Sequential Approach for a Critical-View COlectomy (SACCO): A Laparoscopic Technique to Reduce Operative Time and Complications in IBD Acute Severe Colitis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Sequential Approach for a Critical-View Colectomy (SACCo) Technique
2.3. Phase 1. Left Colectomy
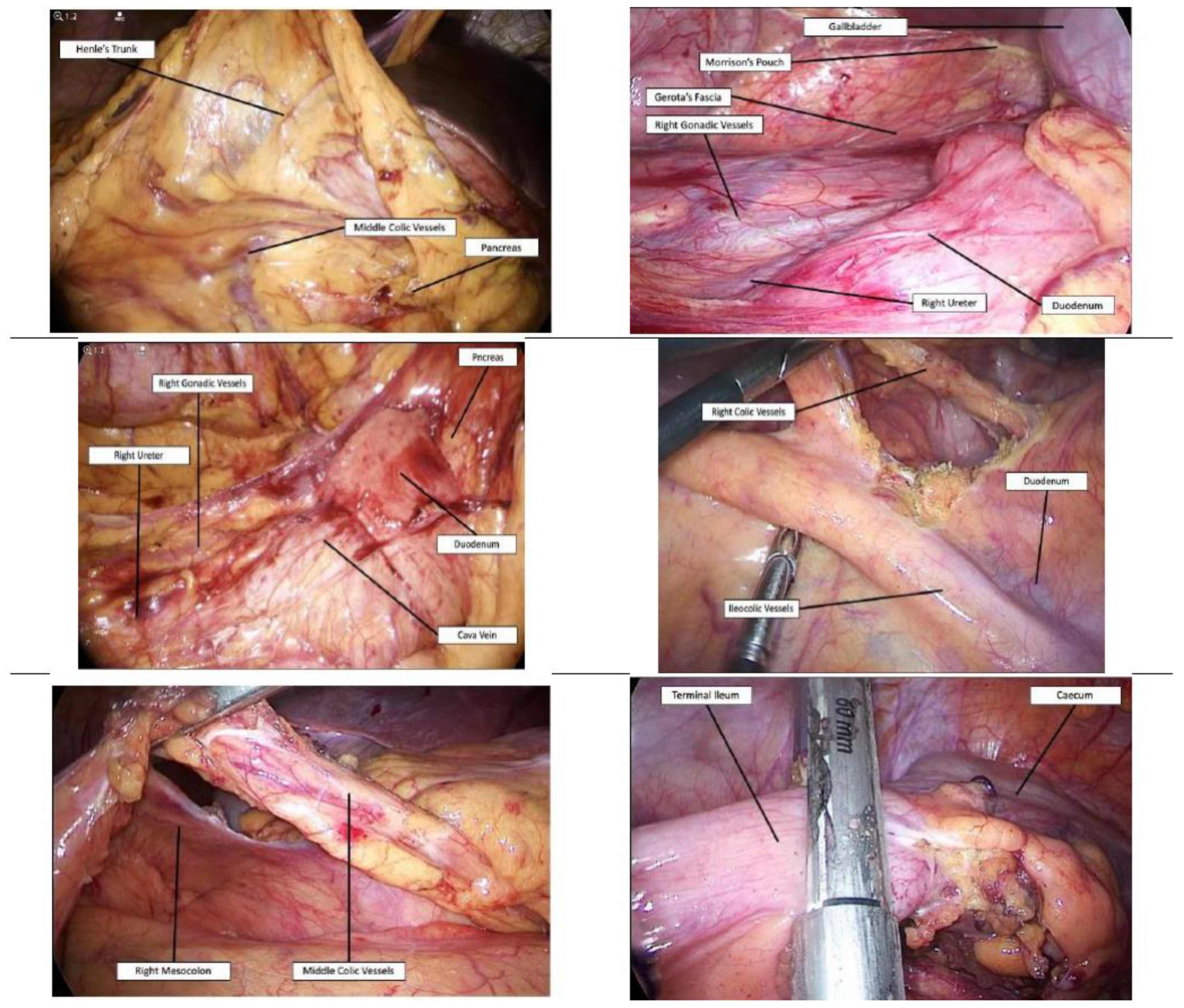
2.4. Phase 2. Right and Transverse Colectomy
2.5. Outcome Measures
2.6. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Abbreviations
| UC | ulcerative colitis |
| CD | Crohn’s Disease |
| IBD | inflammatory bowel disease |
| SCo | subtotal colectomy |
| UC-CARD | Ulcerative Colitis—Clinical Auditing and Research Database |
| CD-CARD | Crohn’s Disease Clinical Auditing and Research Database |
| TPN | total parenteral nutrition |
References
- Øresland, T.; Bemelman, W.A.; Sampietro, G.M.; Spinelli, A.; Windsor, A.; Ferrante, M.; Marteau, P.; Zmora, O.; Kotze, P.G.; Espin-Basany, E.; et al. European evidence based consensus on surgery for ulcerative colitis. J. Crohn’s Colitis 2014, 9, 4–25. [Google Scholar] [CrossRef] [PubMed]
- Bemelman, W.A.; Warusavitarne, J.; Sampietro, G.M.; Serclova, Z.; Zmora, O.; Luglio, G.; Overstraeten, A.D.B.V.; Burke, J.P.; Buskens, C.J.; Francesco, C.; et al. ECCO-ESCP Consensus on Surgery for Crohn’s Disease. J. Crohn’s Colitis 2017, 12, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Pellino, G.; Siccr, T.I.S.O.C.S.; Keller, D.S.; Sampietro, G.M.; Carvello, M.; Celentano, V.; Coco, C.; Colombo, F.; Geccherle, A.; Luglio, G.; et al. Inflammatory bowel disease position statement of the Italian Society of Colorectal Surgery (SICCR): Ulcerative colitis. Tech. Coloproctol. 2020, 24, 397–419. [Google Scholar] [CrossRef]
- Pellino, G.; Siccr, T.I.S.O.C.S.; Keller, D.S.; Sampietro, G.M.; Angriman, I.; Carvello, M.; Celentano, V.; Colombo, F.; Di Candido, F.; Laureti, S.; et al. Inflammatory bowel disease position statement of the Italian Society of Colorectal Surgery (SICCR): Crohn’s disease. Tech. Coloproctol. 2020, 24, 421–448. [Google Scholar] [CrossRef] [PubMed]
- Bartels, S.A.L.; Gardenbroek, T.J.; Ubbink, D.T.; Buskens, C.J.; Tanis, P.J.; Bemelman, W.A. Systematic review and meta-analysis of laparoscopicversusopen colectomy with end ileostomy for non-toxic colitis. Br. J. Surg. 2013, 100, 726–733. [Google Scholar] [CrossRef]
- Colombo, F.; Sahami, S.; Overstraeten, A.D.B.V.; Tulchinsky, H.; Mege, D.; Dotan, I.; Foschi, D.; Leo, C.A.; Warusavitarne, J.; D’Hoore, A.; et al. Restorative Proctocolectomy in Elderly IBD Patients: A Multicentre Comparative Study on Safety and Efficacy. J. Crohn’s Colitis 2016, 11, 671–679. [Google Scholar] [CrossRef]
