Risks Related to the Use of Non-Steroidal Anti-Inflammatory Drugs in Community-Acquired Pneumonia in Adult and Pediatric Patients
Abstract
1. Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) Are Commonly Used to Alleviate Symptoms during Community-Acquired Pneumonia
2. Potential Benefits of NSAIDs during Pneumonia Have Been Explored for Decades, with Conflicting Results
3. NSAIDs Impair the Resolution of Inflammation through COX-2 Inhibition
4. NSAID Exposure during Extra-Pulmonary Infections: A Warning Signal
5. NSAID Exposure during Pneumonia: Numerous Studies Support a Risk of Complicated Course
5.1. In Hospitalized Children
5.2. In Adults Admitted to Intensive Care Units (ICUs)
5.3. In Hospitalized Adults
6. Synthesis of Human Data and Mechanistic Hypotheses
- -
- Temporal hypothesis: By alleviating the major symptoms of inflammation such as fever and pain, NSAID intake might impede the timely recognition and delay the diagnosis of pneumonia and the subsequent initiation of an appropriate antibiotic therapy. The delayed treatment may promote a more invasive disease, with a higher frequency of pleural empyema and bacteremia.
- -
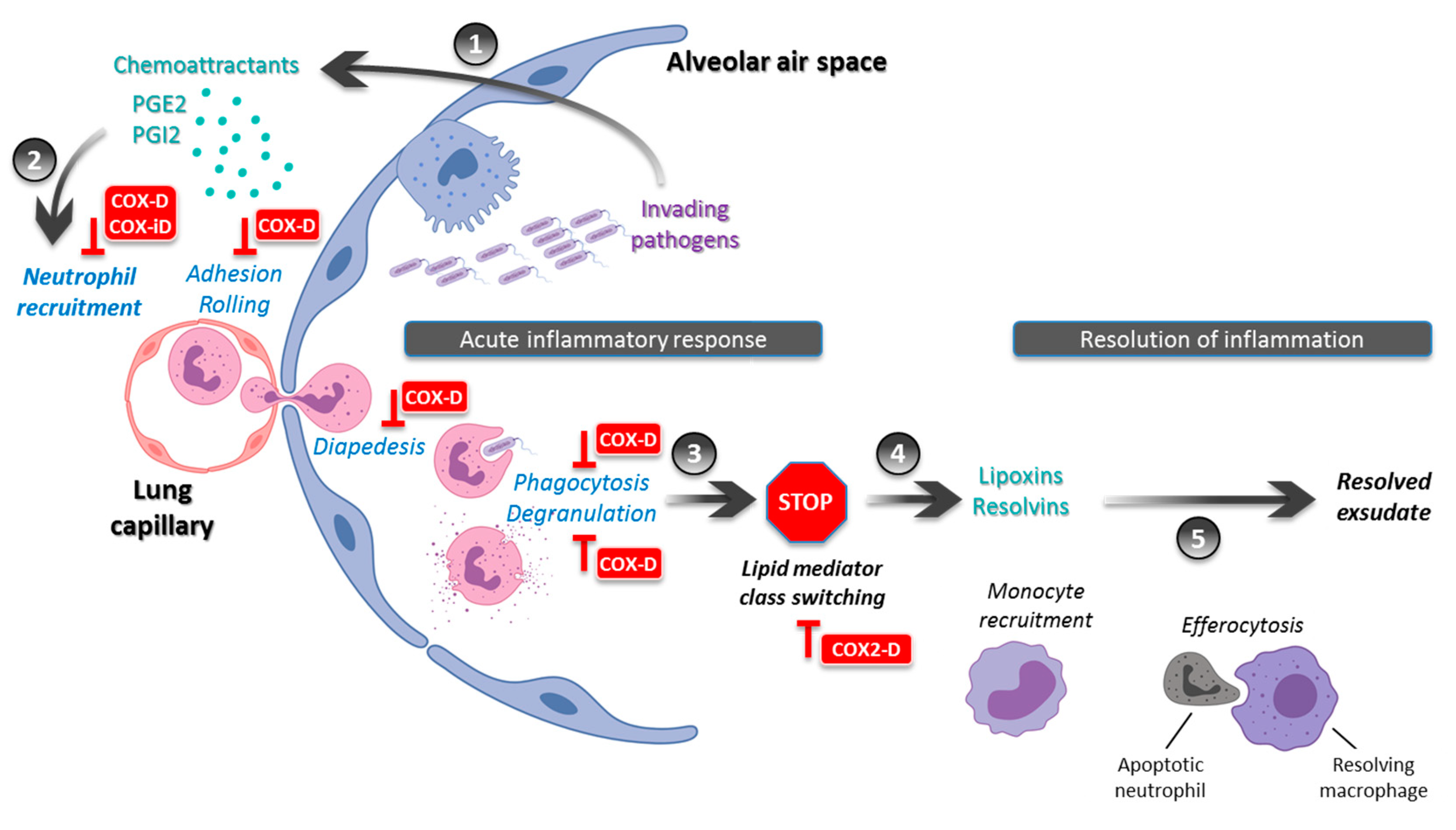
- Immunological hypothesis: During pneumonia, NSAIDs may limit the local recruitment of innate immune cells and alter the intrinsic functions of PMNs including phagocytosis and ROS production (Figure 1). This would result in a lower bacterial clearance and a local noncontainment of the infectious process. This alteration of the immune response may promote multilobar and/or bilateral pneumonia as well as cavitation and pleural effusion. Moreover, the inhibition of COX-2-induced lipid mediator class switching may extend the acute phase and delay the resolution of inflammation (Figure 1). This would result in a prolonged disease with delayed clinical stability and a longer hospital length of stay.
7. Conclusions
Author Contributions
Conflicts of Interest
References
- Almirall, J.; Bolibar, I.; Vidal, J.; Sauca, G.; Coll, P.; Niklasson, B.; Bartolome, M.; Balanzo, X. Epidemiology of community-acquired pneumonia in adults: A population-based study. Eur. Respir. J. 2000, 15, 757–763. [Google Scholar] [CrossRef]
- Welte, T.; Torres, A.; Nathwani, D. Clinical and economic burden of community-acquired pneumonia among adults in Europe. Thorax 2012, 67, 71–79. [Google Scholar] [CrossRef]
- Partouche, H.; Du Vaure, C.B.; Personne, V.; Le Cossec, C.; Garcin, C.; Lorenzo, A.; Ghasarossian, C.; Landais, P.; Toubiana, L.; Gilberg, S. Suspected community-acquired pneumonia in an ambulatory setting (CAPA): A French prospective observational cohort study in general practice. NPJ Prim. Care Respir. Med. 2015, 25, 15010. [Google Scholar] [CrossRef] [PubMed]
