Perioperative Factors for Predicting the Need for Postoperative Intensive Care after Major Lung Resection
Abstract
1. Introduction
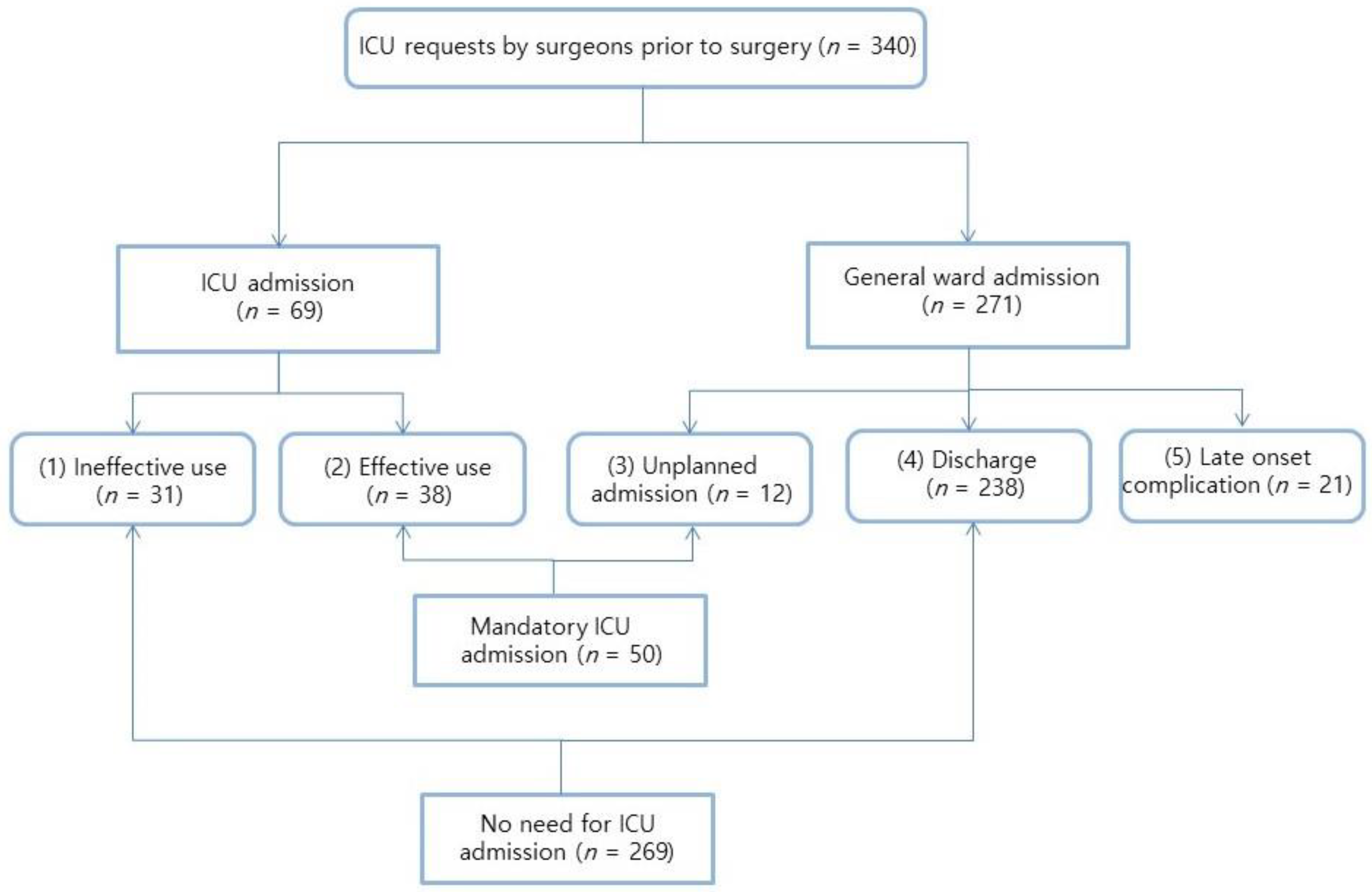
2. Patients and Methods
Statistical Analysis
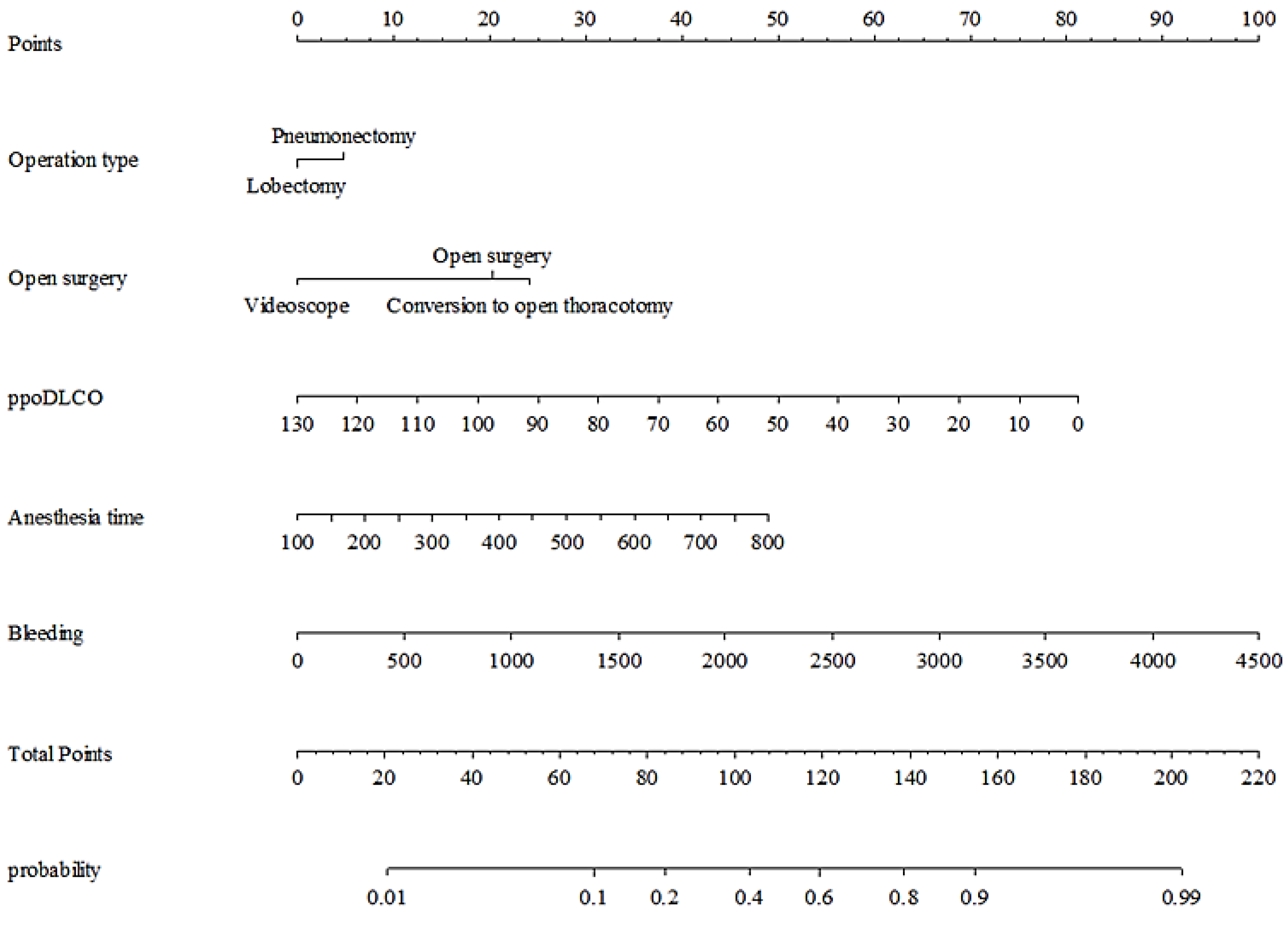
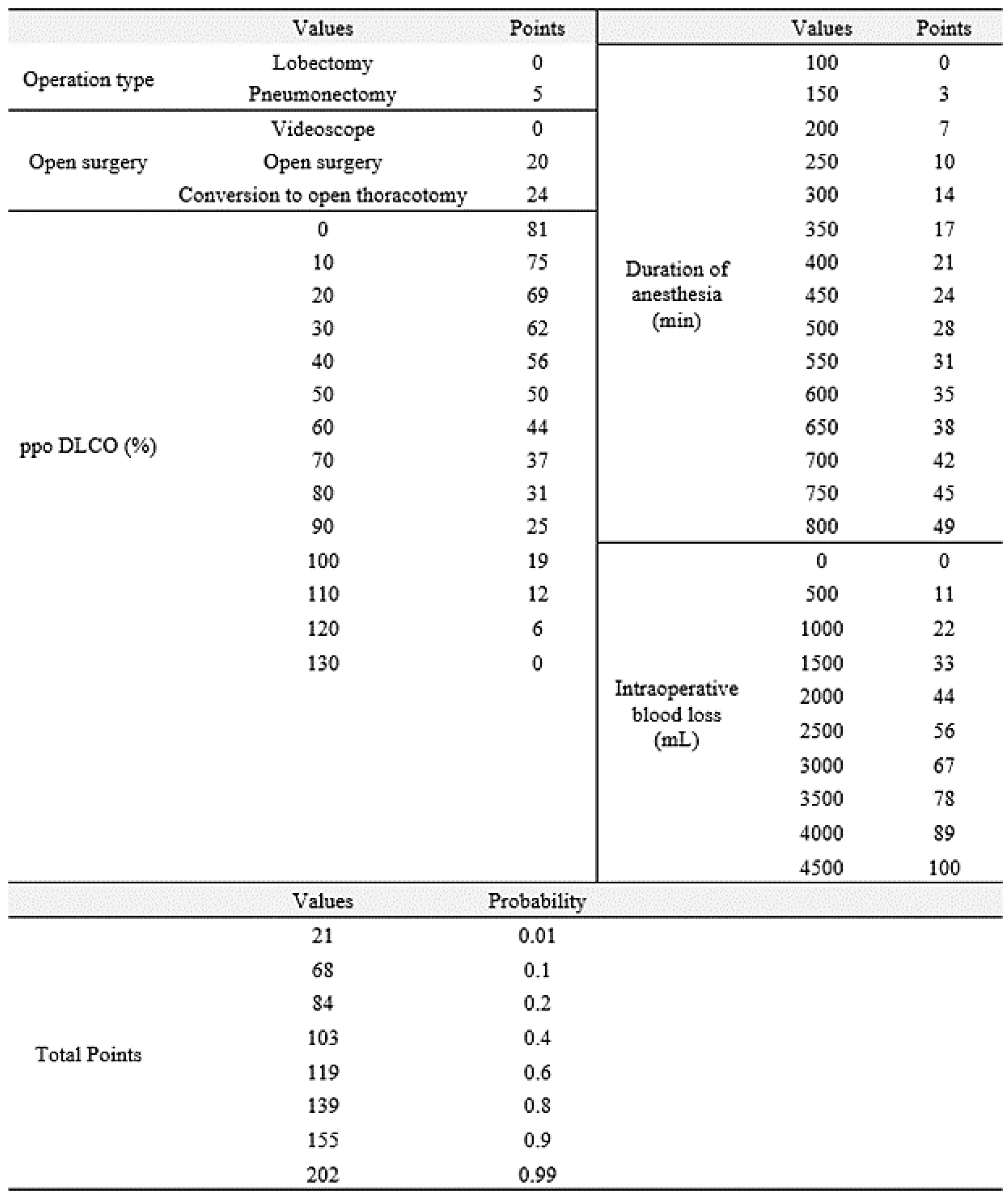
3. Results
4. Discussion
5. Conclusions
Author Contributions
Conflicts of Interest
References
- McCall, P.J.; Macfie, A.; Kinsella, J.; Shelley, B.G. Critical care after lung resection: Calor 1, a single-centre pilot study. Anaesthesia 2015, 70, 1382–1389. [Google Scholar] [CrossRef]
- Pieretti, P.; Alifano, M.; Roche, N.; Vincenzi, M.; Forti Parri, S.N.; Zackova, M.; Boaron, M.; Zanello, M. Predictors of an appropriate admission to an icu after a major pulmonary resection. Respir. Intern. Rev. Thorac. Dis. 2006, 73, 157–165. [Google Scholar] [CrossRef]
- Park, S.Y.; Park, I.K.; Hwang, Y.; Byun, C.S.; Bae, M.K.; Lee, C.Y. Immediate postoperative care in the general thoracic ward is safe for low-risk patients after lobectomy for lung cancer. Korean J. Thorac. Cardiovasc. Surg. 2011, 44, 229–235. [Google Scholar] [CrossRef]
- Pedoto, A.; Heerdt, P.M. Postoperative care after pulmonary resection: Postanesthesia care unit versus intensive care unit. Curr. Opin. Anaesthesiol. 2009, 22, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Pinheiro, L.; Santoro, I.L.; Perfeito, J.A.; Izbicki, M.; Ramos, R.P.; Faresin, S.M. Preoperative predictive factors for intensive care unit admission after pulmonary resection. J. Bras. Pneumol. 2015, 41, 31–38. [Google Scholar] [CrossRef][Green Version]
- Pinheiro, L.; Santoro, I.L.; Faresin, S.M. Who needs to be allocated in icu after thoracic surgery? An observational study. Can. Respir. J. 2016, 2016, 3981506. [Google Scholar] [CrossRef] [PubMed]
- Jordan, S.; Evans, T.W. Predicting the need for intensive care following lung resection. Thorac. Surg. Clin. 2008, 18, 61–69. [Google Scholar] [CrossRef] [PubMed]
