Delirium Superimposed on Dementia in Perioperative Period and Intensive Care
Abstract
1. Introduction
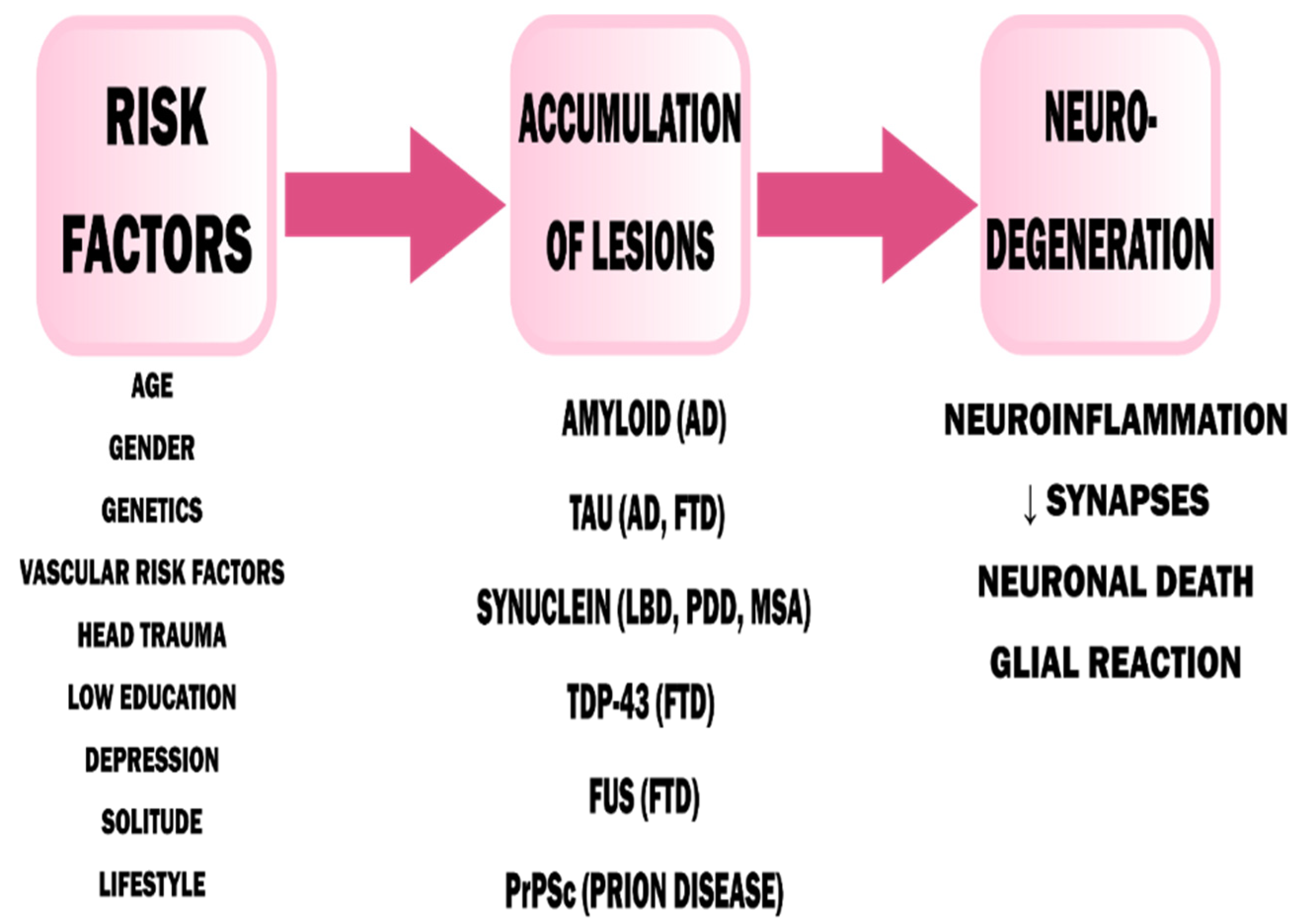
2. Pathophysiology of Dementia
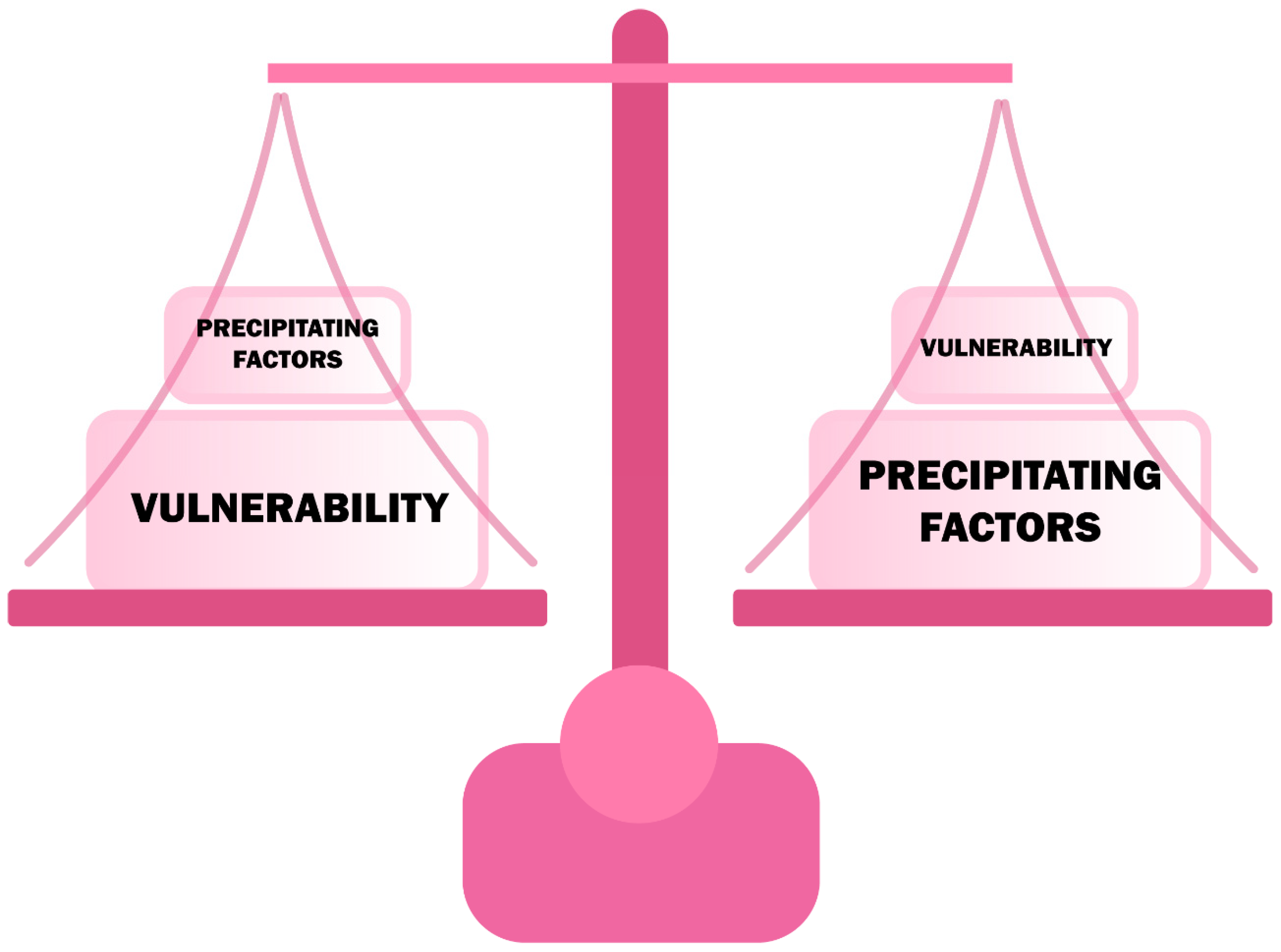
3. Pathophysiology of Delirium
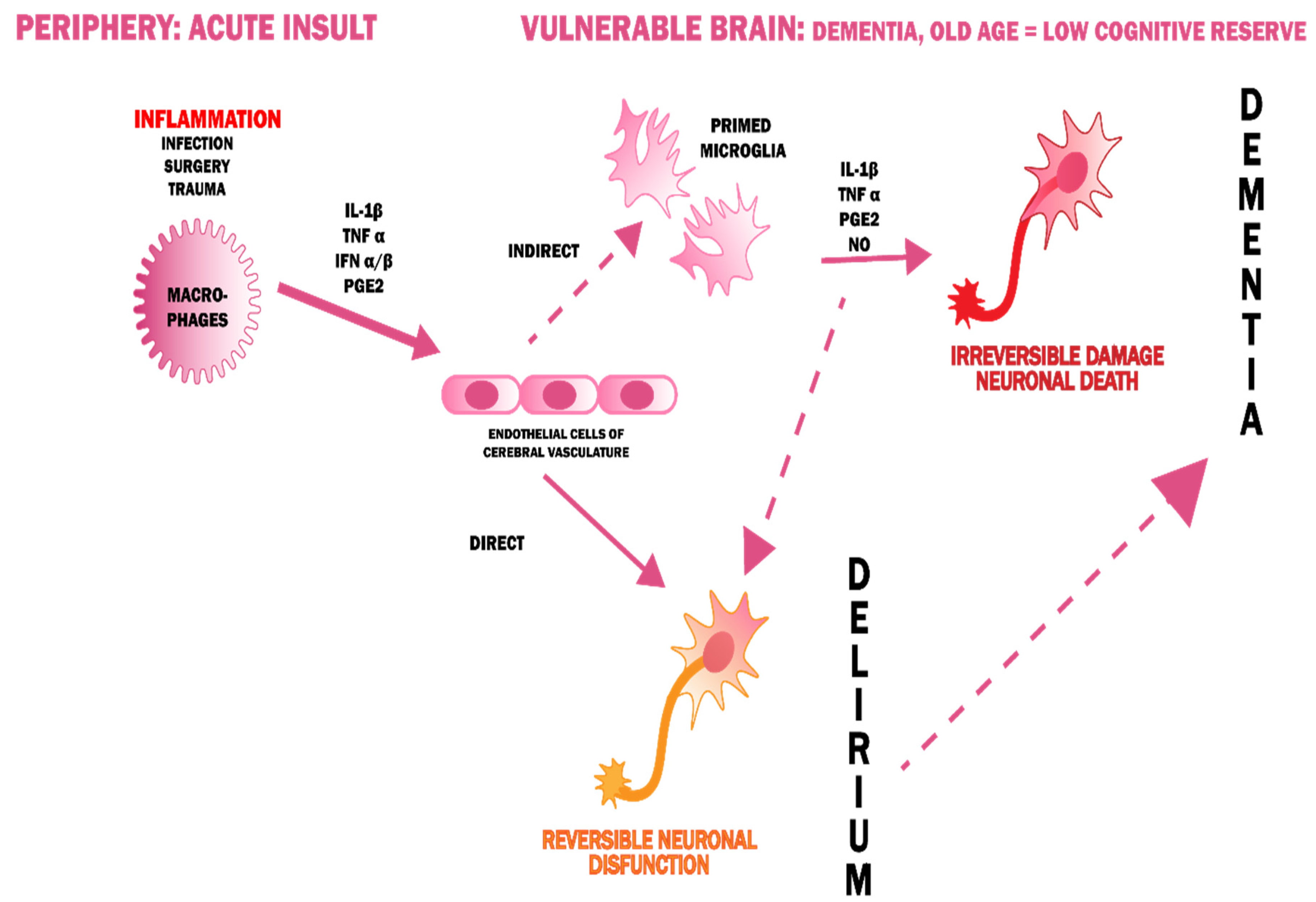
