Clinical Behavior of Short Dental Implants: Systematic Review and Meta-Analysis
Abstract
1. Introduction
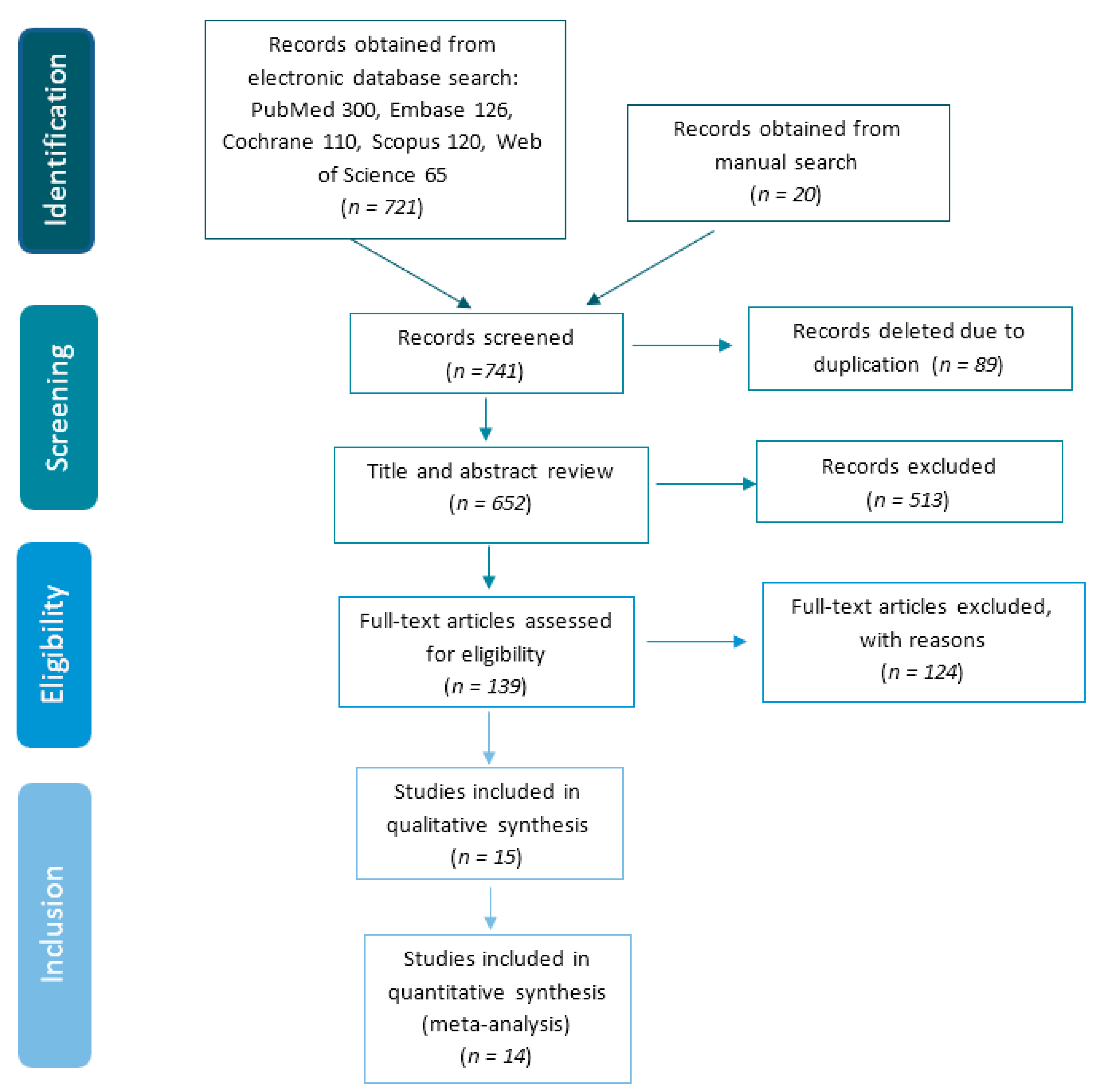
2. Materials and Methods
3. Results
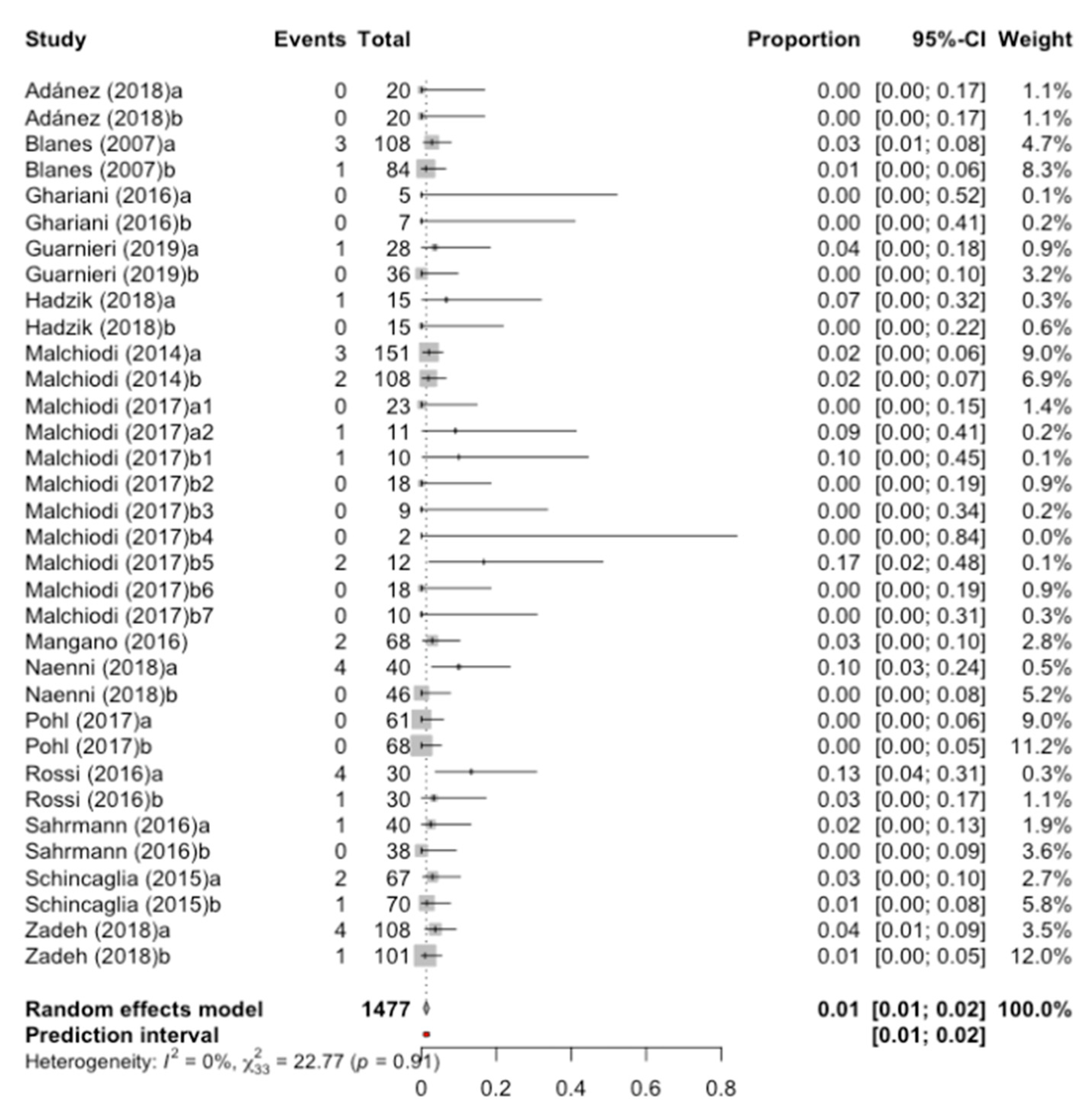
3.1. Percentage of Failure or Implant Loss
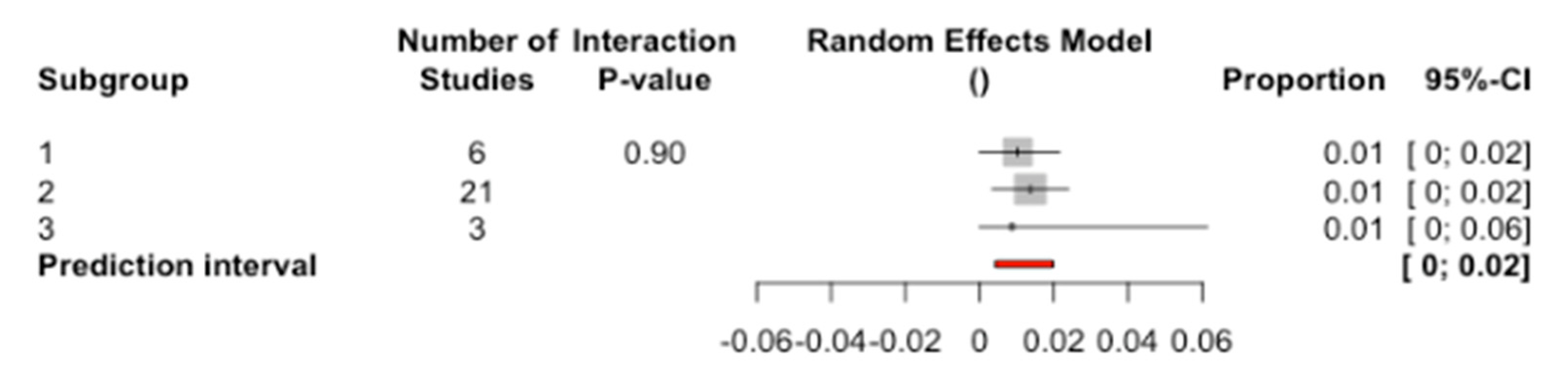
3.2. Analysis by Subgroups According to C/I Ratio
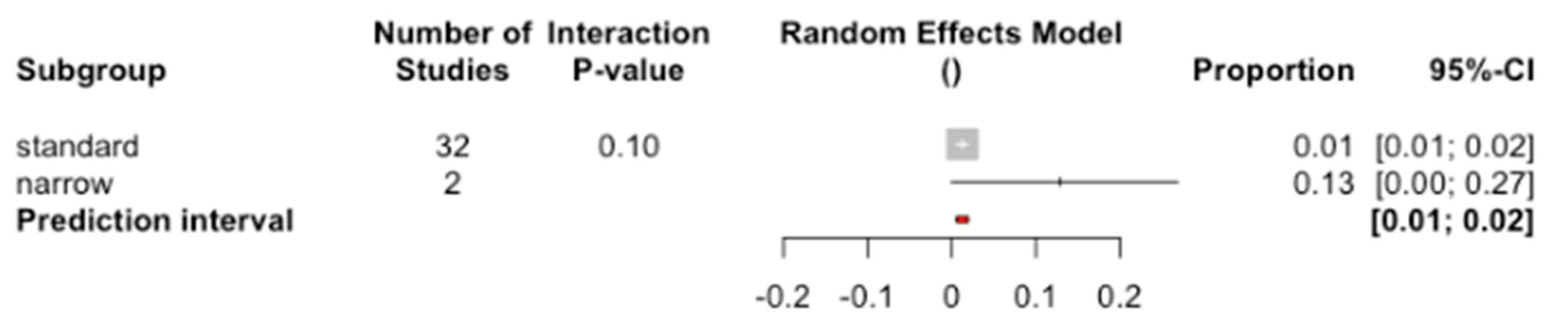
3.3. Analysis by Subgroups According to Diameter
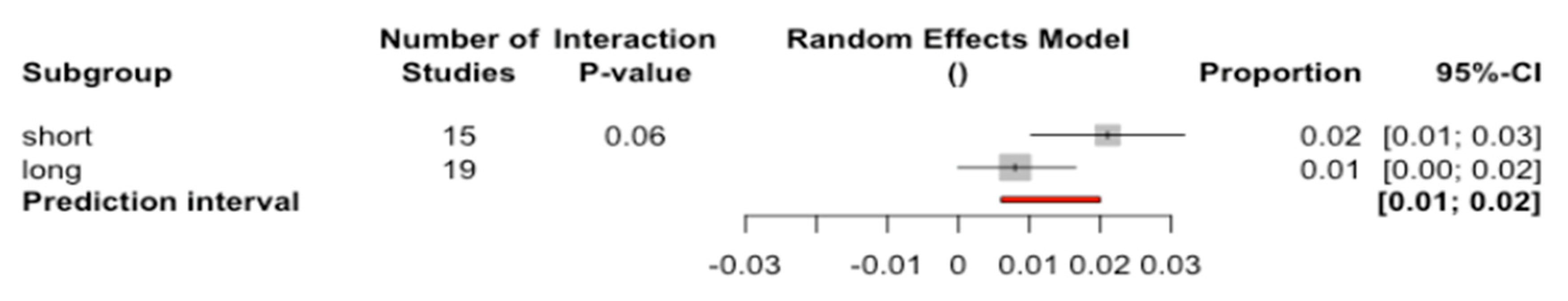
3.4. Analysis by Subgroups According to Length
3.5. Meta-Regression
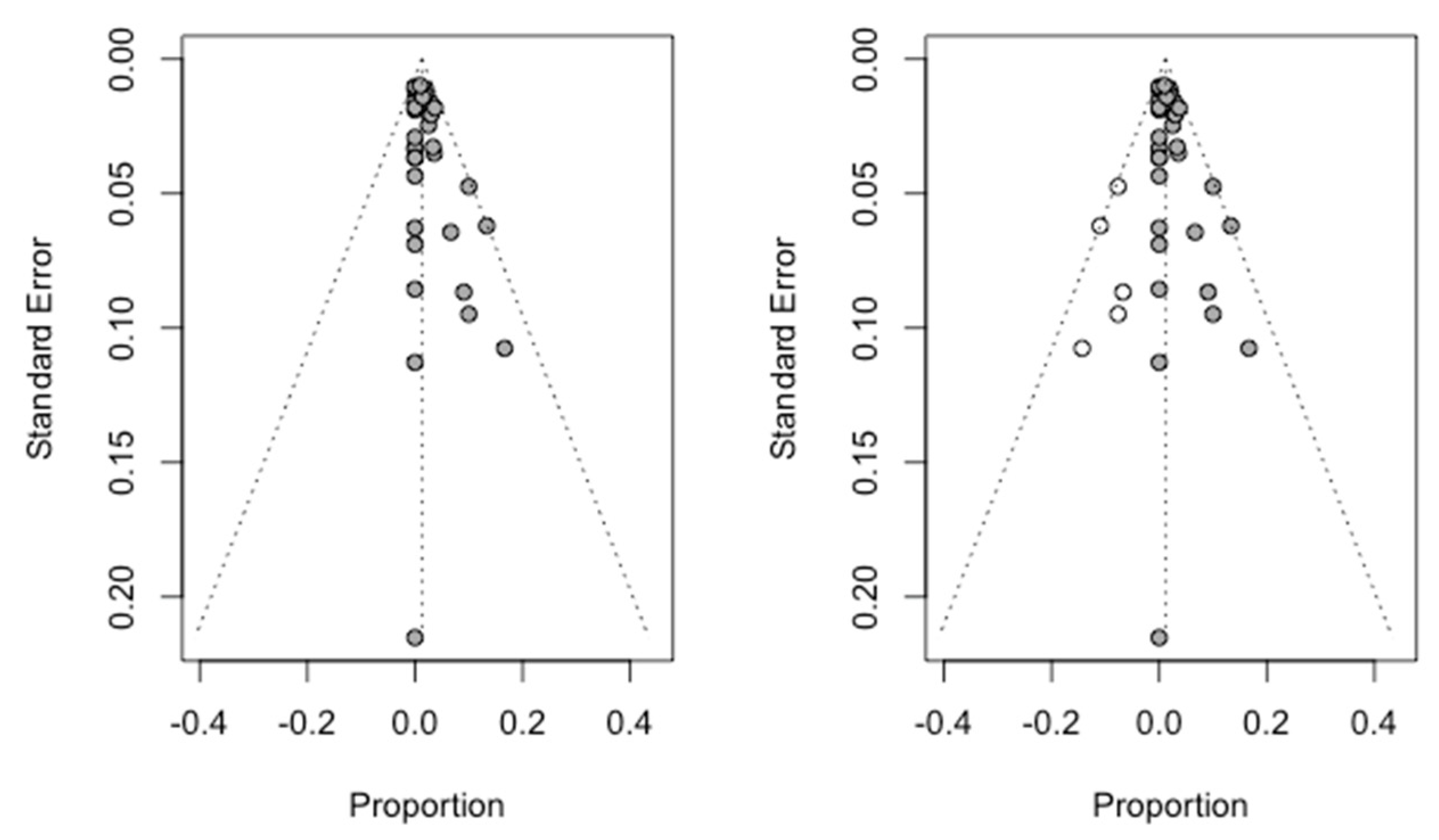
3.6. Publication Bias
3.7. Mean Marginal Bone Loss from the Implant
3.8. Analysis by Subgroups According to C/I ratio
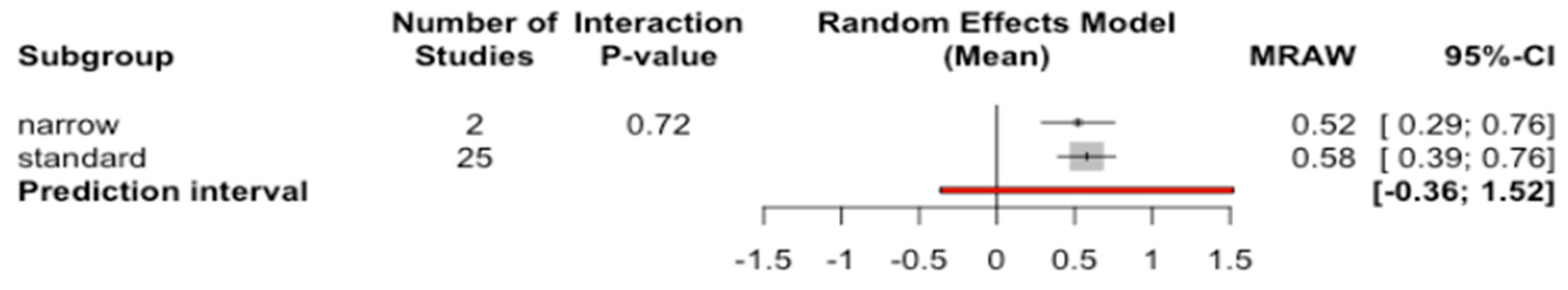
3.9. Analysis by Subgroups According to Diameter
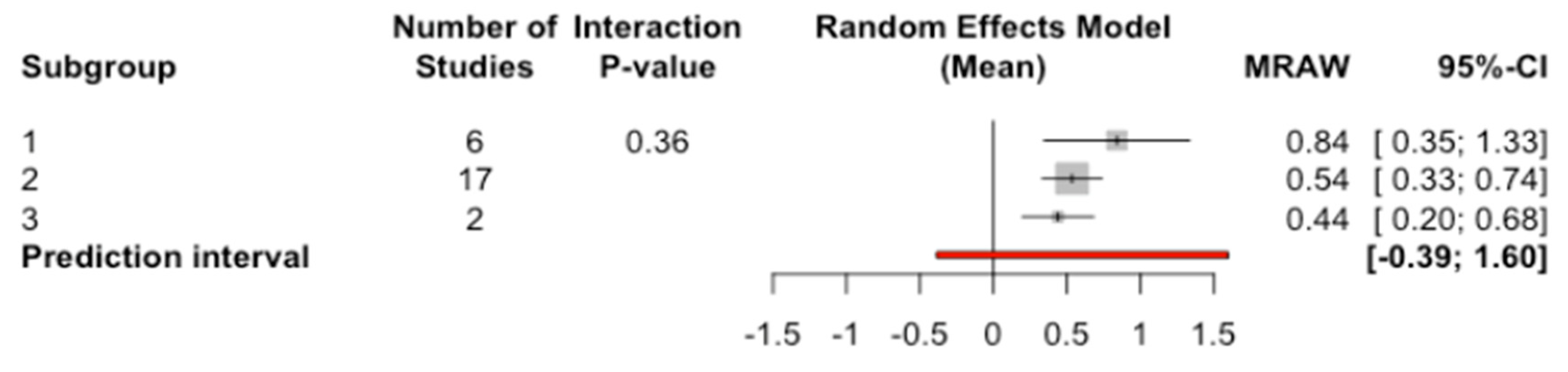
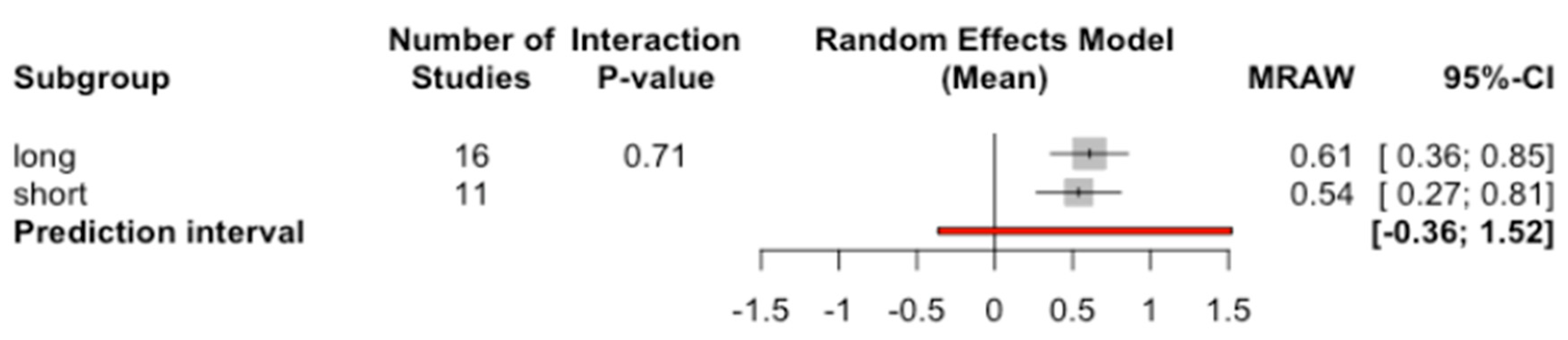
3.10. Analysis by Subgroups According to Length
3.11. Meta-Regression
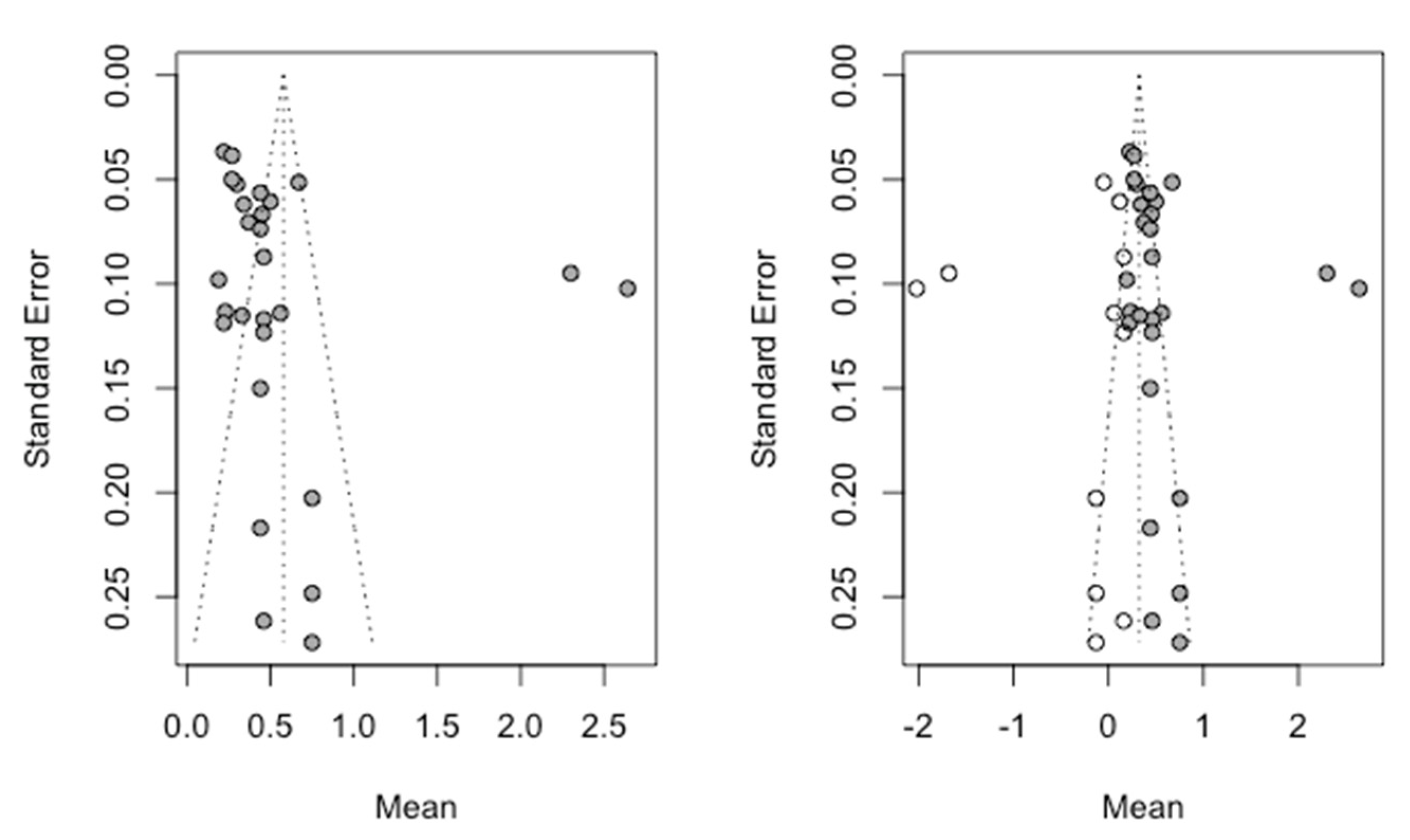
3.12. Publication Bias
4. Discussion
5. Conclusions
- -
- Short implants have a survival and bone loss rate similar to those of conventional length.
- -
- As for the parameter implant length, no statistical significance has been established in terms of its influence on bone or implant loss, but in the latter case (implant loss) a value close to statistical significance is evident.
- -
- The parameter implant diameter has not been established as statistically significant in terms of its influence on bone or implant loss.
- -
- Finally, the parameter crown/implant ratio of the implants has also not been established as being statistically significant in terms of its influence on bone or implant loss.
Author Contributions
Funding
Conflicts of Interest
References
- Lemos, C.A.A.; Ferro-Alves, M.L.; Okamoto, R.; Mendonça, M.R.; Pellizzer, E.P. Short dental implants versus standard dental implants placed in the posterior jaws: A systematic review and meta-analysis. J. Dent. 2016, 47, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Okada, S.; Koretake, K.; Miyamoto, Y.; Oue, H.; Akagawa, Y. Increased Crown-To-Implant Ratio May Not Be a Risk Factor for Dental Implant Failure under Appropriate Plaque Control. PLoS ONE 2013, 8, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Misch, C.E. Implantología Contemporánea, 3rd ed.; Elsevier: Barcelona, España, 2009. [Google Scholar]
