Maternal Obesity and Offspring Long-Term Infectious Morbidity
Abstract
1. Introduction
2. Methods
Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Practice Committee of the American Society for Reproductive Medicine. Obesity and reproduction: A committee opinion. Fertil. Steril. 2015, 104, 1116–1126. [Google Scholar] [CrossRef] [PubMed]
- Hales, C.M.; Fryar, C.D.; Carroll, M.D.; Freedman, D.S.; Ogden, C.L. Trends in obesity and severe obesity prevalence in us youth and adults by sex and age, 2007–2008 to 2015–2016. J. Am. Med. Assoc. 2018, 319, 1723–1725. [Google Scholar] [CrossRef] [PubMed]
- Ogden, C.L.; Carroll, M.D.; Kit, B.K.; Flegal, K.M. Prevalence of childhood and adult obesity in the United States, 2011–2012. J. Am. Med. Assoc. 2014, 311, 806–814. [Google Scholar] [CrossRef] [PubMed]
- Silvestris, E.; de Pergola, G.; Rosania, R.; Loverro, G. Obesity as disruptor of the female fertility. Reprod. Biol. Endocrinol. 2018, 16, 22. [Google Scholar] [CrossRef] [PubMed]
- Gutvirtz, G.; Alexander, C.; Sheiner, E. Bariatric Surgery and Its Impact on Gestational Diabetes. In Nutrition and Diet in Maternal Diabetes: An Evidence-Based Approach; Rajendram, R., Preedy, V.R., Patel, V.B., Eds.; Springer International Publishing: Cham, Switzerland, 2018; pp. 207–226. [Google Scholar]
- Torloni, M.R.; Betrán, A.P.; Horta, B.L.; Nakamura, M.U.; Atallah, A.N.; Moron, A.F.; Valente, O. Prepregnancy BMI and the risk of gestational diabetes: A systematic review of the literature with meta-analysis. Obes. Rev. 2009, 10, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Group HSCR. Hyperglycaemia and Adverse Pregnancy Outcome (HAPO) Study: Associations with maternal body mass index. Int. J. Obstet. Gynaecol. 2010, 117, 575–584. [Google Scholar] [CrossRef] [PubMed]
- Sheiner, E.; Levy, A.; Menes, T.S.; Silverberg, D.; Katz, M.; Mazor, M. Maternal obesity as an independent risk factor for caesarean delivery. Paediatr. Perinat. Epidemiol. 2004, 18, 196–201. [Google Scholar] [CrossRef] [PubMed]
- Blondon, M.; Harrington, L.B.; Boehlen, F.; Robert-Ebadi, H.; Righini, M.; Smith, N.L. Pre-pregnancy BMI, delivery BMI, gestational weight gain and the risk of postpartum venous thrombosis. Thromb. Res. 2016, 145, 151–156. [Google Scholar] [CrossRef]
- Krieger, Y.; Walfisch, A.; Sheiner, E. Surgical site infection following cesarean deliveries: Trends and risk factors. J. Matern. Fetal Neonatal Med. 2017, 30, 8–12. [Google Scholar] [CrossRef]
- Yaniv-Salem, S.; Shoham-Vardi, I.; Kessous, R.; Pariente, G.; Sergienko, R.; Sheiner, E. Obesity in pregnancy: What’s next? Long-term cardiovascular morbidity in a follow-up period of more than a decade. J. Matern. Fetal Neonatal Med. 2016, 29, 619–623. [Google Scholar] [CrossRef]