- Larson, D.W.; Cima, R.R.; Dozois, E.J.; Davies, M.; Piotrowicz, K.; Barnes, S.A.; Wolff, B.; Pemberton, J. Safety, Feasibility, and Short-term Outcomes of Laparoscopic Ileal-Pouch-Anal Anastomosis. Ann. Surg. 2006, 243, 667–672. [Google Scholar] [CrossRef]
- Baek, S.-J.; Dozois, E.J.; Mathis, K.L.; Lightner, A.L.; Boostrom, S.Y.; Cima, R.R.; Pemberton, J.H.; Larson, D.W. Safety, feasibility, and short-term outcomes in 588 patients undergoing minimally invasive ileal pouch-anal anastomosis: A single-institution experience. Tech. Coloproctol. 2016, 20, 369–374. [Google Scholar] [CrossRef]
- Bartels, S.A.L.; D’hoore, A.; Cuesta, M.A.; Bensdorp, A.J.; Lucas, C.; Bemelman, W.A. Significantly Increased Pregnancy Rates After Laparoscopic Restorative Proctocolectomy. Ann. Surg. 2012, 256, 1045–1048. [Google Scholar] [CrossRef]
- Dunker, M.S.; Bemelman, W.A.; Slors, J.F.M.; Van Duijvendijk, P.; Gouma, D.J. Functional outcome, quality of life, body image, and cosmesis in patients after laparoscopic-assisted and conventional restorative proctocolectomy. Dis. Colon Rectum 2001, 44, 1800–1807. [Google Scholar] [CrossRef]
- Sampietro, G.; Colombo, F.; Frontali, A.; Baldi, C.M.; Carmagnola, S.; Cassinotti, A.; Dell’Era, A.; Massari, A.; Molteni, P.; DiLillo, D.; et al. Totally laparoscopic, multi-stage, restorative proctocolectomy for inflammatory bowel diseases. A prospective study on safety, efficacy and long-term results. Dig. Liver Dis. 2018, 50, 1283–1291. [Google Scholar] [CrossRef] [PubMed]
- Sica, G.S.; Biancone, L. Surgery for inflammatory bowel disease in the era of laparoscopy. World J. Gastroenterol. 2013, 19, 2445–2448. [Google Scholar] [CrossRef] [PubMed]
- Eshuis, E.J.; Al Saady, R.L.; Stokkers, P.C.F.; Ponsioen, C.Y.; Tanis, P.J.; Bemelman, W.A. Previous infliximab therapy and postoperative complications after proctocolectomy with ileum pouch anal anastomosis. J. Crohn’s Colitis 2013, 7, 142–149. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Vlug, M.S.; Diepenhorst, G.M.P.; Van Koperen, P.J.; Renooij, W.; De Smet, M.B.M.; Slors, J.F.M.; Boermeester, M.A.; Bemelman, W.A. Intestinal barrier function in patients undergoing colectomy. Color. Dis. 2011, 13, 1432–1437. [Google Scholar] [CrossRef] [PubMed]
- Miehsler, W.; Reinisch, W.; Valic, E.; Osterode, W.; Tillinger, W.; Feichtenschlager, T.; Grisar, J.; Machold, K.; Scholz, S.; Vogelsang, H.; et al. Is inflammatory bowel disease an independent and disease specific risk factor for thromboembolism? Gut 2004, 53, 542–548. [Google Scholar] [CrossRef]