- Atieh, M.A.; Zadeh, H.; Stanford, C.M.; Cooper, L.F. Survival of short dental implants for treatment of posterior partial edentulism: A systematic review. Int. J. Oral Maxillofac. Implant. 2012, 27, 1323–1331. [Google Scholar]
- Malchiodi, L.; Giacomazzi, E.; Cucchi, A.; Ricciotti, G.; Caricasulo, R.; Bertossi, D.; Gherlone, E. Relationship between crestal bone levels and crown-to-implant ratio of ultra-short implants with a microrough surface: A prospective study with 48 months of follow-up. J. Oral Implantol. 2019, 45, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Lombardo, G.; Pighi, J.; Marincola, M.; Corrocher, G.; Simancas-Pallares, M.; Nocini, P.F. Cumulative Success Rate of Short and Ultrashort Implants Supporting Single Crowns in the Posterior Maxilla: A 3-Year Retrospective Study. Int. J. Dent. 2017, 2017, 8434281. [Google Scholar] [CrossRef] [PubMed]
- Ali, S.A.; Karthigeyan, S.; Deivanai, M.; Kumar, A. Implant rehabilitation for atrophic maxilla: A review. J. Indian Prosthodont. Soc. 2014, 14, 196–207. [Google Scholar] [CrossRef] [PubMed]
- Misch, C.E.; Polido, W. A “Graft Less” Approach for Dental Implant Placement in Posterior Edentulous Sites. Int. J. Periodontics Restor. Dent. 2019, 39, 771–779. [Google Scholar] [CrossRef]
- Schwartz, S.R. Short Implants: Are They a Viable Option in Implant Dentistry? Dent. Clin. N. Am. 2015, 59, 317–328. [Google Scholar] [CrossRef]
- Nisand, D.; Renouard, F. Short implant in limited bone volume. Periodontology 2000 2014, 66, 72–96. [Google Scholar] [CrossRef]
- Benlidayi, M.E.; Ucar, Y.; Tatli, U.; Ekren, O.; Evlice, B.; Kisa, H.I.; Baksi, U. Short implants versus standard implants: Midterm outcomes of a clinical study. Implant. Dent. 2018, 27, 95–100. [Google Scholar] [CrossRef]
- Becerra-santos, G.; Becerra-moreno, N. Clinical considerations of the implants in posterior areas. CES Odontol. 2014, 27, 75–89. [Google Scholar]