- Okiror, L.; Patel, N.; Kho, P.; Ladas, G.; Dusmet, M.; Jordan, S.; Cordingley, J.; Lim, E. Predicting risk of intensive care unit admission after resection for non-small cell lung cancer: A validation study. Interact. Cardiovasc. Thorac. Surg. 2012, 14, 31–33. [Google Scholar] [CrossRef]
- Falcoz, P.E.; Conti, M.; Brouchet, L.; Chocron, S.; Puyraveau, M.; Mercier, M.; Etievent, J.P.; Dahan, M. The thoracic surgery scoring system (thoracoscore): Risk model for in-hospital death in 15,183 patients requiring thoracic surgery. J. Thorac. Cardiovasc. Surg. 2007, 133, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Brunelli, A.; Ferguson, M.K.; Rocco, G.; Pieretti, P.; Vigneswaran, W.T.; Morgan-Hughes, N.J.; Zanello, M.; Salati, M. A scoring system predicting the risk for intensive care unit admission for complications after major lung resection: A multicenter analysis. Ann. Thorac. Surg. 2008, 86, 213–218. [Google Scholar] [CrossRef]
- Seely, A.J.; Ivanovic, J.; Threader, J.; Al-Hussaini, A.; Al-Shehab, D.; Ramsay, T.; Gilbert, S.; Maziak, D.E.; Shamji, F.M.; Sundaresan, R.S. Systematic classification of morbidity and mortality after thoracic surgery. Ann. Thorac. Surg. 2010, 90, 936–942. [Google Scholar] [CrossRef]
- Birim, O.; Zuydendorp, H.M.; Maat, A.P.; Kappetein, A.P.; Eijkemans, M.J.; Bogers, A.J. Lung resection for non-small-cell lung cancer in patients older than 70: Mortality, morbidity, and late survival compared with the general population. Ann. Thorac. Surg. 2003, 76, 1796–1801. [Google Scholar] [CrossRef]
- Wang, Y.; Wu, N.; Zheng, Q.; Wang, J.; Yan, S.; Li, S.; Liu, Y.; Chen, J.; Yang, Y. Prediction of surgical outcome by modeling based on risk factors of morbidity after pulmonary resection for lung cancer in older adults. Ann. Thorac. Surg. 2016, 102, 971–978. [Google Scholar] [CrossRef] [PubMed]
- Park, J.S.; Kim, H.K.; Choi, Y.S.; Kim, J.; Shim, Y.M.; Kim, K. Unplanned conversion to thoracotomy during video-assisted thoracic surgery lobectomy does not compromise the surgical outcome. World J. Surg. 2011, 35, 590–595. [Google Scholar] [CrossRef] [PubMed]
- Byun, C.S.; Lee, S.; Kim, D.J.; Lee, J.G.; Lee, C.Y.; Jung, I.; Chung, K.Y. Analysis of unexpected conversion to thoracotomy during thoracoscopic lobectomy in lung cancer. Ann. Thorac. Surg. 2015, 100, 968–973. [Google Scholar] [CrossRef]
