Effect of Instrument Design and Technique on the Precision and Accuracy of Objective Refraction Measurement
Abstract
:1. Introduction
2. Methods and Materials
2.1. Subjects
2.2. Instrumentation
2.3. Measurements
2.4. Statistical Analysis
3. Results
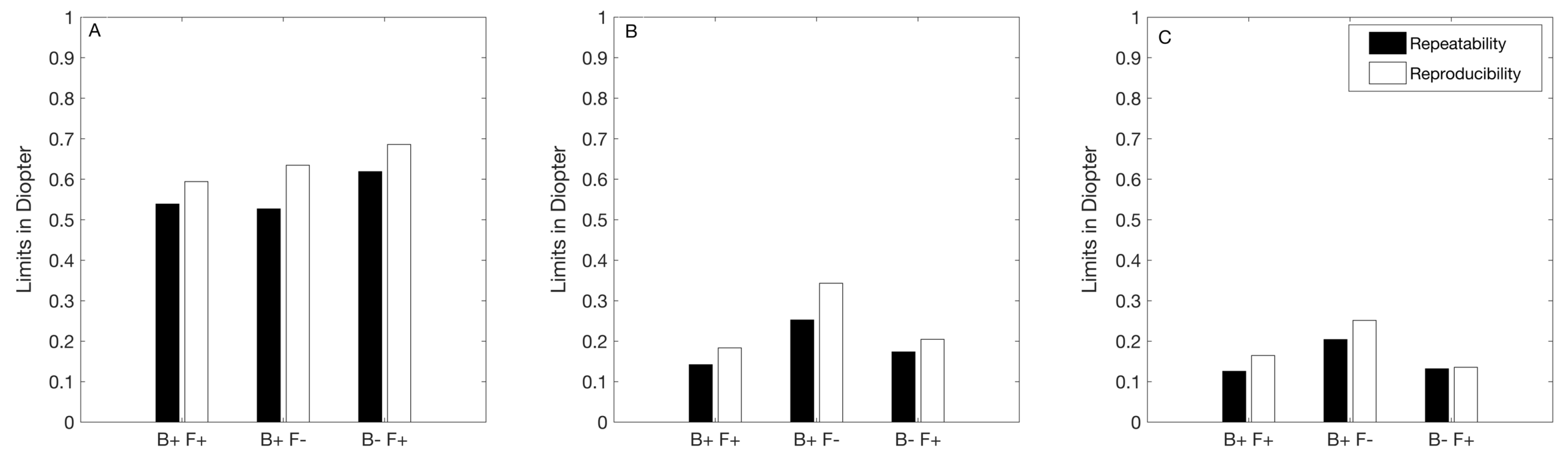
3.1. Precision
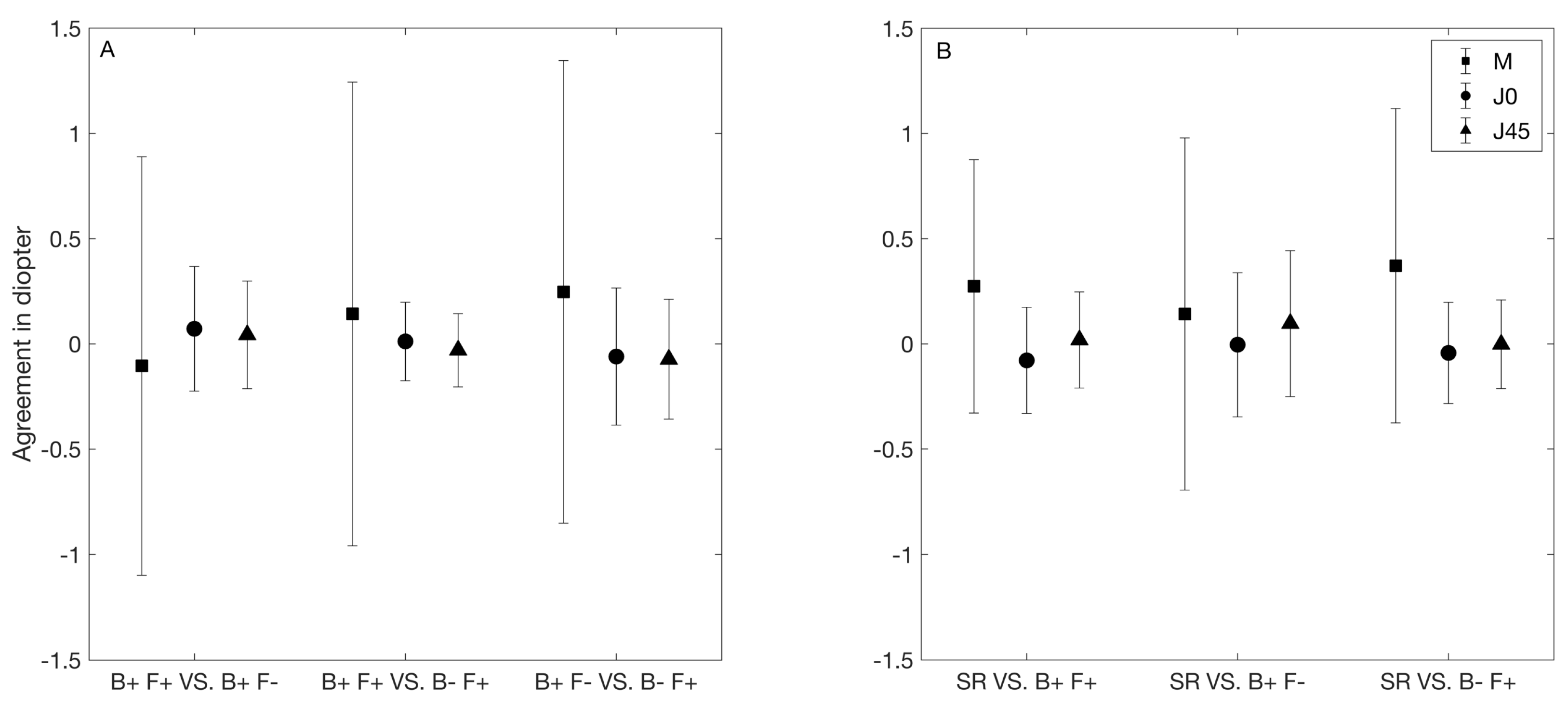
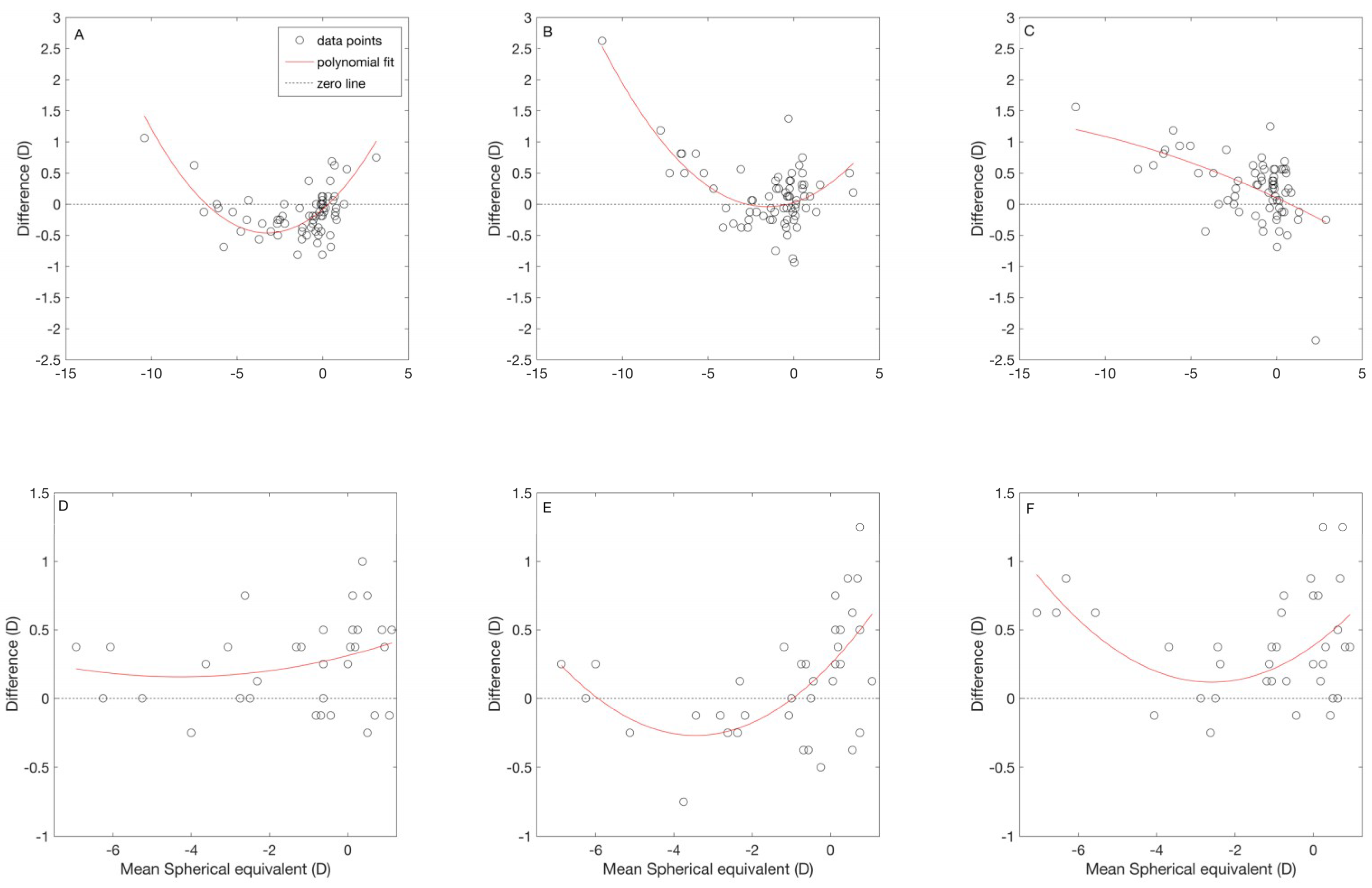
3.2. Agreement among Autorefractors
3.3. Agreement between the Subjective and Objective Refraction
4. Discussion
Author Contributions
Funding
Conflicts of Interest
References
- Fotedar, R.; Rochtchina, E.; Morgan, I.; Wang, J.J.; Mitchell, P.; Rose, K.A. Necessity of cycloplegia for assessing refractive error in 12-year-old children: A population-based study. Am. J. Ophthalmol. 2007, 144, 307–309. [Google Scholar] [CrossRef] [PubMed]
- Jorge, J.; Queiros, A.; González-Méijome, J.; Fernandes, P.; Almeida, J.B.; Parafita, M.A. The influence of cycloplegia in objective refraction. Ophthalmic Physiol. Opt. J. Br. Coll. Ophthalmic Opt. 2005, 25, 340–345. [Google Scholar] [CrossRef] [PubMed]
- Morgan, I.G.; Iribarren, R.; Fotouhi, A.; Grzybowski, A. Cycloplegic refraction is the gold standard for epidemiological studies. Acta Ophthalmol. 2015, 93, 581–585. [Google Scholar] [CrossRef]
- Sanfilippo, P.G.; Chu, B.-S.; Bigault, O.; Kearns, L.S.; Boon, M.-Y.; Young, T.L.; Hammond, C.J.; Hewitt, W.; Mackey, A. What is the appropriate age cut-off for cycloplegia in refraction? Acta Ophthalmol. 2014, 92, e458–e462. [Google Scholar] [CrossRef] [PubMed]
- Wesemann, W.; Dick, B. Accuracy and accommodation capability of a handheld autorefractor. J. Cataract. Refract. Surg. 2000, 26, 62–70. [Google Scholar] [CrossRef]
- Yassa, E.T.; Ünlü, C. Comparison of Autorefraction and Photorefraction with and without Cycloplegia Using 1% Tropicamide in Preschool Children. J. Ophthalmol. 2019, 2019, 1487013. [Google Scholar] [CrossRef]