- Al-Hashedi, A.A.; Ali, T.B.T.; Yunus, N. Short dental implants: An emerging concept in implant treatment. Quintessence Int. 2014, 45, 499–514. [Google Scholar] [PubMed]
- Neugebauer, J.; Nickenig, H.J.; Zöller, J.E. Guideline: Update on short, angulated and diameter-reduced implants. Eur. Assoc. Dent. Implantol. 2016, 1–9. [Google Scholar]
- Thoma, D.S.; Zeltner, M.; Hüsler, J.; Hämmerle, C.H.F.; Jung, R.E. EAO Supplement Working Group 4—EAO CC 2015 Short implants versus sinus lifting with longer implants to restore the posterior maxilla: A systematic review. Clin. Oral Implant. Res. 2015, 26, 154–169. [Google Scholar] [CrossRef] [PubMed]
- Fan, T.; Li, Y.; Deng, W.W.; Wu, T.; Zhang, W. Short Implants (5 to 8 mm) Versus Longer Implants (>8 mm) with Sinus Lifting in Atrophic Posterior Maxilla: A Meta-Analysis of RCTs. Clin. Implant. Dent. Relat. Res. 2017, 19, 207–215. [Google Scholar] [CrossRef]
- Hof, M.; Pommer, B.; Zukic, N.; Vasak, C.; Lorenzoni, M.; Zechner, W. Influence of prosthetic parameters on peri-implant bone resorption in the first year of loading: A multi-factorial analysis. Clin. Implant. Dent. Relat. Res. 2015, 17, 183–191. [Google Scholar] [CrossRef]
- Quaranta, A.; Piemontese, M.; Rappelli, G.; Sammartino, G.; Procaccini, M. Technical and biological complications related to crown to implant ratio: A systematic review. Implant. Dent. 2014, 23, 180–187. [Google Scholar] [CrossRef]
- Rokni, S.; Todescan, R.; Watson, P.; Pharoah, M.; Adegbembo, A.O.; Deporter, D. An assessment of crown-to-root ratios with short sintered porous-surfaced implants supporting prostheses in partially edentulous patients. Int. J. Oral Maxillofac. Implant. 2005, 20, 69–76. [Google Scholar]
- Urdaneta, R.; Rodriguez, S.; McNeil, D.C.; Weed, M.; Chuang, S.K. The effect of increased crown-to-implant ratio on single-tooth locking-taper implants. Int. J. Oral Maxillofac. Implant. 2010, 25, 729–743. [Google Scholar]
- Anitua, E.; Piñas, L.; Orive, G. Retrospective study of short and extra-short implants placed in posterior regions: Influence of crown-to-implant ratio on marginal bone loss. Clin. Implant. Dent. Relat. Res. 2015, 17, 102–110. [Google Scholar] [CrossRef]