- Samson, P.; Guitron, J.; Reed, M.F.; Hanseman, D.J.; Starnes, S.L. Predictors of conversion to thoracotomy for video-assisted thoracoscopic lobectomy: A retrospective analysis and the influence of computed tomography-based calcification assessment. J. Thorac. Cardiovasc. Surg. 2013, 145, 1512–1518. [Google Scholar] [CrossRef] [PubMed]
- Amore, D.; Di Natale, D.; Scaramuzzi, R.; Curcio, C. Reasons for conversion during vats lobectomy: What happens with increased experience. J. Vis. Surg. 2018, 4, 53. [Google Scholar] [CrossRef]
- Mason, A.C.; Krasna, M.J.; White, C.S. The role of radiologic imaging in diagnosing complications of video-assisted thoracoscopic surgery. Chest 1998, 113, 820–825. [Google Scholar] [CrossRef]
- Miyazaki, T.; Yamasaki, N.; Tsuchiya, T.; Matsumoto, K.; Hatachi, G.; Kitamura, Y.; Obata, T.; Doi, R.; Machino, R.; Nagayasu, T. Management of unexpected intraoperative bleeding during thoracoscopic pulmonary resection: A single institutional experience. Surg. Today 2016, 46, 901–907. [Google Scholar] [CrossRef]
- Dreiseitl, S.; Harbauer, A.; Binder, M.; Kittler, H. Nomographic representation of logistic regression models: A case study using patient self-assessment data. J. Biomed. Inform. 2005, 38, 389–394. [Google Scholar] [CrossRef] [PubMed]
- Rotman, J.A.; Plodkowski, A.J.; Hayes, S.A.; de Groot, P.M.; Shepard, J.A.; Munden, R.F.; Ginsberg, M.S. Postoperative complications after thoracic surgery for lung cancer. Clin. Imaging 2015, 39, 735–749. [Google Scholar] [CrossRef]
- Gazala, S.; Hunt, I.; Valji, A.; Stewart, K.; Bedard, E.R. A method of assessing reasons for conversion during video-assisted thoracoscopic lobectomy. Interact. Cardiovasc. Thorac. Surg. 2011, 12, 962–964. [Google Scholar] [CrossRef][Green Version]
