |
| PROM | 10 (10.0%) | 0 (0.0%) | 0.663 | |
| Fetal distress | 14 (14.0%) | 0 (0.0%) | 0.556 | |
| Abortion | 3 (3.0%) | 0 (0.0%) | 1.000 | |
| Prematurity | 9 (8.0%) | 0 (0.0%) | 0.692 | |
| Pregnancy-induced hypertension | 4 (4.0%) | 0 (0.0%) | 0.853 | |
| Placental abruption | 1 (1.0%) | 0 (0.0%) | 0.962 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abou Ghayda, R.; Li, H.; Lee, K.H.; Lee, H.W.; Hong, S.H.; Kwak, M.; Lee, M.; Kwon, M.; Koyanagi, A.; Kronbichler, A.; et al. COVID-19 and Adverse Pregnancy Outcome: A Systematic Review of 104 Cases. J. Clin. Med. 2020, 9, 3441. https://doi.org/10.3390/jcm9113441
Abou Ghayda R, Li H, Lee KH, Lee HW, Hong SH, Kwak M, Lee M, Kwon M, Koyanagi A, Kronbichler A, et al. COVID-19 and Adverse Pregnancy Outcome: A Systematic Review of 104 Cases. Journal of Clinical Medicine. 2020; 9(11):3441. https://doi.org/10.3390/jcm9113441
Chicago/Turabian StyleAbou Ghayda, Ramy, Han Li, Keum Hwa Lee, Hee Won Lee, Sung Hwi Hong, Moonsu Kwak, Minwoo Lee, Minjae Kwon, Ai Koyanagi, Andreas Kronbichler, and et al. 2020. "COVID-19 and Adverse Pregnancy Outcome: A Systematic Review of 104 Cases" Journal of Clinical Medicine 9, no. 11: 3441. https://doi.org/10.3390/jcm9113441
APA StyleAbou Ghayda, R., Li, H., Lee, K. H., Lee, H. W., Hong, S. H., Kwak, M., Lee, M., Kwon, M., Koyanagi, A., Kronbichler, A., Jacob, L., Smith, L., & Shin, J. I. (2020). COVID-19 and Adverse Pregnancy Outcome: A Systematic Review of 104 Cases. Journal of Clinical Medicine, 9(11), 3441. https://doi.org/10.3390/jcm9113441








