Incidence and Predictors of Unplanned Hospital Readmission after Percutaneous Coronary Intervention
Abstract
1. Introduction
2. Methods
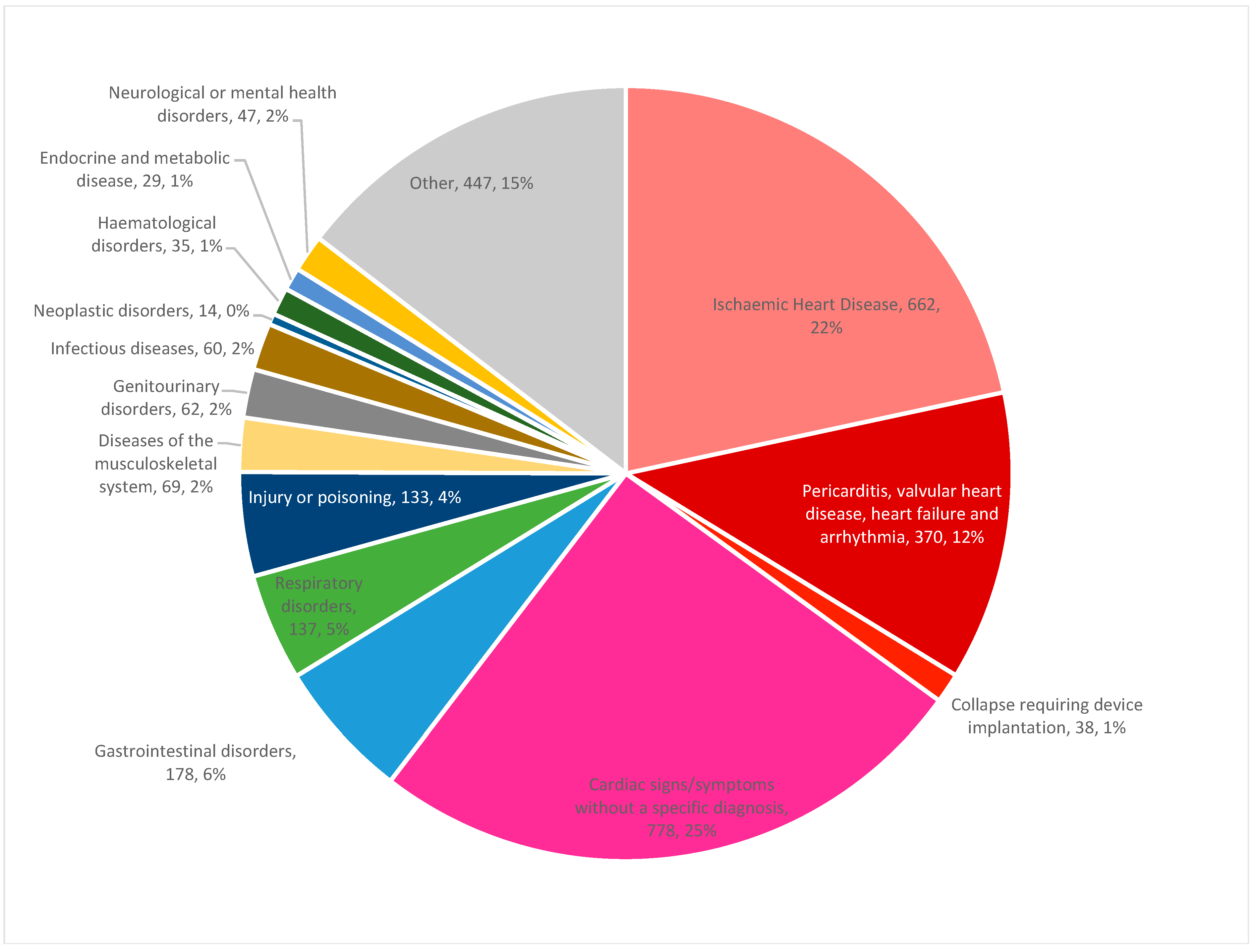
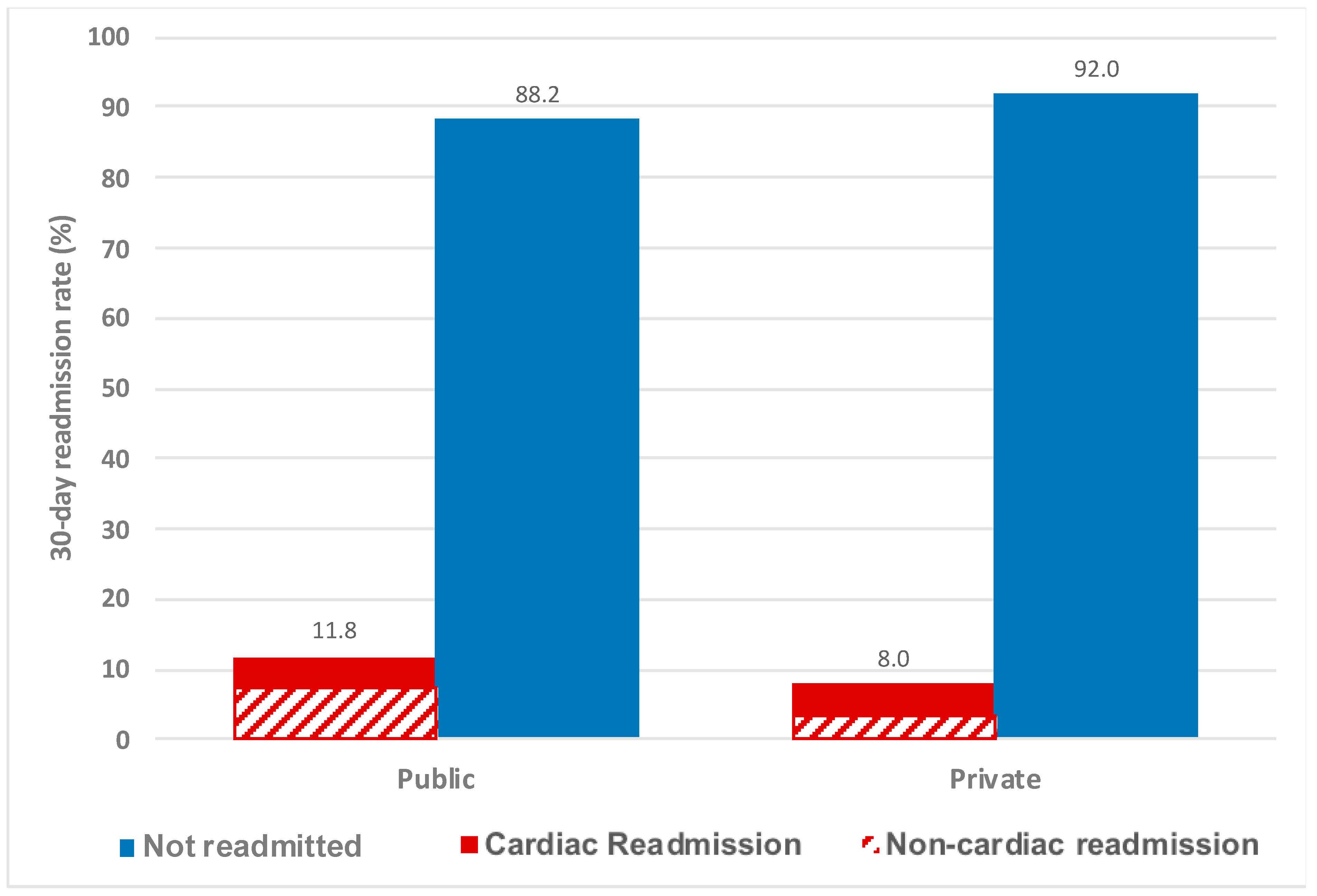
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Jencks, S.F.; Williams, M.V.; Coleman, E.A. Rehospitalizations among patients in the Medicare fee-for-service program. N. Engl. J. Med. 2009, 360, 1418–1428. [Google Scholar] [CrossRef] [PubMed]
- Curtis, J.P.; Schreiner, G.; Wang, Y.; Chen, J.; Spertus, J.A.; Rumsfeld, J.S.; Brindis, R.G.; Krumholz, H.M. All-cause readmission and repeat revascularization after percutaneous coronary intervention in a cohort of medicare patients. J. Am. Coll. Cardiol. 2009, 54, 903–907. [Google Scholar] [CrossRef] [PubMed]
- Kwok, C.S.; Hulme, W.; Olier, I.; Holroyd, E.; Mamas, M.A. Review of early hospitalisation after percutaneous coronary intervention. Int. J. Cardiol. 2017, 227, 370–377. [Google Scholar] [CrossRef] [PubMed]
- Robinson, P. Hospital Readmissions and the 30 Day Threshold, 2010. A CHKS Market Intelligence Report 2010. Available online: http://www.chks.co.uk/userfiles/files/CHKS%20Report%20Hospital%20readmissions.pdf (accessed on 1 April 2020).
- Joynt, K.E.; Jha, A.K. A path forward on Medicare readmissions. N. Engl. J. Med. 2013, 368, 1175–1177. [Google Scholar] [CrossRef]
- Biswas, S.; Lefkovits, J.; Liew, D.; Gale, C.P.; Reid, C.M.; Stub, D. Characteristics of national and major regional percutaneous coronary intervention registries: A structured literature review. Eurointervention 2018, 14, 1112–1120. [Google Scholar] [CrossRef]
- Stub, D.; Lefkovits, J.; Brennan, A.L.; Dinh, D.; Brien, R.; Duffy, S.J.; Cox, N.; Nadurata, V.; Clark, D.J.; Andrianopoulos, N.; et al. The Establishment of the Victorian Cardiac Outcomes Registry (VCOR): Monitoring and Optimising Outcomes for Cardiac Patients in Victoria. Heart Lung Circ. 2018, 27, 451–463. [Google Scholar] [CrossRef]