- Puri, V.; Patel, A.; Majumder, K.; Bell, J.M.; Crabtree, T.D.; Krupnick, A.S.; Kreisel, D.; Broderick, S.R.; Patterson, G.A.; Meyers, B.F. Intraoperative conversion from video-assisted thoracoscopic surgery lobectomy to open thoracotomy: A study of causes and implications. J. Thorac. Cardiovasc. Surg. 2015, 149, 55–61. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hanna, J.M.; Berry, M.F.; D’Amico, T.A. Contraindications of video-assisted thoracoscopic surgical lobectomy and determinants of conversion to open. J. Thorac. Dis. 2013, 5, S182–S189. [Google Scholar]
- Lim, C.G.; Shin, K.M.; Lim, J.S.; Lim, J.K.; Kim, H.J.; Kim, W.H.; Cho, S.H.; Cha, S.I.; Lee, E.B.; Seock, Y.; et al. Predictors of conversion to thoracotomy during video-assisted thoracoscopic surgery lobectomy in lung cancer: Additional predictive value of fdg-pet/ct in a tuberculosis endemic region. J. Thorac. Dis. 2017, 9, 2427–2436. [Google Scholar] [CrossRef]
- Roviaro, G.; Rebuffat, C.; Varoli, F.; Vergani, C.; Mariani, C.; Maciocco, M. Videoendoscopic pulmonary lobectomy for cancer. Surg. Laparosc. Endosc. 1992, 2, 244–247. [Google Scholar]
- Landreneau, R.J.; Hazelrigg, S.R.; Ferson, P.F.; Johnson, J.A.; Nawarawong, W.; Boley, T.M.; Curtis, J.J.; Bowers, C.M.; Herlan, D.B.; Dowling, R.D. Thoracoscopic resection of 85 pulmonary lesions. Ann. Thorac. Surg. 1992, 54, 415–419. [Google Scholar] [CrossRef]
- Jeon, J.H.; Kang, C.H.; Kim, H.S.; Seong, Y.W.; Park, I.K.; Kim, Y.T.; Kim, J.H. Video-assisted thoracoscopic lobectomy in non-small-cell lung cancer patients with chronic obstructive pulmonary disease is associated with lower pulmonary complications than open lobectomy: A propensity score-matched analysis. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2014, 45, 640–645. [Google Scholar] [CrossRef]
- Desai, H.; Natt, B.; Kim, S.; Bime, C. Decreased in-hospital mortality after lobectomy using video-assisted thoracoscopic surgery compared with open thoracotomy. Ann. Am. Thorac. Soc. 2017, 14, 262–266. [Google Scholar] [CrossRef]
- Seok, Y.; Jheon, S.; Cho, S. Serial changes in pulmonary function after video-assisted thoracic surgery lobectomy in lung cancer patients. Thorac. Cardiovasc. Surg. 2014, 62, 133–139. [Google Scholar] [CrossRef]