- Carracedo, G.; Carpena-Torres, C.; Batres, L.; Serramito, M.; Gonzalez-Bergaz, A. Comparison of Two Wavefront Autorefractors: Binocular Open-Field versus Monocular Closed-Field. J. Ophthalmol. 2020, 2020, 8580471. [Google Scholar] [CrossRef] [Green Version]
- Xiong, S.; Lv, M.; Zou, H.; Zhu, J.; Lu, L.; Zhang, B.; Deng, J.; Yao, C.; He, X.; Xu, X.; et al. Comparison of Refractive Measures of Three Autorefractors in Children and Adolescents. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom. 2017, 94, 894–902. [Google Scholar] [CrossRef] [Green Version]
- Elliott, D.B. What is the appropriate gold standard test for refractive error? Ophthalmic Physiol. Opt. J. Br. Coll. Ophthalmic Opt. 2017, 37, 115–117. [Google Scholar] [CrossRef] [Green Version]
- Gwiazda, J.; Weber, C. Comparison of spherical equivalent refraction and astigmatism measured with three different models of autorefractors. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom. 2004, 81, 56–61. [Google Scholar] [CrossRef]
- Zhao, J.; Mao, J.; Luo, R.; Li, F.; Pokharel, G.P.; Ellwein, L.B. Accuracy of noncycloplegic autorefraction in school-age children in China. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom. 2004, 81, 49–55. [Google Scholar] [CrossRef] [PubMed]
- McAlinden, C.; Khadka, J.; Pesudovs, K. Statistical methods for conducting agreement (comparison of clinical tests) and precision (repeatability or reproducibility) studies in optometry and ophthalmology. Ophthalmic Physiol. Opt. J. Br. Coll. Ophthalmic Opt. 2011, 31, 330–338. [Google Scholar] [CrossRef] [PubMed]
- Carracedo, G.; Carpena-Torres, C.; Serramito, M.; Batres-Valderas, L.; Gonzalez-Bergaz, A. Comparison Between Aberrometry-Based Binocular Refraction and Subjective Refraction. Transl. Vis. Sci. Technol. 2018, 7, 11. [Google Scholar] [CrossRef] [Green Version]
