Short-Term Exercise Progression of Cardiovascular Patients throughout Cardiac Rehabilitation: An Observational Study
Abstract
1. Introduction
2. Materials and Methods
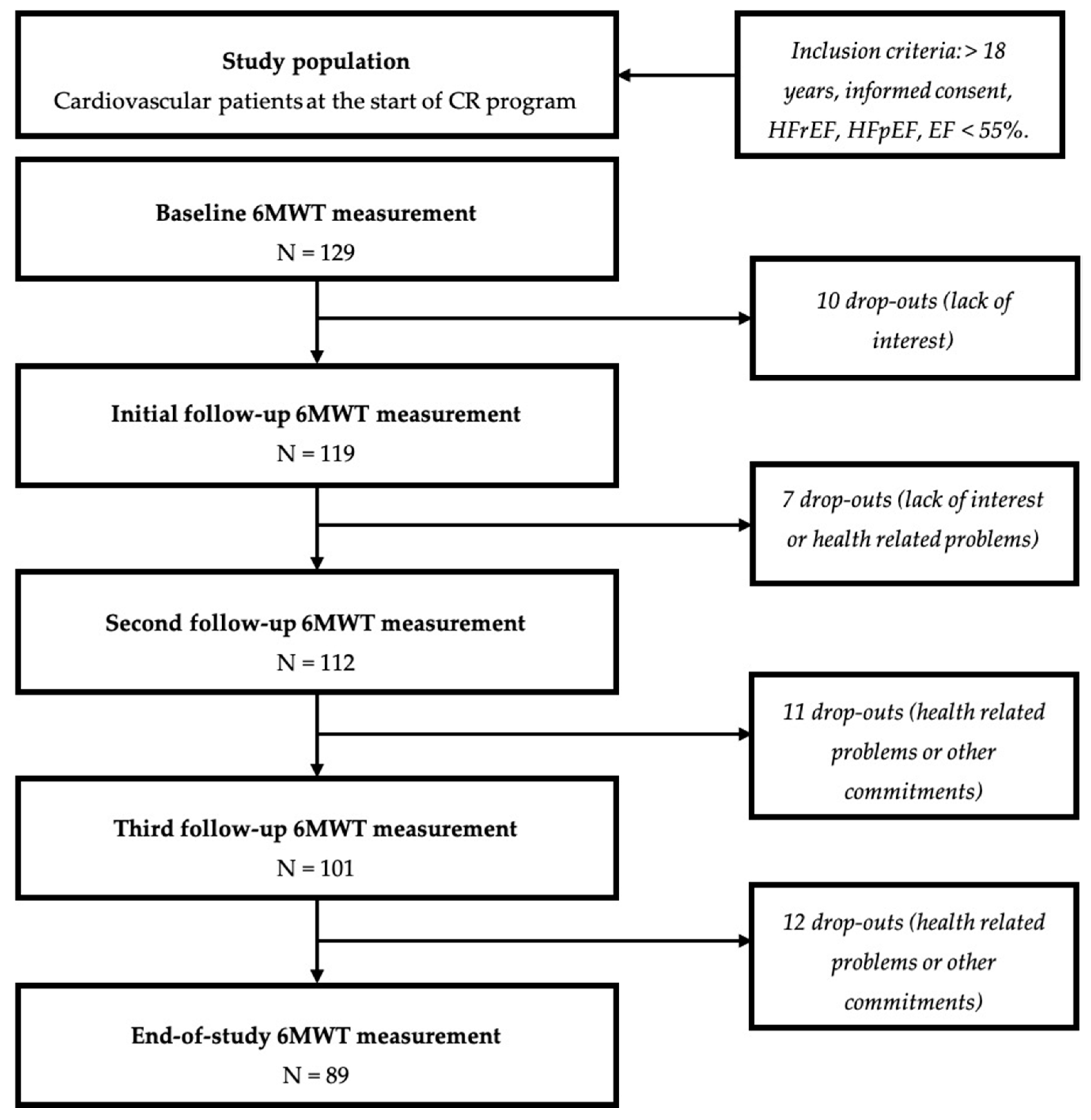
2.1. Study Population
2.2. Standard of Care Multidisciplinary CR Program
2.3. Baseline Characteristics and Experimental Study Protocol
2.4. Study-Endpoints
2.5. Statistics
3. Results
3.1. Demographics and Baseline Population
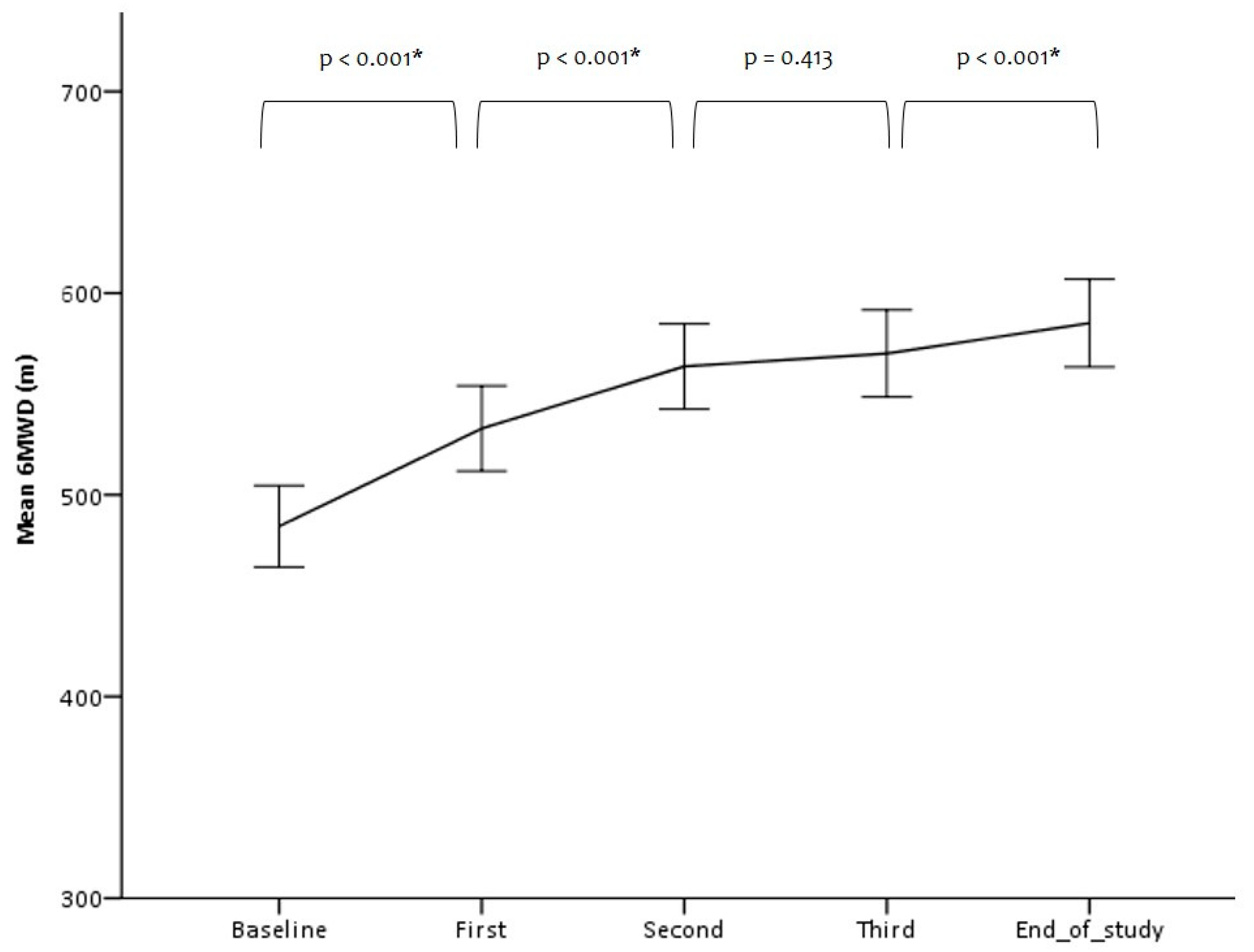
3.2. Measuring Exercise Capacity and HRQoL: CPET Data and 6MWT
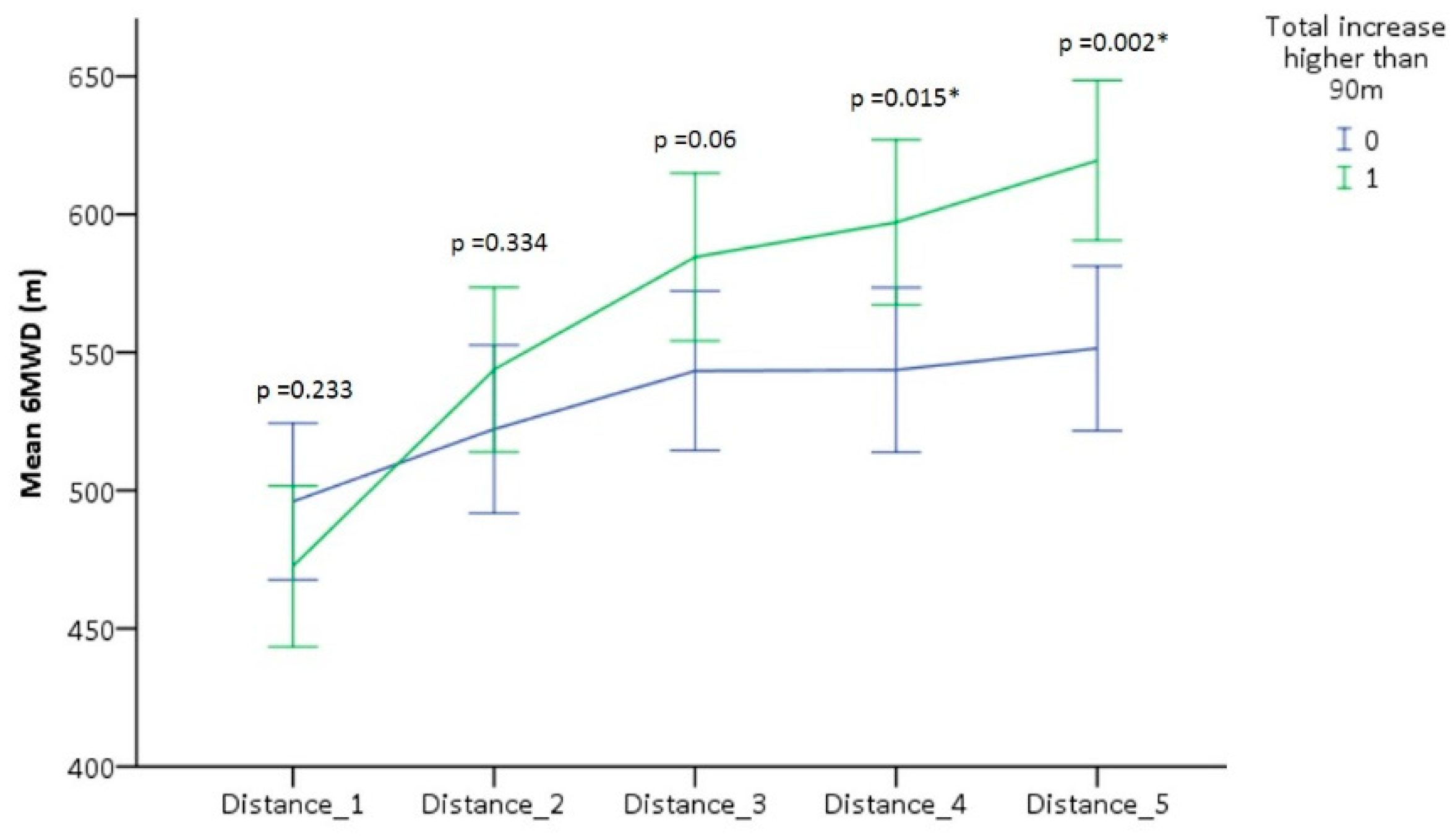
3.3. Different Levels of Response to CR
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix A
| Reason for Referral, Others | (n = 129) |
|---|---|
| Non-ischemic cardiomyopathy | 9 (7%) |
| Low fitness level | 7 (5%) |
| Valve disease | 5 (4%) |
| Following CRT implantation | 6 (4%) |
| Variable | Complete (n = 89) | Non-Complete (n = 40) | p-Value |
|---|---|---|---|
| Demographics | |||
| Male | 65 (73%) | 27 (68%) | 0.534 |
| Age, yrs >65 yrs | 63 (10) 37 (42%) | 62 (14) 18 (45%) | 0.398 |
| Height, m | 1.72 (1.70–1.74) | 1.71 (1.67–1.74) | 0.498 |
| BMI, kg/m2 | 26.7 (4.1) | 28.4 (6.3) | 0.072 |
| Active smoker | 18 (20%) | 10 (25%) | 0.495 |
| Past smoker | 34 (38%) | 13 (33%) | 0.692 |
| LV ejection fraction baseline, % | 45 (43–49) | 42 (38–46) | 0.123 |
| LV ejection fraction final, % | 50 (47–53) | NA | |
| CRT, % | 17 (19%) | 9 (23%) | 0.627 |
| CRT-D | 10 (59%) | 5 (50%) | |
| CRT-P | 7 (41%) | 4 (50%) | |
| Reason of referral | |||
| MI, % HF, % | 23 (26%) | 9 (23%) | 0.826 |
| 21 (24%) | 17 (43%) | 0.037 * | |
| CABG, % | 14 (16%) | 3 (8%) | 0.266 |
| PCI, % | 11 (12%) | 4 (10%) | 0.776 |
| Other, % | 20 (22%) | 7 (16%) | |
| Comorbidities | |||
| Atrial fibrillation | 22 (25%) | 11 (28%) | 0.828 |
| Hypertension | 38 (43%) | 22 (55%) | 0.084 |
| Dyslipidemia | 39 (44%) | 14 (35%) | 0.440 |
| Diabetes | 12 (14%) | 9 (23%) | 0.208 |
| NYHA class | 0.222 | ||
| Class I | 26 (29%) | 10 (25%) | |
| Class II | 44 (50%) | 16 (40%) | |
| Class III | 19 (21%) | 14 (35%) | |
| Medications | |||
| ACE inhibitor | 50 (56.2%) | 17 (43%) | 0.184 |
| Beta-blocker | 63 (71%) | 34 (85%) | 0.122 |
| Diuretics | 39 (43%) | 27 (68%) | 0.014 * |
| Statins | 64 (71%) | 29 (73%) | 0.999 |
| Calcium-channel blockers | 9 (10%) | 1 (3%) | 0.172 |
| Anticoagulants | 28 (32%) | 14 (35%) | 0.690 |
| Baseline CPET (n = 101) | |||
| Peak VO2, mL/kg/min | 17.00 (5.09) | 14.06 (5.46) | 0.013 * |
| Percent predicted peak VO2, % | 60 (20) | 52 (18) | 0.373 |
| Peak power, watts | 114 (106–122) | 96 (84–108) | 0.014 * |
| Respiratory exchange ratio | 1.10 (0.10) | 1.05 (0.11) | 0.061 |
| Baseline 6MWT | |||
| Distance, m | 484 (96) | 431 (110) | 0.006 * |
| Rest HR, bpm | 68 (65–71) | 67 (63–71) | 0.543 |