- National Centre for Classification in Health. The International Statistical Classification of Diseases and Related Health Problems, 10th ed.; Australian modification (ICD-10-AM); National Centre for Classification in Health, Faculty of Health Sciences, University of Sydney: Sydney, Australia, 2018. [Google Scholar]
- Ahern, S.; Hopper, I.; Evans, S.M. Clinical quality registries for clinician-level reporting: Strengths and limitations. Med. J. Aust. 2017, 206, 427–429. [Google Scholar] [CrossRef]
- Moretti, C.; D’Ascenzo, F.; Omede, P.; Sciuto, F.; Presutti, D.G.; Di Cuia, M.; Colaci, C.; Giusto, F.; Ballocca, F.; Cerrato, E.; et al. Thirty-day readmission rates after PCI in a metropolitan center in Europe: Incidence and impact on prognosis. J. Cardiovasc. Med. 2015, 16, 238–245. [Google Scholar] [CrossRef] [PubMed]
- Tripathi, A.; Abbott, J.D.; Fonarow, G.C.; Khan, A.R.; Barry, N.G.; Ikram, S.; Coram, R.; Mathew, V.; Kirtane, A.J.; Nallamothu, B.K.; et al. Thirty-Day Readmission Rate and Costs after Percutaneous Coronary Intervention in the United States: A National Readmission Database Analysis. Circ. Cardiovasc. Interv. 2017, 10, e005925. [Google Scholar] [CrossRef]
- Przybysz-Zdunek, B.; Ploch, M.; Pluta, W.; Dada, M.; Opolski, G. All-cause readmission and repeat revascularization after percutaneous coronary intervention. Cardiol. J. 2012, 19, 174–179. [Google Scholar] [CrossRef]
- Yost, G.W.; Puher, S.L.; Graham, J.; Scott, T.D.; Skelding, K.A.; Berger, P.B.; Blankenship, J.C. Readmission in the 30 days after percutaneous coronary intervention. JACC Cardiovasc. Interv. 2013, 6, 237–244. [Google Scholar] [CrossRef]
- Wasfy, J.H.; Strom, J.B.; O’Brien, C.; Zai, A.H.; Luttrell, J.; Kennedy, K.F.; Spertus, J.A.; Zelevinsky, K.; Normand, S.L.; Mauri, L.; et al. Causes of short-term readmission after percutaneous coronary intervention. Circ. Cardiovasc. Interv. 2014, 7, 97–103. [Google Scholar] [CrossRef] [PubMed]
- Khawaja, F.J.; Shah, N.D.; Lennon, R.J.; Slusser, J.P.; Alkatib, A.A.; Rihal, C.S.; Gersh, B.J.; Montori, V.M.; Holmes, D.R.; Bell, M.R.; et al. Factors associated with 30-day readmission rates after percutaneous coronary intervention. Arch. Intern. Med. 2012, 172, 112–117. [Google Scholar] [CrossRef] [PubMed]