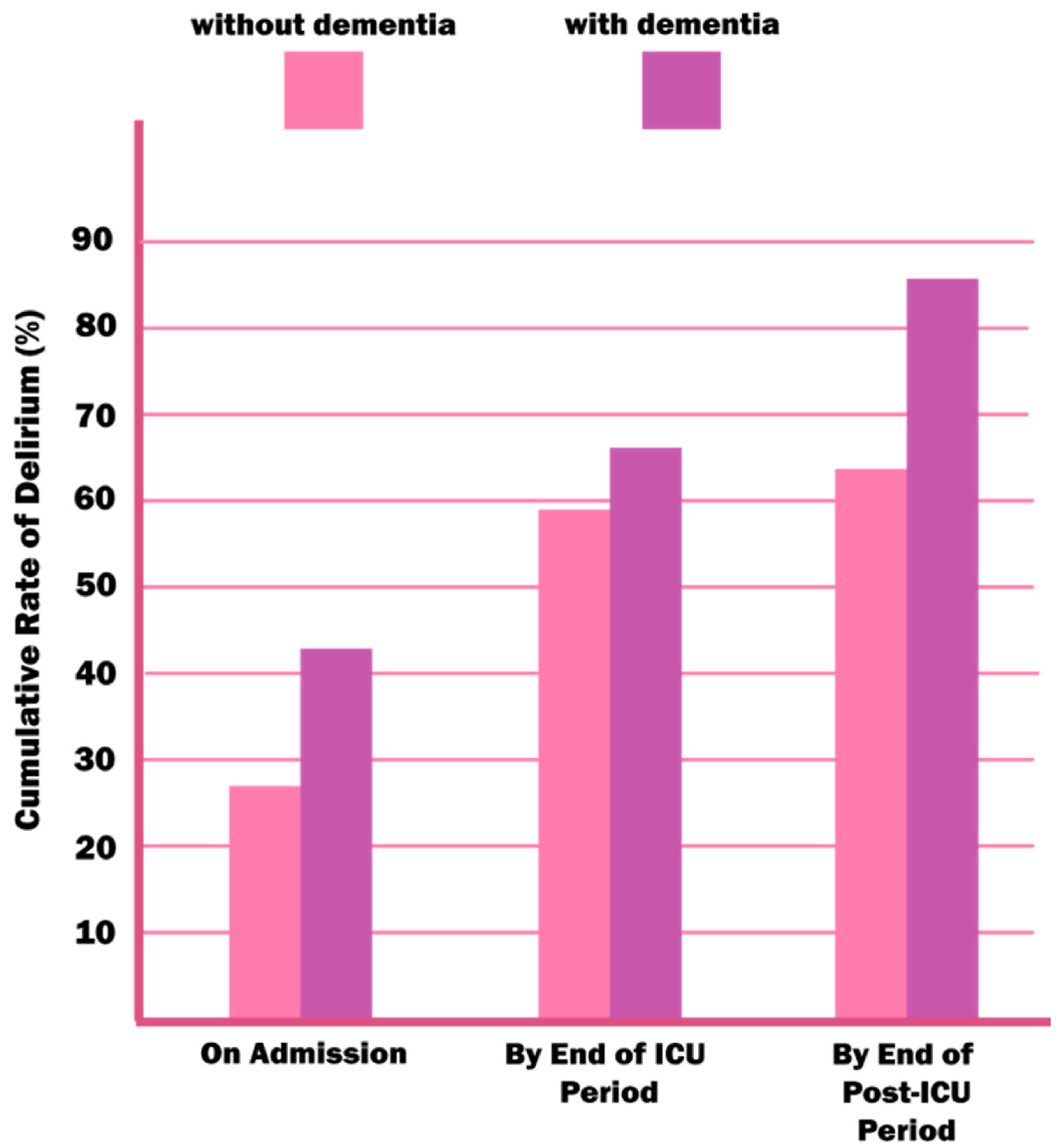
4. Delirium and Dementia—A Pathophysiological Interrelationship
5. Symptoms of Delirium
6. Types of Delirium
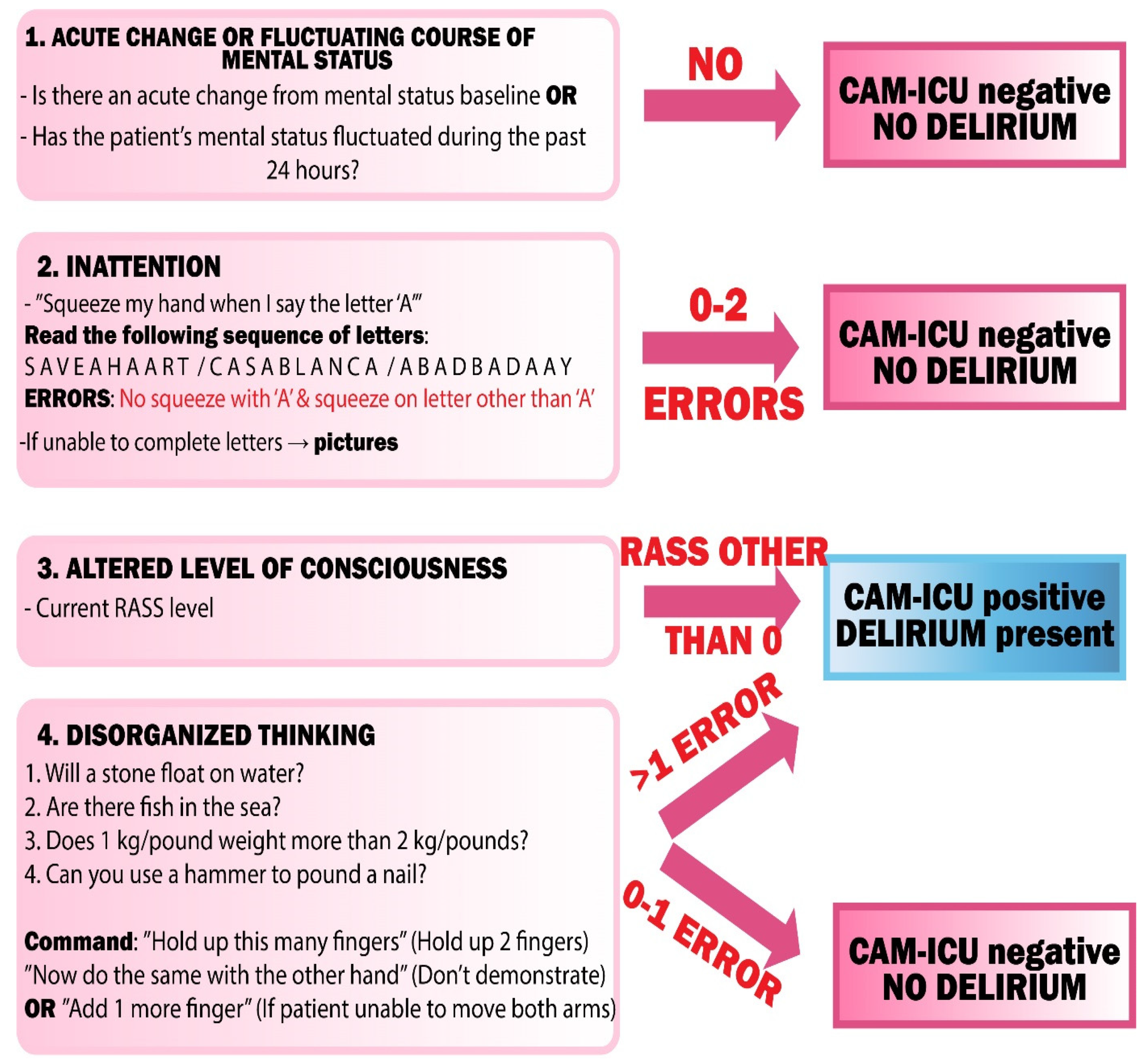
7. Diagnosis of Delirium Superimposed on Dementia
- Loneliness of the patient and absence of a person that would monitor the patient’s daily condition and who could notice a sudden change in behavior;
- Lack of doctor–patient communication;
- Misconception that older people are “withdrawn” and disorganized on their own;
- Misconception that a patient being asleep is only attributable to fatigue.