| Rest blood pressure, mmHg | 127/76 (19/10) | 124/73 (18/13) | 0.320/0.006 * |
References
- Dalal, H.M.; Doherty, P.; Taylor, R.S. Cardiac rehabilitation. BMJ (Clin. Res. Ed.) 2015, 351, h5000. [Google Scholar] [CrossRef]
- Wenger, N.K. Current status of cardiac rehabilitation. J. Am. Coll. Cardiol. 2008, 51, 1619–1631. [Google Scholar] [CrossRef]
- Piepoli, M.F.; Hoes, A.W.; Agewall, S.; Albus, C.; Brotons, C.; Catapano, A.L.; Cooney, M.T.; Corrà, U.; Cosyns, B.; Deaton, C.; et al. 2016 European Guidelines on cardiovascular disease prevention in clinical practice: The Sixth Joint Task Force of the European Society of Cardiology and Other Societies on Cardiovascular Disease Prevention in Clinical Practice (constituted by representatives of 10 societies and by invited experts) Developed with the special contribution of the European Association for Cardiovascular Prevention & Rehabilitation (EACPR). Atherosclerosis 2016, 252, 207–274. [Google Scholar] [PubMed]
- Bjarnason-Wehrens, B.; Nebel, R.; Jensen, K.; Hackbusch, M.; Grilli, M.; Gielen, S.; Schwaab, B.; Rauch, B. German Society of Cardiovascular Prevention and Rehabilitation (DGPR). Exercise-based cardiac rehabilitation in patients with reduced left ventricular ejection fraction: The Cardiac Rehabilitation Outcome Study in Heart Failure (CROS-HF): A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2020, 27, 929–952. [Google Scholar] [CrossRef] [PubMed]
- Ambrosetti, M.; Abreu, A.; Corrà, U.; Davos, C.H.; Hansen, D.; Frederix, I.; Iliou, M.C.; Pedretti, R.F.; Schmid, J.P.; Vigorito, C.; et al. Secondary prevention through comprehensive cardiovascular rehabilitation: From knowledge to implementation. 2020 update. A position paper from the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 2020, 30, 2047487320913379. [Google Scholar] [CrossRef] [PubMed]
- Lawler, P.R.; Filion, K.B.; Eisenberg, M.J. Efficacy of exercise-based cardiac rehabilitation post-myocardial infarction: A systematic review and meta-analysis of randomized controlled trials. Am. Heart J. 2011, 162, 571–584. [Google Scholar] [CrossRef] [PubMed]
- Anderson, L.; Oldridge, N.; Thompson, D.R.; Zwisler, A.D.; Rees, K.; Martin, N.; Taylor, R.S. Exercise-Based Cardiac Rehabilitation for Coronary Heart Disease: Cochrane Systematic Review and Meta-Analysis. J. Am. Coll. Cardiol. 2016, 67, 1–12. [Google Scholar] [CrossRef]
- O’Connor, C.M.; Whellan, D.J.; Lee, K.L.; Keteyian, S.J.; Cooper, L.S.; Ellis, S.J.; Leifer, E.S.; Kraus, W.E.; Kitzman, D.W.; Blumenthal, J.A.; et al. Efficacy and safety of exercise training in patients with chronic heart failure: HF-ACTION randomized controlled trial. JAMA 2009, 301, 1439–1450. [Google Scholar] [CrossRef]