- Joynt, K.E.; Jha, A.K. Who has higher readmission rates for heart failure, and why? Implications for efforts to improve care using financial incentives. Circ. Cardiovasc. Qual. Outcomes 2011, 4, 53–59. [Google Scholar] [CrossRef] [PubMed]
- Holom, G.H.; Hagen, T.P. Quality differences between private for-profit, private non-profit and public hospitals in Norway: A retrospective national register-based study of acute readmission rates following total hip and knee arthroplasties. BMJ Open 2017, 7, e015771. [Google Scholar] [CrossRef] [PubMed]
- Lefkovits, J.; Brennan, A.; Dinh, D.; Stub, D.; Carruthers, H.; Doyle, J.; Lucas, M.; Reid, C. The Victorian Cardiac Outcomes Registry Annual Report 2018; Monash University SPHPM: Melbourne, Australia, 2019. [Google Scholar]
- Hannan, E.L.; Zhong, Y.; Krumholz, H.; Walford, G.; Holmes, D.R., Jr.; Stamato, N.J.; Jacobs, A.K.; Venditti, F.J.; Sharma, S.; King, S.B., 3rd. 30-day readmission for patients undergoing percutaneous coronary interventions in New York state. JACC Cardiovasc. Interv. 2011, 4, 1335–1342. [Google Scholar] [CrossRef] [PubMed]
- Kwok, C.S.; Rao, S.V.; Potts, J.E.; Kontopantelis, E.; Rashid, M.; Kinnaird, T.; Curzen, N.; Nolan, J.; Bagur, R.; Mamas, M.A. Burden of 30-Day Readmissions after Percutaneous Coronary Intervention in 833,344 Patients in the United States: Predictors, Causes, and Cost: Insights from the Nationwide Readmission Database. JACC Cardiovasc. Interv. 2018, 11, 665–674. [Google Scholar] [CrossRef]
- Stromberg, A.; Martensson, J.; Fridlund, B.; Levin, L.A.; Karlsson, J.E.; Dahlstrom, U. Nurse-led heart failure clinics improve survival and self-care behaviour in patients with heart failure: Results from a prospective, randomised trial. Eur. Heart J. 2003, 24, 1014–1023. [Google Scholar] [CrossRef]