- Nagahiro, I.; Andou, A.; Aoe, M.; Sano, Y.; Date, H.; Shimizu, N. Pulmonary function, postoperative pain, and serum cytokine level after lobectomy: A comparison of vats and conventional procedure. Ann. Thorac. Surg. 2001, 72, 362–365. [Google Scholar] [CrossRef]
- Solaini, L.; Prusciano, F.; Bagioni, P.; di Francesco, F.; Solaini, L.; Poddie, D.B. Video-assisted thoracic surgery (vats) of the lung: Analysis of intraoperative and postoperative complications over 15 years and review of the literature. Surg. Endosc. 2008, 22, 298–310. [Google Scholar] [CrossRef] [PubMed]
- Yamashita, S.; Tokuishi, K.; Moroga, T.; Abe, S.; Yamamoto, K.; Miyahara, S.; Yoshida, Y.; Yanagisawa, J.; Hamatake, D.; Hiratsuka, M.; et al. Totally thoracoscopic surgery and troubleshooting for bleeding in non-small cell lung cancer. Ann. Thorac. Surg. 2013, 95, 994–999. [Google Scholar] [CrossRef] [PubMed]
- Yan, T.D.; Cao, C.; D’Amico, T.A.; Demmy, T.L.; He, J.; Hansen, H.; Swanson, S.J.; Walker, W.S. Video-assisted thoracoscopic surgery lobectomy at 20 years: A consensus statement. Eur. J. Cardio-Thorac. Surg. Off. J. Eur. Assoc. Cardio-Thorac. Surg. 2014, 45, 633–639. [Google Scholar] [CrossRef]
- Thomas, P.A.; Berbis, J.; Baste, J.M.; Le Pimpec-Barthes, F.; Tronc, F.; Falcoz, P.E.; Dahan, M.; Loundou, A. Pneumonectomy for lung cancer: Contemporary national early morbidity and mortality outcomes. J. Thorac. Cardiovasc. Surg. 2015, 149, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Shapiro, M.; Swanson, S.J.; Wright, C.D.; Chin, C.; Sheng, S.; Wisnivesky, J.; Weiser, T.S. Predictors of major morbidity and mortality after pneumonectomy utilizing the society for thoracic surgeons general thoracic surgery database. Ann. Thorac. Surg. 2010, 90, 927–934. [Google Scholar] [CrossRef] [PubMed]
- Aydogdu, K.; Incekara, F.; Sahin, M.F.; Gulhan, S.S.; Findik, G.; Tastepe, I.; Kaya, S. Surgical management of pulmonary aspergilloma: Clinical experience with 77 cases. Turk. J. Med. Sci. 2015, 45, 431–437. [Google Scholar] [CrossRef]
- Chen, Q.K.; Jiang, G.N.; Ding, J.A. Surgical treatment for pulmonary aspergilloma: A 35-year experience in the chinese population. Interact. Cardiovasc. Thorac. Surg. 2012, 15, 77–80. [Google Scholar] [CrossRef] [PubMed]