- Taylor, R.S.; Walker, S.; Smart, N.A.; Piepoli, M.F.; Warren, F.C.; Ciani, O.; O’Connor, C.; Whellan, D.; Keteyian, S.J.; Coats, A.; et al. Impact of Exercise Rehabilitation on Exercise Capacity and Quality-of-Life in Heart Failure: Individual Participant Meta-Analysis. J. Am. Coll. Cardiol. 2019, 73, 1430–1443. [Google Scholar] [CrossRef]
- Taylor, R.S.; Walker, S.; Smart, N.A.; Piepoli, M.F.; Warren, F.C.; Ciani, O.; O’Connor, C.; Whellan, D.; Keteyian, S.J.; Coats, A.; et al. Impact of exercise-based cardiac rehabilitation in patients with heart failure (ExTraMATCH II) on mortality and hospitalisation: An individual patient data meta-analysis of randomised trials. Eur. J. Heart Fail. 2018, 20, 1735–1743. [Google Scholar] [CrossRef]
- Long, L.; Mordi, I.R.; Bridges, C.; Sagar, V.A.; Davies, E.J.; Coats, A.J.; Dalal, H.; Rees, K.; Singh, S.J.; Taylor, R.S.; et al. Exercise-based cardiac rehabilitation for adults with heart failure. Cochrane Database Syst. Rev. 2019, 1, Cd003331. [Google Scholar] [CrossRef] [PubMed]
- Thomas, R.J.; Balady, G.; Banka, G.; Beckie, T.M.; Chiu, J.; Gokak, S.; Ho, P.M.; Keteyian, S.J.; King, M.; Lui, K.; et al. 2018 ACC/AHA Clinical Performance and Quality Measures for Cardiac Rehabilitation: A Report of the American College of Cardiology/American Heart Association Task Force on Performance Measures. J. Am. Coll. Cardiol. 2018, 71, 1814–1837. [Google Scholar] [CrossRef] [PubMed]
- Piepoli, M.F.; Corra, U.; Adamopoulos, S.; Benzer, W.; Bjarnason-Wehrens, B.; Cupples, M.; Dendale, P.; Doherty, P.; Gaita, D.; Hofer, S.; et al. Secondary prevention in the clinical management of patients with cardiovascular diseases. Core components, standards and outcome measures for referral and delivery: A policy statement from the cardiac rehabilitation section of the European Association for Cardiovascular Prevention & Rehabilitation. Endorsed by the Committee for Practice Guidelines of the European Society of Cardiology. Eur. J. Prev. Cardiol. 2014, 21, 664–681. [Google Scholar] [PubMed]
- Abreu, A.; Frederix, I.; Dendale, P.; Janssen, A.; Doherty, P.; Piepoli, M.F.; Völler, H.; Davos, C.H. Standardization and quality improvement of secondary prevention through cardiovascular rehabilitation programmes in Europe: The avenue towards EAPC accreditation programme: A position statement of the Secondary Prevention and Rehabilitation Section of the European Association of Preventive Cardiology (EAPC). Eur. J. Prev. Cardiol. 2020. [Google Scholar] [CrossRef]
- Thomas, R.J.; Beatty, A.L.; Beckie, T.M.; Brewer, L.C.; Brown, T.M.; Forman, D.E.; Franklin, B.A.; Keteyian, S.J.; Kitzman, D.W.; Regensteiner, J.G.; et al. Home-Based Cardiac Rehabilitation: A Scientific Statement From the American Association of Cardiovascular and Pulmonary Rehabilitation, the American Heart Association, and the American College of Cardiology. Circulation 2019, 140, e69–e89. [Google Scholar] [CrossRef]