- Blue, L.; Lang, E.; McMurray, J.J.; Davie, A.P.; McDonagh, T.A.; Murdoch, D.R.; Petrie, M.C.; Connolly, E.; Norrie, J.; Round, C.E.; et al. Randomised controlled trial of specialist nurse intervention in heart failure. BMJ 2001, 323, 715–718. [Google Scholar] [CrossRef]
- Harjai, K.J.; Thompson, H.W.; Turgut, T.; Shah, M. Simple clinical variables are markers of the propensity for readmission in patients hospitalized with heart failure. Am. J. Cardiol. 2001, 87, 234–237. [Google Scholar] [CrossRef]
- Hummel, S.L.; Katrapati, P.; Gillespie, B.W.; Defranco, A.C.; Koelling, T.M. Impact of prior admissions on 30-day readmissions in medicare heart failure inpatients. Mayo Clin. Proc. 2014, 89, 623–630. [Google Scholar] [CrossRef] [PubMed]
- Kilkenny, M.F.; Dewey, H.M.; Sundararajan, V.; Andrew, N.E.; Lannin, N.; Anderson, C.S.; Donnan, G.A.; Cadilhac, D.A. Readmissions after stroke: Linked data from the Australian Stroke Clinical Registry and hospital databases. Med. J. Aust. 2015, 203, 102–106. [Google Scholar] [CrossRef] [PubMed]
- Australian Digital Health Agency. What’s in a My Health Record. Canberra, Australia, 2018. Available online: https://www.myhealthrecord.gov.au/for-healthcare-professionals/what-is-in-my-health-record (accessed on 11 January 2019).
- Tanguturi, V.K.; Temin, E.; Yeh, R.W.; Thompson, R.W.; Rao, S.K.; Mallick, A.; Cavallo, E.; Ferris, T.G.; Wasfy, J.H. Clinical Interventions to Reduce Preventable Hospital Readmission after Percutaneous Coronary Intervention. Circ. Cardiovasc. Qual. Outcomes 2016, 9, 600–604. [Google Scholar] [CrossRef] [PubMed]

| Not Readmitted (n = 25,423) | Any Cardiac Readmission (n = 1848) | All Non-Cardiac Readmissions (n = 1211) | p | |
|---|---|---|---|---|
| Baseline characteristics | ||||
| Median age, years ± SD | 66.2 ± 11.7 | 66.4 ± 12.0 | 71.1 ± 12.8 | <0.001 |
| Female | 5844 (23.0) | 564 (30.5) | 375 (31.0) | <0.001 |
| Body mass index groups: | ||||
| Underweight | 165 (0.7) | 15 (0.8) | 14 (1.2) | <0.001 |
| Normal | 5422 (21.6) | 457 (25.1) | 326 (27.2) | |
| Overweight | 10,342 (41.2) | 701 (38.5) | 439 (36.7) | |
| Obese | 9144 (36.5) | 649 (35.6) | 418 (34.9) | |