- Nguyen, G.C.; Sam, J. Rising Prevalence of Venous Thromboembolism and Its Impact on Mortality Among Hospitalized Inflammatory Bowel Disease Patients. Am. J. Gastroenterol. 2008, 103, 2272–2280. [Google Scholar] [CrossRef]
- Wallaert, J.B.; De Martino, R.R.; Marsicovetere, P.S.; Goodney, P.P.; Finlayson, S.R.G.; Murray, J.J.; Holubar, S.D. Venous Thromboembolism After Surgery for Inflammatory Bowel Disease. Dis. Colon Rectum 2012, 55, 1138–1144. [Google Scholar] [CrossRef]
- Aalbers, A.G.J.; Doeksen, A.; Henegouwen, M.I.V.B.; Bemelman, W.A. Hand-assisted laparoscopic versus open approach in colorectal surgery: A systematic review. Color. Dis. 2010, 12, 287–295. [Google Scholar] [CrossRef]
- Marcello, P.W.; Milsom, J.W.; Wong, S.K.; Hammerhofer, K.A.; Goormastic, M.; Church, J.; Fazio, V.W. Laparoscopic restorative proctocolectomy. Dis. Colon Rectum 2000, 43, 604–608. [Google Scholar] [CrossRef]
- Maartense, S.; Dunker, M.S.; Slors, J.F.; Cuesta, M.A.; Gouma, D.J.; Van Deventer, S.J.; Van Bodegraven, A.A.; Bemelman, W.A. Hand-Assisted Laparoscopic Versus Open Restorative Proctocolectomy With Ileal Pouch Anal Anastomosis. Ann. Surg. 2004, 240, 984–992. [Google Scholar] [CrossRef]
- Antolovic, D.; Kienle, P.; Knaebel, H.-P.; Schmidt, J.; Gutt, C.; Weitz, J.; Koch, M.; Büchler, M.; Seiler, C.M. Totally laparoscopic versus conventional ileoanal pouch procedure–design of a single-centre, expertise based randomised controlled trial to compare the laparoscopic and conventional surgical approach in patients undergoing primary elective restorative proctocolectomy- LapConPouch-Trial. BMC Surg. 2006, 6, 13. [Google Scholar] [CrossRef]
- Zhang, H.; Hu, S.; Zhang, G.; Wang, K.; Chen, B.; Li, B.; Frezza, E.E. Laparoscopic versus open proctocolectomy with ileal pouch?anal anastomosis. Minim. Invasive Ther. Allied Technol. 2007, 16, 187–191. [Google Scholar] [CrossRef] [PubMed]
- McLeod, R. Long-term Results of Laparoscopic-assisted Colectomy Are Comparable to Results After Open Colectomy. Ann. Surg. 2008, 248, 8–9. [Google Scholar] [CrossRef] [PubMed]
- Fichera, A.; Silvestri, M.T.; Hurst, R.D.; Rubin, M.A.; Michelassi, F. Laparoscopic Restorative Proctocolectomy with Ileal Pouch Anal Anastomosis: A Comparative Observational Study on Long-term Functional Results. J. Gastrointest. Surg. 2008, 13, 526–532. [Google Scholar] [CrossRef]
- Geisler, D.P.; Condon, E.T.; Remzi, F.H. Single incision laparoscopic total proctocolectomy with ileopouch anal anastomosis. Color. Dis. 2009, 12, 941–943. [Google Scholar] [CrossRef]
