Prevention, Treatment, and Monitoring of Seizures in the Intensive Care Unit
Abstract
1. Introduction
2. Epidemiology
3. Pathophysiology
4. Monitoring
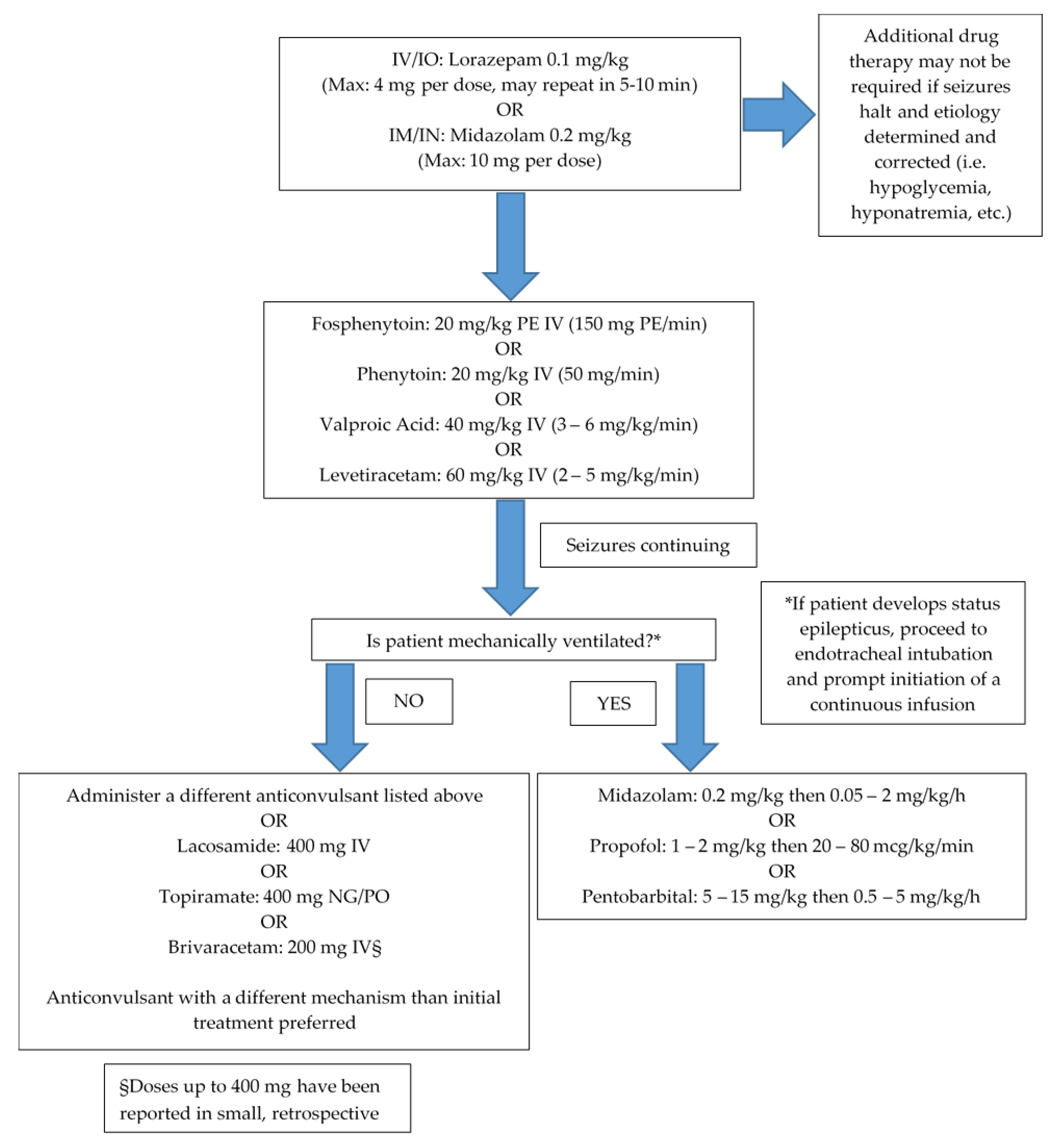
5. Treatment
6. Special Considerations
7. Older Adults, Pediatrics, and Pregnancy
8. Summary
Author Contributions
Funding
Conflicts of Interest
References
- Cost of Status Epilepticus: A Systematic Review—ScienceDirect. Available online: https://www.sciencedirect.com/science/article/pii/S1059131114003021 (accessed on 18 December 2018).