- Sasson, I.; Beharier, O.; Sergienko, R.; Szaingurten-Solodkin, I.; Kessous, R.; Belfair, N.J.; Sheiner, E. Obesity during pregnancy and long-term risk for ophthalmic morbidity—A population-based study with a follow-up of more than a decade. J. Matern. Fetal Neonatal Med. 2016, 29, 2924–2928. [Google Scholar] [CrossRef] [PubMed]
- Kessous, R.; Davidson, E.; Meirovitz, M.; Sergienko, R.; Sheiner, E. Prepregnancy obesity: A risk factor for future development of ovarian and breast cancer. Eur. J. Cancer Prev. 2016, 26, 151–155. [Google Scholar] [CrossRef] [PubMed]
- Fuchs, O.; Sheiner, E.; Meirovitz, M.; Davidson, E.; Sergienko, R.; Kessous, R. The association between a history of gestational diabetes mellitus and future risk for female malignancies. Arch. Gynecol. Obstet. 2017, 295, 731–736. [Google Scholar] [CrossRef] [PubMed]
- Stothard, K.J.; Tennant, P.W.; Bell, R.; Rankin, J. Maternal overweight and obesity and the risk of congenital anomalies: A systematic review and meta-analysis. JAMA 2009, 301, 636–650. [Google Scholar] [CrossRef] [PubMed]
- Ovesen, P.; Rasmussen, S.; Kesmodel, U. Effect of prepregnancy maternal overweight and obesity on pregnancy outcome. Obstet. Gynecol. 2011, 118, 305–312. [Google Scholar] [CrossRef]
- Aune, D.; Saugstad, O.D.; Henriksen, T.; Tonstad, S. Maternal body mass index and the risk of fetal death, stillbirth, and infant death: A systematic review and meta-analysis. JAMA 2014, 311, 1536–1546. [Google Scholar] [CrossRef]
- Doherty, D.A.; Magann, E.F.; Francis, J.; Morrison, J.C.; Newnham, J.P. Pre-pregnancy body mass index and pregnancy outcomes. Int. J. Gynaecol. Obstet. 2006, 95, 242–247. [Google Scholar] [CrossRef]
- Mitanchez, D.; Chavatte-Palmer, P. Review shows that maternal obesity induces serious adverse neonatal effects and is associated with childhood obesity in their offspring. Acta Paediatr. 2018, 107, 1156–1165. [Google Scholar] [CrossRef]
- Genoni, G.; Prodam, F.; Marolda, A.; Giglione, E.; Demarchi, I.; Bellone, S.; Bona, G. Obesity and infection: Two sides of one coin. Eur. J. Pediatr. 2014, 173, 25–32. [Google Scholar] [CrossRef]
- Barker, D.J. The fetal and infant origins of adult disease. Br. Med. J. 1990, 301, 1111. [Google Scholar] [CrossRef]
- Galliano, D.; Bellver, J. Female obesity: Short- and long-term consequences on the offspring. Gynecol. Endocrinol. 2013, 29, 626–631. [Google Scholar] [CrossRef]
- Håberg, S.E.; Stigum, H.; London, S.J.; Nystad, W.; Nafstad, P. Maternal obesity in pregnancy and respiratory health in early childhood. Paediatr. Perinat. Epidemiol. 2009, 23, 352–362. [Google Scholar] [CrossRef]