8. Dementia Management
8.1. Acetylcholinesterase Inhibitors
8.2. Memantine
9. Delirium Management
10. Summary
Author Contributions
Funding
Conflicts of Interest
References
- American Society of Psychiatrists. DSM-5 Criteria for Delirium. The Diagnostic and Statistical Manual of Mental Disorders (DSM-5); American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Elie, M.; Rousseau, F.; Cole, M.; Primeau, F.; McCusker, J.; Bellavance, F. Prevalence and detection of delirium in elderly emergency department patients. CMAJ 2000, 163, 977–981. [Google Scholar]
- Fong, T.G.; Davis, D.; Growdon, M.E.; Albuquerque, A.; Inouye, S.K. The interface between delirium and dementia in elderly adults. Lancet Neurol. 2015, 14, 823–832. [Google Scholar] [CrossRef]
- Jackson, J.C.; Gordon, S.M.; Hart, R.P.; Hopkins, R.O.; Ely, E.W. The association between delirium and cognitive decline: A review of the empirical literature. Neuropsychol. Rev. 2004, 14, 87–98. [Google Scholar] [CrossRef]
- Pompei, P.; Foreman, M.; Rudberg, M.A.; Inouye, S.K.; Braund, V.; Cassel, C.K. Delirium in hospitalized older persons: Outcomes and predictors. J. Am. Geriatr. Soc. 1994, 42, 809–815. [Google Scholar] [CrossRef]
- Roden, M.; Simmons, B.B. Delirium superimposed on dementia and mild cognitive impairment. Postgrad. Med. 2014, 126, 129–137. [Google Scholar]
- World Health Organisation. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 10 August 2020).
- Inouye, S.K.; Westendorp, R.G.; Saczynski, J.S. Delirium in elderly people. Lancet 2014, 383, 911–922. [Google Scholar] [CrossRef]
- Alzheimer Europe. Available online: https://www.alzheimer-europe.org/Publications/Dementia-in-Europe-Yearbooks (accessed on 10 August 2020).
- Fick, D.M.; Agostini, J.V.; Inouye, S.K. Delirium superimposed on dementia: A systematic review. J. Am. Geriatr. Soc. 2002, 50, 1723–1732. [Google Scholar] [CrossRef]
- Reynish, E.; Hapca, S.M.; De Souza, N.; Cvoro, V.; Donnan, P.T.; Guthrie, B. Epidemiology and outcomes of people with dementia, delirium, and unspecified cognitive impairment in the general hospital: Prospective cohort study of 10,014 admissions. BMC Med. 2017, 15, 140. [Google Scholar] [CrossRef]
- Leslie, D.L.; Marcantonio, E.R.; Zhang, Y.; Leo-Summers, L.; Inouye, S.K. One-year health care costs associated with delirium in the elderly population. Arch. Intern. Med. 2008, 168, 27–32. [Google Scholar] [CrossRef]
- Marcantonio, E.R.; Flacker, J.M.; Wright, R.J.; Resnick, N.M. Reducing delirium after hip fracture: A randomized trial. J. Am. Geriatr. Soc. 2001, 49, 516–522. [Google Scholar] [CrossRef]
- Inouye, S.K.; Bogardus, S.T.; Charpentier, P.A.; Leo-Summers, L.; Acampora, D.; Holford, T.R.; Cooney, L.M. A multicomponent intervention to prevent delirium in hospitalized older patients. N. Engl. J. Med. 1999, 340, 669–676. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Available online: https://www.who.int/classifications/icd/en/bluebook.pdf (accessed on 10 August 2020).
- Stępień, A. Neurologia; Medical Tribune Polska: Warsaw, Poland, 2014; pp. 591–620. (In Polish) [Google Scholar]
- Salardini, A. An overview of primary dementias as clinicopathological entities. Semin. Neurol. 2019, 39, 153–166. [Google Scholar] [CrossRef] [PubMed]
- Bright, F.M.; Werry, E.L.; Dobson-Stone, C.; Piguet, O.; Ittner, L.M.; Halliday, G.M.; Hodges, J.R.; Kiernan, M.C.; Loy, C.T.; Kassiou, M.; et al. Neuroinflammation in frontotemporal dementia. Nat. Rev. Neurol. 2019, 15, 540–555. [Google Scholar] [PubMed]
- Block, M.L.; Hong, J.S. Microglia and inflammation-mediated neurodegeneration: Multiple triggers with a common mechanism. Prog. Neurobiol. 2005, 76, 77–98. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.; Liu, J.; Xu, C.; Keblesh, J.; Zang, W.; Xiong, H. HIV-1gp120 induces neuronal apoptosis through enhancement of 4-aminopyridine-senstive outward K+ currents. PLoS ONE 2011, 6, e25994. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, J.R. Acute brain failure: Pathophysiology, diagnosis, management, and sequelae of delirium. Crit. Care Clin. 2017, 33, 461–519. [Google Scholar] [CrossRef]
- Van der Mast, R.C. Pathophysiology of delirium. J. Geriatr. Psychiatry Neurol. 1998, 11, 138–145. [Google Scholar] [CrossRef]
- Inouye, S.K. Delirium in hospitalized older patients: Recognition and risk factors. J. Geriatr. Psychiatry Neurol. 1998, 11, 118–158. [Google Scholar] [CrossRef]
- Elie, M.; Cole, M.G.; Primeau, F.J.; Bellavance, F. Delirium risk factors in elderly hospitalized patients. J. Gen. Intern. Med. 1998, 13, 204–212. [Google Scholar] [CrossRef]
- Kennedy, M.; Ms, R.A.E.; Bs, S.P.T.; Wolfe, R.E.; Shapiro, N.I.; Marcantonio, E.R. Delirium risk prediction, healthcare use and mortality of elderly adults in the emergency department. J. Am. Geriatr. Soc. 2014, 62, 462–469. [Google Scholar] [CrossRef]
- Maldonado, J.R. Delirium in the acute care setting: Characteristics, diagnosis and treatment. Crit. Care Clin. 2008, 24, 657–722. [Google Scholar] [PubMed]
- Inouye, S.K. Predisposing and precipitating factors for delirium in hospitalized older patients. Dement. Geriatr. Cogn. Disord. 1999, 10, 393–400. [Google Scholar] [CrossRef] [PubMed]
- Han, J.H.; Suyama, J. Delirium and dementia. Clin. Geriatr. Med. 2018, 34, 327–354. [Google Scholar] [CrossRef] [PubMed]
- Maldonado, J.R. Delirium pathophysiology: An updated hypothesis of the etiology of acute brain failure. Int. J. Geriatr. Psychiatry 2018, 33, 1428–1457. [Google Scholar] [PubMed]