- McNett, M.; Moran, C.; Johnson, H. Evidence-Based Review of Clinical Trials in Neurocritical Care. AACN Adv. Crit. Care 2018, 29, 195–203. [Google Scholar] [CrossRef] [PubMed]
- Ko, S.-B. Multimodality Monitoring in the Neurointensive Care Unit: A Special Perspective for Patients with Stroke. J. Stroke 2013, 15, 99–108. [Google Scholar] [CrossRef] [PubMed]
- Westover, M.B.; Shafi, M.M.; Bianchi, M.T.; Moura, L.M.V.R.; O’Rourke, D.; Rosenthal, E.S.; Chu, C.J.; Donovan, S.; Hoch, D.B.; Kilbride, R.D.; et al. The probability of seizures during EEG monitoring in critically ill adults. Clin. Neurophysiol. 2015, 126, 463–471. [Google Scholar] [CrossRef] [PubMed]
- Claassen, J.; Mayer, S.A.; Kowalski, R.G.; Emerson, R.G.; Hirsch, L.J. Detection of electrographic seizures with continuous EEG monitoring in critically ill patients. Neurology 2004, 62, 1743–1748. [Google Scholar] [CrossRef] [PubMed]
- Brophy, G.M.; Bell, R.; Claassen, J.; Alldredge, B.; Bleck, T.P.; Glauser, T.; LaRoche, S.M.; Riviello, J.J.; Shutter, L.; Sperling, M.R.; et al. Guidelines for the Evaluation and Management of Status Epilepticus. Neurocrit. Care 2012, 17, 3–23. [Google Scholar] [CrossRef] [PubMed]
- Shorvon, S.; Ferlisi, M. The treatment of super-refractory status epilepticus: A critical review of available therapies and a clinical treatment protocol. Brain J. Neurol. 2011, 134, 2802–2818. [Google Scholar] [CrossRef] [PubMed]
- Chapter 41. Status Epilepticus | Pharmacotherapy: A Pathophysiologic Approach, 9e | AccessPharmacy | McGraw-Hill Medical. Available online: https://accesspharmacy.mhmedical.com/content.aspx?bookid=689§ionid=45310491#57485199 (accessed on 21 September 2018).
- Dham, B.S.; Hunter, K.; Rincon, F. The Epidemiology of Status Epilepticus in the United States. Neurocrit. Care 2014, 20, 476–483. [Google Scholar] [CrossRef] [PubMed]
- Shin, J.-W.; Koo, Y.S.; Kim, Y.-S.; Kim, D.W.; Kim, K.K.; Lee, S.-Y.; Kim, H.K.; Moon, H.-J.; Lim, J.-A.; Byun, J.-I.; et al. Clinical characterization of unknown/cryptogenic status epilepticus suspected as encephalitis: A multicenter cohort study. J. Neuroimmunol. 2018, 315, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Yan, B.; Wang, R.; Li, C.; Chen, C.; Zhou, D.; Hong, Z. Seizure outcomes in patients with anti-NMDAR encephalitis: A follow-up study. Epilepsia 2017, 58, 2104–2111. [Google Scholar] [CrossRef] [PubMed]
- McNally, B.; Robb, R.; Mehta, M.; Vellano, K.; Valderrama, A.L.; Yoon, P.W.; Sasson, C.; Crouch, A.; Perez, A.B.; Merritt, R.; et al. Out-of-hospital cardiac arrest surveillance—Cardiac Arrest Registry to Enhance Survival (CARES), United States, October 1, 2005–December 31, 2010. Morb. Mortal. Wkly. Rep. Surveill. Summ. 2011, 60, 1–19. [Google Scholar]
- Nielsen, N.; Sunde, K.; Hovdenes, J.; Riker, R.R.; Rubertsson, S.; Stammet, P.; Nilsson, F.; Friberg, H.; Hypothermia Network. Adverse events and their relation to mortality in out-of-hospital cardiac arrest patients treated with therapeutic hypothermia. Crit. Care Med. 2011, 39, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Crepeau, A.Z.; Rabinstein, A.A.; Fugate, J.E.; Mandrekar, J.; Wijdicks, E.F.; White, R.D.; Britton, J.W. Continuous EEG in therapeutic hypothermia after cardiac arrest: Prognostic and clinical value. Neurology 2013, 80, 339–344. [Google Scholar] [CrossRef] [PubMed]
- Won, S.-Y.; Dubinski, D.; Brawanski, N.; Strzelczyk, A.; Seifert, V.; Freiman, T.M.; Konczalla, J. Significant increase in acute subdural hematoma in octo- and nonagenarians: Surgical treatment, functional outcome, and predictors in this patient cohort. Neurosurg. Focus 2017, 43, E10. [Google Scholar] [CrossRef] [PubMed]
- Pruitt, P.; Naidech, A.; Ornam, J.V.; Borczuk, P. Seizure frequency in patients with isolated subdural hematoma and preserved consciousness. Brain Inj. 2019, 0, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Delanty, N.; Vaughan, C.J.; French, J.A. Medical causes of seizures. The Lancet 1998, 352, 383–390. [Google Scholar] [CrossRef]
- Vezzani, A.; Balosso, S.; Ravizza, T. Chapter 10—Inflammation and epilepsy. In Handbook of Clinical Neurology—Epilepsy; Stefan, H., Theodore, W.H., Eds.; Elsevier: Maryland Heights, MO, USA, 2012; Volume 107, pp. 163–175. [Google Scholar]
