Co-Morbidities and Sex Differences in Long-Term Quality-of-Life Outcomes among Patients with and without Diabetes after Total Knee Replacement: Five-Year Data from Registry Study
Abstract
1. Introduction
2. Methods
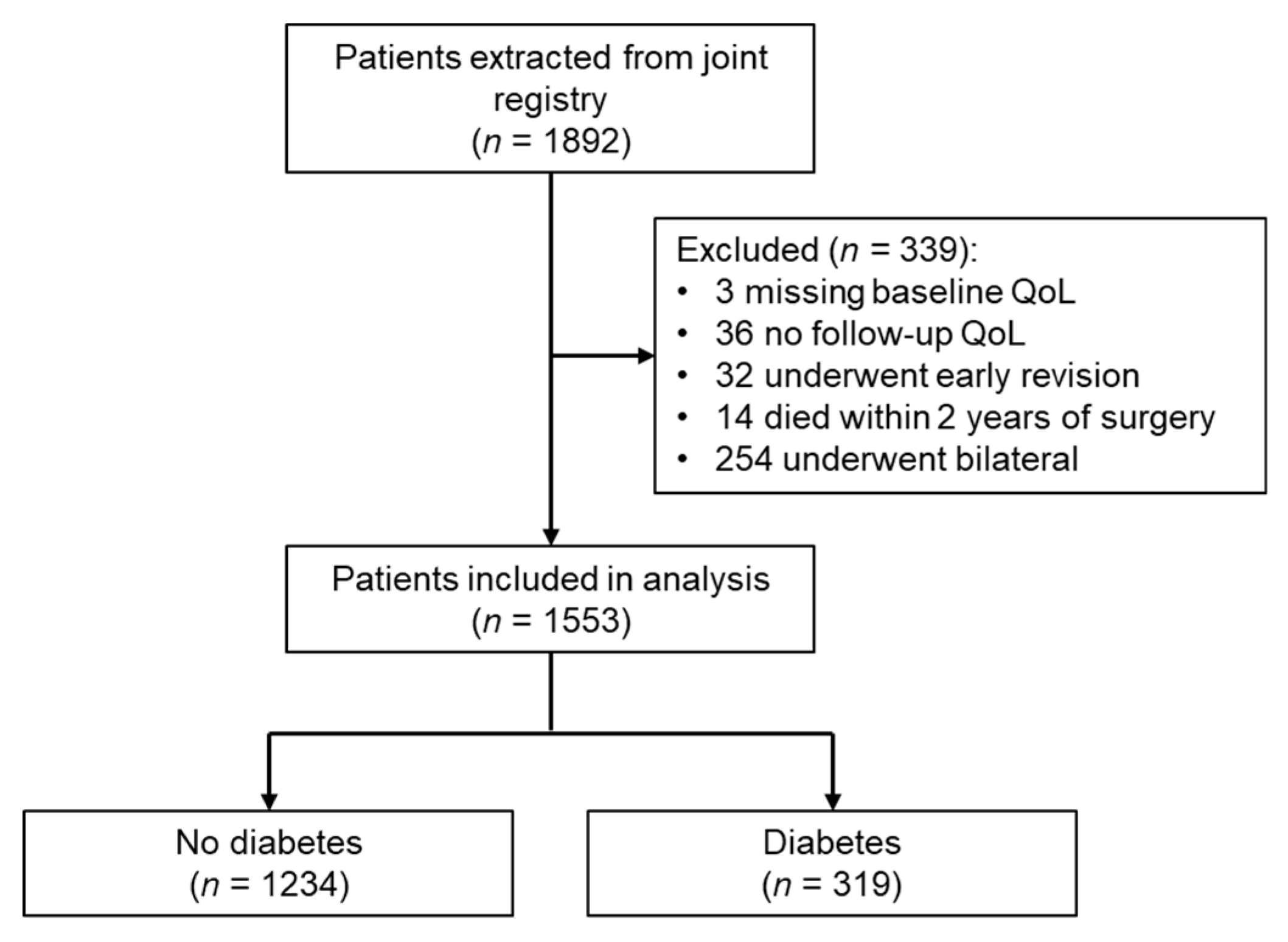
2.1. Data Source and Study Population
2.2. Quality-of-Life Measurements
2.3. Diabetes Classification
2.4. Statistical Analysis
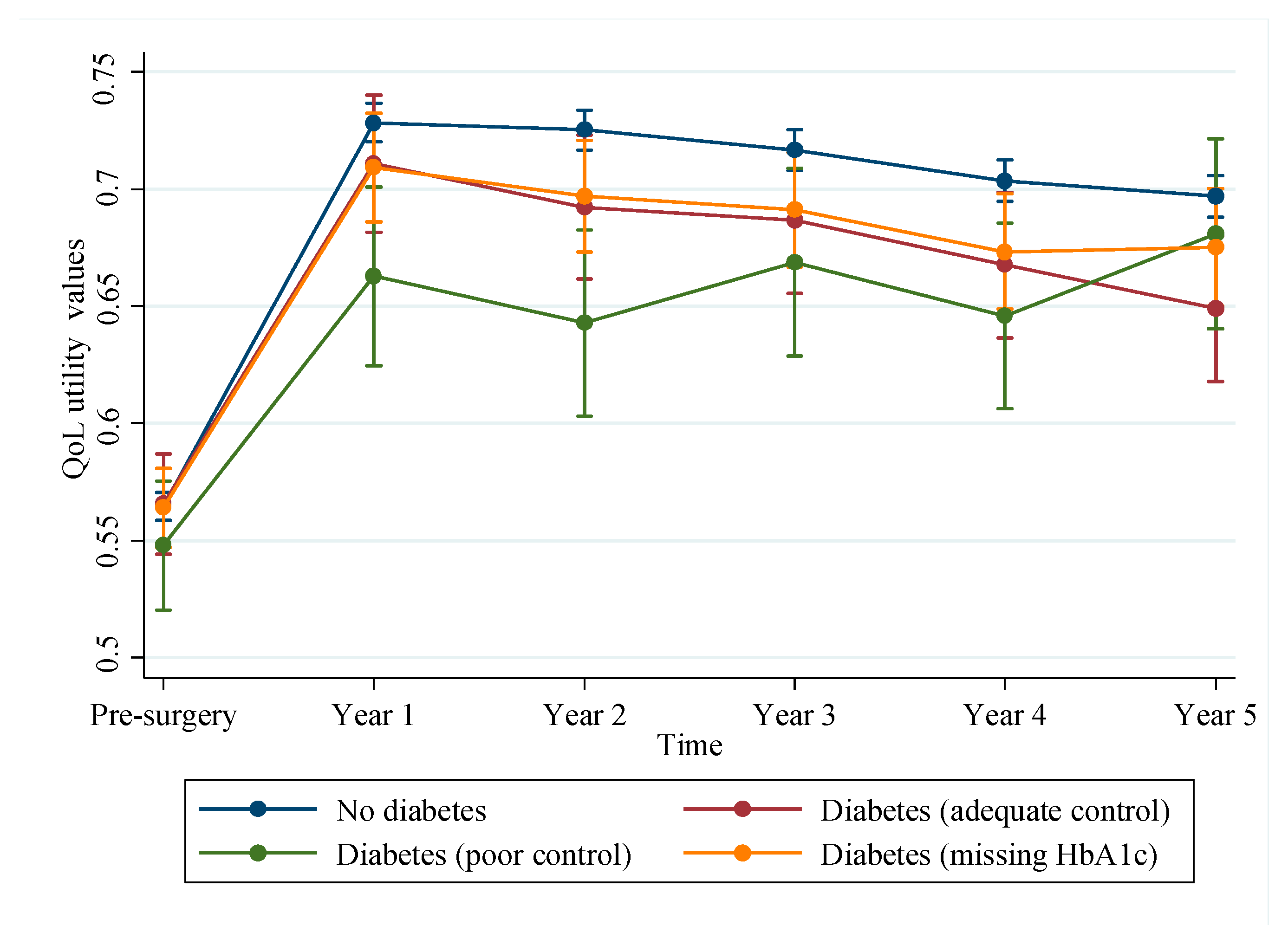
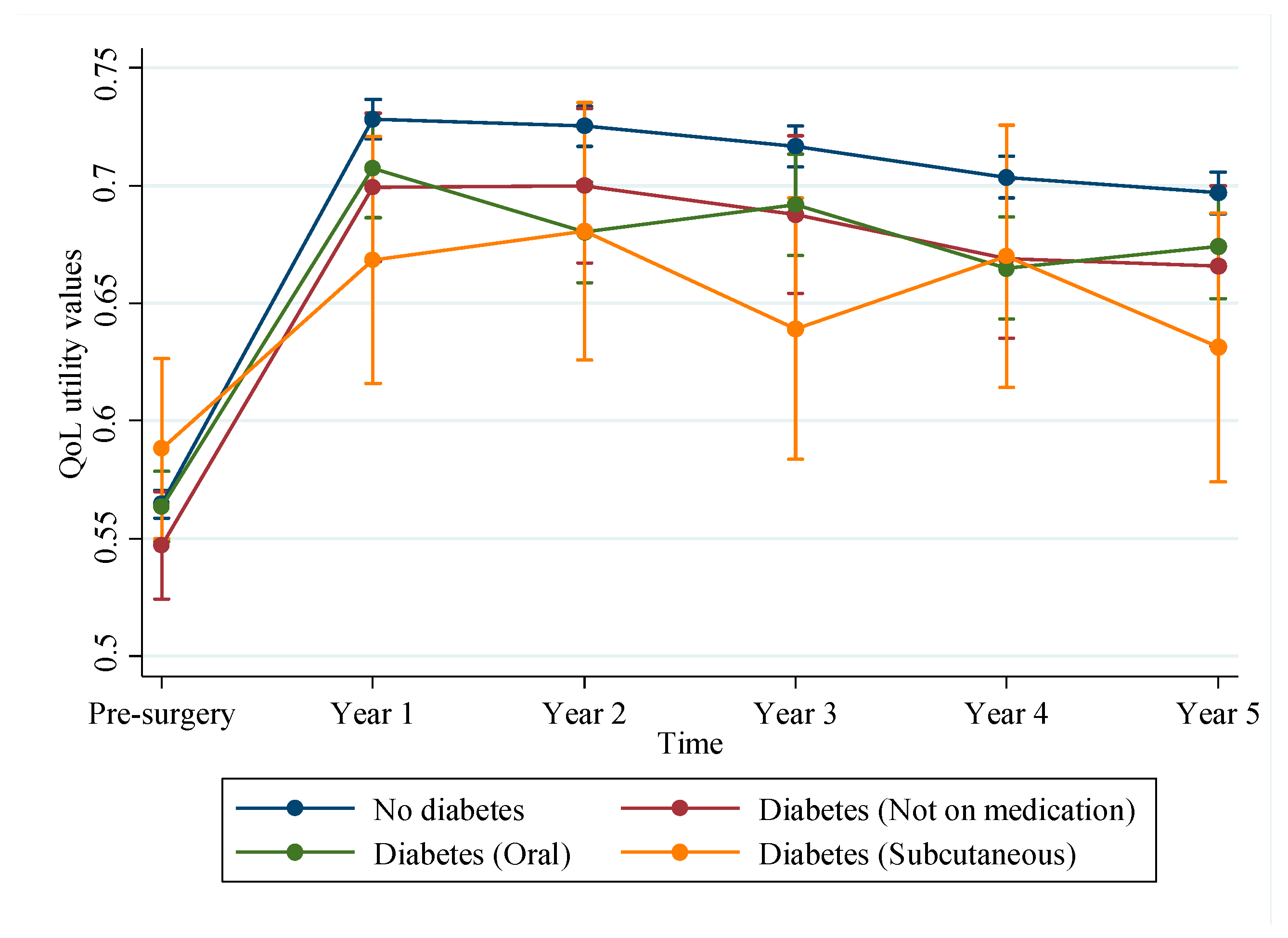
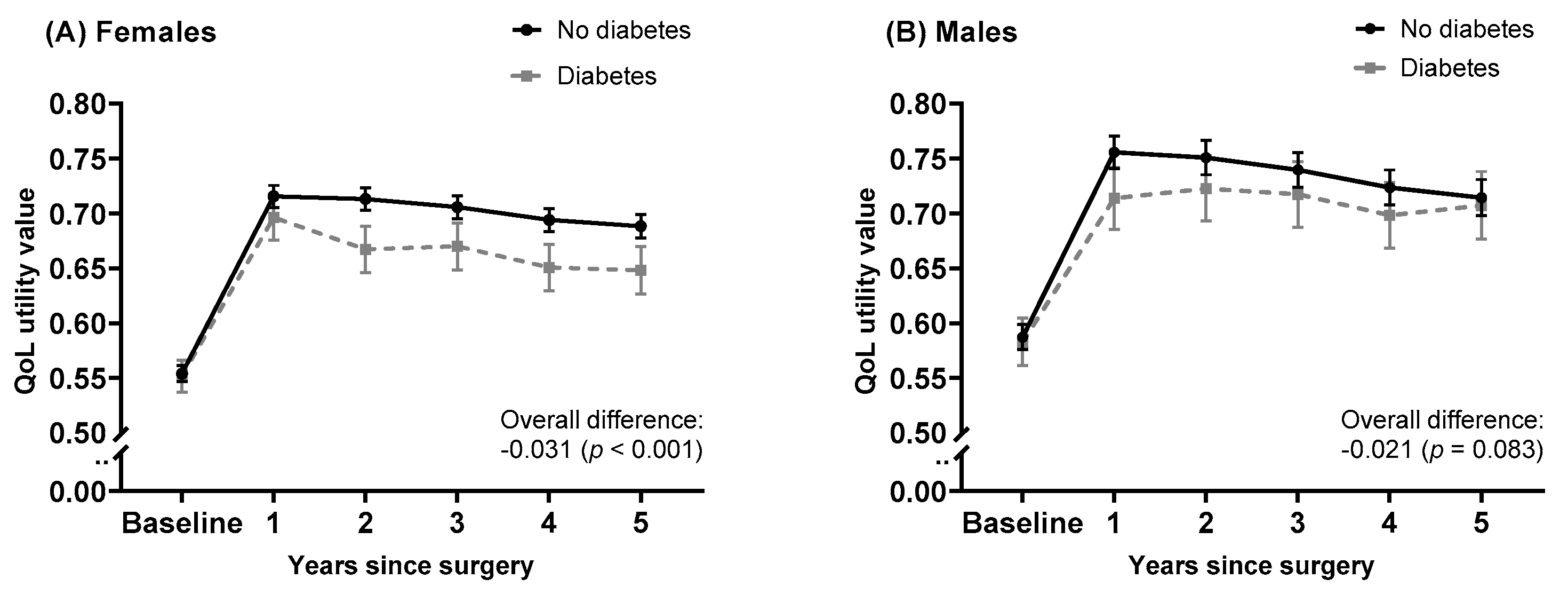
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Appendix A
References
- Cho, N.; Shaw, J.; Karuranga, S.; Huang, Y.; da Rocha Fernandes, J.; Ohlrogge, A.; Malanda, B. IDF Diabetes Atlas: Global estimates of diabetes prevalence for 2017 and projections for 2045. Diabetes Res. Clin. Pract. 2018, 138, 271–281. [Google Scholar] [CrossRef] [PubMed]
- Control, C.F.D. Prevention. Arthritis as a potential barrier to physical activity among adults with diabetes—United States, 2005 and 2007. Morb. Mortal. Wkly. Rep. 2008, 57, 486. [Google Scholar]
- Fingar, K.R.; Stocks, C.; Weiss, A.J.; Steiner, C. Most frequent operating room procedures performed in US hospitals, 2003–2012: Statistical brief# 186. In Healthcare Cost and Utilization Project (HCUP) Statistical Briefs; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2006. [Google Scholar]