- Han, L.; McCusker, J.; Cole, M.; Abrahamowicz, M.; Primeau, F.; Élie, M. Use of medications with anticholinergic effect predicts clinical severity of delirium symptoms in older medical inpatients. Arch. Intern. Med. 2001, 161, 1099–1105. [Google Scholar] [CrossRef]
- Cancelli, I.; Beltrame, M.; Gigli, G.L.; Valente, M. Drugs with anticholinergic properties: Cognitive and neuropsychiatric side-effects in elderly patients. Neurol. Sci. 2009, 30, 87–92. [Google Scholar] [CrossRef]
- Gibson, G.E.; Blass, J.P.; Huang, H.M.; Freeman, G.B. The cellular basis of delirium and its relevance to age-related disorders including Alzheimer’s disease. Int. Psychogeriatr. 1991, 3, 373–395. [Google Scholar] [CrossRef]
- Ramírez-Bermúdez, J.; Perez-Neri, I.; Montes, S.; Nente, F.; Ramirez-Abascal, M.; Carrillo-Mezo, R.; Pérez-Esparza, R.; Soto-Hernandez, J.L.; Espinola-Nadurille, M.; Bayliss, L.; et al. Dopaminergic hyperactivity in neurological patients with delirium. Arch. Med. Res. 2019, 50, 477–483. [Google Scholar] [CrossRef]
- Steiner, L.A. Postoperative delirium. Part 1: Pathophysiology and risk factors. Eur. J. Anaesthesiol. 2011, 28, 628–636. [Google Scholar] [CrossRef]
- Trzepacz, P.T. Is there a final common neural pathway in delirium? Focus on acetylcholine and dopamine. Semin. Clin. Neuropsychiatry 2000, 5, 132–148. [Google Scholar]
- Zaal, I.J.; Slooter, A.J.C. Delirium in critically Ill patients. Drugs 2012, 72, 1457–1471. [Google Scholar] [CrossRef] [PubMed]
- Riker, R.R.; Shehabi, Y.; Bokesch, P.M.; Ceraso, D.; Wisemandle, W.; Koura, F.; Whitten, P.; Margolis, B.D.; Byrne, D.W.; Ely, E.W.; et al. Dexmedetomidine vs midazolam for sedation of critically ill patients: A randomized trial. JAMA 2009, 301, 489–499. [Google Scholar] [CrossRef] [PubMed]
- Pandharipande, P.P.; Shintani, A.; Peterson, J.; Pun, B.T.; Wilkinson, G.R.; Dittus, R.S.; Bernard, G.R.; Ely, E.W. Lorazepam is an independent risk factor for transitioning to delirium in intensive care unit patients. Anesthesiology 2006, 104, 21–26. [Google Scholar] [PubMed]
- Coleman, P.D.; Flood, D.G. Neuron numbers and dendritic extent in normal aging and Alzheimer’s disease. Neurobiol. Aging. 1987, 8, 521–545. [Google Scholar] [CrossRef]
- Gibon, E.; Lu, L.; Goodman, S.B. Aging, inflammation, stem cells, and bone healing. Stem Cell Res. Ther. 2016, 7, 44. [Google Scholar]
- Liochev, S.I. Reactive oxygen species and the free radical theory of aging. Free Radic. Biol. Med. 2013, 60, 1–4. [Google Scholar] [CrossRef]
- Van Gool, W.A.; van de Beek, D.; Eikelenboom, P. Systemic infection and delirium: When cytokines and acetylcholine collide. Lancet 2010, 375, 773–775. [Google Scholar] [CrossRef]
- Maldonado, J.R. Neuropathogenesis of delirium: Review of current etiologic theories and common pathways. Am. J. Geriatr. Psychiatry 2013, 21, 1190–1222. [Google Scholar]
- Maldonado, J.R. Pathoetiological model of delirium: A comprehensive understanding of the neurobiology of delirium and an evidence-based approach to prevention and treatment. Crit. Care Clin. 2008, 24, 789–856. [Google Scholar] [CrossRef]
- Boogaard, M.V.D.; Kox, M.; Quinn, K.L.; van Achterberg, T.; van der Hoeven, J.G.; Schoonhoven, L.; Pickkers, P. Biomarkers associated with delirium in critically ill patients and their relation with long-term subjective cognitive dysfunction; indications for different pathways governing delirium in inflamed and noninflamed patients. Crit. Care 2011, 15, R297. [Google Scholar] [CrossRef]
- De Rooij, S.E.; van Munster, B.C.; Korevaar, J.C.; Levi, M. Cytokines and acute phase response in delirium. J. Psychosom. Res. 2007, 62, 521–525. [Google Scholar] [PubMed]
- Simone, M.J.; Tan, Z.S. The role of inflammation in the pathogenesis of delirium and dementia in older adults: A review. CNS Neurosci. Ther. 2011, 17, 506–513. [Google Scholar] [PubMed]
- Karlidag, R.; Unal, S.; Sezer, O.H.; Karabulut, A.B.; Battaloğlu, B.; But, A.; Ozcan, C. The role of oxidative stress in postoperative delirium. Gen. Hosp. Psychiatry 2006, 28, 418–423. [Google Scholar] [CrossRef]
- Cerejeira, J.; Mukaetova-Ladinska, E.B. A clinical update on delirium: From early recognition to effective management. Nurs. Res. Pract. 2011, 2011, 1–12. [Google Scholar]
- Han, J.H.; Zimmerman, E.E.; Cutler, N.; Schnelle, J.; Morandi, A.; Dittus, R.S.; Storrow, A.B.; Ely, E.W. Delirium in older emergency department patients: Recognition, risk factors, and psychomotor subtypes. Acad. Emerg. Med. 2009, 16, 193–200. [Google Scholar] [CrossRef] [PubMed]
- Fujishiro, H.; Kawakami, I.; Oshima, K.; Niizato, K.; Iritani, S. Delirium prior to dementia as a clinical phenotype of Lewy body disease: An autopsied case report. Int. Psychogeriatr. 2017, 29, 687–689. [Google Scholar] [CrossRef] [PubMed]
- McNicoll, L.; Pisani, M.A.; Zhang, Y.; Ely, E.W.; Siegel, M.D.; Inouye, S.K. Delirium in the intensive care unit: Occurrence and clinical course in older patients. J. Am. Geriatr. Soc. 2003, 51, 591–598. [Google Scholar] [CrossRef] [PubMed]
- Calderón, J.; Perry, R.; Erzinclioglu, S.; Berrios, G.; Dening, T.; Hodges, J. Perception, attention, and working memory are disproportionately impaired in dementia with Lewy bodies compared with Alzheimer’s disease. J. Neurol. Neurosurg. Psychiatry 2001, 70, 157–164. [Google Scholar]
- Plum, F.; Posner, J.B. The diagnosis of stupor and coma. Contemp. Neurol. Ser. 1972, 10, 1–286. [Google Scholar]