- Scherrenberg, M.; Wilhelm, M.; Hansen, D.; Völler, H.; Cornelissen, V.; Frederix, I.; Kemps, H.; Dendale, P. The future is now: A call for action for cardiac telerehabilitation in the COVID-19 pandemic from the secondary prevention and rehabilitation section of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 2020. [Google Scholar] [CrossRef]
- Buckingham, S.A.; Taylor, R.S.; Jolly, K.; Zawada, A.; Dean, S.G.; Cowie, A.; Norton, R.J.; Dalal, H.M. Home-based versus centre-based cardiac rehabilitation: Abridged Cochrane systematic review and meta-analysis. Open Heart 2016, 3, e000463. [Google Scholar] [CrossRef]
- Dalal, H.M.; Zawada, A.; Jolly, K.; Moxham, T.; Taylor, R.S. Home based versus centre based cardiac rehabilitation: Cochrane systematic review and meta-analysis. BMJ (Clin. Res. Ed.) 2010, 340, b5631. [Google Scholar] [CrossRef]
- Anderson, L.; Sharp, G.A.; Norton, R.J.; Dalal, H.; Dean, S.G.; Jolly, K.; Cowie, A.; Zawada, A.; Taylor, R.S. Home-based versus centre-based cardiac rehabilitation. Cochrane Database Syst. Rev. 2017, 6, Cd007130. [Google Scholar] [CrossRef]
- Marchionni, N.; Fattirolli, F.; Fumagalli, S.; Oldridge, N.; Del Lungo, F.; Morosi, L.; Burgisser, C.; Masotti, G. Improved Exercise Tolerance and Quality of Life With Cardiac Rehabilitation of Older Patients After Myocardial Infarction. Circulation 2003, 107, 2201–2206. [Google Scholar] [CrossRef]
- Cowie, A.; Thow, M.K.; Granat, M.H.; Mitchell, S.L. A comparison of home and hospital-based exercise training in heart failure: Immediate and long-term effects upon physical activity level. Eur. J. Cardiovasc. Prev. Rehabil. 2011, 18, 158–166. [Google Scholar] [CrossRef] [PubMed]
- Kraal, J.J.; Peek, N.; Van den Akker-Van Marle, M.E.; Kemps, H.M.C. Effects of home-based training with telemonitoring guidance in low to moderate risk patients entering cardiac rehabilitation: Short-term results of the FIT@Home study. Eur. J. Prev. Cardiol. 2014, 21 (Suppl. 2), 26–31. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, D.M.; Haennel, R.G. Validity and reliability of the 6-min walk test in a cardiac rehabilitation population. J. Cardiopulm. Rehabil. 2000, 20, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Enright, P.L. The six-minute walk test. Respir. Care 2003, 48, 783–785. [Google Scholar]
- Guazzi, M.; Dickstein, K.; Vicenzi, M.; Arena, R. Six-minute walk test and cardiopulmonary exercise testing in patients with chronic heart failure: A comparative analysis on clinical and prognostic insights. Circ. Heart Fail. 2009, 2, 549–555. [Google Scholar] [CrossRef]
- ATS. Statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef]
- Jehn, M.; Schmidt-Trucksaess, A.; Schuster, T.; Hanssen, H.; Weis, M.; Halle, M.; Koehler, F. Accelerometer-based quantification of 6-min walk test performance in patients with chronic heart failure: Applicability in telemedicine. J. Card. Fail. 2009, 15, 334–340. [Google Scholar] [CrossRef]