- Wells, G.A.; Shea, B.; O’Connell, D.; Peterson, J.; Welch, V.; Losos, M.; Tugwell, P. The Newcastle–Ottawa Scale(NOS) for assessing the quality of nonrandomised studies in meta-analyses. Eur. J. Epidemiol. 2010, 25, 603–605. [Google Scholar]
- Kim, Y.K.; Yun, P.Y.; Yi, Y.J.; Bae, J.H.; Kim, S.B.; Ahn, G.J. One-year prospective study of 7-mm-long implants in the mandible: Installation technique and crown/implant ratio of 1.5 or less. J. Oral Implantol. 2015, 41, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Adánez, M.H.; Brezavšček, M.; Vach, K.; Fonseca, M.; Att, W. Clinical and radiographic evaluation of short implants placed in the posterior mandible: A 1-year pilot split-mouth study. J. Oral Implantol. 2018, 44, 250–259. [Google Scholar] [CrossRef]
- Guarnieri, R.; Di Nardo, D.; Gaimari, G.; Miccoli, G.; Testarelli, L. Short vs. Standard Laser-Microgrooved Implants Supporting Single and Splinted Crowns: A Prospective Study with 3 Years Follow-Up. J. Prosthodont. 2019, 28, 771–779. [Google Scholar] [CrossRef] [PubMed]
- Sahrmann, P.; Naenni, N.; Jung, R.E.; Held, U.; Truninger, T.; Hämmerle, C.H.F.; Attin, T.; Schmidlin, P.R. Success of 6-mm implants with single-tooth restorations: A 3-year randomized controlled clinical trial. J. Dent. Res. 2016, 95, 623–628. [Google Scholar] [CrossRef] [PubMed]
- Hadzik, J.; Krawiec, M.; Sławecki, K.; Kunert-Keil, C.; Dominiak, M.; Gedrange, T. The Influence of the Crown-Implant Ratio on the Crestal Bone Level and Implant Secondary Stability: 36-Month Clinical Study. Biomed. Res. Int. 2018, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Ghariani, L.; Segaan, L.; Rayyan, M.M.; Galli, S.; Jimbo, R.; Ibrahim, A. Does crown/implant ratio influence the survival and marginal bone level of short single implants in the mandibular molar? A preliminary investigation consisting of 12 patients. J. Oral Rehabil. 2016, 43, 127–135. [Google Scholar] [CrossRef]
- Malchiodi, L.; Caricasulo, R.; Cucchi, A.; Vinci, R.; Agliardi, E.; Gherlone, E. Evaluation of Ultrashort and Longer Implants with Microrough Surfaces: Results of a 24- to 36-Month Prospective Study. Int. J. Oral Maxillofac. Implant. 2017, 32, 171–179. [Google Scholar] [CrossRef]