- Brown, L.J.; Fordyce, C.; Zaghdani, H.; Starr, J.M.; MacLullich, P.A.M.J. Detecting deficits of sustained visual attention in delirium. J. Neurol. Neurosurg. Psychiatry 2011, 82, 1334–1340. [Google Scholar] [CrossRef]
- Morandi, A.; Davis, D.; Bellelli, G.; Arora, R.C.; Caplan, G.A.; Kamholz, B.; Kolanowski, A.; Fick, D.M.; Kreisel, S.; MacLullich, A.; et al. The diagnosis of delirium superimposed on dementia: An emerging challenge. J. Am. Med. Dir. Assoc. 2017, 18, 12–18. [Google Scholar] [CrossRef] [PubMed]
- Khachiyants, N.; Trinkle, D.; Son, S.J.; Kim, K.Y. Sundown syndrome in persons with dementia: An update. Psychiatry Investig. 2011, 8, 275–287. [Google Scholar] [PubMed]
- Parrish, E. Delirium superimposed on dementia: Challenges and opportunities. Nurs. Clin. N. Am. 2019, 54, 541–550. [Google Scholar] [CrossRef] [PubMed]
- Brooke, J. Differentiation of delirium, dementia and delirium superimposed on dementia in the older person. Br. J. Nurs. 2018, 27, 363–367. [Google Scholar] [CrossRef]
- Levkoff, S.E.; Liptzin, B.; Cleary, P.D.; Wetle, T.; Evans, D.A.; Rowe, J.W.; Lipsitz, L.A. Subsyndromal delirium. Am. J. Geriatr. Psychiatry 1996, 4, 320–329. [Google Scholar] [CrossRef]
- Inouye, S.K.; Foreman, M.D.; Mion, L.C.; Katz, K.H.; Cooney, J.L.M. Nurses’ recognition of delirium and its symptoms: Comparison of nurse and researcher ratings. Arch. Intern. Med. 2001, 161, 2467–2473. [Google Scholar] [CrossRef]
- Meagher, D. Motor subtypes of delirium: Past, present and future. Int. Rev. Psychiatry 2009, 21, 59–73. [Google Scholar]
- Peritogiannis, V.; Bolosi, M.; Lixouriotis, C.; Rizos, D.V. Recent insights on prevalence and correlations of hypoactive delirium. Behav. Neurol. 2015, 416792. [Google Scholar]
- Robinson, T.N.; Raeburn, C.D.; Tran, Z.V.; Brenner, L.A.; Moss, M. Motor subtypes of postoperative delirium in older adults. Arch. Surg. 2011, 146, 295–300. [Google Scholar] [CrossRef]
- Kim, S.-Y.; Kim, S.-W.; Kim, J.-M.; Shin, I.-S.; Bae, K.-Y.; Shim, H.-J.; Bae, W.-K.; Cho, S.; Chung, I.; Yoon, J.-S. Differential associations between delirium and mortality according to delirium subtype and age: A prospective cohort study. Psychosom. Med. 2015, 77, 903–910. [Google Scholar] [CrossRef]
- Hosker, C.; Ward, D. Hypoactive delirium. BMJ 2017, 357, 2047. [Google Scholar] [CrossRef] [PubMed]
- Inouye, S.K.; Van Dyck, C.H.; Alessi, C.A.; Balkin, S.; Siegal, A.P.; Horwitz, R.I. Clarifying confusion: The confusion assessment method. A new method for detection of delirium. Ann. Intern. Med. 1990, 113, 941–948. [Google Scholar] [CrossRef] [PubMed]
- Carpenter, C.R.; Bassett, E.R.; Fischer, G.M.; Shirshekan, J.; Galvin, J.E.; Morris, J.C. Four sensitive screening tools to detect cognitive dysfunction in geriatric emergency department patients: Brief alzheimer’s screen, short blessed test, Ottawa 3DY, and the caregiver-completed AD8. Acad. Emerg. Med. 2011, 18, 374–384. [Google Scholar] [PubMed]
- Proicu. Available online: http://proicu.pl/images/pdf/CAMICU_Training_Manual_Polish_Nov2015.pdf (accessed on 15 August 2020). (In Polish).
- Tieges, Z.; Brown, L.J.; MacLullich, A.M. Objective assessment of attention in delirium: A narrative review. Int. J. Geriatr. Psychiatry 2014, 29, 1185–1197. [Google Scholar] [CrossRef]
- Adamis, D.; Meagher, D.; Murray, O.; O’Neill, D.; O’Mahony, E.; Mulligan, O.; McCarthy, G. Evaluating attention in delirium: A comparison of bedside tests of attention. Geriatr. Gerontol. Int. 2016, 16, 1028–1035. [Google Scholar] [CrossRef]
- Hospital Elder Life Program. Available online: https://www.hospitalelderlifeprogram.org/uploads/disclaimers/Long_CAM_Training_Manual_10-9-14.pdf (accessed on 15 August 2020).
- Bellelli, G.; Morandi, A.; Davis, D.H.; Mazzola, P.; Turco, R.; Gentile, S.; Ryan, T.; Cash, H.; Guerini, F.; Torpilliesi, T.; et al. Validation of the 4AT, a new instrument for rapid delirium screening: A study in 234 hospitalised older people. Age Ageing 2014, 43, 496–502. [Google Scholar] [CrossRef]
- O’Keeffe, S.T.; Gosney, M.A. Assessing attentiveness in older hospital patients: Global assessment versus tests of attention. J. Am. Geriatr. Soc. 1997, 45, 470–473. [Google Scholar] [CrossRef]
- Bellelli, G.; Speciale, S.; Morghen, S.; Torpilliesi, T.; Turco, R.; Trabucchi, M. Are fluctuations in motor performance a diagnostic sign of delirium? J. Am. Med. Dir. Assoc. 2011, 12, 578–583. [Google Scholar] [CrossRef]
- Walker, M.P.; Ayre, G.A.; Cummings, J.L.; Wesnes, K.; McKeith, I.G.; O’Brien, J.T.; Ballard, C.G. Quantifying fluctuation in dementia with Lewy bodies, Alzheimer’s disease, and vascular dementia. Neurology 2000, 54, 1616–1625. [Google Scholar] [CrossRef]
- Gomperts, S.N. Lewy body dementias: Dementia with lewy bodies and parkinson disease dementia. Contin. Minneap Minn. 2016, 22, 435–463. [Google Scholar] [CrossRef]
- Oh, E.S.; Fong, T.G.; Hshieh, T.T.; Inouye, S.K. Delirium in older persons: Advances in diagnosis and treatment. JAMA 2017, 318, 1161–1174. [Google Scholar] [CrossRef] [PubMed]
- Lane, C.A.; Hardy, J.; Schott, J.M. Alzheimer’s disease. Eur. J. Neurol. 2018, 25, 59–70. [Google Scholar] [CrossRef] [PubMed]
- Louis, E.; Mayer, S.; Rowland, L. Merrit Neurologia—Tom 1. Edycja Polska pod Redakcją Wojciecha Turaja; Edra Urban & Partner: Wrocław, Poland, 2017; pp. 446–480. (In Polish) [Google Scholar]
- Tisher, A.; Salardini, A. A comprehensive update on treatment of dementia. Semin. Neurol. 2019, 39, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2012/020690s035,021720s008,022568s005lbl.pdf (accessed on 20 August 2020).