- Holder-Murray, J.; Zoccali, M.B.; Hurst, R.D.; Umanskiy, K.; Rubin, M.; Fichera, A. Totally laparoscopic total proctocolectomy: A safe alternative to open surgery in inflammatory bowel disease. Inflamm. Bowel Dis. 2012, 18, 863–868. [Google Scholar] [CrossRef]
- Gu, J.; Stocchi, L.; Remzi, F.H.; Kiran, R.P. Total abdominal colectomy for severe ulcerative colitis: Does the laparoscopic approach really have benefit? Surg. Endosc. 2013, 28, 617–625. [Google Scholar] [CrossRef] [PubMed]
- Mege, D.; Stellingwerf, M.; Germain, A.; Colombo, F.; Pellino, G.; Di Candido, F.; Maggiori, L.; Foschi, D.; Buskens, C.J.; Adegbola, S.; et al. Management of Rectal Stump During Laparoscopic Subtotal Colectomy for IBD. A Comparative Cohort Study from 6 Referral Centres. J. Crohn’s Colitis 2020. [Google Scholar] [CrossRef]
- Strasberg, S.M.; Hertl, M.; Soper, N.J. An analysis of the problem of biliary injury during laparoscopic cholecystectomy. J. Am. Coll. Surg. 1995, 180, 101–125. [Google Scholar]
- Sampietro, G.M.; Cristaldi, M.; Maconi, G.; Fabrizio, P.; Alessandra SSandro, A.; Piergiorgio, D.; Gabriele, B.P.; Angelo, M.T. A Prospective, Longitudinal Study of Nonconventional Strictureplasty in Crohn’s Disease. J. Am. Coll. Surg. 2004, 199, 8–20, discussion-2. [Google Scholar] [CrossRef]
- Sampietro, G.; Cristaldi, M.; Porretta, T.; Montecamozzo, G.; Danelli, P.; Taschieri, A.M. Early perioperative results and surgical recurrence after strictureplasty and miniresection for complicated Crohn’s disease. Dig. Surg. 2000, 17, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Taschieri, A.M.; Cristaldi, M.; Elli, M.; Pier, G.D.; Barbara, M.; Marco, R.; Gabriele, B.P. Description of new “bowel-sparing” techniques for long strictures of Crohn’s disease. Am. J. Surg. 1997, 173, 509–512. [Google Scholar] [CrossRef]
- Sampietro, G.M.; Corsi, F.; Maconi, G.; Sandro, A.; Alice, F.; Alberto, C.; Gabriele, B.P.; Diego, F. Prospective study of long-term results and prognostic factors after conservative surgery for small bowel Crohn’s disease. Clinical gastroenterology and hepatology. Off. Clin. Pract. J. Am. Gastroenterol. Assoc. 2009, 7, 83–91. [Google Scholar]
- Dindo, D.; Demartines, N.; Clavien, P.-A. Classification of Surgical Complications. Ann. Surg. 2004, 240, 205–213. [Google Scholar] [CrossRef] [PubMed]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Initiative, F.T.S. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) Statement: Guidelines for Reporting Observational Studies. PLoS Med. 2007, 4, e296. [Google Scholar] [CrossRef] [PubMed]