- Davies, L.N.; Mallen, E.A.H.; Wolffsohn, J.S.; Gilmartin, B. Clinical Evaluation of the Shin-Nippon NVision-K 5001/Grand Seiko WR-5100K Autorefractor. Optom. Vis. Sci. 2003, 80. Available online: https://journals.lww.com/optvissci/Fulltext/2003/04000/Clinical_Evaluation_of_the_Shin_Nippon_NVision_K.11.aspx (accessed on 22 September 2020). [CrossRef] [PubMed]
- Wolffsohn, J.S.; Davies, L.N.; Naroo, S.A.; Buckhurst, P.J.; Gibson, G.A.; Gupta, N.; Craig, J.P.; Shah, S. Evaluation of an open-field autorefractor’s ability to measure refraction and hence potential to assess objective accommodation in pseudophakes. Br. J. Ophthalmol. 2011, 95, 498–501. [Google Scholar] [CrossRef]
- Thibos, L.N.; Wheeler, W.; Horner, D. Power vectors: An application of Fourier analysis to the description and statistical analysis of refractive error. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom. 1997, 74, 367–375. [Google Scholar] [CrossRef]
- Tiland, J.; Altman, D. Measuring agreement in method comparison studies. Stat Methods Med. Res. 1999, 8, 135–160. [Google Scholar]
- Allen, P.M.; Radhakrishnan, H.; O’Leary, D.J. Repeatability and validity of the PowerRefractor and the Nidek AR600-A in an adult population with healthy eyes. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom. 2003, 80, 245–251. [Google Scholar] [CrossRef] [PubMed]
- Ogbuehi, K.C.; Almaliki, W.H.; AlQarni, A.; Osuagwu, U.L. Reliability and reproducibility of a handheld videorefractor. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom. 2015, 92, 632–641. [Google Scholar] [CrossRef] [Green Version]
- Paudel, N.; Adhikari, S.; Thakur, A.; Shrestha, B.; Loughman, J. Clinical Accuracy of the Nidek ARK-1 Autorefractor. Optom. Vis. Sci. Off. Publ. Am. Acad. Optom. 2019, 96, 407–413. [Google Scholar] [CrossRef]