- Food and Drug Administration. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/nda/2000/20823_Exelon_prntlbl.pdf (accessed on 20 August 2020).
- Food and Drug Administration. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/021169Orig1s032,021224Orig1s030,021615Orig1s023lbl.pdf (accessed on 20 August 2020).
- Galimberti, D.; Scarpini, E. Old and new acetylcholinesterase inhibitors for Alzheimer’s disease. Expert Opin. Investig. Drugs 2016, 25, 1181–1187. [Google Scholar] [CrossRef]
- Malone, K.; Hancox, J.C. QT interval prolongation and Torsades de Pointes with donepezil, rivastigmine and galantamine. Ther. Adv. Drug Saf. 2020, 11, 2042098620942416. [Google Scholar] [CrossRef]
- Sönnerstam, E.; Sjölander, M.; Lövheim, H.; Gustafsson, M. Clinically relevant drug-drug interactions among elderly people with dementia. Eur. J. Clin. Pharmacol. 2018, 74, 1351–1360. [Google Scholar] [CrossRef]
- Marra, A.; Ely, E.W.; Pandharipande, P.P.; Patel, M.B. The ABCDEF bundle in critical care. Crit. Care Clin. 2017, 33, 225–243. [Google Scholar] [CrossRef]
- Jann, M.W.; Shirley, K.L.; Small, G.W.; Jann, M.W. Clinical pharmacokinetics and pharmacodynamics of cholinesterase inhibitors. Clin. Pharmacokinet. 2002, 41, 719–739. [Google Scholar] [CrossRef]
- Ferreira-Valente, A.; Pais-Ribeiro, J.L.; Jensen, M.P. Validity of four pain intensity rating scales. Pain 2011, 152, 2399–2404. [Google Scholar] [CrossRef]
- Crismon, M.L. Pharmacokinetics and drug interactions of cholinesterase inhibitors administered in Alzheimer’s disease. Pharmacotherapy 1998, 18, 47–82. [Google Scholar]
- Defilippi, J.L.; Crismon, M.L. Drug interactions with cholinesterase inhibitors. Drugs Aging 2003, 20, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration. Available online: https://www.accessdata.fda.gov/drugsatfda_docs/label/2013/021487s010s012s014,021627s008lbl.pdf (accessed on 20 August 2020).
- Jarvis, B.; Figgitt, D.P. Memantine. Drugs Aging 2003, 20, 465–478. [Google Scholar] [CrossRef] [PubMed]
- Inouye, S.K. Prevention of delirium in hospitalized older patients: Risk factors and targeted intervention strategies. Ann. Med. 2000, 32, 257–263. [Google Scholar] [CrossRef] [PubMed]
- National Center for Biotechnology Information. Available online: https://www.ncbi.nlm.nih.gov/books/NBK551003/ (accessed on 28 August 2020).
- Devlin, J.W.; Skrobik, Y.; Gélinas, C.; Needham, D.M.; Slooter, A.J.C.; Pandharipande, P.P.; Watson, P.L.; Weinhouse, G.L.; Nunnally, M.E.; Rochwerg, B.; et al. Clinical practice guidelines for the prevention and management of pain, agitation/sedation, delirium, immobility, and sleep disruption in adult patients in the ICU. Crit. Care Med. 2018, 46, e825–e873. [Google Scholar] [PubMed]
- Vincent, J.-L.; Shehabi, Y.; Walsh, T.S.; Pandharipande, P.P.; Ball, J.A.; Spronk, P.; Longrois, D.; Strøm, T.; Conti, G.; Funk, G.-C.; et al. Comfort and patient-centred care without excessive sedation: The eCASH concept. Intensive Care Med. 2016, 42, 962–971. [Google Scholar]
- Hsu, W.-H.; Wen, Y.-W.; Chen, L.-K.; Hsiao, F.-Y. Comparative associations between measures of anti-cholinergic burden and adverse clinical outcomes. Ann. Fam. Med. 2017, 15, 561–569. [Google Scholar] [CrossRef]
- Campbell, N.; Boustani, M.A.; Lane, K.A.; Gao, S.; Hendrie, H.; Khan, B.A.; Murrell, J.R.; Unverzagt, F.W.; Hake, A.; Smith-Gamble, V.; et al. Use of anticholinergics and the risk of cognitive impairment in an African-American population. Neurology 2010, 75, 152–159. [Google Scholar] [CrossRef]
- Fox, C.; Richardson, K.; Maidment, I.D.; Savva, G.M.; Matthews, F.E.; Smithard, D.; Coulton, S.; Katona, C.; Boustani, M.; Brayne, C. Anticholinergic medication use and cognitive impairment in the older population: The medical research council cognitive function and ageing study. J. Am. Geriatr. Soc. 2011, 59, 1477–1483. [Google Scholar] [CrossRef]
- NHS Milton Keynes Clinical Commissioning Group. Available online: http://www.miltonkeynesccg.nhs.uk/resources/uploads/ACB_scale_-_legal_size.pdf (accessed on 12 August 2020).