- Taytard, A.; Daures, J.P.; Arsac, P.; Chirumberro, J.L.; Grignet, J.P.; Micoud, M.; Poirier, R.; Romand, P.; Tartavel, J.M.; Touron, D. Prise en charge des infections respiratoires basses en médecine générale en France. Revue des Maladies Respiratoires 2001, 18, 163. [Google Scholar] [PubMed]
- Raherison, C.; Peray, P.; Poirier, R.; Romand, P.; Grignet, J.-P.; Arsac, P.; Taytard, A.; Daures, J.-P. Management of lower respiratory tract infections by French general practitioners: The AIR II study. Eur. Respir. J. 2002, 19, 314–319. [Google Scholar] [CrossRef]
- Raherison, C.; Poirier, R.; Daurès, J.P.; Romand, P.; Grignet, J.P.; Arsac, P.; Tartavel, J.M.; Touron, D.; Taytard, A. Lower respiratory tract infections in adults: Non-antibiotic prescriptions by GPs. Respir. Med. 2003, 97, 995–1000. [Google Scholar] [CrossRef]
- Qato, D.M.; Wilder, J.; Schumm, L.P.; Gillet, V.; Alexander, G.C. Changes in Prescription and Over-the-Counter Medication and Dietary Supplement Use Among Older Adults in the United States, 2005 vs. 2011. JAMA Intern. Med. 2016, 176, 473. [Google Scholar] [CrossRef] [PubMed]
- Gómez-Acebo, I.; Dierssen-Sotos, T.; de Pedro, M.; Pérez-Gómez, B.; Castaño-Vinyals, G.; Fernández-Villa, T.; Palazuelos-Calderón, C.; Amiano, P.; Etxeberria, J.; Benavente, Y.; et al. Epidemiology of non-steroidal anti-inflammatory drugs consumption in Spain. The MCC-Spain study. BMC Public Health 2018, 18, 1134. [Google Scholar] [CrossRef]
- Mandell, L.A.; Wunderink, R.G.; Anzueto, A.; Bartlett, J.G.; Campbell, G.D.; Dean, N.C.; Dowell, S.F.; File, T.M.; Musher, D.M.; Niederman, M.S.; et al. Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2007, 44, 27–72. [Google Scholar] [CrossRef]
- Lim, W.S.; Baudouin, S.V.; George, R.C.; Hill, A.T.; Jamieson, C.; Le Jeune, I.; Macfarlane, J.T.; Read, R.C.; Roberts, H.J.; Levy, M.L.; et al. BTS guidelines for the management of community acquired pneumonia in adults: Update 2009. Thorax 2009, 64, 1–55. [Google Scholar] [CrossRef]
- Woodhead, M.; Blasi, F.; Ewig, S.; Garau, J.; Huchon, G.; Ieven, M.; Ortqvist, A.; Schaberg, T.; Torres, A.; van der Heijden, G.; et al. Guidelines for the management of adult lower respiratory tract infections - Full version. Clin. Microbiol. Infect. 2011, 17, 1–59. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.Y.; Chang, Y.-J.; Cho, H.M.; Hwang, Y.-W.; Moon, Y.S. Non-steroidal anti-inflammatory drugs for the common cold. Cochrane Database Syst. Rev. 2015. [Google Scholar] [CrossRef] [PubMed]
- Eccles, R. Efficacy and safety of over-the-counter analgesics in the treatment of common cold and flu. J. Clin. Pharm. Ther. 2006, 31, 309–319. [Google Scholar] [CrossRef] [PubMed]
- Mizgerd, J.P. Acute lower respiratory tract infection. N. Engl. J. Med. 2008, 358, 716–727. [Google Scholar] [CrossRef] [PubMed]