- Riazi, K.; Galic, M.A.; Kuzmiski, J.B.; Ho, W.; Sharkey, K.A.; Pittman, Q.J. Microglial activation and TNFα production mediate altered CNS excitability following peripheral inflammation. Proc. Natl. Acad. Sci. 2008, 105, 17151–17156. [Google Scholar] [CrossRef] [PubMed]
- Riazi, K.; Galic, M.A.; Pittman, Q.J. Contributions of peripheral inflammation to seizure susceptibility: Cytokines and brain excitability. Epilepsy Res. 2010, 89, 34–42. [Google Scholar] [CrossRef] [PubMed]
- Mayhan, W.G. Cellular mechanisms by which tumor necrosis factor-α produces disruption of the blood–brain barrier. Brain Res. 2002, 927, 144–152. [Google Scholar] [CrossRef]
- Welser-Alves, J.V.; Milner, R. Microglia are the major source of TNF-α and TGF-β1 in postnatal glial cultures; regulation by cytokines, lipopolysaccharide, and vitronectin. Neurochem. Int. 2013, 63, 47–53. [Google Scholar] [CrossRef]
- Ha, J.; Choi, J.; Kwon, A.; Kim, K.; Kim, S.-J.; Bae, S.H.; Son, J.S.; Kim, S.-N.; Kwak, B.O.; Lee, R. Interleukin-4 and tumor necrosis factor-alpha levels in children with febrile seizures. Seizure 2018, 58, 156–162. [Google Scholar] [CrossRef]
- Zhao, W.; Xie, W.; Xiao, Q.; Beers, D.R.; Appel, S.H. Protective effects of an anti-inflammatory cytokine, interleukin-4, on motoneuron toxicity induced by activated microglia. J. Neurochem. 2006, 99, 1176–1187. [Google Scholar] [CrossRef] [PubMed]
- Hart, Y.M.; Andermann, F.; Robitaille, Y.; Laxer, K.D.; Rasmussen, T.; Davis, R. Double pathology in Rasmussen’s syndrome: A window on the etiology? Neurology 1998, 50, 731–735. [Google Scholar] [CrossRef] [PubMed]
- Lagarde, S.; Villeneuve, N.; Trébuchon, A.; Kaphan, E.; Lepine, A.; McGonigal, A.; Roubertie, A.; Barthez, M.-A.J.; Trommsdorff, V.; Lefranc, J.; et al. Anti–tumor necrosis factor alpha therapy (adalimumab) in Rasmussen’s encephalitis: An open pilot study. Epilepsia 2016, 57, 956–966. [Google Scholar] [CrossRef] [PubMed]
- Varelas, P.N.; Mirski, M.A. Seizures in the Adult Intensive Care Unit. J. Neurosurg. Anesthesiol. 2001, 13, 163–175. [Google Scholar] [CrossRef]
- Castilla-Guerra, L.; Fernández-Moreno, M.d.C.; López-Chozas, J.M.; Fernández-Bolaños, R. Electrolytes Disturbances and Seizures. Epilepsia 2006, 47, 1990–1998. [Google Scholar] [CrossRef] [PubMed]
- Hitchings, A.W. Drugs that lower the seizure threshold. Adverse Drug React. Bull. 2016, 298, 1151–1154. [Google Scholar]
- Buchanan, N. Medications which may lower seizure threshold. Aust. Prescr. 2001, 24, 51–55. [Google Scholar] [CrossRef]
- Tesoro, E.P.; Brophy, G.M. Pharmacological Management of Seizures and Status Epilepticus in Critically Ill Patients. J. Pharm. Pract. 2010, 23, 441–454. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, L.J. Continuous EEG monitoring in the intensive care unit: An overview. J. Clin. Neurophysiol. Off. Publ. Am. Electroencephalogr. Soc. 2004, 21, 332–340. [Google Scholar] [CrossRef]
- Drislane, F.W.; Lopez, M.R.; Blum, A.S.; Schomer, D.L. Detection and Treatment of Refractory Status Epilepticus in the Intensive Care Unit. J. Clin. Neurophysiol. 2008, 25, 181–186. [Google Scholar] [CrossRef]
- Kubota, Y.; Nakamoto, H.; Egawa, S.; Kawamata, T. Continuous EEG monitoring in ICU. J. Intensive Care 2018, 6. [Google Scholar] [CrossRef] [PubMed]
- Boly, M.; Maganti, R. Monitoring epilepsy in the intensive care unit: Current state of facts and potential interest of high density EEG. Brain Inj. 2014, 28, 1151–1155. [Google Scholar] [CrossRef] [PubMed]
- Vespa, P.M.; Nenov, V.; Nuwer, M.R. Continuous EEG monitoring in the intensive care unit: Early findings and clinical efficacy. J. Clin. Neurophysiol. Off. Publ. Am. Electroencephalogr. Soc. 1999, 16, 1–13. [Google Scholar] [CrossRef]
- Pandian, J.D.; Cascino, G.D.; So, E.L.; Manno, E.; Fulgham, J.R. Digital video-electroencephalographic monitoring in the neurological-neurosurgical intensive care unit: Clinical features and outcome. Arch. Neurol. 2004, 61, 1090–1094. [Google Scholar] [CrossRef] [PubMed]