- Culliford, D.; Maskell, J.; Judge, A.; Cooper, C.; Prieto-Alhambra, D.; Arden, N.; Group, C.S. Future projections of total hip and knee arthroplasty in the UK: Results from the UK Clinical Practice Research Datalink. Osteoarthr. Cartil. 2015, 23, 594–600. [Google Scholar] [CrossRef] [PubMed]
- Australian Orthopaedic Association. Hip, Knee & Shoulder Arthroplasty Annual Report 2018; AOA: Adelaide, Australia, 2018. [Google Scholar]
- Dakin, H.; Gray, A.; Fitzpatrick, R.; MacLennan, G.; Murray, D.; Group, K.T. Rationing of total knee replacement: A cost-effectiveness analysis on a large trial data set. BMJ Open 2012, 2, e000332. [Google Scholar] [CrossRef]
- Dowsey, M.; Smith, A.; Choong, P. Latent class growth analysis predicts long term pain and function trajectories in total hip arthroplasty: A study of 605 consecutive patients. Osteoarthr. Cartil. 2015, 23, A340–A341. [Google Scholar] [CrossRef][Green Version]
- Schilling, C.; Dowsey, M.M.; Clarke, P.M.; Choong, P.F. Using patient-reported outcomes for economic evaluation: Getting the timing right. Value Health 2016, 19, 945–950. [Google Scholar] [CrossRef]
- Wexler, D.J.; Grant, R.W.; Wittenberg, E.; Bosch, J.L.; Cagliero, E.; Delahanty, L.; Blais, M.A.; Meigs, J.B. Correlates of health-related quality of life in type 2 diabetes. Diabetologia 2006, 49, 1489–1497. [Google Scholar] [CrossRef]
