Obstructive Sleep Apnea as a Predictor of Abnormal Heart Rate Turbulence
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Group
2.2. Study Methodology
2.3. Heart Rate Turbulence (HRT)
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
- OSA should be considered as a predictor of abnormal heart rate turbulence.
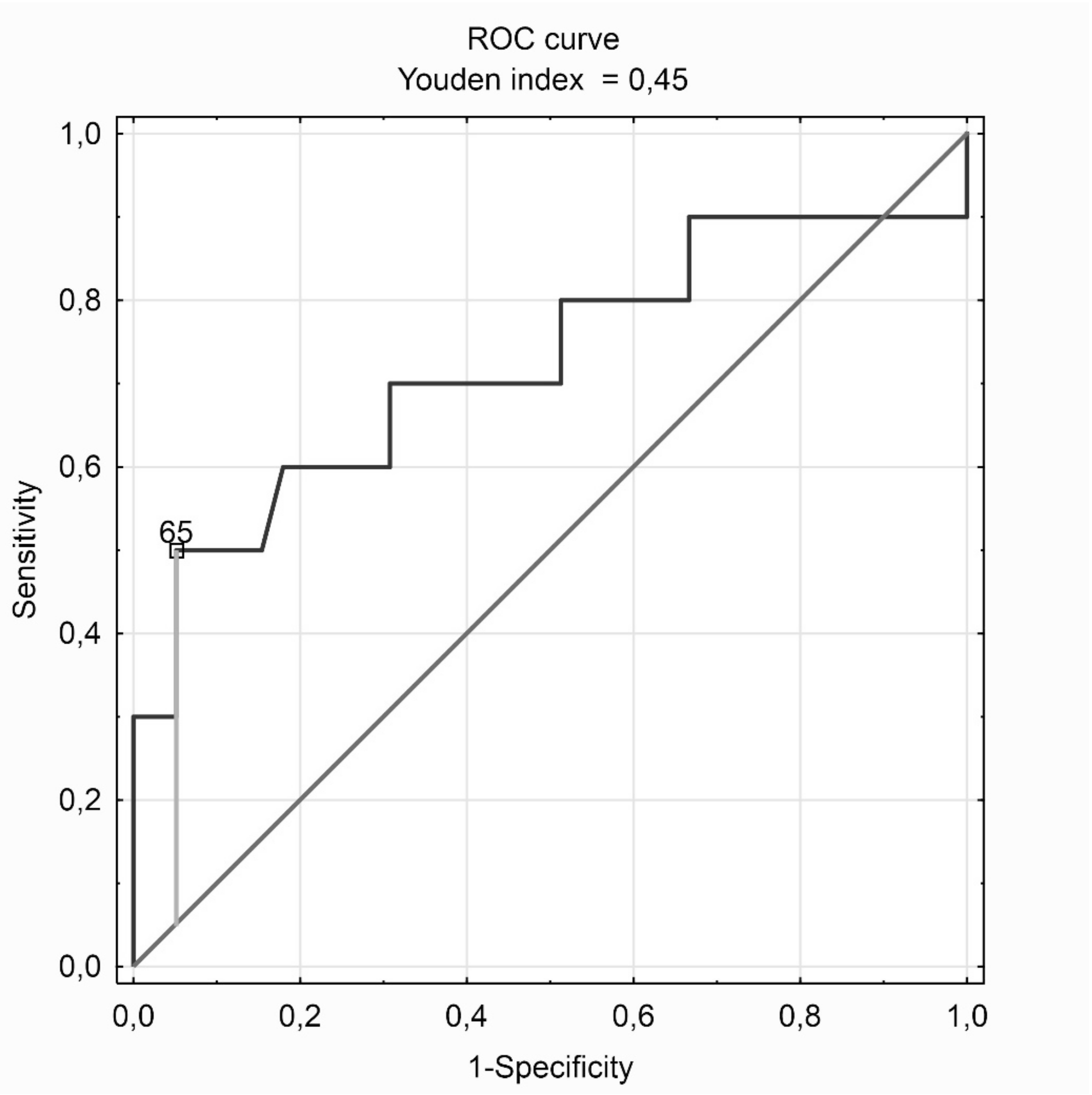
- AHI ≥65 is characterized by the highest accuracy of abnormal heart rate turbulence in both the whole study group and the subgroup of patients with confirmed OSA.