- Chouaib, S.; Bertoglio, J.H. Prostaglandins E as modulators of the immune response. Lymphokine Res. 1988, 7, 237–245. [Google Scholar]
- Kaplan, H.B.; Edelson, H.S.; Korchak, H.M.; Given, W.P.; Abramson, S.; Weissmann, G. Effects of non-steroidal anti-inflammatory agents on human neutrophil functions in vitro and in vivo. Biochem. Pharmacol. 1984, 33, 371–378. [Google Scholar] [CrossRef]
- Ip, M.; Lomas, D.A.; Shaw, J.; Burnett, D.; Stockley, R.A. Effect of non-steroidal anti-inflammatory drugs on neutrophil chemotaxis--An in vitro and in vivo study. Br. J. Rheumatol. 1990, 29, 363–367. [Google Scholar] [CrossRef]
- Perianin, A.; Roch-Arveiller, M.; Giroud, J.P.; Hakim, J. In vivo interaction of nonsteroidal anti-inflammatory drugs on the locomotion of neutrophils elicited by acute non-specific inflammations in the rat--effect of indomethacin, ibuprofen and flurbiprofen. Biochem. Pharmacol. 1984, 33, 2239–2243. [Google Scholar] [CrossRef]
- Dauletbaev, N.; Lam, J.; Eklove, D.; Iskandar, M.; Lands, L.C. Ibuprofen modulates NF-kB activity but not IL-8 production in cystic fibrosis respiratory epithelial cells. Respir. Int. Rev. Thorac. Dis. 2010, 79, 234–242. [Google Scholar]
- Rocca, J.; Manin, S.; Hulin, A.; Aissat, A.; Verbecq-Morlot, W.; Prulière-Escabasse, V.; Wohlhuter-Haddad, A.; Epaud, R.; Fanen, P.; Tarze, A. New use for an old drug: COX-independent anti-inflammatory effects of sulindac in models of cystic fibrosis. Br. J. Pharmacol. 2016, 173, 1728–1741. [Google Scholar] [CrossRef]
- Konstan, M.W.; Vargo, K.M.; Davis, P.B. Ibuprofen Attenuates the Inflammatory Response to Pseudomonas aeruginosa in a Rat Model of Chronic Pulmonary Infection: Implications for Antiinflammatory Therapy in Cystic Fibrosis1-4. Am. Rev. Respir. Dis. 1990, 141, 186–192. [Google Scholar] [CrossRef] [PubMed]
- Sordelli, D.O.; Cerquetti, M.C.; Fontán, P.A.; Meiss, R.P. Piroxicam treatment protects mice from lethal pulmonary challenge with Pseudomonas aeruginosa. J. Infect. Dis. 1989, 159, 232–238. [Google Scholar] [CrossRef] [PubMed]
- Sordelli, D.O.; Cerquetti, M.C.; el-Tawil, G.; Ramwell, P.W.; Hooke, A.M.; Bellanti, J.A. Ibuprofen modifies the inflammatory response of the murine lung to Pseudomonas aeruginosa. Eur. J. Respir. Dis. 1985, 67, 118–127. [Google Scholar] [PubMed]
- Esposito, A.L. Aspirin impairs antibacterial mechanisms in experimental pneumococcal pneumonia. Am. Rev. Respir. Dis. 1984, 130, 857–862. [Google Scholar] [PubMed]
- Fletcher, J.R.; Ramwell, P.W. Modification, by aspirin and indomethacin, of the haemodynamic and prostaglandin releasing effects of E. coli endotoxin in the dog. Br. J. Pharmacol. 1977, 61, 175–181. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, J.R.; Ramwell, P.W. Indomethacin improves survival after endotoxin in baboons. Adv. Prostaglandin Thromboxane Res. 1980, 7, 821–828. [Google Scholar] [PubMed]