- Drake, M.E.; Padamadan, H.; Newell, S.A. Interictal quantitative EEG in epilepsy. Seizure 1998, 7, 39–42. [Google Scholar] [CrossRef][Green Version]
- van Putten, M.J.A.M.; Tavy, D.L.J. Continuous quantitative EEG monitoring in hemispheric stroke patients using the brain symmetry index. Stroke 2004, 35, 2489–2492. [Google Scholar] [CrossRef] [PubMed]
- Coates, S.; Clarke, A.; Davison, G.; Patterson, V. Tele-EEG in the UK: A report of over 1,000 patients. J. Telemed. Telecare 2012, 18, 243–246. [Google Scholar] [CrossRef]
- Hobbs, K.; Krishnamohan, P.; Legault, C.; Goodman, S.; Parvizi, J.; Gururangan, K.; Mlynash, M. Rapid Bedside Evaluation of Seizures in the ICU by Listening to the Sound of Brainwaves: A Prospective Observational Clinical Trial of Ceribell’s Brain Stethoscope Function. Neurocrit. Care 2018, 29, 302–312. [Google Scholar] [CrossRef]
- Waziri, A.; Claassen, J.; Stuart, R.M.; Arif, H.; Schmidt, J.M.; Mayer, S.A.; Badjatia, N.; Kull, L.L.; Connolly, E.S.; Emerson, R.G.; et al. Intracortical electroencephalography in acute brain injury. Ann. Neurol. 2009, 66, 366–377. [Google Scholar] [CrossRef]
- Yamazaki, M.; Terrill, M.; Fujimoto, A.; Yamamoto, T.; Tucker, D.M. Integrating dense array EEG in the presurgical evaluation of temporal lobe epilepsy. ISRN Neurol. 2012, 2012, 924081. [Google Scholar] [CrossRef]
- Yamazaki, M.; Tucker, D.M.; Fujimoto, A.; Yamazoe, T.; Okanishi, T.; Yokota, T.; Enoki, H.; Yamamoto, T. Comparison of dense array EEG with simultaneous intracranial EEG for interictal spike detection and localization. Epilepsy Res. 2012, 98, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Hutchinson, P.J.; Hutchinson, D.B.; Barr, R.H.; Burgess, F.; Kirkpatrick, P.J.; Pickard, J.D. A new cranial access device for cerebral monitoring. Br. J. Neurosurg. 2000, 14, 46–48. [Google Scholar] [CrossRef] [PubMed]
- Tavakoli, S.; Peitz, G.; Ares, W.; Hafeez, S.; Grandhi, R. Complications of invasive intracranial pressure monitoring devices in neurocritical care. Neurosurg. Focus 2017, 43, E6. [Google Scholar] [CrossRef] [PubMed]
- Ritter, A.C.; Wagner, A.K.; Fabio, A.; Pugh, M.J.; Walker, W.C.; Szaflarski, J.P.; Zafonte, R.D.; Brown, A.W.; Hammond, F.M.; Bushnik, T.; et al. Incidence and risk factors of posttraumatic seizures following traumatic brain injury: A Traumatic Brain Injury Model Systems Study. Epilepsia 2016, 57, 1968–1977. [Google Scholar] [CrossRef]
- Kodankandath, T.V.; Farooq, S.; Wazni, W.; Cox, J.-A.; Southwood, C.; Rozansky, G.; Johnson, V.; Lynch, J.R. Seizure Prophylaxis in the Immediate Post-Hemorrhagic Period in Patients with Aneurysmal Subarachnoid Hemorrhage. J. Vasc. Interv. Neurol. 2017, 9, 1–4. [Google Scholar]
- Yerram, S.; Katyal, N.; Premkumar, K.; Nattanmai, P.; Newey, C.R. Seizure prophylaxis in the neuroscience intensive care unit. J. Intensive Care 2018, 6. [Google Scholar] [CrossRef]
- Connolly, E.S.; Rabinstein, A.A.; Carhuapoma, J.R.; Derdeyn, C.P.; Dion, J.; Higashida, R.T.; Hoh, B.L.; Kirkness, C.J.; Naidech, A.M.; Ogilvy, C.S.; et al. Guidelines for the Management of Aneurysmal Subarachnoid Hemorrhage: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association. Stroke 2012, 43, 1711–1737. [Google Scholar] [CrossRef]
- Carney, N.; Totten, A.M.; O’Reilly, C.; Ullman, J.S.; Hawryluk, G.W.J.; Bell, M.J.; Bratton, S.L.; Chesnut, R.; Harris, O.A.; Kissoon, N.; et al. Guidelines for the Management of Severe Traumatic Brain Injury. Neurosurgery 2017, 80, 6–15. [Google Scholar]
- Temkin, N.R.; Dikmen, S.S.; Anderson, G.D.; Wilensky, A.J.; Holmes, M.D.; Cohen, W.; Newell, D.W.; Nelson, P.; Awan, A.; Winn, H.R. Valproate therapy for prevention of posttraumatic seizures: A randomized trial. J. Neurosurg. 1999, 91, 593–600. [Google Scholar] [CrossRef]
- Temkin, N.R.; Dikmen, S.S.; Wilensky, A.J.; Keihm, J.; Chabal, S.; Winn, H.R. A randomized, double-blind study of phenytoin for the prevention of post-traumatic seizures. N. Engl. J. Med. 1990, 323, 497–502. [Google Scholar] [CrossRef]
- Temkin, N.R. Antiepileptogenesis and seizure prevention trials with antiepileptic drugs: Meta-analysis of controlled trials. Epilepsia 2001, 42, 515–524. [Google Scholar] [CrossRef] [PubMed]