- Ouaïssi, M.; Lefevre, J.H.; Bretagnol, F.; Alves, A.; Valleur, P.; Panis, Y. Laparoscopic 3-step Restorative Proctocolectomy. Surg. Laparosc. Endosc. Percutaneous Tech. 2008, 18, 357–362. [Google Scholar] [CrossRef] [PubMed]
- Dunker, M.S.; Bemelman, W.A.; Slors, J.F.; Van Hogezand, R.; Ringers, J.; Gouma, D.J. Laparoscopic-assisted vs open colectomy for severe acute colitis in patients with inflammatory bowel disease (IBD): A retrospective study in 42 patients. Surg. Endosc. 2000, 14, 911–914. [Google Scholar] [CrossRef]
- Marceau, C.; Alves, A.; Ouaissi, M.; Bouhnik, Y.; Valleur, P.; Panis, Y. Laparoscopic subtotal colectomy for acute or severe colitis complicating inflammatory bowel disease: A case-matched study in 88 patients. Surgery 2007, 141, 640–644. [Google Scholar] [CrossRef]
- Buchs, N.C.; Bloemendaal, A.L.A.; Wood, C.P.J.; Travis, S.; Mortensen, N.J.; Guy, R.J.; George, B.D. Subtotal colectomy for ulcerative colitis: Lessons learned from a tertiary centre. Color. Dis. 2017, 19, O153–O161. [Google Scholar] [CrossRef]
- Tøttrup, A.; Erichsen, R.; Sværke, C.; Laurberg, S.; Srensen, H.T. Thirty-day mortality after elective and emergency total colectomy in Danish patients with inflammatory bowel disease: A population-based nationwide cohort study. BMJ Open 2012, 2, e000823. [Google Scholar] [CrossRef]
- Teeuwen, P.H.; Stommel, M.W.J.; Bremers, A.J.A.; Krabbenborg, L.; De Jong, D.J.; Bleichrodt, R.P. Colectomy in Patients with Acute Colitis: A Systematic Review. J. Gastrointest. Surg. 2009, 13, 676–686. [Google Scholar] [CrossRef]
- Randall, J.; Singh, B.; Warren, B.F.; Travis, S.P.L.; Mortensen, N.J.; George, B.D. Delayed surgery for acute severe colitis is associated with increased risk of postoperative complications. Br. J. Surg. 2010, 97, 404–409. [Google Scholar] [CrossRef] [PubMed]
- Buskens, C.J.; Sahami, S.; Tanis, P.J.; Bemelman, W.A. The potential benefits and disadvantages of laparoscopic surgery for ulcerative colitis: A review of current evidence. Best Pr. Res. Clin. Gastroenterol. 2014, 28, 19–27. [Google Scholar] [CrossRef] [PubMed]
- De Zeeuw, S.; Ali, U.A.; Donders, R.A.R.T.; Hueting, W.E.; Keus, F.; Van Laarhoven, C.J.H.M. Update of complications and functional outcome of the ileo-pouch anal anastomosis: Overview of evidence and meta-analysis of 96 observational studies. Int. J. Color. Dis. 2012, 27, 843–853. [Google Scholar] [CrossRef] [PubMed]
- Gu, J.; Stocchi, L.; Remzi, F.; Kiran, R.P. Factors associated with postoperative morbidity, reoperation and readmission rates after laparoscopic total abdominal colectomy for ulcerative colitis. Color. Dis. 2013, 15, 1123–1129. [Google Scholar] [CrossRef]