- Parratt, J.R.; Sturgess, R.M. E. coli endotoxin shock in the cat; treatment with indomethacin. Br. J. Pharmacol. 1975, 53, 485–488. [Google Scholar] [CrossRef] [PubMed]
- Sprague, R.S.; Stephenson, A.H.; Lonigro, A.J. Prostaglandin I2 supports blood flow to hypoxic alveoli in anesthetized dogs. J. Appl. Physiol. 1984, 56, 1246–1251. [Google Scholar] [CrossRef] [PubMed]
- Hanly, P.; Sienko, A.; Light, R.B. Effect of cyclooxygenase blockade on gas exchange and hemodynamics in Pseudomonas pneumonia. J. Appl. Physiol. Bethesda Md 1985 1987, 63, 1829–1836. [Google Scholar] [CrossRef]
- Ferrer, M.; Torres, A.; Baer, R.; Hernández, C.; Roca, J.; Rodriguez-Roisin, R. Effect of acetylsalicylic acid on pulmonary gas exchange in patients with severe pneumonia: A pilot study. Chest 1997, 111, 1094–1100. [Google Scholar] [CrossRef]
- Hanly, P.J.; Roberts, D.; Dobson, K.; Light, R.B. Effect of indomethacin on arterial oxygenation in critically ill patients with severe bacterial pneumonia. Lancet Lond. Engl. 1987, 1, 351–354. [Google Scholar] [CrossRef]
- Bernard, G.R.; Wheeler, A.P.; Russell, J.A.; Schein, R.; Summer, W.R.; Steinberg, K.P.; Fulkerson, W.J.; Wright, P.E.; Christman, B.W.; Dupont, W.D.; et al. The effects of ibuprofen on the physiology and survival of patients with sepsis. The Ibuprofen in Sepsis Study Group. N. Engl. J. Med. 1997, 336, 912–918. [Google Scholar] [CrossRef]
- Levy, B.D.; Clish, C.B.; Schmidt, B.; Gronert, K.; Serhan, C.N. Lipid mediator class switching during acute inflammation: signals in resolution. Nat. Immunol. 2001, 2, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Serhan, C.N. Pro-resolving lipid mediators are leads for resolution physiology. Nature 2014, 510, 92–101. [Google Scholar] [CrossRef] [PubMed]
- Fukunaga, K.; Kohli, P.; Bonnans, C.; Fredenburgh, L.E.; Levy, B.D. Cyclooxygenase 2 plays a pivotal role in the resolution of acute lung injury. J. Immunol. Baltim. Md 1950 2005, 174, 5033–5039. [Google Scholar] [CrossRef]
- Gilroy, D.W.; Colville-Nash, P.R.; Willis, D.; Chivers, J.; Paul-Clark, M.J.; Willoughby, D.A. Inducible cyclooxygenase may have anti-inflammatory properties. Nat. Med. 1999, 5, 698–701. [Google Scholar] [CrossRef] [PubMed]
- Brun-Buisson, C.J.; Saada, M.; Trunet, P.; Rapin, M.; Roujeau, J.C.; Revuz, J. Haemolytic streptococcal gangrene and non-steroidal anti-inflammatory drugs. Br. Med. J. Clin. Res. Ed 1985, 290, 1786. [Google Scholar] [CrossRef] [PubMed]
- Aronoff, D.M.; Bloch, K.C. Assessing the relationship between the use of nonsteroidal antiinflammatory drugs and necrotizing fasciitis caused by group A streptococcus. Medicine (Baltimore) 2003, 82, 225–235. [Google Scholar] [CrossRef] [PubMed]