- Mangano, F.; Frezzato, I.; Frezzato, A.; Veronesi, G.; Mortellaro, C.; Mangano, C. The effect of crown-to-implant ratio on the clinical performance of extra-short locking-taper implants. J. Craniofac. Surg. 2016, 27, 675–681. [Google Scholar] [CrossRef]
- Pohl, V.; Thoma, D.S. Sporniak-Tutak, K.; Garcia-Garcia, A.; Taylor, T.D.; Haas, R.; Hämmerle, C.H.F. Short dental implants (6 mm) versus long dental implants (11–15 mm) in combination with sinus floor elevation procedures: 3-year results from a multicentre, randomized, controlled clinical trial. J. Clin. Periodontol. 2017, 44, 438–445. [Google Scholar]
- Schincaglia, G.P.; Thoma, D.S.; Haas, R.; Tutak, M.; Garcia, A.; Taylor, T.D.; Hämmerle, C.H.F. Randomized controlled multicenter study comparing short dental implants (6 mm) versus longer dental implants (11-15 mm) in combination with sinus floor elevation procedures. Part 2: Clinical and radiographic outcomes at 1 year of loading. J. Clin. Periodontol. 2015, 42, 1042–1051. [Google Scholar] [CrossRef] [PubMed]
- Malchiodi, L.; Cucchi, A.; Ghensi, P.; Consonni, D.; Nocini, P.F. Influence of crown-implant ratio on implant success rates and crestal bone levels: A 36-month follow-up prospective study. Clin. Oral Implant. Res. 2014, 25, 240–251. [Google Scholar] [CrossRef] [PubMed]
- Naenni, N.; Sahrmann, P.; Schmidlin, P.R.; Attin, T.; Wiedemeier, D.B.; Sapata, V.; Hämmerle, C.H.F.; Jung, R.E. Five-Year Survival of Short Single-Tooth Implants (6 mm): A Randomized Controlled Clinical Trial. J. Dent. Res. 2018, 97, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Rossi, F.; Botticelli, D.; Cesaretti, G.; De Santis, E.; Storelli, S.; Lang, N.P. Use of short implants (6 mm) in a single-tooth replacement: A 5-year follow-up prospective randomized controlled multicenter clinical study. Clin. Oral Implant. Res. 2016, 27, 458–464. [Google Scholar] [CrossRef]