- Lejay, A.; Falcoz, P.E.; Santelmo, N.; Helms, O.; Kochetkova, E.; Jeung, M.; Kessler, R.; Massard, G. Surgery for aspergilloma: Time trend towards improved results? Interact. Cardiovasc. Thorac. Surg. 2011, 13, 392–395. [Google Scholar] [CrossRef] [PubMed]
| Variables | Univariable | Multivariable | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p-Value | OR | 95% CI | p-Value | |
| Type of Surgery | ||||||
| Lobectomy | Ref | Ref | ||||
| Pneumonectomy | 3.290 | 1.616–6.701 | 0.001 | 1.271 | 0.475–3.398 | 0.633 |
| Duration of Anesthesia | 1.008 | 1.004–1.012 | <0.001 | 1.004 | 0.997–1.010 | 0.280 |
| Intraoperative Blood Loss | 1.002 | 1.001–1.003 | <0.001 | 1.001 | 1.000–1.002 | 0.040 |
| ppoFEV1 | 0.964 | 0.946–0.982 | <0.001 | |||
| ppoDLCO | 0.964 | 0.947–0.981 | <0.001 | 0.969 | 0.949–0.989 | 0.003 |
| Pleural Adhesion | ||||||
| No Adhesion | Ref | |||||
| Mild | 4.400 | 1.720–11.253 | 0.002 | |||
| Severe | 12.158 | 4.596–32.161 | <0.001 | |||
| Surgical Approach | ||||||
| Videoscope | Ref | Ref | ||||
| Open Thoracotomy | 4.154 | 2.065–8.358 | <0.001 | 2.794 | 1.105–7.066 | 0.030 |
| Conversion to Open Thoracotomy | 4.696 | 1.827–12.069 | 0.001 | 3.388 | 1.037–11.066 | 0.043 |
| Major Vessel Injury | ||||||
| No | Ref | |||||
| Yes | 11.590 | 3.701–36.300 | <0.001 | |||
| Total (n = 319) | No Need for ICU Admission Group (n = 269) | Mandatory ICU Admission Group (n = 50) | p-Value | |
|---|---|---|---|---|
| Age (years) | 67.00 (61.00, 74.00) | 68.00 (62.00, 74.00) | 64.50 (60.00, 72.50) | 0.076 |
| Surgical plan | 0.006 | |||
| Lobectomy | 280 (87.8%) | 242 (89.96%) | 38 (76.0%) | |
| Pneumonectomy | 39 (12.2%) | 27 (10.04%) | 12 (24.0%) | |
| Intraoperative Surgical Plan Change | 28 (8.78%) | 21 (7.8%) | 7 (14.0%) | 0.173 |
| Type of Surgery | 0.001 | |||
| Lobectomy | 273 (85.6%) | 238 (88.5%) | 35 (70.0%) | |
| Pneumonectomy | 46 (14.4%) | 31 (11.5%) | 15 (30.0%) | |
| ASA Classification | 3.00 (2.00, 3.00) | 3.00 (2.00, 3.00) | 3.00 (3.00, 3.00) | 0.098 |