- Souyri, C.; Olivier, P.; Grolleau, S.; Lapeyre-Mestre, M. French Network of Pharmacovigilance Centres Severe necrotizing soft-tissue infections and nonsteroidal anti-inflammatory drugs. Clin. Exp. Dermatol. 2008, 33, 249–255. [Google Scholar] [CrossRef]
- Avril, M.F.; Peyramond, D. Érysipèle et fasciite nécrosante: prise en charge Texte court. Médecine Mal. Infect. 2000, 30, 239–240. [Google Scholar] [CrossRef]
- Mikaeloff, Y.; Kezouh, A.; Suissa, S. Nonsteroidal anti-inflammatory drug use and the risk of severe skin and soft tissue complications in patients with varicella or zoster disease. Br. J. Clin. Pharmacol. 2008, 65, 203–209. [Google Scholar] [CrossRef]
- Lepelletier, D.; Pinaud, V.; Le Conte, P.; Bourigault, C.; Asseray, N.; Ballereau, F.; Caillon, J.; Ferron, C.; Righini, C.; Batard, E.; et al. Is there an association between prior anti-inflammatory drug exposure and occurrence of peritonsillar abscess (PTA)? A national multicenter prospective observational case-control study. Eur. J. Clin. Microbiol. Infect. Dis. Off. Publ. Eur. Soc. Clin. Microbiol. 2017, 36, 57–63. [Google Scholar] [CrossRef]
- Le Turnier, P.; Boutoille, D.; Joyau, C.; Veyrac, G.; Asseray, N. Bacterial infections and NSAIDs exposure? Seek septic complications. Eur. J. Intern. Med. 2017, 41, 33–34. [Google Scholar] [CrossRef] [PubMed]
- Legras, A.; Giraudeau, B.; Jonville-Bera, A.-P.; Camus, C.; François, B.; Runge, I.; Kouatchet, A.; Veinstein, A.; Tayoro, J.; Villers, D.; et al. A multicentre case-control study of nonsteroidal anti-inflammatory drugs as a risk factor for severe sepsis and septic shock. Crit. Care Lond. Engl. 2009, 13, 43. [Google Scholar] [CrossRef] [PubMed]
- François, P.; Desrumaux, A.; Cans, C.; Pin, I.; Pavese, P.; Labarère, J. Prevalence and risk factors of suppurative complications in children with pneumonia. Acta Paediatr. Oslo Nor. 1992 2010, 99, 861–866. [Google Scholar] [CrossRef] [PubMed]
- Byington, C.L.; Spencer, L.Y.; Johnson, T.A.; Pavia, A.T.; Allen, D.; Mason, E.O.; Kaplan, S.; Carroll, K.C.; Daly, J.A.; Christenson, J.C.; et al. An epidemiological investigation of a sustained high rate of pediatric parapneumonic empyema: risk factors and microbiological associations. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 2002, 34, 434–440. [Google Scholar] [CrossRef] [PubMed]
- Voiriot, G.; Dury, S.; Parrot, A.; Mayaud, C.; Fartoukh, M. Nonsteroidal Antiinflammatory Drugs May Affect the Presentation and Course of Community-Acquired Pneumonia. Chest 2011, 139, 387–394. [Google Scholar] [CrossRef]
- Messika, J.; Sztrymf, B.; Bertrand, F.; Billard-Pomares, T.; Barnaud, G.; Branger, C.; Dreyfuss, D.; Ricard, J.-D. Risks of nonsteroidal antiinflammatory drugs in undiagnosed intensive care unit pneumococcal pneumonia: younger and more severely affected patients. J. Crit. Care 2014, 29, 733–738. [Google Scholar] [CrossRef]