- Association, A.D. Quality of life in type 2 diabetic patients is affected by complications but not by intensive policies to improve blood glucose or blood pressure control (UKPDS 37). UK Prospective Diabetes Study Group. Diabetes Care 1999, 22, 1125–1136. [Google Scholar]
- Clarke, P.; Gray, A.; Holman, R. Estimating utility values for health states of type 2 diabetic patients using the EQ-5D (UKPDS 62). Med. Decis. Mak. 2002, 22, 340–349. [Google Scholar] [CrossRef]
- Coffey, J.T.; Brandle, M.; Zhou, H.; Marriott, D.; Burke, R.; Tabaei, B.P.; Engelgau, M.M.; Kaplan, R.M.; Herman, W.H. Valuing health-related quality of life in diabetes. Diabetes Care 2002, 25, 2238–2243. [Google Scholar] [CrossRef]
- Bolognesi, M.P.; Marchant, M.H., Jr.; Viens, N.A.; Cook, C.; Pietrobon, R.; Vail, T.P. The impact of diabetes on perioperative patient outcomes after total hip and total knee arthroplasty in the United States. J. Arthroplast. 2008, 23, 92–98. [Google Scholar] [CrossRef] [PubMed]
- Iorio, R.; Williams, K.M.; Marcantonio, A.J.; Specht, L.M.; Tilzey, J.F.; Healy, W.L. Diabetes mellitus, hemoglobin A1C, and the incidence of total joint arthroplasty infection. J. Arthroplast. 2012, 27, 726–729. [Google Scholar] [CrossRef] [PubMed]