- Zadeh, H.H.; Guljé, F.; Palmer, P.J.; Abrahamsson, I.; Chen, S.; Mahallati, R.; Stanford, C.M. Marginal bone level and survival of short and standard-length implants after 3 years: An Open Multi-Center Randomized Controlled Clinical Trial. Clin. Oral Implant. Res. 2018, 29, 894–906. [Google Scholar] [CrossRef]
- Blanes, R.J.; Bernard, J.P.; Blanes, Z.M.; Belser, U.C. A 10-year prospective study of ITI dental implants placed in the posterior region. II: Influence of the crown-to-implant ratio and different prosthetic treatment modalities on crestal bone loss. Clin. Oral Implant. Res. 2007, 18, 699–706. [Google Scholar] [CrossRef]
- Nissan, J.; Gross, O.; Ghelfan, O.; Priel, I.; Gross, M.; Chaushu, G. The effect of splinting implant-supported restorations on stress distribution of different crown-implant ratios and crown height spaces. J. Oral Maxillofac. Surg. 2011, 69, 2990–2994. [Google Scholar] [CrossRef]

| AUTHOR (Year) | SELECTION (****) | COMPARABILITY (**) | OUTCOMES (***) | TOTAL | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5a | 5b | 6 | 7 (1 year) | 8 | ||
| Adánez et al. (2018) | * | * | * | * | * | * | * | * | 8 | |
| Blanes et al. (2007) | * | * | * | * | * | * | * | * | 8 | |
| Ghariani et al. (2016) | * | * | * | * | * | * | * | 7 | ||
| Guarnieri et al. (2019) | * | * | * | * | * | * | * | * | * | 9 |
| Hadzik et al. (2018) | * | * | * | * | * | * | * | 7 | ||
| Malchiodi et al. (2014) | * | * | * | * | * | * | * | * | * | 9 |
| Malchiodi et al. (2017) | * | * | * | * | * | * | * | * | 8 | |
| Mangano et al. (2016) | * | * | * | * | * | * | * | * | 8 | |
| Naenni et al. (2018) | * | * | * | * | * | * | * | * | * | 9 |
| Pohl et al. (2017) | * | * | * | * | * | * | * | * | 8 | |
| Rossi et al. (2016) | * | * | * | * | * | * | * | * | * | 9 |
| Sahrmann et al. (2016) | * | * | * | * | * | * | * | * | * | 9 |
| Schincaglia et al. (2015) | * | * | * | * | * | * | * | * | * | 9 |
| Zadeh et al. (2017) | * | * | * | * | * | * | * | * | * | 9 |
| AUTHOR (YEAR) | TYPE OF STUDY | YEARS OF FOLLOW-UP | LENGTH * (mm) | DIAMETER ** (mm) | No. INITIAL IMPLANTS | MEAN MARGINAL BONE LOSS (mm) | SD | S/NS RESTORATIONS | No. LOST IMPLANTS | C/I RATIO | NOS |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Adánez (2018) | PCC | 1 | Short | Standard | 20 | 0′56 | 0′51 | S | 0 | 2 | 8 |