- Elemraid, M.A.; Thomas, M.F.; Blain, A.P.; Rushton, S.P.; Spencer, D.A.; Gennery, A.R.; Clark, J.E. North East of England Pediatric Respiratory Infection Study Group Newcastle upon Tyne, UK Risk factors for the development of pleural empyema in children. Pediatr. Pulmonol. 2015, 50, 721–726. [Google Scholar] [CrossRef]
- Le Bourgeois, M.; Ferroni, A.; Leruez-Ville, M.; Varon, E.; Thumerelle, C.; Brémont, F.; Fayon, M.J.; Delacourt, C.; Ligier, C.; Watier, L.; et al. Nonsteroidal Anti-Inflammatory Drug without Antibiotics for Acute Viral Infection Increases the Empyema Risk in Children: A Matched Case-Control Study. J. Pediatr. 2016, 175, 47–53. [Google Scholar] [CrossRef]
- Kotsiou, O.S.; Zarogiannis, S.G.; Gourgoulianis, K.I. Prehospital NSAIDs use prolong hospitalization in patients with pleuro-pulmonary infection. Respir. Med. 2017, 123, 28–33. [Google Scholar] [CrossRef] [PubMed]
- Basille, D.; Plouvier, N.; Trouve, C.; Duhaut, P.; Andrejak, C.; Jounieaux, V. Non-steroidal Anti-inflammatory Drugs may Worsen the Course of Community-Acquired Pneumonia: A Cohort Study. Lung 2017, 195, 201–208. [Google Scholar] [CrossRef] [PubMed]
- Krenke, K.; Krawiec, M.; Kraj, G.; Peradzynska, J.; Krauze, A.; Kulus, M. Risk factors for local complications in children with community-acquired pneumonia. Clin. Respir. J. 2018, 12, 253–261. [Google Scholar] [CrossRef] [PubMed]
- Basille, D.; Thomsen, R.W.; Madsen, M.; Duhaut, P.; Andrejak, C.; Jounieaux, V.; Sørensen, H.T. Non-steroidal Anti-inflammatory Drug Use and Clinical Outcomes of Community-acquired Pneumonia. Am. J. Respir. Crit. Care Med. 2018, 198, 128–131. [Google Scholar] [CrossRef] [PubMed]
- Horwitz, R.I.; Feinstein, A.R. The problem of “protopathic bias” in case-control studies. Am. J. Med. 1980, 68, 255–258. [Google Scholar] [CrossRef]
| Author; Study Period | Population (Number of Patients); Country | Study Drug | Care Setting | Study Design | Comment |
|---|---|---|---|---|---|
| Francois [45] 1995–2003 | Children (n = 767), CAP, France | Ibuprofen | Hospital ward | Retrospective case-control | Recent NSAID exposure was an independent risk factor of pleural empyema (OR 2.6 (1.5–4.4)) |
| Byington [46] 1993–1999 | Children (n = 540), CAP, United States | Ibuprofen | Hospital ward | Retrospective case-control | Recent NSAID exposure was an independent risk factor of pleural empyema (OR 4.0 (2.5–6.5)) |
| Voiriot [47] 2002–2006 | Adults (n = 90), CAP, France | NSAIDs | ICU | Prospective cohort | Recent NSAID exposure was an independent risk factor of pleuropulmonary complications (pleural empyema, excavation) (OR 8.1 (2.3–28)) |
| Messika [48] 1997–2009 | Adults (n = 106), pneumococcal CAP, France | NSAIDs | ICU | Historical cohort | Recent NSAID exposure was associated with a higher risk of pleuropulmonary complications (pleural empyema, excavation) (OR 5.8 (2.0–17)) |