- Diringer, M.N.; Bleck, T.P.; Claude Hemphill, J.; Menon, D.; Shutter, L.; Vespa, P.; Bruder, N.; Connolly, E.S.; Citerio, G.; Gress, D.; et al. Critical Care Management of Patients Following Aneurysmal Subarachnoid Hemorrhage: Recommendations from the Neurocritical Care Society’s Multidisciplinary Consensus Conference. Neurocrit. Care 2011, 15, 211–240. [Google Scholar] [CrossRef] [PubMed]
- Alldredge, B.K.; Gelb, A.M.; Isaacs, S.M.; Corry, M.D.; Allen, F.; Ulrich, S.; Gottwald, M.D.; O’Neil, N.; Neuhaus, J.M.; Segal, M.R.; et al. A comparison of lorazepam, diazepam, and placebo for the treatment of out-of-hospital status epilepticus. N. Engl. J. Med. 2001, 345, 631–637. [Google Scholar] [CrossRef] [PubMed]
- Silbergleit, R.; Durkalski, V.; Lowenstein, D.; Conwit, R.; Pancioli, A.; Palesch, Y.; Barsan, W.; NETT Investigators. Intramuscular versus intravenous therapy for prehospital status epilepticus. N. Engl. J. Med. 2012, 366, 591–600. [Google Scholar] [CrossRef] [PubMed]
- Scheepers, M.; Scheepers, B.; Clarke, M.; Comish, S.; Ibitoye, M. Is intranasal midazolam an effective rescue medication in adolescents and adults with severe epilepsy? Seizure 2000, 9, 417–422. [Google Scholar] [CrossRef]
- Bhattacharyya, M.; Kalra, V.; Gulati, S. Intranasal midazolam vs rectal diazepam in acute childhood seizures. Pediatr. Neurol. 2006, 34, 355–359. [Google Scholar] [CrossRef]
- Buck, M.L.; Wiggins, B.S.; Sesler, J.M. Intraosseous Drug Administration in Children and Adults During Cardiopulmonary Resuscitation. Ann. Pharmacother. 2007, 41, 1679–1686. [Google Scholar] [CrossRef]
- Goodkin, H.P.; Sun, C.; Yeh, J.-L.; Mangan, P.S.; Kapur, J. GABAA Receptor Internalization during Seizures. Epilepsia 2007, 48, 109–113. [Google Scholar] [CrossRef]
- Glauser, T.; Shinnar, S.; Gloss, D.; Alldredge, B.; Arya, R.; Bainbridge, J.; Bare, M.; Bleck, T.; Dodson, W.E.; Garrity, L.; et al. Evidence-Based Guideline: Treatment of Convulsive Status Epilepticus in Children and Adults: Report of the Guideline Committee of the American Epilepsy Society. Epilepsy Curr. 2016, 16, 48–61. [Google Scholar] [CrossRef]
- Kalss, G.; Rohracher, A.; Leitinger, M.; Pilz, G.; Novak, H.F.; Neuray, C.; Kreidenhuber, R.; Höfler, J.; Kuchukhidze, G.; Trinka, E. Intravenous brivaracetam in status epilepticus: A retrospective single-center study. Epilepsia 2018, 59 Suppl 2, 228–233. [Google Scholar] [CrossRef]
- Santamarina, E.; Carbonell, B.P.; Sala, J.; Gutiérrez-Viedma, Á.; Miró, J.; Asensio, M.; Abraira, L.; Falip, M.; Ojeda, J.; López-González, F.J.; et al. Use of intravenous brivaracetam in status epilepticus: A multicenter registry. Epilepsia 2019, 0. [Google Scholar] [CrossRef] [PubMed]
- Strzelczyk, A.; Steinig, I.; Willems, L.M.; Reif, P.S.; Senft, C.; Voss, M.; Gaida, B.; von Podewils, F.; Rosenow, F. Treatment of refractory and super-refractory status epilepticus with brivaracetam: A cohort study from two German university hospitals. Epilepsy Behav. EB 2017, 70, 177–181. [Google Scholar] [CrossRef] [PubMed]
- Farrokh, S.; Bon, J.; Erdman, M.; Tesoro, E. Use of Newer Anticonvulsants for the Treatment of Status Epilepticus. Pharmacother. J. Hum. Pharmacol. Drug Ther. 2019, 39, 297–316. [Google Scholar] [CrossRef]
- Strzelczyk, A.; Zöllner, J.P.; Willems, L.M.; Jost, J.; Paule, E.; Schubert-Bast, S.; Rosenow, F.; Bauer, S. Lacosamide in status epilepticus: Systematic review of current evidence. Epilepsia 2017, 58, 933–950. [Google Scholar] [CrossRef] [PubMed]
- Treiman, D.M.; Meyers, P.D.; Walton, N.Y.; Collins, J.F.; Colling, C.; Rowan, A.J.; Handforth, A.; Faught, E.; Calabrese, V.P.; Uthman, B.M.; et al. A comparison of four treatments for generalized convulsive status epilepticus. Veterans Affairs Status Epilepticus Cooperative Study Group. N. Engl. J. Med. 1998, 339, 792–798. [Google Scholar] [CrossRef]
- Farrokh, S.; Tahsili-Fahadan, P.; Ritzl, E.K.; Lewin, J.J.; Mirski, M.A. Antiepileptic drugs in critically ill patients. Crit. Care 2018, 22, 153. [Google Scholar] [CrossRef] [PubMed]
- Lexicomp. Available online: https://online.lexi.com/lco/action/home (accessed on 5 September 2018).