- ISO. Probability and General Statistical Terms. Statistics: Vocabulary and Symbols; ISO 3534-1:2006; International Organization for Standardization: Geneva, Switzerland, 2006. [Google Scholar]
- ISO. Accuracy (Trueness and Precision) of Measurement Methods and Results—Part 1: General Principles and Definitions; ISO 5725-1:1994; International Organization for Standardization: Geneva, Switzerland, 1994. [Google Scholar]
- McCullough, S.J.; Little, J.-A.; Breslin, K.M.; Saunders, K.J. Comparison of Refractive Error Measures by the IRX3 Aberrometer and Autorefraction. Optom. Vis. Sci. 2014, 91. Available online: https://journals.lww.com/optvissci/Fulltext/2014/10000/Comparison_of_Refractive_Error_Measures_by_the.9.aspx (accessed on 22 September 2020). [CrossRef] [PubMed]
- Wosik, J.; Patrzykont, M.; Pniewski, J. Comparison of refractive error measurements by three different models of autorefractors and subjective refraction in young adults. J. Opt. Soc. Am. A 2019, 36, B1–B6. Available online: http://josaa.osa.org/abstract.cfm?URI=josaa-36-4-B1 (accessed on 22 September 2020). [CrossRef] [PubMed]
- Bennett, J.R.; Stalboerger, G.M.; Hodge, D.O.; Schornack, M.M. Comparison of refractive assessment by wavefront aberrometry, autorefraction, and subjective refraction. J. Optom. 2015, 8, 109–115. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Choong, Y.-F.; Chen, A.-H.; Goh, P.-P. A comparison of autorefraction and subjective refraction with and without cycloplegia in primary school children. Am. J. Ophthalmol. 2006, 142, 68–74. [Google Scholar] [CrossRef] [PubMed]

| Characteristics | Eye Refract | NVision-K 5001 | WaveAnalyzer 700 |
|---|---|---|---|
| Measurement principle | Wavefront | Retinal image size | Wavefront |
| Open/Binocular view | Yes | Yes | No |