- Van Rompaey, B.; Elseviers, M.M.; Van Drom, W.; Fromont, V.; Jorens, P.G. The effect of earplugs during the night on the onset of delirium and sleep perception: A randomized controlled trial in intensive care patients. Crit. Care 2012, 16, R73. [Google Scholar] [CrossRef]
- Kress, J.P.; Pohlman, A.S.; O’Connor, M.F.; Hall, J.B. Daily interruption of sedative infusions in critically ill patients undergoing mechanical ventilation. N. Engl. J. Med. 2000, 342, 1471–1477. [Google Scholar] [CrossRef]
- Shehabi, Y.; Bellomo, R.; Reade, M.C.; Bailey, M.; Bass, F.; Howe, B.; McArthur, C.; Seppelt, I.M.; Webb, S.; Weisbrodt, L.; et al. Early intensive care sedation predicts long-term mortality in ventilated critically ill patients. Am. J. Respir. Crit. Care Med. 2012, 186, 724–731. [Google Scholar] [CrossRef] [PubMed]
- Vagionas, D.; Vasileiadis, I.; Rovina, N.; Alevrakis, E.; Koutsoukou, A.; Koulouris, N. Daily sedation interruption and mechanical ventilation weaning: A literature review. Anaesthesiol. Intensive Ther. 2019, 51, 380–389. [Google Scholar] [PubMed]
- Jakob, S.M.; Ruokonen, E.; Grounds, R.M.; Sarapohja, T.; Garratt, C.; Pocock, S.J.; Bratty, J.R.; Takala, J. Dexmedetomidine vs midazolam or propofol for sedation during prolonged mechanical ventilation: Two randomized controlled trials. JAMA 2012, 307, 1151–1160. [Google Scholar] [CrossRef] [PubMed]
- Pluta, M.P.; Dziech, M.; Czempik, P.F.; Szczepańska, A.J.; Krzych, L. Antipsychotic drugs in prevention of postoperative delirium-what is known in 2020? Int. J. Environ. Res. Public Health. 2020, 17, 6069. [Google Scholar] [CrossRef]
- Le Guen, M.; Nicolas-Robin, A.; LeBard, C.; Arnulf, I.; Langeron, O. Earplugs and eye masks vs routine care prevent sleep impairment in post-anaesthesia care unit: A randomized study. Br. J. Anaesth. 2014, 112, 89–95. [Google Scholar] [CrossRef]
- Schweickert, W.D.; Pohlman, M.C.; Pohlman, A.S.; Nigos, C.; Pawlik, A.J.; Esbrook, C.L.; Spears, L.; Miller, M.; Franczyk, M.; Deprizio, D.; et al. Early physical and occupational therapy in mechanically ventilated, critically ill patients: A randomised controlled trial. Lancet 2009, 373, 1874–1882. [Google Scholar]
| Vulnerability Factors | Precipitating Factors |
|---|---|
| Demographics male gender age ≥ 65 years old educational background | Severe illness infection, sepsis inadequate pain control trauma hypo- or hyperthermia |
| Comorbidity dementia chronic kidney disease endstage liver disease terminal illness | CNS illness intracerebral hemorrhage cerebrovascular accident meningitis/encephalitis nonconvulsive status epilepticus cerebral edema tumor hydrocephalus |
| Functional status immobility visual impairment hearing impairment | Metabolic disorder thiamine deficiency renal failure liver failure electrolyte imbalance hypo- or hyperglycemia thyroid dysfunction glucocorticoid therapy hypophysis disfunction porphyria |
| Baseline medication usage polypharmacy baseline psychoactive medication and drug use * substance withdrawal | Cardiorespiratory acute coronary disease congestive cardiac failure hypoxemia hypercarbia shock hypertensive encephalopathy |
| Malnutrition & dehydration | Mobility restriction use of physical restraints use of bladder catheters intubation assisted ventilation use of vascular catheters intermittent pneumatic compression orthopedic cast |
| Depression | Other malignant hyperthermia serotonin syndrome malignant catatonia paraneoplastic syndrome >3 medications added anti-NMDA(N-methyl-d-aspartate) encephalitis any iatrogenic event drugs and medications taken |
| Circadian rhythm disruption |
| Feature | Delirium | Dementia |
|---|---|---|
| Onset | Sudden—hours/days | Insidious and slow |
| Cause | Other medical emergency | Baseline CNS disease—neurodegenerative or other |
| Course | Can be short if treated; usually reversible | Progressive—treatment slows the progression |
| Attention | Impaired initially | Usually preserved; may be impaired in advanced stages |
| Orientation | Impaired initially | Usually preserved; may be impaired in advanced stages |
| Memory | Impaired initially; may be unable to recall the incident | Initially lost of short-term memory; degree of memory loss increases as the disease progresses |
| Behaviour | Agitated/somnolent | Usually normal; may become agitated in advanced stages |
| Perceptual Disturbances | Visual hallucinations; misperceptions; illusions | Hallucinations and misperceptions may occur mostly in DLB |
| Feature | Hypoactive | Hyperactive |
|---|---|---|
| Arousal | Decreased arousal and alertness; somnolence; reduced awareness | Hypervigilant; easily startled; distractable |
| Mood | Depressed, irritable; mood swings; patient is disinhibited | Labile: from comative to euphoric |
| Psychomotor activity | Slow, quiet, withdrawn | Restless, agitated, combative, irritable |
| Past psychiatric history | May have experienced delirium before | Correlated with alcohol or drug withdrawal; may have experienced delirium before |
| Circadian rythm | Increased daytime sleepiness | Prominent disturbances; nightmares and night terrors |
| Disease | Diagnostic Method | |
|---|---|---|
| CNS | stroke, trauma brain injury, subsclerotic haemorrhage | CT/MRI |
| Non-convulsive status epilepsy, partial epileptic seizure with cognitive decline | EEG | |
| Cardiovascular System | Acute coronary syndrome | ECG, Troponin, CK-MB |
| Atrial fibrillation | ECG | |
| Abdominal aortic aneurysm | Abdominal ultrasound, CT, MRI | |
| Respiratory System | Pulmonary embolism | CT, angiography of pulmonary vessels, ventilation/perfusion scintigraphy |
| Pulmonary oedema | Chest radiograph | |
| Metabolic Disturbances | Hypermetabolic crisis, myxoedema | TSH, fT4 |
| Diabetes mellitus—keto alkalosis Hyperosmolar Hyperglycaemic Nonketotic Syndrome (HHNS) | Glycaemia measurement | |
| Acid-Base balance disturbances | Arterial blood gas | |
| Electrolyte balance disturbances; dehydration | Plasma electrolytes measurement | |
| Hematologic Disturbances | Acute blood loss | Blood morphology evaluation |
| Medication | benzodiazepines, antipsychotics, opioids, sedation drugs, anticholinergic drugs | Drug level in blood/urine |
| Other | Sleep deprivation, psychosis, depression | Psychiatric evaluation |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Krzych, Ł.J.; Rachfalska, N.; Putowski, Z. Delirium Superimposed on Dementia in Perioperative Period and Intensive Care. J. Clin. Med. 2020, 9, 3279. https://doi.org/10.3390/jcm9103279
Krzych ŁJ, Rachfalska N, Putowski Z. Delirium Superimposed on Dementia in Perioperative Period and Intensive Care. Journal of Clinical Medicine. 2020; 9(10):3279. https://doi.org/10.3390/jcm9103279
Chicago/Turabian StyleKrzych, Łukasz J., Natalia Rachfalska, and Zbigniew Putowski. 2020. "Delirium Superimposed on Dementia in Perioperative Period and Intensive Care" Journal of Clinical Medicine 9, no. 10: 3279. https://doi.org/10.3390/jcm9103279
APA StyleKrzych, Ł. J., Rachfalska, N., & Putowski, Z. (2020). Delirium Superimposed on Dementia in Perioperative Period and Intensive Care. Journal of Clinical Medicine, 9(10), 3279. https://doi.org/10.3390/jcm9103279