- Higher AHI values, together with older age, higher BMI values, higher blood glucose levels, diabetes and hypertension are an independent risk factor for abnormal heart rate turbulence parameters and patients with suspected OSA.
Author Contributions
Funding
Conflicts of Interest
References
- Sateia, M.J. International classification of sleep disorders-third edition: Highlights and modifications. Chest 2014, 146, 1387–1394. [Google Scholar] [CrossRef] [PubMed]
- Peppard, P.E.; Young, T.; Barnet, J.H.; Palta, M.; Hagen, E.W.; Hla, K.M. Increased prevalence of sleep-disordered breathing in adults. Am. J. Epidemiol. 2013, 177, 1006–1014. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nieto, F.J.; Young, T.B.; Lind, B.K.; Shahar, E.; Samet, J.M.; Redline, S.; D’Agostino, R.B.; Newman, A.B.; Lebowitz, M.D.; Pickering, T.G. Association of sleep-disordered breathing, sleep apnea, and hypertension in a large community-based study. Sleep Heart Health Study. JAMA 2000, 283, 1829–1836. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Sorajja, D.; Gami, A.S.; Sommers, V.K.; Behrenbeck, T.R.; Garcia-Touchard, A.; Lopez-Jimenez, F. Independent association between obstructive sleep apnea and subclinical coronary artery disease. Chest 2008, 133, 927–933. [Google Scholar] [CrossRef] [Green Version]
- Gilat, H.; Vinker, S.; Buda, I.; Soudry, E.; Shani, M.; Bachar, G. Obstructive sleep apnea and cardiovascular comorbidities a large epidemiologic study. Medicine (Baltimore) 2014, 93, e45. [Google Scholar] [CrossRef]
- Arzt, M.; Young, T.; Finn, L.; Skatrud, J.B.; Bradley, T.D. Association of sleep-disordered breathing and the occurrence of stroke. Am. J. Respir. Crit. Care Med. 2005, 172, 1447–1451. [Google Scholar] [CrossRef] [Green Version]
- Selim, B.J.; Koo, B.B.; Qin, L.; Jeon, S.; Won, C.; Redeker, N.S.; Lampert, R.J.; Concato, J.P.; Bravata, D.M.; Ferguson, J.; et al. The association between nocturnal cardiac arrhythmias and sleep-disordered breathing: The DREAM study. J. Clin. Sleep Med. 2016, 12, 829–837. [Google Scholar] [CrossRef]
- Parish, J.M.; Somers, V.K. Obstructive sleep apnea and cardiovascular disease. Mayo Clin. Proc. 2004, 79, 1036–1046. [Google Scholar] [CrossRef] [Green Version]
- Schmidt, G.; Malik, M.; Barthel, P.; Schneider, R.; Ulm, K.; Rolnitzky, L.; Camm, A.J.; Bigger, J.T., Jr.; Schömig, A. Heart rate turbulence after ventricular premature beats as a predictor of mortality after acute myocardial infarction. Lancet 1999, 9162, 1390–1396. [Google Scholar] [CrossRef] [Green Version]
- Bauer, A.; Malik, M.; Schmidt, G.; Barthel, P.; Bonnemeier, H.; Cygankiewicz, I.; Guzik, P.; Lombardi, F.; Müller, A.; Oto, A.; et al. Heart rate turbulence: Standards of measurement, physiological interpretation, and clinical use. International Society for Holter; Noninvasive Electrophysiology consensus. J. Am. Coll. Cardiol. 2008, 52, 1353–1365. [Google Scholar] [CrossRef] [Green Version]