- Parsons, E.C.; Patel, K.; Tran, B.T.; Littman, A.J. Maternal pre-gravid obesity and early childhood respiratory hospitalization: A population-based case-control study. Matern. Child Health J. 2013, 17, 1095–1102. [Google Scholar] [CrossRef]
- Cameron, C.M.; Shibl, R.; McClure, R.J.; Ng, S.K.; Hills, A.P. Maternal pregravid body mass index and child hospital admissions in the first 5 years of life: Results from an Australian birth cohort. Int. J. Obes. 2014, 38, 1268–1274. [Google Scholar] [CrossRef]
- McGillick, E.V.; Lock, M.C.; Orgeig, S.; Morrison, J.L. Maternal obesity mediated predisposition to respiratory complications at birth and in later life: Understanding the implications of the obesogenic intrauterine environment. Paediatr. Respir. Rev. 2017, 21, 11–18. [Google Scholar] [CrossRef]
- Velten, M.; Heyob, K.M.; Rogers, L.K.; Welty, S.E. Deficits in lung alveolarization and function after systemic maternal inflammation and neonatal hyperoxia exposure. J. Appl. Physiol. 2010, 108, 1347–1356. [Google Scholar] [CrossRef]
- Challier, J.C.; Basu, S.; Bintein, T.; Minium, J.; Hotmire, K.; Catalano, P.M.; Hauguel-de Mouzon, S. Obesity in pregnancy stimulates macrophage accumulation and inflammation in the placenta. Placenta 2008, 29, 274–281. [Google Scholar] [CrossRef]
- Myles, I.A.; Fontecilla, N.M.; Janelsins, B.M.; Vithayathil, P.J.; Segre, J.A.; Datta, S.K. Parental dietary fat intake alters offspring microbiome and immunity. J. Immunol. 2013, 191, 3200–3209. [Google Scholar] [CrossRef]
- Falagas, M.E.; Kompoti, M. Obesity and infection. Lancet Infect. Dis. 2006, 6, 438–446. [Google Scholar] [CrossRef]
- Huttunen, R.; Syrjänen, J. Obesity and the risk and outcome of infection. Int. J. Obes. 2013, 37, 333–340. [Google Scholar] [CrossRef]
- Karlsson, E.A.; Beck, M.A. The burden of obesity on infectious disease. Exp. Biol. Med. 2010, 235, 1412–1424. [Google Scholar] [CrossRef]
- Milner, J.J.; Beck, M.A. The impact of obesity on the immune response to infection. Proc. Nutr. Soc. 2012, 71, 298–306. [Google Scholar] [CrossRef]
- Martí, A.; Marcos, A.; Martínez, J.A. Obesity and immune function relationships. Obes. Rev. 2001, 2, 131–140. [Google Scholar] [CrossRef]
- Lea, R.G.; Howe, D.; Hannah, L.T.; Bonneau, O.; Hunter, L.; Hoggard, N. Placental leptin in normal, diabetic and fetal growth-retarded pregnancies. Mol. Hum. Reprod. 2000, 6, 763–769. [Google Scholar] [CrossRef]
- Vela-Huerta, M.M.; San Vicente-Santoscoy, E.U.; Guizar-Mendoza, J.M.; Amador-Licona, N.; Aldana-Valenzuela, C.; Hernnández, J. Leptin, insulin, and glucose serum levels in large-for-gestational-age infants of diabetic and non-diabetic mothers. J. Pediatr. Endocrinol. Metab. 2008, 21, 17–22. [Google Scholar] [CrossRef]