- Ross, R.; Blair, S.N.; Arena, R.; Church, T.S.; Després, J.P.; Franklin, B.A.; Haskell, W.L.; Kaminsky, L.A.; Levine, B.D.; Lavie, C.J.; et al. Importance of Assessing Cardiorespiratory Fitness in Clinical Practice: A Case for Fitness as a Clinical Vital Sign: A Scientific Statement from the American Heart Association. Circulation 2016, 134, e653–e699. [Google Scholar] [CrossRef]
- Lang, R.M.; Badano, L.P.; Mor-Avi, V.; Afilalo, J.; Armstrong, A.; Ernande, L.; Flachskampf, F.A.; Foster, E.; Goldstein, S.A.; Kuznetsova, T.; et al. Recommendations for cardiac chamber quantification by echocardiography in adults: An update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 2015, 16, 233–270. [Google Scholar] [CrossRef]
- Russell, S.D.; Saval, M.A.; Robbins, J.L.; Ellestad, M.H.; Gottlieb, S.S.; Handberg, E.M.; Zhou, Y.; Chandler, B. New York Heart Association functional class predicts exercise parameters in the current era. Am. Heart J. 2009, 158 (Suppl. 4), S24–S30. [Google Scholar] [CrossRef]
- Casillas, J.-M.; Gudjoncik, A.; Gremeaux, V.; Aulagne, J.; Besson, D.; Laroche, D. Assessment tools for personalizing training intensity during cardiac rehabilitation: Literature review and practical proposals. Ann. Phys. Rehabil. Med. 2017, 60, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Ciani, O.; Piepoli, M.; Smart, N.; Uddin, J.; Walker, S.; Warren, F.C.; Zwisler, A.D.; Davos, C.H.; Taylor, R.S. Validation of Exercise Capacity as a Surrogate Endpoint in Exercise-Based Rehabilitation for Heart Failure: A Meta-Analysis of Randomized Controlled Trials. JACC Heart Fail. 2018, 6, 596–604. [Google Scholar] [CrossRef] [PubMed]
- Palmer, K.; Bowles, K.A.; Paton, M.; Jepson, M.; Lane, R. Chronic Heart Failure and Exercise Rehabilitation: A Systematic Review and Meta-Analysis. Arch. Phys. Med. Rehabil. 2018, 99, 2570–2582. [Google Scholar] [CrossRef] [PubMed]
- Peretti, A.; Maloberti, A.; Garatti, L.; Palazzini, M.; Triglione, N.; Occhi, L.; Sioli, S.; Sun, J.W.; Moreo, A.; Beretta, G.; et al. Functional Improvement After Outpatient Cardiac Rehabilitation in Acute Coronary Syndrome Patients is Not Related to Improvement in Left Ventricular Ejection Fraction. High Blood Press Cardiovasc. Prev. 2020, 27, 225–230. [Google Scholar] [CrossRef]
- Bellet, R.N.; Francis, R.L.; Jacob, J.S.; Healy, M.; Bartlett, H.J.; Adams, L.; Morris, N.R. Repeated six-minute walk tests for outcome measurement and exercise prescription in outpatient cardiac rehabilitation: A longitudinal study. Arch. Phys. Med. Rehabil. 2011, 92, 1388–1394. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.M.; Lu, Y.; Tang, Y.; Yang, D.; Wu, H.F.; Bian, Z.P.; Xu, J.D.; Gu, C.R.; Wang, L.S.; Chen, X.J. The effects of different initiation time of exercise training on left ventricular remodeling and cardiopulmonary rehabilitation in patients with left ventricular dysfunction after myocardial infarction. Disabil. Rehabil. 2016, 38, 268–276. [Google Scholar] [CrossRef]