| Elemraid [49] 2009–2011 | Children (n = 160), CAP, UK | Ibuprofen | Hospital ward | Prospective case-control | Recent NSAID exposure was involved in 82% of cases with pleural empyema, compared to 46% of cases without complications (OR 1.9 (0.8–3.2)) |
| Le Bourgeois [50] * 2006–2009 | Children (n = 83), viral LRTI, France | NSAIDs | Hospital ward | Prospective case-control | Recent NSAID exposure was an independent risk factor of pleural empyema (OR 2.8 (1.4–5.6)) |
| Kotsiou [51] 2015–2016 | Adults (n = 57), CAP, Greece | NSAIDs | Hospital ward | Prospective cohort | Pre-hospital NSAID use for more than 6 days was associated with a prolonged hospitalization duration |
| Basille [52] 2008–2013 | Adults (n = 221), CAP, France | NSAIDs | Hospital ward | Prospective cohort | Recent NSAID exposure was an independent risk factor of pleural empyema (OR 2.6 (1.02–6.6)) |
| Krenke [53] 2012–2014 | Children (n = 203), CAP, Poland | Ibuprofen | Hospital ward | Prospective cohort | A dose–effect relationship was found: exposure to a cumulative dose of ibuprofen higher than 78 mg/kg was significantly associated with an increased risk of pleuropulmonary complications, such as parapneumonic pleural effusion, pleural empyema, necrotizing pneumonia and pulmonary abscess (OR 2.5 (1.3–4.9)) |
| Basille [54] * 1997–2011 | Adults (n = 59,250), CAP, Denmark | NSAIDs | Hospital ward | Registry-based | NSAID exposure was associated with pleural empyema and/or lung abscess (RR 1.81 (1.60–2.05)) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Voiriot, G.; Philippot, Q.; Elabbadi, A.; Elbim, C.; Chalumeau, M.; Fartoukh, M. Risks Related to the Use of Non-Steroidal Anti-Inflammatory Drugs in Community-Acquired Pneumonia in Adult and Pediatric Patients. J. Clin. Med. 2019, 8, 786. https://doi.org/10.3390/jcm8060786
Voiriot G, Philippot Q, Elabbadi A, Elbim C, Chalumeau M, Fartoukh M. Risks Related to the Use of Non-Steroidal Anti-Inflammatory Drugs in Community-Acquired Pneumonia in Adult and Pediatric Patients. Journal of Clinical Medicine. 2019; 8(6):786. https://doi.org/10.3390/jcm8060786
Chicago/Turabian StyleVoiriot, Guillaume, Quentin Philippot, Alexandre Elabbadi, Carole Elbim, Martin Chalumeau, and Muriel Fartoukh. 2019. "Risks Related to the Use of Non-Steroidal Anti-Inflammatory Drugs in Community-Acquired Pneumonia in Adult and Pediatric Patients" Journal of Clinical Medicine 8, no. 6: 786. https://doi.org/10.3390/jcm8060786
APA StyleVoiriot, G., Philippot, Q., Elabbadi, A., Elbim, C., Chalumeau, M., & Fartoukh, M. (2019). Risks Related to the Use of Non-Steroidal Anti-Inflammatory Drugs in Community-Acquired Pneumonia in Adult and Pediatric Patients. Journal of Clinical Medicine, 8(6), 786. https://doi.org/10.3390/jcm8060786