- La Rovere, M.T.; Bigger, J.T.; Marcus, F.I.; Mortara, A.; Schwartz, P.J. Baroreflex sensitivity and heart-rate variability in prediction of total cardiac mortality after myocardial infarction. ATRAMI (Autonomic Tone and Reflexes After Myocardial Infarction) Investigators. Lancet 1998, 351, 478–484. [Google Scholar] [CrossRef]
- Ghuran, A.; Reid, F.; La Rovere, M.T.; Schmidt, G.; Bigger, J.T., Jr.; Camm, A.J.; Schwartz, P.J.; Malik, M.; Atrami Investigators. Heart rate turbulence-based predictors of fatal and nonfatal cardiac arrest (The Autonomic Tone and Reflexes After Myocardial Infarction substudy). Am. J. Cardiol. 2002, 89, 184–190. [Google Scholar] [CrossRef]
- Moore, R.K.; Groves, D.G.; Barlow, P.E.; Fox, K.A.; Shah, A.; Nolan, J.; Kearney, M.T. Heart rate turbulence and death due to cardiac decompensation in patients with chronic heart failure. Eur. J. Heart Fail. 2006, 8, 585–590. [Google Scholar] [CrossRef] [PubMed]
- Cygankiewicz, I.; Zareba, W.; Vazquez, R.; Vallverdu, M.; Gonzalez-Juanatey, J.R.; Valdes, M.; Almendral, J.; Cinca, J.; Caminal, P.; De Luna, A.B. Heart rate turbulence predicts all-cause mortality and sudden death in congestive heart failure patients. Heart Rhythm 2008, 5, 1095–1102. [Google Scholar] [CrossRef]
- Grünefeld, G.C.; Kuck, K.H.; Ptaszynski, P.; Israel, C.W.; Connolly, S.J.; Roberts, R.S.; Dorian, P.; Hohnloser, S.H. Refined risk stratification by heart rate turbulence in patients with reduced left ventricular function early after myocardial infarction: Results of the DINAMIT Holter substudy. Heart Rhythm 2005, 2, S53. [Google Scholar] [CrossRef]
- Disertori, M.; Mase, M.; Rigoni, M.; Nollo, G.; Ravelli, F. Heart rate turbulence is a powerful predictor of cardiac death and ventricular arrhythmias in postmyocardial infarction and heart failure patients a systematic review and meta-analysis. Circ. Arrhythmia Electrophysiol. 2016, 9, e004610. [Google Scholar] [CrossRef] [Green Version]
- Klingenheben, T.; Ptaszynski, P.; Hohnloser, S.H. Heart rate turbulence and other autonomic risk markers for arrhythmia risk stratification in dilated cardiomyopathy. J. Electrocardiol. 2008, 41, 306–311. [Google Scholar] [CrossRef]
- Grimm, W.; Schmidt, G.; Maisch, B.; Sharkova, J.; Müller, H.H.; Christ, M. Prognostic significance of heart rate turbulence following ventricular premature beats in patients with idiopathic dilated cardiomyopathy. J. Cardiovasc. Electrophysiol. 2003, 14, 819–824. [Google Scholar] [CrossRef] [PubMed]
- Mehra, R.; Benjamin, E.J.; Shahar, E.; Gottlieb, D.J.; Nawabit, R.; Kirchner, H.L.; Sahadevan, J.; Redline, S. Association of nocturnal arrhythmias with sleep-disordered breathing: The Sleep Heart Health Study. Am. J. Respir. Crit. Care Med. 2006, 173, 910–916. [Google Scholar] [CrossRef] [PubMed]