- Frost, A.E.; Langleben, D.; Oudiz, R.; Hill, N.; Horn, E.; McLaughlin, V.; Robbins, I.M.; Shapiro, S.; Tapson, V.F.; Zwicke, D.; et al. The 6-min walk test (6MW) as an efficacy endpoint in pulmonary arterial hypertension clinical trials: Demonstration of a ceiling effect. Vasc. Pharmacol. 2005, 43, 36–39. [Google Scholar] [CrossRef]
- Ferreira, J.P.; Duarte, K.; Graves, T.L.; Zile, M.R.; Abraham, W.T.; Weaver, F.A.; Lindenfeld, J.; Zannad, F. Natriuretic Peptides, 6-Min Walk Test, and Quality-of-Life Questionnaires as Clinically Meaningful Endpoints in HF Trials. J. Am. Coll. Cardiol. 2016, 68, 2690–2707. [Google Scholar] [CrossRef]
- Gevaert, A.B.; Adams, V.; Bahls, M.; Bowen, T.S.; Cornelissen, V.; Dorr, M.; Hansen, D.; Kemps, H.M.; Leeson, P.; Van Craenenbroeck, E.M.; et al. Towards a personalised approach in exercise-based cardiovascular rehabilitation: How can translational research help? A ‘call to action’ from the Section on Secondary Prevention and Cardiac Rehabilitation of the European Association of Preventive Cardiology. Eur. J. Prev. Cardiol. 2019. [Google Scholar] [CrossRef]
- Ritchey, M.D.; Maresh, S.; McNeely, J.; Shaffer, T.; Jackson, S.L.; Keteyian, S.J.; Brawner, C.A.; Whooley, M.A.; Chang, T.; Stolp, H.; et al. Tracking Cardiac Rehabilitation Participation and Completion Among Medicare Beneficiaries to Inform the Efforts of a National Initiative. Circ. Cardiovasc. Qual. Outcomes 2020, 13, e005902. [Google Scholar] [CrossRef]
- Sutherland, N.; Harrison, A.; Doherty, P. Factors influencing change in walking ability in patients with heart failure undergoing exercise-based cardiac rehabilitation. Int. J. Cardiol. 2018, 268, 162–165. [Google Scholar] [CrossRef] [PubMed]
- Choe, Y.; Han, J.Y.; Choi, I.S.; Park, H.K. Improvement of exercise capacity in patients with type 2 diabetes mellitus during cardiac rehabilitation. Eur. J. Phys. Rehabil. Med. 2018, 54, 981–983. [Google Scholar] [CrossRef] [PubMed]
- St. Clair, M.; Mehta, H.; Sacrinty, M.; Johnson, D.; Robinson, K. Effects of Cardiac Rehabilitation in Diabetic Patients: Both Cardiac and Noncardiac Factors Determine Improvement in Exercise Capacity. Clin. Cardiol. 2014, 37, 233–238. [Google Scholar] [CrossRef] [PubMed]
- Vergès, B.; Patois-Vergès, B.; Cohen, M.; Lucas, B.; Galland-Jos, C.; Casillas, J.M. Effects of cardiac rehabilitation on exercise capacity in Type 2 diabetic patients with coronary artery disease. Diabet. Med. 2004, 21, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Kemps, H.; Kränkel, N.; Dörr, M.; Moholdt, T.; Wilhelm, M.; Paneni, F.; Serratosa, L.; Ekker Solberg, E.; Hansen, D.; Halle, M.; et al. Exercise training for patients with type 2 diabetes and cardiovascular disease: What to pursue and how to do it. A Position Paper of the European Association of Preventive Cardiology (EAPC). Eur. J. Prev. Cardiol. 2019, 26, 709–727. [Google Scholar] [CrossRef]