- Garnett, W.R. Clinical Pharmacology of Topiramate: A Review. Epilepsia 2000, 41, 61–65. [Google Scholar] [CrossRef]
- Wu, Y.W.; Shek, D.W.; Garcia, P.A.; Zhao, S.; Johnston, S.C. Incidence and mortality of generalized convulsive status epilepticus in California. Neurology 2002, 58, 1070–1076. [Google Scholar] [CrossRef]
- Guidelines for Standard Order Sets. Available online: https://www.ismp.org/guidelines/standard-order-sets (accessed on 3 October 2018).
- Mahmoud, S.H. Antiepileptic Drug Removal by Continuous Renal Replacement Therapy: A Review of the Literature. Clin. Drug Investig. 2017, 37, 7–23. [Google Scholar] [CrossRef]
- Schetz, M.; Ferdinande, P.; Van den Berghe, G.; Verwaest, C.; Lauwers, P. Pharmacokinetics of continuous renal replacement therapy. Intensive Care Med. 1995, 21, 612–620. [Google Scholar] [CrossRef]
- Lewis, J.H.; Stine, J.G. Review article: Prescribing medications in patients with cirrhosis—A practical guide. Aliment. Pharmacol. Ther. 2013, 37, 1132–1156. [Google Scholar] [CrossRef] [PubMed]
- Cheng, V.; Abdul-Aziz, M.-H.; Roberts, J.A.; Shekar, K. Optimising drug dosing in patients receiving extracorporeal membrane oxygenation. J. Thorac. Dis. 2018, 10, S629–S641. [Google Scholar] [CrossRef] [PubMed]
- Shekar, K.; Roberts, J.A.; Mcdonald, C.I.; Ghassabian, S.; Anstey, C.; Wallis, S.C.; Mullany, D.V.; Fung, Y.L.; Fraser, J.F. Protein-bound drugs are prone to sequestration in the extracorporeal membrane oxygenation circuit: Results from an ex vivo study. Crit. Care Lond. Engl. 2015, 19, 164. [Google Scholar] [CrossRef] [PubMed]
- Lynch, T.; Price, A.L. The Effect of Cytochrome P450 Metabolism on Drug Response, Interactions, and Adverse Effects. Am. Fam. Physician 2007, 76, 391–396. [Google Scholar]
- McElnay, J.C.; D’Arcy, P.F. Protein binding displacement interactions and their clinical importance. Drugs 1983, 25, 495–513. [Google Scholar] [CrossRef]
- Schleibinger, M.; Steinbach, C.L.; Töpper, C.; Kratzer, A.; Liebchen, U.; Kees, F.; Salzberger, B.; Kees, M.G. Protein binding characteristics and pharmacokinetics of ceftriaxone in intensive care unit patients. Br. J. Clin. Pharmacol. 2015, 80, 525–533. [Google Scholar] [CrossRef]
- Lindow, J.; Wijdicks, E.F. Phenytoin toxicity associated with hypoalbuminemia in critically ill patients. Chest 1994, 105, 602–604. [Google Scholar] [CrossRef]
- Wen, Z.-P.; Fan, S.-S.; Du, C.; Yin, T.; Zhou, B.-T.; Peng, Z.-F.; Xie, Y.-Y.; Zhang, W.; Chen, Y.; Xiao, J.; et al. Drug-drug interaction between valproic acid and meropenem: A retrospective analysis of electronic medical records from neurosurgery inpatients. J. Clin. Pharm. Ther. 2017, 42, 221–227. [Google Scholar] [CrossRef]
- Suzuki, E.; Yamamura, N.; Ogura, Y.; Nakai, D.; Kubota, K.; Kobayashi, N.; Miura, S.; Okazaki, O. Identification of Valproic Acid Glucuronide Hydrolase as a Key Enzyme for the Interaction of Valproic Acid with Carbapenem Antibiotics. Drug Metab. Dispos. 2010, 38, 1538–1544. [Google Scholar] [CrossRef]
- Bede, P.; Lawlor, D.; Solanki, D.; Delanty, N. Carbapenems and valproate: A consumptive relationship. Epilepsia Open 2016, 2, 107–111. [Google Scholar] [CrossRef]
- Klotz, U. Pharmacokinetics and drug metabolism in the elderly. Drug Metab. Rev. 2009, 41, 67–76. [Google Scholar] [CrossRef] [PubMed]
- Hutchison, L.C.; O’Brien, C.E. Changes in Pharmacokinetics and Pharmacodynamics in the Elderly Patient. J. Pharm. Pract. 2007, 20, 4–12. [Google Scholar] [CrossRef]
- Batchelor, H.K.; Marriott, J.F. Paediatric pharmacokinetics: Key considerations. Br. J. Clin. Pharmacol. 2015, 79, 395–404. [Google Scholar] [CrossRef] [PubMed]
- Loebstein, R.; Lalkin, A.; Koren, G. Pharmacokinetic Changes During Pregnancy and Their Clinical Relevance. Clin. Pharmacokinet. 1997, 33, 328–343. [Google Scholar] [CrossRef] [PubMed]
| Condition | |
|---|---|
| Pre-existing epilepsy | Traumatic brain injury |
| Central nervous system infection | Ischemic stroke |
| Brain tumor | Hypoxic ischemic encephalopathy |
| Neurosurgical procedure | Altered mental status |