- Mattioli, B.; Giordani, L.; Quaranta, M.G.; Viora, M. Leptin exerts an anti-apoptotic effect on human dendritic cells via the PI3K-Akt signaling pathway. FEBS Lett. 2009, 583, 1102–1106. [Google Scholar] [CrossRef]
- Brynhildsen, J.; Sydsjö, G.; Blomberg, M.; Claesson, I.M.; Theodorsson, E.; Nyström, F.; Josefsson, A. Leptin and adiponectin in cord blood from children of normal weight, overweight and obese mothers. Acta Paediatr. 2013, 102, 620–624. [Google Scholar] [CrossRef]
- Wainstock, T.; Walfisch, A.; Shoham-Vardi, I.; Segal, I.; Sergienko, R.; Landau, D.; Sheiner, E. Term Elective Cesarean Delivery and Offspring Infectious Morbidity—A Population Based Cohort Study. Pediatr. Infect. Dis. J. 2018, 38, 176–180. [Google Scholar] [CrossRef]
- OECD. Health at a Glance 2011: OECD Indicators; OECD Publishing: Paris, France, 2011. [Google Scholar] [CrossRef]
- (MOH) IMoH. Prevention and Treatment of Obesity 2011. Available online: https://www.health.gov.il/PublicationsFiles/Obesity-prof_en.pdf (accessed on 1 September 2019).
- Dobner, J.; Kaser, S. Body mass index and the risk of infection—From underweight to obesity. Clin. Microbiol. Infect. 2018, 24, 24–28. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No 156: Obesity in Pregnancy. Obstet. Gynecol. 2015, 126, e112–e126. [Google Scholar] [CrossRef]
| Maternal Characteristic/Pregnancy Outcome | Maternal Obesity n = 3399 | No Obesity n = 246,441 | p Value |
|---|---|---|---|
| Maternal age (years, mean± SD) | 30.4 ± 5.6 | 28.1 ± 5.8 | <0.01 |
| Recurrent pregnancy loss (n) | 234 (6.9%) | 12,417 (5.0%) | <0.001 |
| Fertility treatments a (n) | 156 (4.6%) | 4340 (1.8%) | <0.001 |
| Diabetes (n) | 285 (8.4%) | 12,293 (5.0%) | <0.001 |
| Pre-gestational | 119 (3.5%) | 1733 (0.7%) | <0.001 |
| Gestational | 166 (4.9%) | 10,560 (4.3%) | 0.087 |
| Hypertensive disease (n) | 314 (9.2%) | 12,385 (5.0%) | <0.001 |
| Pre-gestational (chronic HTN) | 137 (4.0%) | 3313 (1.3%) | <0.001 |
| Gestational, preeclampsia and eclampsia | 203 * (6.0%) | 9755 * (4.0%) | <0.001 |
| Birthweight (gr., mean ± SD) | 3354.1 ± 550 | 3196.8 ± 521 | <0.001 |
| Gestational age at birth (weeks, mean ± SD) | 39.1 ± 2.1 | 39.1 ± 2.1 | 0.64 |
| Chorioamnionitis (n) | 28 (0.8%) | 1682 (0.7%) | 0.32 |
| Induction of labor (n) | 1,157 (34.0%) | 64,220 (26.1%) | <0.001 |
| Cesarean delivery (n) | 1,167 (34.3%) | 33,189 (13.5%) | <0.001 |
| Preterm delivery (n) | 244 (7.2%) | 17,764 (7.2%) | 0.95 |
| 34–37 weeks’ gestation | 198 (5.8%) | 13,784 (5.6%) | 0.403 |
| 28–34 weeks’ gestation | 35 (1.0%) | 3098 (1.2%) | 0.403 |
| <28 weeks’ gestation | 11 (0.4%) | 882 (0.4%) | 0.403 |
| Low Apgar b at 1 min. (n) | 260 (7.6%) | 13,800 (5.6%) | <0.001 |
| Low Apgar b at 5 min. (n) | 63 (1.9%) | 605 (2.5%) | 0.02 |
| Low birth weight c (n) | 170 (5.0%) | 17,612 (7.1%) | <0.001 |