| Charlson Score | 5.00 (4.00, 6.00) | 5.00 (4.00, 6.00) | 5.00 (4.00, 6.00) | 0.758 |
| Cardiac Comorbidity | 50 (15.72%) | 39 (14.5%) | 11 (22.45%) | 0.160 |
| Duration of Anesthesia (min) | 225.00 (190.00, 265.00) | 220.00 (185.00, 255.00) | 270.00 (212.50, 356.75) | 0.001 |
| Total Remifentanil Dose (µg/hour/kg) | 4.90 ± 3.23 | 4.97 ± 3.44 | 4.46 ± 1.51 | 0.399 |
| Intraoperative Blood Loss (mL) | 100.00 (50.00, 300.00) | 100.00 (50.00, 250.00) | 400.00 (250.00, 775.00) | <0.001 |
| Emergency | 2 (0.63%) | 1 (0.37%) | 1 (2.0%) | 0.289 |
| ppoFEV1 (%) | 67.39 ± 19.49 | 69.24 ± 18.76 | 56.34 ± 20.29 | <0.001 |
| ppoDLCO (%) | 65.59 (52.58, 77.80) | 67.82 (57.12, 79.70) | 47.16 (43.32, 65.68) | <0.001 |
| Diagnosis | 0.014 | |||
| Lung cancer | 293 (91.9%) | 252 (93.7%) | 41 (82.0%) | |
| Metastatic | 7 (2.2%) | 4 (1.5%) | 3 (6.0%) | |
| Benign Disease | 19 (6.0%) | 13 (4.8%) | 6 (12.0%) | |
| Preoperative Hemoglobin (g/dL) | 12.10 (10.90, 13.00) | 12.10 (11.10, 13.10) | 11.10 (10.40, 12.28) | 0.002 |
| Postoperative Hemoglobin (g/dL) | 12.50 (10.90, 13.30) | 12.80 (11.85, 13.70) | 11.60 (10.62, 12.85) | 0.006 |
| Postoperative PaO2/FiO2 (mmHg) | 306.50 (224.00, 411.50) | 264.38 (205.19, 384.88) | 354.50 (274.31, 432.63) | 0.009 |
| Postoperative Lactate (mmol/L) | 1.87 ± 0.96 | 1.54 ± 0.76 | 2.09 ± 1.02 | 0.0635 |
| SOFA score | 2.00 (1.00, 2.00) | 2.00 (1.00, 2.00) | 1.00 (1.00, 2.00) | 0.221 |
| Epidural PCA | 153 (48.0%) | 126 (46.8%) | 27 (54.0%) | 0.352 |
| Pleural Adhesion | ||||
| No Mild Severe | 132 (41.4%) 127 (39.8%) 60 (18.8%) | 126 (46.8%) 105 (39.0%) 38 (14.1%) | 6 (12.0%) 22 (44.0%) 22 (44.0%) | <0.001 |
| Open surgery Videoscope Open Surgery Conversion to Open Surgery | 182 (57.1%) 105 (32.9%) 32 (10.0%) | 168 (62.5%) 78 (29.0%) 23 (8.6%) | 14 (28.0%) 27 (54.0%) 9 (18.0%) | <0.001 |
| Major Vessel Injury | 14 (4.4%) | 5 (1.9%) | 9 (18.0%) | <0.001 |
| Total (n = 319) | No Need for ICU Group (n = 269) | Mandatory ICU Admission Group (n = 50) | p-Value |
|---|---|---|---|
| Arrhythmia | 13 (4.8 %) | 8 (16.0%) | 0.008 |
| Atrial Fibrillation | 12 (4.5%) | 5 (10.0%) | 0.159 |