- Gami, A.S.; Hodge, D.O.; Herges, R.M.; Olson, E.J.; Nykodym, J.; Kara, T.; Somers, V.K. Obstructive sleep apnea, obesity, and the risk of incident atrial fibrillation. J. Am. Coll. Cardiol. 2007, 49, 565–571. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Becker, H.F.; Koehler, U.; Stammnitz, A.; Peter, J.H. Heart block in patients with sleep apnoea. Thorax 1998, 53, 29–32. [Google Scholar] [CrossRef] [Green Version]
- Gami, A.S.; Olson, E.J.; Shen, W.K.; Wright, R.S.; Ballman, K.V.; Hodge, D.O.; Herges, R.M.; Howard, D.E.; Somers, V.K. Obstructive sleep apnea and the risk of sudden cardiac death: A longitudinal study of 10,701 adults. J. Am. Coll. Cardiol. 2013, 62, 610–616. [Google Scholar] [CrossRef] [Green Version]
- Bisogni, V.; Pengo, M.F.; Maiolino, G.; Rossi, G.P. The sympathetic nervous system and catecholamines metabolism in obstructive sleep apnoea. J. Thorac. Dis. 2016, 8, 243–254. [Google Scholar]
- Yin, D.C.; Wang, Z.J.; Guo, S.; Xie, H.Y.; Sun, L.; Feng, W.; Qiu, W.; Qu, X.F. Prognostic significance of heart rate turbulence parameters in patients with chronic heart failure. BMC Cardiovasc. Disord. 2014, 14, 50. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yang, A.; Schäfer, H.; Manka, R.; Andrié, R.; Schwab, J.O.; Lewalter, T.; LüDERITZ, B.; Tasci, S. Influence of obstructive sleep apnea on heart rate turbulence. Basic Res. Cardiol. 2005, 100, 439–445. [Google Scholar] [CrossRef] [PubMed]
- Aytemir, K.; Deniz, A.; Yavuz, B.; Demir, A.U.; Sahiner, L.; Ciftci, O.; Tokgozoglu, L.; Can, I.; Sahin, A.; Oto, A. Increased myocardial vulnerability and autonomic nervous system imbalance in obstructive sleep apnea syndrome. Respir. Med. 2007, 101, 1277–1282. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zuern, C.S.; Barthel, P.; Bauer, A. Heart rate turbulence as risk-predictor after myocardial infarction. Front. Physiol. 2011, 2, 99. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Ponti, R.; Marazzato, J.; Bagliani, G.; Leonelli, F.M.; Padeletti, L. Sick Sinus Syndrome. Card. Electrophysiol. Clin. 2018, 10, 183–195. [Google Scholar] [CrossRef] [PubMed]
- Yoshihisa, A.; Suzuki, S.; Takiguchi, M.; Shimizu, T.; Abe, S.; Sato, T.; Yamaki, T.; Sugimoto, K.; Kunii, H.; Nakazato, K.; et al. Impact of sleep-disordered breathing on heart rate turbulence in heart failure patients. PLoS ONE 2014, 9, e101307. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yu, Y.; Xu, Y.; Zhang, M.; Wang, Y.; Zou, W.; Gu, Y. Value of assessing autonomic nervous function by heart rate variability and heart rate turbulence in hypertensive patients. Int. J. Hypertens 2018, 1–9. [Google Scholar] [CrossRef]
- Balcioğlu, S.; Arslan, U.; Türkoğlu, S.; Ozdemir, M.; Cengel, A. Heart rate variability and heart rate turbulence in patients with type 2 diabetes mellitus with versus without cardiac autonomic neuropathy. Am. J. Cardiol. 2007, 100, 890–893. [Google Scholar] [CrossRef] [PubMed]
- Schwab, J.O.; Eichner, G.; Shlevkov, N.; Schrickel, J.; Yang, A.; Balta, O.; Lewalter, T.; Lüderitz, B. Impact of age and basic heart rate on heart rate turbulence in healthy persons. Pacing Clin. Electrophysiol. 2005, 28, 198–201. [Google Scholar] [CrossRef]