| Standard | Standard | 20 | 0′67 | 0′23 | S | 0 | 1 | ||||
| Blanes (2007) | PCC | 10 | Short | Standard | 108 | 0′5 | 0′63 | S and NS | 3 | 1 | 8 |
| Standard | Standard | 84 | 0′3 | 0′48 | S and NS | 1 | 2 | ||||
| Ghariani (2016) | PCC | 1 | Short | Standard | 5 | NS | 0 | 3 | 7 | ||
| Standard | Standard | 7 | NS | 0 | 2 | ||||||
| Guarnieri (2019) | PCC | 3 | Short | Standard | 28 | 0′23 | 0′6 | S and NS | 1 | 9 | |
| Standard | Standard | 36 | 0′27 | 0′3 | S and NS | 0 | |||||
| Hadzik (2018) | PCC | 3 | Short | Standard | 15 | 0′34 | 0′24 | NS | 1 | 2 | 7 |
| Standard | Standard | 15 | 0′22 | 0′46 | NS | 0 | 2 | ||||
| Malchiodi (2014) | PCC | 3 | Short | Standard | 151 | S and NS | 3 | 9 | |||
| Standard | Standard | 108 | S and NS | 2 | |||||||
| Malchiodi (2017) | PCC | 3 | Short | Standard | 23 | 0′44 | 0′72 | S and NS | 0 | 3 | 8 |
| Short | Standard | 11 | 0′44 | 0′72 | S and NS | 1 | 3 | ||||
| Standard | Narrow | 10 | 0′46 | 0′37 | S and NS | 1 | 2 | ||||
| Standard | Standard | 18 | 0′46 | 0′37 | S and NS | 0 | 2 | ||||
| Standard | Standard | 9 | 0′46 | 0′37 | S and NS | 0 | 2 | ||||
| Standard | Standard | 2 | 0′46 | 0′37 | S and NS | 0 | 2 | ||||
| Standard | Narrow | 12 | 0′75 | 0′86 | S and NS | 2 | 2 | ||||
| Standard | Standard | 18 | 0′75 | 0′86 | S and NS | 0 | 2 | ||||
| Standard | Standard | 10 | 0′75 | 0′86 | S and NS | 0 | 2 | ||||
| Mangano (2016) | PCC | 5 | Short | Standard | 68 | S and NS | 2 | 2 | 8 | ||
| Naenni (2018) | RCT | 5 | Short | Standard | 40 | NS | 4 | 2 | 9 | ||
| Standard | Standard | 46 | NS | 0 | 2 | ||||||
| Pohl (2017) | RCT | 3 | Short | Standard | 61 | 0′44 | 0′44 | NS | 0 | 2 | 8 |
| Standard | Standard | 68 | 0′45 | 0′55 | NS | 0 | 1 | ||||
| Rossi (2016) | PCC | 5 | Short | Standard | 30 | 2′3 | 0′52 | NS | 2 | 9 | |
| Standard | Standard | 30 | 2′64 | 0′56 | NS | 1 | |||||
| Sahrmann (2016) | RCT | 3 | Short | 40 | 0′19 | 0′62 | NS | 1 | 2 | 9 | |
| Standard | 38 | 0′33 | 0′71 | NS | 0 | 2 | |||||
| Schincaglia (2015) | RCT | 1 | Short | Standard | 67 | 0′22 | 0′3 | NS | 2 | 2 | 9 |