| Air Leak > 5 Days | 30 (11.2%) | 7 (14.0%) | 0.630 |
| Pneumothorax | 3 (1.1%) | 3 (6.0%) | 0.051 |
| Bleeding Requiring Reoperation | 1 (0.4%) | 1 (2.0%) | 0.289 |
| Pneumonia | 34 (12.6%) | 18 (36.0%) | < 0.001 |
| Myocardial Infarct | 1 (0.4%) | 0 (0.0%) | > 0.999 |
| Bronchopleural Fistula | 4 (1.5%) | 3 (6.0%) | 0.080 |
| ARDS | 7 (2.6%) | 13 (26.0%) | < 0.001 |
| Ventricular Arrhythmia | 0 (0.0%) | 3 (6.0%) | 0.004 |
| Ventilatory Support | 5 (1.9%) | 14 (28.0%) | < 0.001 |
| Pulmonary Edema | 10 (3.7%) | 12 (24.0%) | < 0.001 |
| Heart Failure | 0 (0.0%) | 2 (4.0%) | 0.024 |
| Renal Failure Requiring Hemodialysis | 1 (0.4%) | 1 (2.0%) | 0.289 |
| CVA or TIA | 2 (0.7%) | 3 (6.0%) | 0.029 |
| Charlson Comorbidity Score | 4.81 ± 2.44 | 4.92 ± 2.75 | 0.800 |
| Charlson Comorbidity Score Change | 0.0 (−2.0–2.0) | 0.0 (−2.0–1.25) | 0.164 |
| Hospital Stay After Surgery | 7.0 (5.0–9.0) | 12.5 (8.75–23.00) | <0.001 |
| 1 Year Mortality | 7 (2.6%) | 7 (14.0%) | 0.002 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kim, S.H.; Na, S.; Park, S.Y.; Lee, J.; Kang, Y.-S.; Jung, H.-h.; Kim, J. Perioperative Factors for Predicting the Need for Postoperative Intensive Care after Major Lung Resection. J. Clin. Med. 2019, 8, 744. https://doi.org/10.3390/jcm8050744
Kim SH, Na S, Park SY, Lee J, Kang Y-S, Jung H-h, Kim J. Perioperative Factors for Predicting the Need for Postoperative Intensive Care after Major Lung Resection. Journal of Clinical Medicine. 2019; 8(5):744. https://doi.org/10.3390/jcm8050744
Chicago/Turabian StyleKim, Seung Hyun, Sungwon Na, Seong Yong Park, Jinae Lee, Yhen-Seung Kang, Hwan-ho Jung, and Jeongmin Kim. 2019. "Perioperative Factors for Predicting the Need for Postoperative Intensive Care after Major Lung Resection" Journal of Clinical Medicine 8, no. 5: 744. https://doi.org/10.3390/jcm8050744
APA StyleKim, S. H., Na, S., Park, S. Y., Lee, J., Kang, Y.-S., Jung, H.-h., & Kim, J. (2019). Perioperative Factors for Predicting the Need for Postoperative Intensive Care after Major Lung Resection. Journal of Clinical Medicine, 8(5), 744. https://doi.org/10.3390/jcm8050744