- Cahalin, L.P.; Arena, R.; Labate, V.; Bandera, F.; Lavie, C.J.; Guazzi, M. Heart rate recovery after the 6 min walk test rather than distance ambulated is a powerful prognostic indicator in heart failure with reduced and preserved ejection fraction: A comparison with cardiopulmonary exercise testing. Eur. J. Heart Fail. 2013, 15, 519–527. [Google Scholar] [CrossRef]
- De Cannière, H.; Smeets, C.J.P.; Schoutteten, M.; Varon, C.; Van Hoof, C.; Van Huffel, S.; Groenendaal, W.; Vandervoort, P. Using Biosensors and Digital Biomarkers to Assess Response to Cardiac Rehabilitation: Observational Study. J. Med Internet Res. 2020, 22, e17326. [Google Scholar] [CrossRef]
- Du, H.; Wonggom, P.; Tongpeth, J.; Clark, R.A. Six-Minute Walk Test for Assessing Physical Functional Capacity in Chronic Heart Failure. Curr. Heart Fail. Rep. 2017, 14, 158–166. [Google Scholar] [CrossRef]
- Giannitsi, S.; Bougiakli, M.; Bechlioulis, A.; Kotsia, A.; Michalis, L.K.; Naka, K.K. 6-min walking test: A useful tool in the management of heart failure patients. Ther. Adv. Cardiovasc. Dis. 2019, 13, 1753944719870084. [Google Scholar] [CrossRef]
- Olsson, L.G.; Swedberg, K.; Clark, A.L.; Witte, K.K.; Cleland, J.G. Six minute corridor walk test as an outcome measure for the assessment of treatment in randomized, blinded intervention trials of chronic heart failure: A systematic review. Eur. Heart J. 2005, 26, 778–793. [Google Scholar] [CrossRef]
| Variable | Total Population (n = 129) |
|---|---|
| Demographics | |
| Male | 92 (71.3%) |
| Age, years >65 years | 63 (11) 55 (42%) |
| Height, m | 1.72 (1.70–1.74) |
| BMI, kg/m2 | 27.2 (5.0) |
| Active smoker | 28 (22%) |
| Past smoker | 47 (37%) |
| LV ejection fraction baseline, % | 45 (42–47) |
| LV ejection fraction final, % | 50 (47–53) |
| CRT, % | 26 (20%) |
| CRT-D | 15 (58%) |
| CRT-P | 11 (42%) |
| Reason of referral | |
| MI, % HF, % | 32 (24.8%) |
| 38 (29.5%) | |
| CABG, % | 17 (13.2%) |
| PCI, % | 15 (11.6%) |
| Other, % | 27 (20.9%) |
| Comorbidities | |
| Atrial fibrillation | 33 (25.6%) |
| Hypertension | 60 (46.5%) |
| Dyslipidemia | 53 (41.1%) |
| Diabetes | 21 (16.3%) |
| NYHA class | |
| Class I | 36 (27.9%) |
| Class II | 60 (46.5%) |
| Class III | 33 (25.6%) |
| Medications | |
| ACE inhibitor | 67 (51.9%) |
| Beta-blocker | 97 (75.2%) |
| Diuretics | 66 (51.2%) |
| Statins | 93 (72%) |
| Calcium-channel blockers | 10 (8%) |
| Anticoagulants | 42(32%) |
| Baseline CPET (n = 101) | |
| Peak VO2, mL/kg/min | 16.21 (5.33) |