- Kremers, H.M.; Lewallen, L.W.; Mabry, T.M.; Berry, D.J.; Berbari, E.F.; Osmon, D.R. Diabetes mellitus, hyperglycemia, hemoglobin A1C and the risk of prosthetic joint infections in total hip and knee arthroplasty. J. Arthroplast. 2015, 30, 439–443. [Google Scholar] [CrossRef] [PubMed]
- Meding, J.B.; Reddleman, K.; Keating, M.E.; Klay, A.; Ritter, M.A.; Faris, P.M.; Berend, M.E. Total knee replacement in patients with diabetes mellitus. Clin. Orthop. Relat. Res. 2003, 416, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Adams, A.L.; Paxton, E.W.; Wang, J.Q.; Johnson, E.S.; Bayliss, E.A.; Ferrara, A.; Nakasato, C.; Bini, S.A.; Namba, R.S. Surgical outcomes of total knee replacement according to diabetes status and glycemic control, 2001 to 2009. J. Bone Jt. Surg. Am. 2013, 95, 481–487. [Google Scholar] [CrossRef]
- Clement, N.D.; MacDonald, D.; Burnett, R.; Breusch, S.J. Diabetes does not influence the early outcome of total knee replacement: A prospective study assessing the Oxford knee score, short form 12, and patient satisfaction. Knee 2013, 20, 437–441. [Google Scholar] [CrossRef]
- Black, N. Patient reported outcome measures could help transform healthcare. BMJ 2013, 346, f167. [Google Scholar] [CrossRef]
- Statistics, A.B.O. Information Paper: An Introduction to Socio-Economic Indexes for Areas (SEIFA)-2039.0. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/mf/2039.0 (accessed on 10 May 2019).