| Intracerebral hemorrhage | Drug toxicity/withdrawal |
| Subarachnoid hemorrhage | Toxic metabolic encephalopathy |
| Subdural hemorrhage | Congenital |
| Medication Class | Select Medications |
|---|---|
| Antimicrobials | Carbapenems (imipenem, meropenem), cephalosporins (cefepime), fluoroquinolones (levofloxacin), macrolides (erythromycin), penicillins, isoniazid, linezolid, metronidazole, amphotericin, fluconazole, mefloquine, chloroquine, pyrimethamine, acyclovir, ganciclovir, foscarnet |
| Analgesics | Alfentanyl, codeine, fentanyl, meperidine, morphine, NSAIDs, pentazocine, tramadol |
| Antihistamines | Cyproheptadine, promethazine |
| Antiasthmatics | Albuterol, aminophylline, theophylline, terbutaline |
| Antineoplastics | Alkylating agents (busulfan, carmustine, chlorambucil), Platinum analogs (cisplatin), cytarabine, methotrexate, vinblastine, vincristine |
| Anesthetics | Bupivacaine, etomidate, lidocaine, mepivacaine, methohexital, procaine, tetracaine |
| Antipsychotics | Clozapine, haloperidol, lithium, olanzapine, risperidone, phenothiazines, pimozide, thiothixene |
| Antidepressants | Bupropion, TCAs, SSRIs, MAOIs, doxepin, trazodone, venlafaxine |
| Antiarrhythmics | Digoxin, flecainide |
| Alpha/beta agonists/antagonists | Ephedrine, esmolol, propranolol |
| Immunosuppressants | Cyclosporine, hydrocortisone, INF-α, methylprednisolone, Muromonab-CD3, sulfasalazine, tacrolimus |
| Stimulants | Dextroamphetamine, methylphenidate |
| Other | Atropine, baclofen, bromocriptine, desmopressin, flumazenil, levodopa, metrizamide, cyclosporine, oxytocin, sumatriptan |
| Anticonvulsant Drug and Mechanism | Initial Dosing * | Protein Binding | Half-Life | Metabolism | Elimination | Adverse Effects |
|---|---|---|---|---|---|---|
| Brivaracetam SV2A modulation | 100–200 mg over at least 2 min | ≤20% | ~9 h | Hydrolysis and hepatic via CYP2C19 | >95% renally, <10% as unchanged drug | Psychiatric disturbances, nystagmus |
| Diazepam GABA potentiation | 0.15 mg/kg (Max: 10 mg) undiluted up to 5 mg/min | 98% | Parent drug: 60–72 h Metabolite: 152–174 h | Hepatic via CYP3A4 and 2C19; active metabolites | Renally as glucuronide conjugates | Respiratory depression, hypotension (more common with rapid administration) |
| Fosphenytoin/ Phenytoin Na+ channel blockade | 20 mg/kg PE at 150 mg/kg/min PE 20 mg/kg at 50 mg/min | 90%–95% | 7–42 h | Fos: Prodrug, rapidly hydrolyzed to phenytoin. Hepatic via CYP2C9, 2C19, 3A4 | <5% renally as phenytoin metabolites | Hypotension, phlebitis, cardiac arrhythmias. Consider slower administration in elderly |
| Lacosamide Enhances slow inactivation of voltage-gated Na+ channels | 200–400 mg over 15–30 min | <15% | 13 h | Hepatic via CYP3A4, 2C9, and 2C19; inactive metabolite | ~40% renally as unchanged drug | PR interval prolongation, hypotension |
| Levetiracetam SV2A modulation, AMPA inhibition | 3000 mg or 60 mg/kg (Max: 4500 mg) at 2–5 mg/kg/min | <10% | 6–8 h | Nonhepatic hydrolysis | ~66% renally as unchanged drug | Agitation, irritability, psychotic symptoms |
| Lorazepam GABA potentiation | 0.1 mg/kg (Max: 4 mg per dose, may repeat once) up to 2 mg/min | ~91% | 12–18 h | Hepatic; rapidly conjugated to inactive metabolite | ~88% renally as inactive metabolites | Respiratory depression, hypotension (more common with rapid administration) |
| Midazolam GABA potentiation | 0.2 mg/kg IM (Max: 10 mg) | ~97% | 3 h | Extensively hepatic CYP3A4; 60% to 70% to active metabolite | ~90% renally as metabolites | Respiratory depression, hypotension |
| Pentobarbital GABA potentiation, AMPA inhibition | 5–15 mg/kg up to 50 mg/min; followed by a continuous infusion 1–5 mg/kg/h | 45%–70% | 15–50 h | Hepatic via hydroxylation and glucuronidation | <1% renally as unchanged drug | Respiratory depression (patient must be intubated), hypotension, constipation |
| Phenobarbital GABA potentiation, AMPA inhibition | 15–20 mg/kg at 50–100 mg/min | 50%–60% | 53–118 h | Hepatic via CYP2C9 and to a lesser extent 2C19 and 2E1, and by N-glucosidation | 25–50% renally as unchanged drug | Respiratory depression, hypotension, contains propylene glycol |