- Mrowka, R.; Persson, P.B.; Theres, H.; Patzak, A. Blunted arterial baroreflex causes “physiological” heart rate turbulence. Am. J. Physiol. Regul. Integr. Comp. Physiol. 2000, 279, R1171–R1175. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Davies, L.; Francis, D.; Ponikowski, P.; Piepoli, M.; Coats, A. Relation of heart rate and blood pressure turbulence following premature ventricular complexes to baroreflex sensitivity in chronic congestive heart failure. Am. J. Cardiol. 2001, 87, 737–742. [Google Scholar] [CrossRef]
- Szymanowska, K.; Piatkowska, A.; Nowicka, A.; Cofta, S.; Wierzchowiecki, M. Heart rate turbulence in patients with obstructive sleep apnea syndrome. Cardiol. J. 2008, 15, 441–445. [Google Scholar]
- Erdem, A.; Dogan, O.T.; Yontar, O.C.; Epozturk, K.; Ozlu, M.F.; Ozturk, S.; Ayhan, S.S.; Erdem, F.H.; Yazici, M.; Akkurt, I.; et al. The pure effects of obstructive sleep apnea syndrome on cardiac autonomic functions: Heart rate turbulence analysis. Eur. Rev. Med. Pharmacol. Sci. 2013, 17, 2778–2783. [Google Scholar]
- Yates, B.J.; Bolton, P.S.; Macefield, V.G. Vestibulo-sympathetic responses. Compr. Physiol. 2014, 4, 851–887. [Google Scholar]
- Berry, R.B.; Brooks, R.; Gamaldo, C.E.; Harding, S.M.; Lloyd, R.M.; Marcus, C.L.; Vaughn, B.V. The AASM manual for the scoring of sleep and associated events: Rules, terminology, and technical specifications, version 2.2. Am. Acad. Sleep Med. 2015, 28, 391–397. [Google Scholar]
- Watanabe, M.A.; Bhalodia, R.; Lundequam, E.J.; Domitrovich, P.P.; Steinmeyer, B.C.; Stein, P.K.; Freedland, K.E.; Duntley, S.P.; Carney, R.M. Increased ventricular premature contraction frequency during REM sleep in patients with coronary artery disease and obstructive sleep apnea. Indian Pacing Electrophysiol. J. 2008, 8, 258–267. [Google Scholar]
- Ozkececi, G.; Ulasli, S.S.; Akci, O.; Avsar, A.; Unlu, M.; Onrat, E. The effect of sleep apnea severity on cardiac autonomic activity during night time in obstructive sleep apnea patients. Sao Paulo Med. J. 2016, 134, 430–436. [Google Scholar] [CrossRef]
- Kendzerska, T.; Gershon, A.S.; Hawker, G.; Leung, R.S.; Tomlinson, G. Obstructive sleep apnea and risk of cardiovascular events and all-cause mortality: A decade-long historical cohort study. PLoS Med. 2014, 11, e1001599. [Google Scholar] [CrossRef] [PubMed] [Green Version]


| Whole Study Group | Obstructive Sleep Apnea (OSA) (Group A) | Without OSA (Group B) | p A vs. B | |
|---|---|---|---|---|
| number | 71 / 100.0 | 49 / 100.0 | 22 / 100.0 | – |
| men | 43 / 60.6 | 31 / 63.3 | 12 / 54.5 | 0.486 |
| women | 28 / 39.4 | 18 / 36.7 | 10 / 45.5 | 0.486 |
| age (years) | 58.86 ± 11.69 | 61.16 ± 10.43 | 53.73 ± 12.92 | 0.012 |
| height (m) | 1.71 ± 0.09 | 1.70 ± 0.09 | 1.74 ± 0.10 | 0.133 |
| body mass (kg) | 91.97 ± 18.16 | 96.80 ± 17.74 | 79.89 ± 13.08 | 0.001 |
| BMI (kg/m2) | 31.57 ± 6.57 | 33.60 ± 6.22 | 26.38 ± 4.23 | 0.000 |