- Statistics, A.B.O. Australian Statistical Geography Standard (ASGS): Volume 5—Remoteness Structure—1270.0.55.005. Available online: http://www.abs.gov.au/ausstats/abs@.nsf/mf/1270.0.55.005?OpenDocument (accessed on 10 May 2019).
- Brazier, J.E.; Roberts, J. The estimation of a preference-based measure of health from the SF-12. Med. Care 2004, 42, 851–859. [Google Scholar] [CrossRef]
- Griffiths, A.; Paracha, N.; Davies, A.; Branscombe, N.; Cowie, M.R.; Sculpher, M. Analyzing health-related quality of life data to estimate parameters for cost-effectiveness models: An example using longitudinal EQ-5D data from the SHIFT randomized controlled trial. Adv. Ther. 2017, 34, 753–764. [Google Scholar] [CrossRef]
- Raudenbush, S.W.; Bryk, A.S. Hierarchical Linear Models: Applications and Data Analysis Methods; Sage: Thousand Oaks, CA, USA, 2002; Volume 1. [Google Scholar]
- Mitchell, M.N. Interpreting and Visualizing Regression Models using STATA; Stata Press College Station: College Station, TX, USA, 2012. [Google Scholar]
- Robertson, F.; Geddes, J.; Ridley, D.; McLeod, G.; Cheng, K. Patients with Type 2 diabetes mellitus have a worse functional outcome post knee arthroplasty: A matched cohort study. Knee 2012, 19, 286–289. [Google Scholar] [CrossRef]
- Singh, J.A.; Lewallen, D.G. Diabetes: A risk factor for poor functional outcome after total knee arthroplasty. PLoS ONE 2013, 8, e78991. [Google Scholar] [CrossRef] [PubMed]
- Foy, C.G.; Lewis, C.E.; Hairston, K.G.; Miller, G.D.; Lang, W.; Jakicic, J.M.; Rejeski, W.J.; Ribisl, P.M.; Walkup, M.P.; Wagenknecht, L.E. Intensive lifestyle intervention improves physical function among obese adults with knee pain: Findings from the Look AHEAD trial. Obesity 2011, 19, 83–93. [Google Scholar] [CrossRef] [PubMed]
- Nicolucci, A.; Balducci, S.; Cardelli, P.; Cavallo, S.; Fallucca, S.; Bazuro, A.; Simonelli, P.; Iacobini, C.; Zanuso, S.; Pugliese, G.; et al. Relationship of exercise volume to improvements of quality of life with supervised exercise training in patients with type 2 diabetes in a randomised controlled trial: The Italian Diabetes and Exercise Study (IDES). Diabetologia 2012, 55, 579–588. [Google Scholar] [CrossRef] [PubMed]
- Jaeschke, R.; Singer, J.; Guyatt, G.H. Measurement of health status. Ascertaining the minimal clinically important difference. Control Clin. Trials 1989, 10, 407–415. [Google Scholar] [CrossRef]
- Walters, S.J.; Brazier, J.E. What is the relationship between the minimally important difference and health state utility values? The case of the SF-6D. Health Qual. Life Outcomes 2003, 1, 4. [Google Scholar] [CrossRef] [PubMed]
- Gall, S.L.; Tran, P.L.; Martin, K.; Blizzard, L.; Srikanth, V. Sex differences in long-term outcomes after stroke: Functional outcomes, handicap, and quality of life. Stroke 2012, 43, 1982–1987. [Google Scholar] [CrossRef] [PubMed]
- Gall, S.; Phan, H.; Madsen, T.E.; Reeves, M.; Rist, P.; Jimenez, M.; Lichtman, J.; Dong, L.; Lisabeth, L.D. Focused update of sex differences in patient reported outcome measures after stroke. Stroke 2018, 49, 531–535. [Google Scholar] [CrossRef]
- Hekmat, K.; Jacobsson, L.T.; Nilsson, J.-Å.; Lindroth, Y.; Turesson, C. Changes and sex differences in patient reported outcomes in rheumatoid factor positive RA–results from a community based study. BMC Musculoskelet. Disord. 2014, 15, 44. [Google Scholar] [CrossRef]