- Holubar, S.D.; Larson, D.W.; Dozois, E.J.; Pattana-Arun, J.; Pemberton, J.H.; Cima, R.R. Minimally Invasive Subtotal Colectomy and Ileal Pouch-Anal Anastomosis for Fulminant Ulcerative Colitis. Dis. Colon Rectum 2009, 52, 187–192. [Google Scholar] [CrossRef]
- Messenger, D.E.; Mihailovic, D.; Macrae, H.M.; O’Connor, B.I.; Victor, J.C.; McLeod, R.S. Subtotal Colectomy in Severe Ulcerative and Crohn’s Colitis. Dis. Colon Rectum 2014, 57, 1349–1357. [Google Scholar] [CrossRef]
- Colombo, F.; Pellino, G.; Selvaggi, F.; Corsi, F.; Sciaudone, G.; Sampietro, G.; Foschi, D. Minimally invasive surgery and stoma-related complications after restorative proctocolectomy for ulcerative colitis. A two-centre comparison with open approach. Am. J. Surg. 2019, 217, 682–688. [Google Scholar] [CrossRef]
- Greenstein, A.J.; Romanoff, A.M.; Moskowitz, A.J.; Sosunov, E.A.; Khaitov, S.; Egorova, N.N. Payer Status and Access to Laparoscopic Subtotal Colectomy for Ulcerative Colitis. Dis. Colon Rectum 2013, 56, 1062–1067. [Google Scholar] [CrossRef]
- Causey, M.W.; Stoddard, D.; Johnson, E.K.; Maykel, J.A.; Martin, M.J.; Rivadeneira, D.; Steele, S.R. Laparoscopy impacts outcomes favorably following colectomy for ulcerative colitis: A critical analysis of the ACS-NSQIP database. Surg. Endosc. 2012, 27, 603–609. [Google Scholar] [CrossRef]
- Chung, T.P.; Fleshman, J.W.; Birnbaum, E.H.; Hunt, S.R.; Dietz, D.W.; Read, T.E.; Mutch, M.G. Laparoscopic vs. Open Total Abdominal Colectomy for Severe Colitis. Dis. Colon Rectum 2009, 52, 4–10. [Google Scholar] [CrossRef] [PubMed]
- El-Gazzaz, G.S.; Kiran, R.P.; Remzi, F.H.; Hull, T.L.; Geisler, D.P. Outcomes for case-matched laparoscopically assistedversusopen restorative proctocolectomy. BJS 2009, 96, 522–526. [Google Scholar] [CrossRef] [PubMed]
- Goede, A.C.; Reeves, A.; Dixon, A.R. Laparoscopic restorative proctocolectomy: A 10-year experience of an evolving technique. Color. Dis. 2011, 13, 1153–1157. [Google Scholar] [CrossRef] [PubMed]
- Hata, K.; Kazama, S.; Nozawa, H.; Kawai, K.; Kiyomatsu, T.; Tanaka, J.; Tanaka, T.; Nishikawa, T.; Yamaguchi, H.; Ishihara, S.; et al. Laparoscopic surgery for ulcerative colitis: A review of the literature. Surg. Today 2014, 45, 933–938. [Google Scholar] [CrossRef] [PubMed]
- Sakpal, S.V.; Bindra, S.S.; Chamberlain, R.S. Laparoscopic Cholecystectomy Conversion Rates Two Decades Later. JSLS J. Soc. Laparoendosc. Surg. 2010, 14, 476–483. [Google Scholar] [CrossRef]

| Group A (n = 86) | Group B (n = 59) | p | |
|---|---|---|---|
| Age (years) | 42.8 ± 17.3 | 45 ± 16.3 | ns |
| Gender | |||
| M | 47 (54.6%) | 37 (62.7%) | |