| Aboriginal and/or Torres Strait Islander | 104 (0.4) | 10 (0.6) | 7 (0.6) | 0.50 |
| Diabetes mellitus | 5427 (21.3) | 425 (23.0) | 315 (26.0) | <0.001 |
| Peripheral vascular disease | 833 (3.3) | 80 (4.3) | 60 (5.0) | <0.001 |
| Previous cerebrovascular disease | 915 (3.6) | 105 (5.7) | 72 (5.9) | <0.001 |
| Previous percutaneous coronary intervention | 5557 (21.9) | 349 (18.9) | 219 (18.1) | <0.001 |
| Previous coronary artery bypass graft surgery | 1971 (7.8) | 150 (8.1) | 102 (8.4) | 0.61 |
| Stage 4–5 chronic kidney disease (estimated glomerular filtration rate (eGFR) < 30 mL/min/1.73 m2) | 445 (1.9) | 54 (3.1) | 63 (5.6) | <0.001 |
| Left ventricular ejection fraction (LVEF): | ||||
| LVEF ≥50 | 14,744 (67.1) | 1035 (63.3) | 591 (55.6) | <0.001 |
| LVEF 45–49 | 4284 (19.5) | 297 (18.2) | 248 (23.4) | |
| LVEF 35–44 | 2099 (9.6) | 208 (12.7) | 143 (13.5) | |
| LVEF <35 | 843 (3.8) | 94 (5.8) | 80 (7.5) | |
| Number of admissions within the previous 12 months: | ||||
| 0 | 20,196 (79.4) | 1306 (70.7) | 789 (65.2) | <0.001 |
| 1 | 3749 (14.7) | 311 (16.8) | 238 (19.7) | |
| 2 | 953 (3.7) | 110 (6.0) | 88 (7.3) | |
| 3–5 | 480 (1.9) | 90 (4.9) | 81 (6.7) | |
| >5 | 45 (0.2) | 31 (1.7) | 15 (1.2) | |
| Presentation characteristics: | ||||
| Stable angina | 11,499 (45.2) | 470 (25.4) | 396 (32.7) | <0.001 |
| Non-ST elevation acute coronary syndrome | 8512 (33.5) | 853 (46.2) | 486 (40.1) | |
| ST-elevation myocardial infarction | 5412 (21.3) | 525 (28.4) | 329 (27.2) | |
| Cardiogenic shock | 329 (1.3) | 37 (2.0) | 39 (3.2) | <0.001 |
| Intubated-out-of-hospital cardiac arrest | 41 (0.2) | 3 (0.2) | 5 (0.4) | 0.12 |
| Out-of-hours presentation | 12,226 (48.1) | 952 (51.5) | 607 (50.1) | 0.008 |
| Procedural characteristics: | ||||
| Radial/brachial access | 13,038 (51.3) | 927 (50.2) | 577 (47.6) | 0.03 |
| Femoral access | 12,385 (48.7) | 921 (49.8) | 634 (52.4) | |
| Multi-vessel disease | 1689 (6.6) | 117 (6.3) | 84 (6.9) | 0.80 |
| ACC/AHA B2/C lesion | 14,252 (56.1) | 1047 (56.7) | 727 (60.0) | 0.02 |