- Robb, J.C.; Young, L.T.; Cooke, R.G.; Joffe, R.T. Gender differences in patients with bipolar disorder influence outcome in the medical outcomes survey (SF-20) subscale scores. J. Affect. Disord. 1998, 49, 189–193. [Google Scholar] [CrossRef]
- Rosseland, L.A.; Stubhaug, A. Gender is a confounding factor in pain trials: Women report more pain than men after arthroscopic surgery. Pain 2004, 112, 248–253. [Google Scholar] [CrossRef]
- Tonelli, S.M.; Rakel, B.A.; Cooper, N.A.; Angstom, W.L.; Sluka, K.A. Women with knee osteoarthritis have more pain and poorer function than men, but similar physical activity prior to total knee replacement. Biol. Sex Differ. 2011, 2, 12. [Google Scholar] [CrossRef] [PubMed]
- Neuburger, J.; Hutchings, A.; Black, N.; Van Der Meulen, J. Socioeconomic differences in patient-reported outcomes after a hip or knee replacement in the English National Health Service. J. Public Health 2012, 35, 115–124. [Google Scholar] [CrossRef] [PubMed]
- Adriaanse, M.C.; Drewes, H.W.; van der Heide, I.; Struijs, J.N.; Baan, C.A. The impact of comorbid chronic conditions on quality of life in type 2 diabetes patients. Qual. Life Res. 2016, 25, 175–182. [Google Scholar] [CrossRef] [PubMed]
- Larkin, M.E.; Walders-Abramson, N.; Hirst, K.; Keady, J.; Ievers-Landis, C.E.; Venditti, E.M.; Yasuda, P.M. Effects of comorbid conditions on health-related quality of life in youth with Type 2 diabetes: The TODAY clinical trial. Diabetes Manag. (Lond) 2015, 5, 431–439. [Google Scholar] [CrossRef]
- Dhatariya, K.; Levy, N.; Kilvert, A.; Watson, B.; Cousins, D.; Flanagan, D.; Hilton, L.; Jairam, C.; Leyden, K.; Lipp, A. NHS Diabetes guideline for the perioperative management of the adult patient with diabetes. Diabet. Med. 2012, 29, 420–433. [Google Scholar] [CrossRef]
- Akiboye, F.; Rayman, G. Management of Hyperglycemia and Diabetes in Orthopedic Surgery. Curr. Diabetes Rep. 2017, 17, 13. [Google Scholar] [CrossRef]
- Manca, A.; Hawkins, N.; Sculpher, M.J. Estimating mean QALYs in trial-based cost-effectiveness analysis: The importance of controlling for baseline utility. Health Econ. 2005, 14, 487–496. [Google Scholar] [CrossRef]
- Dowsey, M.M.; Castle, D.J.; Knowles, S.R.; Monshat, K.; Salzberg, M.R.; Choong, P.F. The effect of mindfulness training prior to total joint arthroplasty on post-operative pain and physical function: Study protocol for a randomised controlled trial. Trials 2014, 15, 208. [Google Scholar] [CrossRef]
- Marchant, M.H., Jr.; Viens, N.A.; Cook, C.; Vail, T.P.; Bolognesi, M.P. The impact of glycemic control and diabetes mellitus on perioperative outcomes after total joint arthroplasty. JBJS 2009, 91, 1621–1629. [Google Scholar] [CrossRef]
- Kurowicki, J.; Rosas, S.; Khlopas, A.; Newman, J.M.; yee Law, T.; Roche, M.W.; Higuera, C.A.; Mont, M.A. Impact of perioperative HbA1c on reimbursements in diabetes mellitus patients undergoing total hip arthroplasty: A nationwide analysis. J. Arthroplast. 2018, 33, 2038–2042. [Google Scholar] [CrossRef]
- Ahn, A.; Ferrer, C.; Park, C.; Snyder, D.J.; Maron, S.Z.; Mikhail, C.; Keswani, A.; Molloy, I.B.; Bronson, M.J.; Moschetti, W.E.; et al. Defining and Optimizing Value in Total Joint Arthroplasty from the Patient, Payer, and Provider Perspectives. J. Arthroplast. 2019, 34, 2290–2296. [Google Scholar] [CrossRef] [PubMed]