| Percent predicted peak VO2, % | 58 (19) |
| Peak power, watts | 109 (102–115) |
| Respiratory exchange ratio | 1.09 (1.08) |
| Baseline 6MWT | |
| Distance, m | 468 (104) |
| Rest HR, bpm | 68 (65–70) |
| Rest blood pressure, mmHg | 127/75 (19/11) |
| SF-36 Scores (Baseline—End-of-Study) | Mean (SD) | 95% CI | t-Value | p-Value | Effect Size |
|---|---|---|---|---|---|
| Physical Functioning | −14.09 (19.22) | −18.58 to −9.61 | −6.26 | ≤0.001 | −0.73 |
| Role Physical | −27.41 (46.99) | −38.22 to −16.60 | −5.05 | ≤0.001 | −0.58 |
| Role Emotional | −14.02 (42.71) | −25.35 to −2.69 | −2.48 | 0.016 | −0.33 |
| Vitality | −13.22 (17.85) | −17.30 to −9.13 | −6.45 | ≤0.001 | −0.74 |
| Mental Health | −9.20 (15.44) | −12.73 to −5.67 | −5.20 | ≤0.001 | −0.60 |
| Social Functioning | −20.31 (21.67) | −26.61 to −14.02 | −6.50 | ≤0.001 | −0.94 |
| Bodily Pain | −10.44 (24.47) | −17.39 to −3.49 | −3.02 | 0.004 | −0.43 |
| General Health | −2.61 (17.72) | −8.89 to 3.67 | −0.85 | 0.404 | −0.15 |
| Baseline | 1st Follow-Up | 2nd Follow-Up | 3rd Follow-Up | End-of-Study | |
|---|---|---|---|---|---|
| Distance, m | 484 (96) | 533 (100) | 564 (100) | 570 (103) | 585 (104) |
| HR start 6MWT | 66 (57–80) | 67 (57–73) | 65 (58–72) | 64 (55–70) | 62 (55–72) |
| HR end 6MWT | 85 (73–94) | 86 (77–96) | 85 (77–103) | 89 (80–99) | 89 (79–104) |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
De Cannière, H.; Smeets, C.J.P.; Schoutteten, M.; Varon, C.; Morales Tellez, J.F.; Van Hoof, C.; Van Huffel, S.; Groenendaal, W.; Vandervoort, P. Short-Term Exercise Progression of Cardiovascular Patients throughout Cardiac Rehabilitation: An Observational Study. J. Clin. Med. 2020, 9, 3160. https://doi.org/10.3390/jcm9103160
De Cannière H, Smeets CJP, Schoutteten M, Varon C, Morales Tellez JF, Van Hoof C, Van Huffel S, Groenendaal W, Vandervoort P. Short-Term Exercise Progression of Cardiovascular Patients throughout Cardiac Rehabilitation: An Observational Study. Journal of Clinical Medicine. 2020; 9(10):3160. https://doi.org/10.3390/jcm9103160
Chicago/Turabian StyleDe Cannière, Hélène, Christophe J. P. Smeets, Melanie Schoutteten, Carolina Varon, John F. Morales Tellez, Chris Van Hoof, Sabine Van Huffel, Willemijn Groenendaal, and Pieter Vandervoort. 2020. "Short-Term Exercise Progression of Cardiovascular Patients throughout Cardiac Rehabilitation: An Observational Study" Journal of Clinical Medicine 9, no. 10: 3160. https://doi.org/10.3390/jcm9103160
APA StyleDe Cannière, H., Smeets, C. J. P., Schoutteten, M., Varon, C., Morales Tellez, J. F., Van Hoof, C., Van Huffel, S., Groenendaal, W., & Vandervoort, P. (2020). Short-Term Exercise Progression of Cardiovascular Patients throughout Cardiac Rehabilitation: An Observational Study. Journal of Clinical Medicine, 9(10), 3160. https://doi.org/10.3390/jcm9103160