| Chronic total occlusion lesion treated | 966 (3.8) | 62 (3.4) | 46 (3.8) | 0.62 |
| Unprotected left main vessel lesion | 257 (1.0) | 19 (1.0) | 12 (1.0) | 0.99 |
| Drug-eluting stent used | 20,894 (82.2) | 1421 (76.9) | 940 (77.6) | <0.001 |
| Glycoprotein IIb/IIIa inhibitor used | 2756 (10.8) | 246 (13.3) | 161 (13.3) | <0.001 |
| Unsuccessful percutaneous coronary intervention | 1407 (5.5) | 140 (7.6) | 73 (6.0) | 0.001 |
| Not Readmitted (n = 25,423) | Any Cardiac Readmission (n = 1848) | All Non-Cardiac Readmission (n = 1211) | p | |
|---|---|---|---|---|
| Median length of stay, days [IQR] | 2 (1–4) | 3 (2–5) | 4 (2–6) | <0.001 |
| Length of stay <3 days | 13,183 (51.9) | 661 (35.8) | 394 (32.5) | <0.001 |
| Length of stay ≥3 | 12,240 (48.1) | 1187 (64.2) | 817 (67.5) | |
| Discharge destination: | ||||
| Home | 24,382 (95.9) | 1724 (93.3) | 1106 (91.3) | <0.001 |
| Hospital in the home | 109 (0.4) | 7 (0.4) | 7 (0.6) | |
| Rehab | 445 (1.8) | 40 (2.2) | 54 (4.5) | |
| Local or referring hospital | 380 (1.5) | 57 (3.1) | 32 (2.6) | |
| Tertiary referral centre | 107 (0.4) | 20 (1.1) | 12 (1.0) | |
| In-hospital complications | ||||
| New renal impairment | 426 (2.3) | 58 (3.8) | 64 (6.5) | <0.001 |
| Cardiogenic shock | 164 (0.6) | 32 (1.7) | 19 (1.6) | <0.001 |
| Peri-procedural myocardial infarction | 142 (0.6) | 25 (1.4) | 16 (1.3) | <0.001 |
| Unplanned PCI for target vessel revascularisation | 53 (0.2) | 9 (0.5) | 5 (0.4) | 0.03 |
| Target lesion revascularisation | 106 (0.4) | 17 (1.0) | 9 (0.8) | 0.003 |
| Unplanned coronary artery bypass surgery | 101 (0.4) | 11 (0.6) | 14 (1.2) | <0.001 |
| Stent thrombosis | 38 (0.1) | 2 (0.1) | 3 (0.2) | 0.61 |
| Major bleeding | 156 (0.6) | 14 (0.8) | 20 (1.7) | <0.001 |
| Stroke | 49 (0.2) | 5 (0.3) | 3 (0.2) | 0.72 |
| Any of the above in-hospital complications | 621 (2.5) | 90 (5.0) | 69 (5.9) | <0.001 |
| Discharge medications | ||||
| Aspirin | 24,727 (97.5) | 1791 (97.3) | 1165 (96.4) | 0.09 |
| Thienopyridine | 13,802 (54.5) | 900 (49.0) | 625 (51.8) | <0.001 |