- Spertus, J.A.; Ghaferi, A.A. Transforming the National Surgical Quality Improvement Program to the Delivery of Precision Medicine to Improve the Value of Surgical Care: Summary of the John R. Clarke Keynote Address for the Surgical Outcomes Club 2016 Annual MeetingTransforming NSQIP to the Delivery of Precision MedicineTransforming NSQIP to the Delivery of Precision Medicine. Jama Surg. 2017, 152, 815–816. [Google Scholar] [CrossRef] [PubMed]
- Frisch, A.; Chandra, P.; Smiley, D.; Peng, L.; Rizzo, M.; Gatcliffe, C.; Hudson, M.; Mendoza, J.; Johnson, R.; Lin, E.; et al. Prevalence and clinical outcome of hyperglycemia in the perioperative period in noncardiac surgery. Diabetes Care 2010, 33, 1783–1788. [Google Scholar] [CrossRef] [PubMed]
- Lauruschkat, A.H.; Arnrich, B.; Albert, A.A.; Walter, J.A.; Amann, B.; Rosendahl, U.P.; Alexander, T.; Ennker, J. Prevalence and risks of undiagnosed diabetes mellitus in patients undergoing coronary artery bypass grafting. Circulation 2005, 112, 2397–2402. [Google Scholar] [CrossRef] [PubMed]
| No Diabetes | Diabetes | p-Value for Difference | |||
|---|---|---|---|---|---|
| n | % | n | % | ||
| Demographics | 1234 | 79.46 | 319 | 20.54 | |
| Age (SD) | 69.90 | 8.73 | 70.67 | 7.74 | 0.149 |
| Female | 838 | 67.96 | 209 | 65.31 | 0.416 |
| Smoking status | 0.321 | ||||
| No | 840 | 68.05 | 225 | 70.53 | |
| Ex | 303 | 24.57 | 78 | 24.45 | |
| Yes | 91 | 7.38 | 16 | 5.02 | |
| SEIFA | 0.400 | ||||
| 1–5 | 453 | 36.71 | 109 | 34.17 | |
| 6–10 | 781 | 63.29 | 210 | 65.83 | |
| Rurality | 0.093 | ||||
| Metropolitan | 1015 | 82.24 | 275 | 86.21 | |
| Regional | 219 | 17.76 | 44 | 13.79 | |
| Clinical characteristics | |||||
| BMI | <0.001 | ||||
| <30 | 449 | 36.39 | 64 | 20.06 | |
| 30–35 | 406 | 32.9 | 104 | 32.6 | |
| 35–40 | 238 | 19.29 | 104 | 32.6 | |
| 40+ | 141 | 11.43 | 47 | 14.73 | |
| Aetiology | 0.067 | ||||
| Osteoarthritis | 1148 | 93.03 | 308 | 96.55 | |
| Other * | 86 | 7.97 | 11 | 3.44 | |
| Kellgren and Lawrence score † | 0.677 | ||||
| ≤3 | 597 | 48.54 | 159 | 49.84 | |
| 4 | 633 | 51.46 | 160 | 50.16 | |
| Bilateral surgery | 196 | 15.88 | 52 | 16.3 | 0.856 |
| Reported co-morbid conditions | |||||
| Cancer | 108 | 8.75 | 20 | 6.27 | 0.151 |
| Cardiovascular | 984 | 79.74 | 297 | 93.1 | <0.001 |
| Respiratory | 225 | 18.23 | 57 | 17.87 | 0.88 |
| Mental health disorder | 223 | 18.07 | 71 | 22.26 | 0.089 |
| Pre-operative status | |||||
| ASA | <0.001 | ||||
| 1/2 | 773 | 62.64 | 128 | 40.13 | |
| 3/4 | 461 | 37.36 | 191 | 59.87 | |
| Patient-reported QoL (SD) | 0.57 | 0.11 | 0.56 | 0.11 | 0.138 |
| Description | All | Female | Male | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Coef. | 95%CI | p-Value | Coef. | 95%CI | p-Value | Coef. | 95%CI | p-Value | ||||
| Year since surgery | ||||||||||||
| 1 | 0.164 | 0.155 | 0.172 | <0.001 | 0.161 | 0.151 | 0.172 | <0.001 | 0.168 | 0.153 | 0.184 | <0.001 |
| 2 | 0.161 | 0.152 | 0.170 | <0.001 | 0.159 | 0.148 | 0.170 | <0.001 | 0.164 | 0.147 | 0.180 | <0.001 |
| 3 | 0.152 | 0.143 | 0.161 | <0.001 | 0.152 | 0.141 | 0.162 | <0.001 | 0.152 | 0.136 | 0.169 | <0.001 |
| 4 | 0.139 | 0.129 | 0.148 | <0.001 | 0.140 | 0.129 | 0.151 | <0.001 | 0.136 | 0.119 | 0.153 | <0.001 |
| 5 | 0.132 | 0.123 | 0.142 | <0.001 | 0.134 | 0.123 | 0.146 | <0.001 | 0.127 | 0.109 | 0.145 | <0.001 |
| Diabetes | −0.003 | −0.017 | 0.010 | 0.655 | −0.002 | −0.018 | 0.014 | 0.792 | −0.004 | −0.029 | 0.020 | 0.719 |
| Diabetes × year interaction | ||||||||||||
| 1#Diabetes | −0.024 | −0.043 | −0.005 | 0.015 | −0.017 | −0.041 | 0.007 | 0.159 | −0.037 | −0.071 | −0.003 | 0.031 |