| Macrosomia d (n) | 336 (9.9%) | 11,344 (4.6%) | <0.001 |
| Perinatal mortality (n) | 30 (0.9%) | 1960 (0.8%) | 0.57 |
| Antepartum death | 17 (0.5%) | 937 (1.4%) | 0.262 |
| Intra-partum death | 3 (0.1%) | 94 (0.1%) | 0.141 |
| Post-partum death | 10 (0.3%) | 929 (0.4%) | 0.434 |
| Infectious Morbidity | Maternal Obesity n = 3399 | No Obesity n = 246,441 | p Value |
|---|---|---|---|
| Respiratory infections | 214 (6.3%) | 13,538 (5.5%) | 0.04 |
| Viral infections | 42 (1.2%) | 2107 (0.9%) | 0.01 |
| ENT infections | 73 (2.1%) | 3616 (1.5%) | <0.01 |
| Ophthalmic infections | 17 (0.5%) | 727 (0.3%) | 0.03 |
| Neonatal infections | 8 (0.2%) | 679 (0.3%) | 0.65 |
| Bacterial infections | 7 (0.2%) | 342 (0.1%) | 0.29 |
| Bacteremia/Septicemia | 5 (0.1%) | 190 (0.1%) | 0.14 |
| Central nervous system infections | 6 (0.2%) | 564 (0.2%) | 0.52 |
| Gastrointestinal infections | 62 (1.8%) | 4043 (1.6%) | 0.40 |
| Total infectious hospitalization | 426 (12.5%) | 27,133 (11.0%) | <0.01 |
| Variables | Adjusted HR | 95%CI | p Value | |
|---|---|---|---|---|
| Min | Max | |||
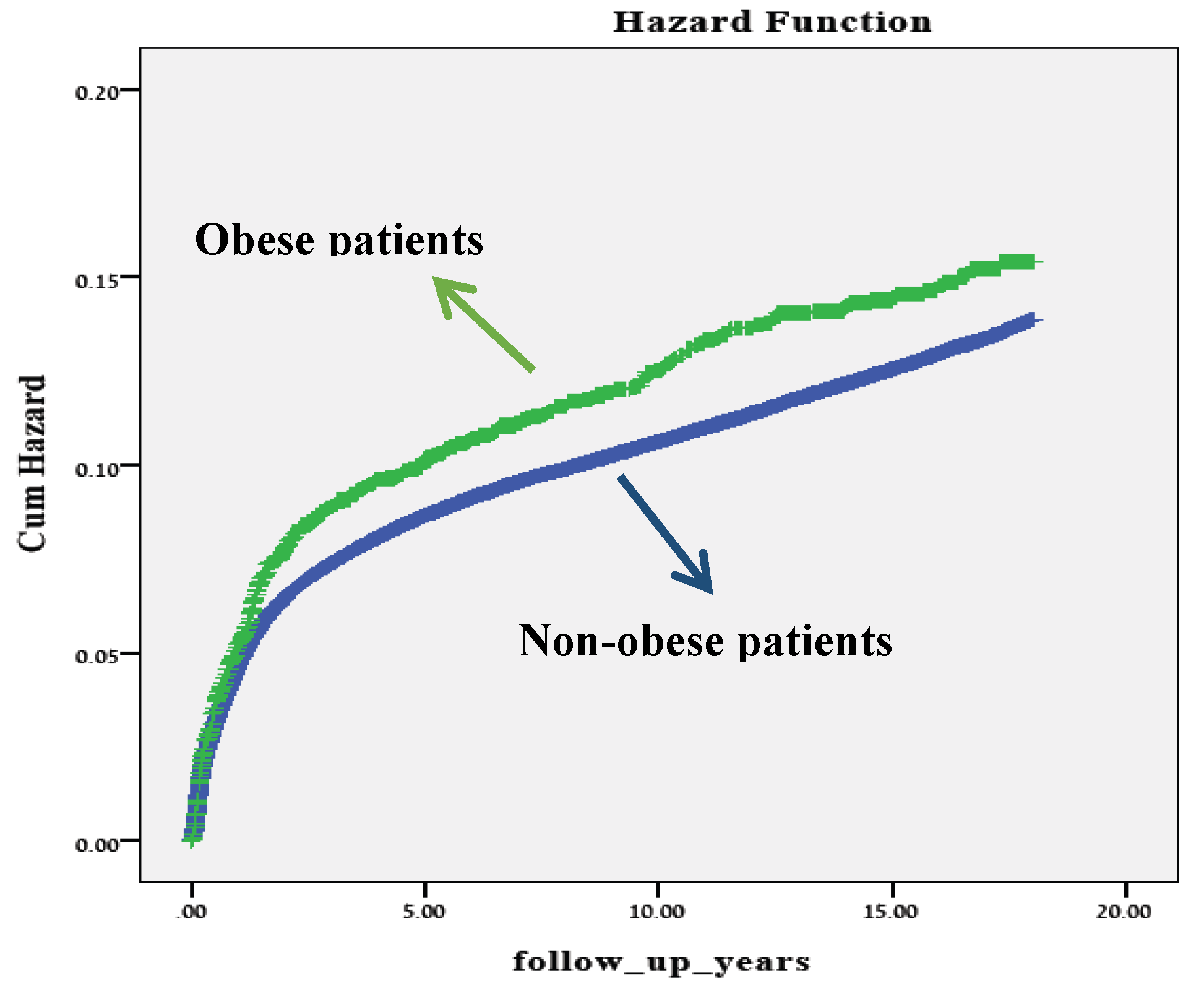
| Maternal obesity | 1.125 | 1.021 | 1.238 | 0.017 |
| Maternal age (years) | 0.998 | 0.995 | 1.000 | 0.027 |
| Birthweight (grams) | 1.000 | 1.000 | 1.000 | 1.000 |
| Chorioamnionitis | 0.735 | 0.634 | 0.853 | <0.001 |
| Preterm delivery (<37 weeks) | 1.203 | 1.147 | 1.262 | <0.001 |
| Induction of labor | 1.145 | 1.114 | 1.177 | <0.001 |
| Cesarean delivery | 1.220 | 1.179 | 1.262 | <0.001 |
| Pre-gestational (chronic HTN) | 0.865 | 0.782 | 0.958 | 0.005 |
| Gestational, preeclampsia and eclampsia | 0.924 | 0.870 | 0.982 | 0.011 |
| Pre-gestational diabetes | 1.478 | 1.314 | 1.662 | <0.001 |
| Gestational diabetes | 0.979 | 0.924 | 1.039 | 0.488 |
| Lack of prenatal care | 0.750 | 0.717 | 0.785 | <0.001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gutvirtz, G.; Wainstock, T.; Landau, D.; Sheiner, E. Maternal Obesity and Offspring Long-Term Infectious Morbidity. J. Clin. Med. 2019, 8, 1466. https://doi.org/10.3390/jcm8091466
Gutvirtz G, Wainstock T, Landau D, Sheiner E. Maternal Obesity and Offspring Long-Term Infectious Morbidity. Journal of Clinical Medicine. 2019; 8(9):1466. https://doi.org/10.3390/jcm8091466
Chicago/Turabian StyleGutvirtz, Gil, Tamar Wainstock, Daniella Landau, and Eyal Sheiner. 2019. "Maternal Obesity and Offspring Long-Term Infectious Morbidity" Journal of Clinical Medicine 8, no. 9: 1466. https://doi.org/10.3390/jcm8091466
APA StyleGutvirtz, G., Wainstock, T., Landau, D., & Sheiner, E. (2019). Maternal Obesity and Offspring Long-Term Infectious Morbidity. Journal of Clinical Medicine, 8(9), 1466. https://doi.org/10.3390/jcm8091466