| obesity | 42 / 59.1 | 36 / 73.5 | 6 / 27.3 | 0.000 |
| total cholesterol (mg/dL) | 214.02 ± 46.63 | 223.06 ± 51.41 | 192.71 ± 22.18 | 0.040 |
| LDL cholesterol (mg/dL) | 129.23 ± 40.63 | 138,24 ± 43.69 | 108.00 ± 21.27 | 0.018 |
| HDL cholesterol (mg/dL) | 52.45 ± 12.80 | 50.70 ± 11.40 | 56.57 ± 15.28 | 0.152 |
| triglicerides (mg/dL) | 165.94 ± 61.08 | 172.76 ± 64.23 | 149.86 ± 51.47 | 0.244 |
| hyperlipidemia | 48 / 67.6 | 36 / 73.5 | 12 / 54.5 | 0.115 |
| glucose (mg/dL) | 116.86 ± 33.11 | 120.81 ± 37.40 | 106.71 ± 14.57 | 0.179 |
| diabetes mellitus | 14 / 19.7 | 12 / 24.5 | 2 / 9.1 | 0.131 |
| arterial hypertension | 53 / 74.6 | 43 / 87.8 | 10 / 45.5 | 0.006 |
| coronary artery diseases | 12 / 16.9 | 4 / 8.2 | 8 / 36.4 | 0.093 |
| stroke | 1 / 1.4 | 1 / 2.0 | 0 / 0.0 | 0.978 |
| smoking | 9 / 12.7 | 7 / 14.3 | 2 / 9.1 | 0.984 |
| AHI | 24.79 ± 24.79 | 35.12 ± 23.32 | 1.80 ± 1.41 | 0.000 |
| Parameter | Unit | Definitions |
|---|---|---|
| TO | % | Turbulence onset: percentage difference between the heart rate immediately following premature ventricular complex and the heart rate immediately preceding premature ventricular complex. normal TO < 0 %. |
| TS | ms/RR | Turbulence slope: the steepest slope of the linear regression line for each sequence of five consecutive normal intervals in the local tachogram. normal TS > 2.5 ms per RR interval. |
| HRT0 | – | Normal heart rate turbulence: normal TO and normal TS or inability to calculate TO and TS. |
| HRT1/2 | – | Abnormal heart rate turbulence: abnormal TO or/and abnormal TS |
| HRT1 | – | Abnormal TO or abnormal TS. |
| HRT2 | – | Abnormal TO and abnormal TS. |
| Whole Study Group | OSA (Group A) n = 49 | Without OSA (Group B) n = 22 | p A vs. B | |
|---|---|---|---|---|
| TO (%) | −2.77 ± 2.31 | −2.36 ± 2.27 | −3.69 ± 2.20 | 0.025 |
| normal TO | 66 / 92.9 | 46 / 93.9 | 20 / 90.9 | 0.651 |
| TS (ms/RR) | 8.43 ± 6.47 | 6.85 ± 5.78 | 11.95 ± 6.66 | 0.002 |
| normal TS | 62 / 87.3 | 40 / 81.6 | 22 / 100.0 | 0.031 |
| HRT0 | 59 / 83.1 | 39 / 79.6 | 20 / 90.9 | 0.239 |
| HRT1/2 | 12 / 16.9 | 10 / 20.4 | 2 / 9.1 | 0.239 |
| HRT1 | 10 / 14.1 | 8 / 16.3 | 2 / 9.1 | 0.428 |
| HRT2 | 2 / 2.8 | 2 / 4.1 | 0 / 0.0 | 0.428 |
| For AHI ≥ 65 | For AHI ≥ 5 | |
|---|---|---|
| Sensitivity | 0.966 | 0.339 |
| Specificity | 0.417 | 0.833 |
| Accuracy | 0.873 | 0.423 |
| Positive predictive values | 0.891 | 0.909 |
| Negative predictive values | 0.714 | 0.204 |
| Likelihood ratios positive | 1.656 | 2.034 |
| Likelihood ratios negative | 0.081 | 0.793 |
| AHI ≥ 65 (Group C) n = 7 | AHI < 65 (Group D) n = 64 | p C vs. D | |
|---|---|---|---|
| TO (%) | −1.26 ± 0.85 | −2.94 ± 2.36 | 0.068 |
| normal TO | 7 / 100.0 | 59 / 92.2 | 0.443 |
| TS (ms/RR) | 2.88 ± 1.98 | 9.04 ± 6.51 | 0.016 |
| normal TS | 2 / 28.6 | 60 / 93.7 | 0.000 |
| HRT0 | 2 / 28.6 | 57 / 89.1 | 0.000 |
| HRT1/2 | 5 / 71.4 | 7 / 10.9 | 0.000 |
| HRT1 | 5 / 71.4 | 5 / 7.8 | 0.000 |