| Standard | Standard | 70 | 0′37 | 0′59 | NS | 1 | 1 | ||||
| Zadeh (2018) | RCT | 3 | Short | Standard | 108 | 0′27 | 0′4 | S | 4 | 2 | 9 |
| Standard | Standard | 101 | 0′44 | 0′74 | S | 1 | 1 |
| Estimator | IC-95% | p-Value | |
|---|---|---|---|
| Intercept | 0.131 | −0.009; 0.272 | 0.067 |
| Standard diameter | −0.126 | −0.267; 0.014 | 0.077 |
| C/I ratio = 2 | −0.005 | −0.022; 0.012 | 0.558 |
| C/I ratio = 3 | −0.016 | −0.072; 0.040 | 0.577 |
| Years of follow-up | 0.001 | −0.002; 0.004 | 0.485 |
| Short length | 0.017 | −0.001; 0.035 | 0.055 |
| Estimator | IC-95% | p-Value | |
|---|---|---|---|
| intercept | 0.975 | −0.002; 1.952 | 0.050 |
| Standard diameter | −0.084 | −0.937; 0.768 | 0.845 |
| C/I ratio = 2 | −0.322 | −0.849; 0.204 | 0.230 |
| C/I ratio = 3 | −0.453 | −1.424; 0.517 | 0.360 |
| Years of follow-up | −0.019 | −0.114; 0.075 | 0.685 |
| Short length | 0.061 | −0.433; 0.556 | 0.807 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Torres-Alemany, A.; Fernández-Estevan, L.; Agustín-Panadero, R.; Montiel-Company, J.M.; Labaig-Rueda, C.; Mañes-Ferrer, J.F. Clinical Behavior of Short Dental Implants: Systematic Review and Meta-Analysis. J. Clin. Med. 2020, 9, 3271. https://doi.org/10.3390/jcm9103271
Torres-Alemany A, Fernández-Estevan L, Agustín-Panadero R, Montiel-Company JM, Labaig-Rueda C, Mañes-Ferrer JF. Clinical Behavior of Short Dental Implants: Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2020; 9(10):3271. https://doi.org/10.3390/jcm9103271
Chicago/Turabian StyleTorres-Alemany, Andrea, Lucía Fernández-Estevan, Rubén Agustín-Panadero, José María Montiel-Company, Carlos Labaig-Rueda, and José Félix Mañes-Ferrer. 2020. "Clinical Behavior of Short Dental Implants: Systematic Review and Meta-Analysis" Journal of Clinical Medicine 9, no. 10: 3271. https://doi.org/10.3390/jcm9103271
APA StyleTorres-Alemany, A., Fernández-Estevan, L., Agustín-Panadero, R., Montiel-Company, J. M., Labaig-Rueda, C., & Mañes-Ferrer, J. F. (2020). Clinical Behavior of Short Dental Implants: Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 9(10), 3271. https://doi.org/10.3390/jcm9103271