| Simultaneous binocular measurement | Yes | No | No |
| Fogging | Yes | No | Yes |
| Acronym used in the text | B+ F+ | B+ F− | B− F+ |
| M | J0 | J45 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Measurements | 1 | 2 | 3 | 1 | 2 | 3 | 1 | 2 | 3 |
| B+ F+ | −1.30 ± 2.44 | −1.31 ± 2.47 | −1.26 ± 2.45 | 0.15 ± 0.36 | 0.16 ± 0.35 | 0.16 ± 0.36 | −0.05 ± 0.19 | −0.05 ± 0.20 | −0.05 ± 0.18 |
| B+ F- | −1.20 ± 2.40 | −1.21 ± 2.42 | −1.14 ± 2.35 | 0.08 ± 0.34 | 0.09 ± 0.35 | 0.06 ± 0.35 | −0.09 ± 0.17 | −0.10 ± 0.18 | −0.09 ± 0.16 |
| B− F+ | −1.44 ± 2.73 | −1.45 ± 2.64 | −1.38 ± 2.62 | 0.14 ± 0.37 | 0.15 ± 0.37 | 0.15 ± 0.36 | −0.02 ± 0.20 | −0.01 ± 0.21 | −0.03 ± 0.21 |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Domínguez-Vicent, A.; Al-Soboh, L.; Brautaset, R.; Venkataraman, A.P. Effect of Instrument Design and Technique on the Precision and Accuracy of Objective Refraction Measurement. J. Clin. Med. 2020, 9, 3061. https://doi.org/10.3390/jcm9103061
Domínguez-Vicent A, Al-Soboh L, Brautaset R, Venkataraman AP. Effect of Instrument Design and Technique on the Precision and Accuracy of Objective Refraction Measurement. Journal of Clinical Medicine. 2020; 9(10):3061. https://doi.org/10.3390/jcm9103061
Chicago/Turabian StyleDomínguez-Vicent, Alberto, Loujain Al-Soboh, Rune Brautaset, and Abinaya Priya Venkataraman. 2020. "Effect of Instrument Design and Technique on the Precision and Accuracy of Objective Refraction Measurement" Journal of Clinical Medicine 9, no. 10: 3061. https://doi.org/10.3390/jcm9103061
APA StyleDomínguez-Vicent, A., Al-Soboh, L., Brautaset, R., & Venkataraman, A. P. (2020). Effect of Instrument Design and Technique on the Precision and Accuracy of Objective Refraction Measurement. Journal of Clinical Medicine, 9(10), 3061. https://doi.org/10.3390/jcm9103061