| HRT2 | 0 / 0.0 | 2 / 3.1 | 0.135 |
| OSA with AHI ≥15 (Subgroup A1) n = 41 | OSA with AHI <15 (Subgroup A2) n = 8 | p A1 vs. A2 | |
|---|---|---|---|
| TO (%) | −2.06 ± 1.72 | −3.94 ± 3.87 | 0.030 |
| normal TO | 38 / 92.7 | 8 / 100.0 | 0.430 |
| TS (ms/RR) | 6.15 ± 3.72 | 10.43 ± 11.52 | 0.049 |
| normal TS | 33 / 80.5 | 7 / 87.5 | 0.639 |
| HRT0 | 32 / 78.1 | 7 / 87.5 | 0.544 |
| HRT1/2 | 9 / 21.9 | 1 / 12.5 | 0.544 |
| HRT1 | 7 / 17.0 | 1 / 12.5 | 0.759 |
| HRT2 | 2 / 4.9 | 2 / 0.0 | 0.759 |
| OSA with AHI ≥30 (Subgroup A3) n = 24 | OSA with AHI <30 (Subgroup A4) n = 25 | p A3 vs. A4 | |
|---|---|---|---|
| TO (%) | −2.05 ± 1.89 | −2.67 ± 2.58 | 0.347 |
| normal TO | 22 / 91.7 | 24 / 96.0 | 0.527 |
| TS (ms/RR) | 5.77 ± 4.08 | 7.88 ± 6.97 | 0.204 |
| normal TS | 17 / 70.8 | 23 / 92.0 | 0.049 |
| HRT0 | 17 / 70.8 | 22 / 88.0 | 0.136 |
| HRT1/2 | 7 / 29.1 | 3 / 12.0 | 0.136 |
| HRT1 | 5 / 20.8 | 3 / 12.0 | 0.209 |
| HRT2 | 2 / 8.3 | 0 / 0.0 | 0.209 |
| for AHI ≥ 65 | for AHI ≥ 15 | for AHI ≥ 30 | |
|---|---|---|---|
| Sensitivity | 0.949 | 0.179 | 0.564 |
| Specificity | 0.500 | 0.900 | 0.700 |
| Accuracy | 0.857 | 0.327 | 0.592 |
| Positive predictive values | 0.881 | 0.875 | 0.880 |
| Negative predictive values | 0.714 | 0.220 | 0.292 |
| Likelihood ratios positive | 1.897 | 1.795 | 1.880 |
| Likelihood ratios negative | 0.103 | 0.912 | 0.623 |
| OSA with AHI ≥ 65 (Subgroup A5) n = 7 | OSA with AHI < 65 (Subgroup A6) n = 42 | p A5 vs. A6 | |
|---|---|---|---|
| TO (%) | −1.26 ± 0.85 | −2.55 ± 2.38 | 0.167 |
| normal TO | 7 / 100.0 | 39 / 92.9 | 0.465 |
| TS (ms/RR) | 2.88 ± 1.98 | 7.51 ± 5.95 | 0.048 |
| normal TS | 2 / 28.6 | 38 / 90.5 | 0.000 |
| HRT0 | 2 / 28.6 | 37 / 88.1 | 0.000 |
| HRT1/2 | 5 / 71.4 | 5 / 11.9 | 0.000 |
| HRT1 | 5 / 71.4 | 3 / 7.1 | 0.000 |
| HRT2 | 0 / 0.0 | 2 / 4.8 | 0.068 |
| AHI | |||
|---|---|---|---|
| R | p | ||
| whole study group | TO (%) | 0.33 | 0.005 |
| TS (ms/RR) | −0.42 | 0.000 | |
| group with OSA | TO (%) | 0.28 | 0.045 |
| TS (ms/RR) | −0.32 | 0.023 | |
| group without OSA | TO (%) | 0.22 | 0.310 |
| TS (ms/RR) | −0.35 | 0.109 | |
| Model for: TO (%) | ||||||
|---|---|---|---|---|---|---|
| Univariate Regression | Multivariable Stepwise Regression | |||||
| Rc | SEM of Rc | p | Rc | SEM of Rc | p | |
| men | −0.451 | 1.161 | 0.425 | − | − | − |
| women | 0.451 | 1.161 | 0.425 | − | − | − |
| age (years) | 0.091 | 0.029 | 0.000 | 0.090 | 0.027 | 0.002 |
| height (m) | −3.955 | 4.435 | 0.197 | − | − | − |
| body mass (kg) | 0.027 | 0.030 | 0.072 | − | − | − |
| BMI (kg/m2) | 0.105 | 0.086 | 0.012 | −0.073 | 0.012 | 0.039 |
| obesity | 1.183 | 0.368 | 0.033 | − | − | − |
| total cholesterol (mg/dL) | −0.004 | 0.015 | 0.568 | − | − | − |
| LDL cholesterol (mg/dL) | −0.003 | 0.016 | 0.739 | − | − | − |
| HDL cholesterol (mg/dL) | 0.006 | 0.031 | 0.980 | − | − | − |
| triglicerides (mg/dL) | −0.004 | 0.007 | 0.409 | − | − | − |
| hyperlipidemia | 0.972 | 0.631 | 0.098 | − | − | − |