| 2#Diabetes | −0.036 | −0.056 | −0.017 | <0.001 | −0.044 | −0.068 | −0.020 | <0.001 | −0.024 | −0.059 | 0.011 | 0.186 |
| 3#Diabetes | −0.028 | −0.048 | −0.008 | 0.006 | −0.033 | −0.058 | −0.009 | 0.007 | −0.018 | −0.053 | 0.018 | 0.321 |
| 4#Diabetes | −0.034 | −0.055 | −0.013 | 0.001 | −0.041 | −0.066 | −0.016 | 0.001 | −0.021 | −0.057 | 0.016 | 0.262 |
| 5#Diabetes | −0.026 | −0.047 | −0.005 | 0.016 | −0.038 | −0.063 | −0.013 | 0.003 | −0.003 | −0.041 | 0.035 | 0.892 |
| Female | −0.030 | −0.040 | −0.020 | <0.001 | - | - | - | - | - | - | - | - |
| Respiratory | −0.020 | −0.032 | −0.008 | 0.001 | −0.018 | −0.032 | −0.004 | 0.014 | −0.026 | −0.049 | −0.002 | 0.031 |
| Mental health disorder | −0.040 | −0.052 | −0.028 | <0.001 | −0.034 | −0.048 | −0.020 | <0.001 | −0.053 | −0.076 | −0.030 | <0.001 |
| ASA | ||||||||||||
| 1/2 | Ref | Ref | Ref | |||||||||
| 3/4 | −0.028 | −0.037 | −0.018 | <0.001 | −0.028 | −0.039 | −0.016 | <0.001 | −0.026 | −0.044 | −0.009 | 0.004 |
| Rurality | ||||||||||||
| Metropolitan | Ref | Ref | Ref | |||||||||
| Rural | 0.031 | 0.018 | 0.043 | <0.001 | 0.030 | 0.014 | 0.046 | <0.001 | 0.032 | 0.012 | 0.053 | 0.002 |
| Aetiology | ||||||||||||
| Osteoarthritis | Ref | Ref | Ref | |||||||||
| Other* | −0.030 | −0.049 | −0.011 | 0.002 | −0.020 | −0.042 | 0.003 | 0.083 | −0.055 | −0.093 | −0.017 | 0.005 |
| Constant | 0.601 | 0.578 | 0.623 | <0.001 | 0.571 | 0.562 | 0.581 | <0.001 | 0.607 | 0.592 | 0.621 | <0.001 |
| Random effect | ||||||||||||
| Residual standard deviation at each time point (SE) | ||||||||||||
| 0 | 0.108 | 0.002 | - | - | 0.105 | 0.002 | - | - | 0.115 | 0.004 | - | - |
| 1 | 0.148 | 0.003 | - | - | 0.147 | 0.003 | - | - | 0.150 | 0.005 | - | - |
| 2 | 0.152 | 0.003 | - | - | 0.150 | 0.003 | - | - | 0.156 | 0.005 | - | - |
| 3 | 0.153 | 0.003 | - | - | 0.152 | 0.003 | - | - | 0.155 | 0.005 | - | - |
| 4 | 0.151 | 0.003 | - | - | 0.150 | 0.003 | - | - | 0.154 | 0.005 | - | - |
| 5 | 0.152 | 0.003 | - | - | 0.150 | 0.003 | - | - | 0.156 | 0.005 | - | - |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tew, M.; Dowsey, M.M.; Choong, A.; Choong, P.F.; Clarke, P. Co-Morbidities and Sex Differences in Long-Term Quality-of-Life Outcomes among Patients with and without Diabetes after Total Knee Replacement: Five-Year Data from Registry Study. J. Clin. Med. 2020, 9, 19. https://doi.org/10.3390/jcm9010019
Tew M, Dowsey MM, Choong A, Choong PF, Clarke P. Co-Morbidities and Sex Differences in Long-Term Quality-of-Life Outcomes among Patients with and without Diabetes after Total Knee Replacement: Five-Year Data from Registry Study. Journal of Clinical Medicine. 2020; 9(1):19. https://doi.org/10.3390/jcm9010019
Chicago/Turabian StyleTew, Michelle, Michelle M. Dowsey, Annabelle Choong, Peter F. Choong, and Philip Clarke. 2020. "Co-Morbidities and Sex Differences in Long-Term Quality-of-Life Outcomes among Patients with and without Diabetes after Total Knee Replacement: Five-Year Data from Registry Study" Journal of Clinical Medicine 9, no. 1: 19. https://doi.org/10.3390/jcm9010019
APA StyleTew, M., Dowsey, M. M., Choong, A., Choong, P. F., & Clarke, P. (2020). Co-Morbidities and Sex Differences in Long-Term Quality-of-Life Outcomes among Patients with and without Diabetes after Total Knee Replacement: Five-Year Data from Registry Study. Journal of Clinical Medicine, 9(1), 19. https://doi.org/10.3390/jcm9010019