| Ticagrelor | 11,048 (43.6) | 889 (48.5) | 548 (45.5) | <0.001 |
| Beta-blocker | 17,666 (70.1) | 1382 (75.5) | 898 (74.6) | <0.001 |
| Angiotensin converting enzyme inhibitors/angiotensin receptor blockers | 18,233 (72.3) | 1325 (72.4) | 880 (73.2) | 0.82 |
| Any lipid lowering therapies | 23,791 (94.2) | 1731 (94.2) | 1119 (92.9) | 0.21 |
| Oral anticoagulants | 1728 (6.8) | 170 (9.3) | 158 (13.1) | <0.001 |
| Any Cardiac Readmission | All Non-Cardiac Readmissions | ||||
|---|---|---|---|---|---|
| Odds Ratio (95% CI) | p | Odds Ratio (95% CI) | p | ||
| Age group | |||||
| 51–60 years | 1 (ref.) | 1 (ref.) | |||
| <40 years | 0.78 (0.53–1.16) | 0.22 | 0.64 (0.34–1.20) | 0.16 | |
| 41–50 years | 1.18 (0.98–1.42) | 0.08 | 1.03 (0.77–1.39) | 0.83 | |
| 61–70 years | 0.94 (0.81–1.09) | 0.38 | 1.45 (1.18–1.78) | <0.001 | |
| 71–80 years | 0.97 (0.83–1.14) | 0.72 | 2.00 (1.63–2.45) | <0.001 | |
| >80 years | 1.15 (0.94–1.40) | 0.18 | 2.47 (1.94–3.13) | <0.001 | |
| Sex | |||||
| Male | 1 (ref.) | 1 (ref.) | |||
| Female | 1.46 (1.30–1.64) | <0.001 | 1.29 (1.12–1.49) | <0.001 | |
| Diabetes mellitus | 1.08 (0.95–1.23) | 0.25 | 1.21 (1.04–1.40) | 0.02 | |
| Peripheral vascular disease | 1.21 (0.92–1.58) | 0.18 | 1.03 (0.76–1.42) | 0.83 | |
| Previous stroke | 1.37 (1.08–1.74) | 0.009 | 1.18 (0.89–1.56) | 0.25 | |
| Previous PCI | 0.87 (0.75–1.01) | 0.06 | 0.76 (0.63–0.90) | 0.002 | |
| Previous CABG | 1.02 (0.82–1.27) | 0.88 | 0.91 (0.71–1.18) | 0.48 | |
| Presentation diagnosis | |||||
| Stable angina | 1 (ref.) | 1 (ref.) | |||
| NSTEACS | 2.62 (2.23–3.09) | <0.001 | 1.71 (1.42–2.06) | <0.001 | |
| STEMI | 2.79 (2.29–3.38) | <0.001 | 1.76 (1.40–2.22) | <0.001 | |
| Cardiogenic shock at presentation | 1.52 (1.02–2.24) | 0.04 | 1.19 (0.96–1.47) | 0.11 | |
| Number of admissions within previous 12 months: | |||||
| 0 | 1 (ref.) | 1 (ref.) | |||
| 1 | 1.50 (1.29–1.73) | <0.001 | 1.71 (1.44–2.02) | <0.001 | |
| 2 | 1.86 (1.47–2.36) | <0.001 | 2.20 (1.69–2.85) | <0.001 | |
| 3 | 3.36 (2.56–4.40) | <0.001 | 4.58 (3.47–6.06) | <0.001 | |