| Propofol GABA potentiation, NMDAR blockade | 1–2 mg/kg followed by infusion 20–80 mcg/kg/min | 97%–99% | 40 min; prolonged with extended infusions | Hepatic to water-soluble sulfate and glucuronide conjugates | ~90% renally as metabolites | Respiratory depression (patient must be intubated), hypotension, PRIS |
| Topiramate Blocks neuronal voltage-dependent Na+ channels, enhances GABAA activity, antagonizes AMPA/kainate receptors, weakly inhibits carbonic anhydrase | 200–400 mg NG/PO (not available IV) | 15%–41% | 19–23 h | ~20% hepatically via hydroxylation, hydrolysis, and glucuronidation. | ~70% renally as unchanged drug | Memory impairment, ↓ serum bicarbonate |
| Valproic Acid GABA potentiation, glutamate (NMDAR) inhibition, Na+ and Ca2+ channel blockade | 20–40 mg/kg at 3–6 mg/kg/min | 80%–90% | 9–19 h | Hepatic via glucuronide conjugation and mitochondrial beta-oxidation | 50–80% renally | Hepatotoxicity, pancreatitis, thrombocytopenia, hyperammonemia |
| Anticonvulsant Drug | Renal Impairment | Hepatic Impairment |
|---|---|---|
| Brivaracetam | Mild to severe impairment: No dosage adjustment ESRD with HD: Not recommended (not studied) | Mild to severe impairment (Child Pugh classes A, B, and C): Initial: 25 mg twice daily, up to a max of 75 mg twice daily |
| Fosphenytoin/Phenytoin | No empiric dosage adjustment necessary Total serum concentration is difficult to interpret in renal failure; free concentration highly preferred | May require dosing ↓. Close monitoring of serum drug concentrations recommended |
| Lacosamide | CrCl ≥ 30 mL/min: No dosage adjustment necessary. Consider dose ↓ in patients taking concomitant strong CYP3A4 or CYP2C9 inhibitors CrCl < 30 mL/min: ↓ to 75% of the max dose. Further dose ↓ may be necessary with concomitant use of strong CYP3A4 or CYP2C9 inhibitors ESRD requiring HD: ↓ to 75% of the max dose. Further dose ↓ may be necessary with concomitant use of strong CYP3A4 or CYP2C9 inhibitors. Post-HD, consider supplemental dose of up to 50% | Mild to moderate hepatic impairment: ↓ dose to 75% of max dose. Further dose ↓ may be necessary in patients taking concomitant strong CYP3A4 and/or CYP2C9 inhibitors Severe hepatic impairment: Use not recommended |
| Levetiracetam | CrCl > 80 mL/min/1.73 m2: 500–1500 mg every 12 h CrCl 50–80 mL/min/1.73 m2: 500–1000 mg every 12 h CrCl 30–50 mL/min/1.73 m2: 250–750 mg every 12 h CrCl < 30 mL/min/1.73 m2: 250–500 mg every 12 h ESRD with HD: 500–1000 mg every 24 h; supplemental dose of 250–500 mg post-HD | No dosage adjustment necessary |
| Pentobarbital/ Phenobarbital | Dose ↓ recommended due to propylene glycol and potential for neurotoxicity (no specific guidance) | Dose ↓ recommended (no specific guidance) |
| Propofol | No dosage adjustment necessary | No dosage adjustment necessary |
| Topiramate | CrCl < 70 mL/min/1.73 m2: ↓ to 50% of normal dose and titrate slowly HD: 50–100 mg every 12 h; supplemental dose (50 to 100 mg) post-HD | No dosage adjustment necessary |
| Valproic Acid | No dosage adjustment necessary | Avoid |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Strein, M.; Holton-Burke, J.P.; Smith, L.R.; Brophy, G.M. Prevention, Treatment, and Monitoring of Seizures in the Intensive Care Unit. J. Clin. Med. 2019, 8, 1177. https://doi.org/10.3390/jcm8081177
Strein M, Holton-Burke JP, Smith LR, Brophy GM. Prevention, Treatment, and Monitoring of Seizures in the Intensive Care Unit. Journal of Clinical Medicine. 2019; 8(8):1177. https://doi.org/10.3390/jcm8081177
Chicago/Turabian StyleStrein, Micheal, John P. Holton-Burke, LaTangela R. Smith, and Gretchen M. Brophy. 2019. "Prevention, Treatment, and Monitoring of Seizures in the Intensive Care Unit" Journal of Clinical Medicine 8, no. 8: 1177. https://doi.org/10.3390/jcm8081177
APA StyleStrein, M., Holton-Burke, J. P., Smith, L. R., & Brophy, G. M. (2019). Prevention, Treatment, and Monitoring of Seizures in the Intensive Care Unit. Journal of Clinical Medicine, 8(8), 1177. https://doi.org/10.3390/jcm8081177