| F | 39 (45.4%) | 22 (37.3%) | ns |
| Age at Diagnosis (years) | 35.2 ± 18.06 | 38.3 ± 17.5 | ns |
| Disease Duration (years) | 7.19 ± 7.3 | 7 ± 7.2 | ns |
| Smoking Habit | 2 (2.3%) | 5 (8.4%) | ns |
| Family History | 6 (6.9%) | 3 (5%) | ns |
| Extraintestinal Manifestations | 11 (12.7%) | 7 (11.8%) | ns |
| Hb (g/L) | 10.6 | 10.4 | ns |
| WBC count (×109/L) | 10.543 | 8.971 | ns |
| CRP (mg/L) | 42.82 | 37.4 | ns |
| Albumin (g/L) | 3.7 | 2.8 | ns |
| Transthyretine (g/L) | 0.17 | 0.14 | ns |
| TPN | 64 (74.41%) | 42 (71.1%) | ns |
| Preoperative Therapy | |||
| 5-ASA | 6 (6.9%) | 5 (8.4%) | ns |
| Immunomodulators | 18 (20.9%) | 10 (16.9%) | ns |
| Biologicals | 67 (77.9%) | 17 (28.8%) | <0.0001 |
| Steroids | 74 (86%) | 49 (83%) | ns |
| Combo | 29 (33.7%) | 17 (28.8%) | ns |
| Group A (n = 86) | Group B (n = 59) | p | ||
|---|---|---|---|---|
| Duration of Surgery (min) | 144.65 ± 37.4 | 224.65 ± 52.5 | <0.0001 | |
| Conversion | 1 (1.1%) | 2 (3.3%) | ns | |
| Clavien-Dindo I-II | 4 (4.6%) | 5 (8.4%) | ns | |
| Clavien-Dindo III | III A | 3 (3.4%) | 1 (1.6%) | ns |
| III B | 3 (3.4%) | 4 (6.7%) | ns | |
| Mortality | / | / | ns | |
| Readmission | 2 (2.3%) | 8 (13.5%) | 0.01 | |
| Reoperation | 4 (4.6%) | 5 (8.4%) | ns | |
| Hospital stay (days) | 13.4 ± 7.3 | 15.3 ± 8.1 | ns | |
| Postoperative stay (days) | 7.2 ± 2.3 | 8.8 ± 4.1 | 0.003 | |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sampietro, G.M.; Colombo, F.; Corsi, F. Sequential Approach for a Critical-View COlectomy (SACCO): A Laparoscopic Technique to Reduce Operative Time and Complications in IBD Acute Severe Colitis. J. Clin. Med. 2020, 9, 3382. https://doi.org/10.3390/jcm9103382
Sampietro GM, Colombo F, Corsi F. Sequential Approach for a Critical-View COlectomy (SACCO): A Laparoscopic Technique to Reduce Operative Time and Complications in IBD Acute Severe Colitis. Journal of Clinical Medicine. 2020; 9(10):3382. https://doi.org/10.3390/jcm9103382
Chicago/Turabian StyleSampietro, Gianluca Matteo, Francesco Colombo, and Fabio Corsi. 2020. "Sequential Approach for a Critical-View COlectomy (SACCO): A Laparoscopic Technique to Reduce Operative Time and Complications in IBD Acute Severe Colitis" Journal of Clinical Medicine 9, no. 10: 3382. https://doi.org/10.3390/jcm9103382
APA StyleSampietro, G. M., Colombo, F., & Corsi, F. (2020). Sequential Approach for a Critical-View COlectomy (SACCO): A Laparoscopic Technique to Reduce Operative Time and Complications in IBD Acute Severe Colitis. Journal of Clinical Medicine, 9(10), 3382. https://doi.org/10.3390/jcm9103382