| 4 | 11.83 (6.89–20.31) | <0.001 | 8.34 (4.18–16.66) | <0.001 | |
| Drug-eluting stent used | 0.88 (0.77–1.01) | 0.08 | 0.87 (0.74–1.03) | 0.11 | |
| Unsuccessful PCI | 1.32 (1.05–1.66) | 0.02 | 1.05 (0.86–1.29) | 0.62 | |
| Any in-hospital complication | 1.72 (1.32–2.23) | <0.001 | 1.71 (1.26–2.31) | 0.001 | |
| Left ventricular ejection fraction (LVEF): | |||||
| LVEF 50% | 1 (ref.) | 1 (ref.) | |||
| LVEF 45–49% | 1.22 (1.04–1.45) | 0.02 | 1.07 (0.90–1.27) | 0.44 | |
| LVEF 35–44% | 1.33 (1.09 1.64) | 0.006 | 1.14 (0.89–1.45) | 0.30 | |
| LVEF <35% | 1.39 (1.06–1.82) | 0.02 | 1.19 (0.96–1.47) | 0.11 | |
| Discharged on oral anticoagulant | 1.26 (1.05–1.53) | 0.02 | 1.50 (1.22–1.84) | <0.001 | |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biswas, S.; Dinh, D.; Lucas, M.; Duffy, S.J.; Brennan, A.L.; Liew, D.; Cox, N.; Nadurata, V.; Reid, C.M.; Lefkovits, J.; et al. Incidence and Predictors of Unplanned Hospital Readmission after Percutaneous Coronary Intervention. J. Clin. Med. 2020, 9, 3242. https://doi.org/10.3390/jcm9103242
Biswas S, Dinh D, Lucas M, Duffy SJ, Brennan AL, Liew D, Cox N, Nadurata V, Reid CM, Lefkovits J, et al. Incidence and Predictors of Unplanned Hospital Readmission after Percutaneous Coronary Intervention. Journal of Clinical Medicine. 2020; 9(10):3242. https://doi.org/10.3390/jcm9103242
Chicago/Turabian StyleBiswas, Sinjini, Diem Dinh, Mark Lucas, Stephen J. Duffy, Angela L. Brennan, Danny Liew, Nicholas Cox, Voltaire Nadurata, Christopher M. Reid, Jeffrey Lefkovits, and et al. 2020. "Incidence and Predictors of Unplanned Hospital Readmission after Percutaneous Coronary Intervention" Journal of Clinical Medicine 9, no. 10: 3242. https://doi.org/10.3390/jcm9103242
APA StyleBiswas, S., Dinh, D., Lucas, M., Duffy, S. J., Brennan, A. L., Liew, D., Cox, N., Nadurata, V., Reid, C. M., Lefkovits, J., & Stub, D. (2020). Incidence and Predictors of Unplanned Hospital Readmission after Percutaneous Coronary Intervention. Journal of Clinical Medicine, 9(10), 3242. https://doi.org/10.3390/jcm9103242