| glucose (mg/dL) | 0.009 | 0.010 | 0.349 | − | − | − |
| diabetes mellitus | 1.493 | 0.554 | 0.029 | 1.486 | 0.646 | 0.025 |
| arterial hypertension | 2.527 | 0.741 | 0.000 | 0.343 | 0.190 | 0.046 |
| coronary artery diseases | 0.194 | 0.792 | 0.793 | − | − | − |
| stroke | 0.887 | 2.145 | 0.706 | − | − | − |
| smoking | 0.148 | 0.857 | 0.876 | − | − | − |
| AHI | 0.031 | 0.004 | 0.005 | 0.019 | 0.008 | 0.011 |
| Model for: TS (ms/RR) | ||||||
|---|---|---|---|---|---|---|
| Univariate Regression | Multivariable Stepwise Regression | |||||
| Rc | SEM of Rc | p | Rc | SEM of Rc | p | |
| men | 0.003 | 3.005 | 0.977 | − | − | − |
| women | −0.003 | 3.005 | 0.977 | − | − | − |
| age (years) | −0.456 | 0.075 | 0.000 | −0.158 | 0.093 | 0.048 |
| height (m) | 0.146 | 1.469 | 0.253 | − | − | − |
| body mas (kg) | −0.358 | 0.075 | 0.004 | − | − | − |
| BMI (kg/m2) | −0.428 | 0.224 | 0.000 | − | − | − |
| obesity | −0.464 | 0.172 | 0.000 | − | − | − |
| total cholesterol (mg/dL) | −0.080 | 0.038 | 0.592 | − | − | − |
| LDL cholesterol (mg/dL) | −0.052 | 0.040 | 0.727 | − | − | − |
| HDL cholestero (mg/dL) | 0.107 | 0.082 | 0.475 | − | − | − |
| triglicerides (mg/dL) | −0.257 | 0.017 | 0.081 | − | − | − |
| hyperlipidemia | −0.295 | 0.063 | 0.013 | − | − | − |
| glucose (mg/dL) | −0.324 | 0.027 | 0.022 | −0.028 | 0.007 | 0.027 |
| diabetes mellitus | − 0.210 | 0.195 | 0.079 | − | − | − |
| arterial hypertension | −0.593 | 0.177 | 0.000 | −3.480 | 0.975 | 0.024 |
| coronary artery diseases | − 0.144 | 0.204 | 0.233 | − | − | − |
| stroke | − 0.125 | 0.554 | 0.297 | − | − | − |
| smoking | − 0.021 | 0.042 | 0.918 | − | − | − |
| AHI | −0.423 | 0.036 | 0.000 | −0.044 | 0.009 | 0.024 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Urbanik, D.; Gać, P.; Martynowicz, H.; Poręba, M.; Podgórski, M.; Negrusz-Kawecka, M.; Mazur, G.; Sobieszczańska, M.; Poręba, R. Obstructive Sleep Apnea as a Predictor of Abnormal Heart Rate Turbulence. J. Clin. Med. 2020, 9, 1. https://doi.org/10.3390/jcm9010001
Urbanik D, Gać P, Martynowicz H, Poręba M, Podgórski M, Negrusz-Kawecka M, Mazur G, Sobieszczańska M, Poręba R. Obstructive Sleep Apnea as a Predictor of Abnormal Heart Rate Turbulence. Journal of Clinical Medicine. 2020; 9(1):1. https://doi.org/10.3390/jcm9010001
Chicago/Turabian StyleUrbanik, Dominika, Paweł Gać, Helena Martynowicz, Małgorzata Poręba, Maciej Podgórski, Marta Negrusz-Kawecka, Grzegorz Mazur, Małgorzata Sobieszczańska, and Rafał Poręba. 2020. "Obstructive Sleep Apnea as a Predictor of Abnormal Heart Rate Turbulence" Journal of Clinical Medicine 9, no. 1: 1. https://doi.org/10.3390/jcm9010001
APA StyleUrbanik, D., Gać, P., Martynowicz, H., Poręba, M., Podgórski, M., Negrusz-Kawecka, M., Mazur, G., Sobieszczańska, M., & Poręba, R. (2020). Obstructive Sleep Apnea as a Predictor of Abnormal Heart Rate Turbulence. Journal of Clinical Medicine, 9(1), 1. https://doi.org/10.3390/jcm9010001







