Treatment Outcomes of Novel Targeted Agents in Relapse/Refractory Chronic Lymphocytic Leukemia: A Systematic Review and Network Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
2.2. Inclusion Criteria
2.3. Exclusion Criteria
2.4. Risk of Bias Assessment
2.5. Data Extraction
2.6. Data Synthesis and Statistical Analysis
3. Results
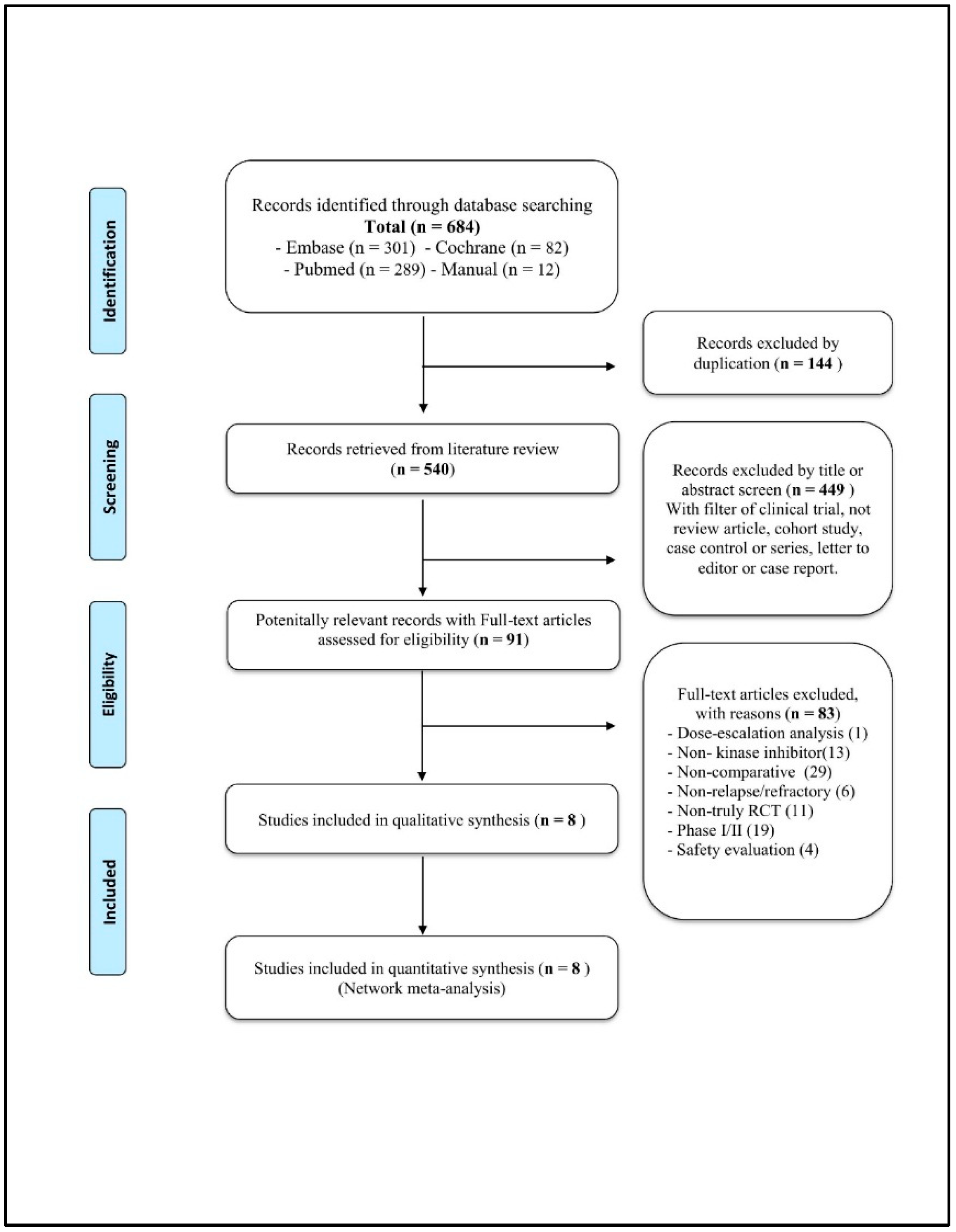
3.1. Systematic Literature Review
3.2. Data Extraction
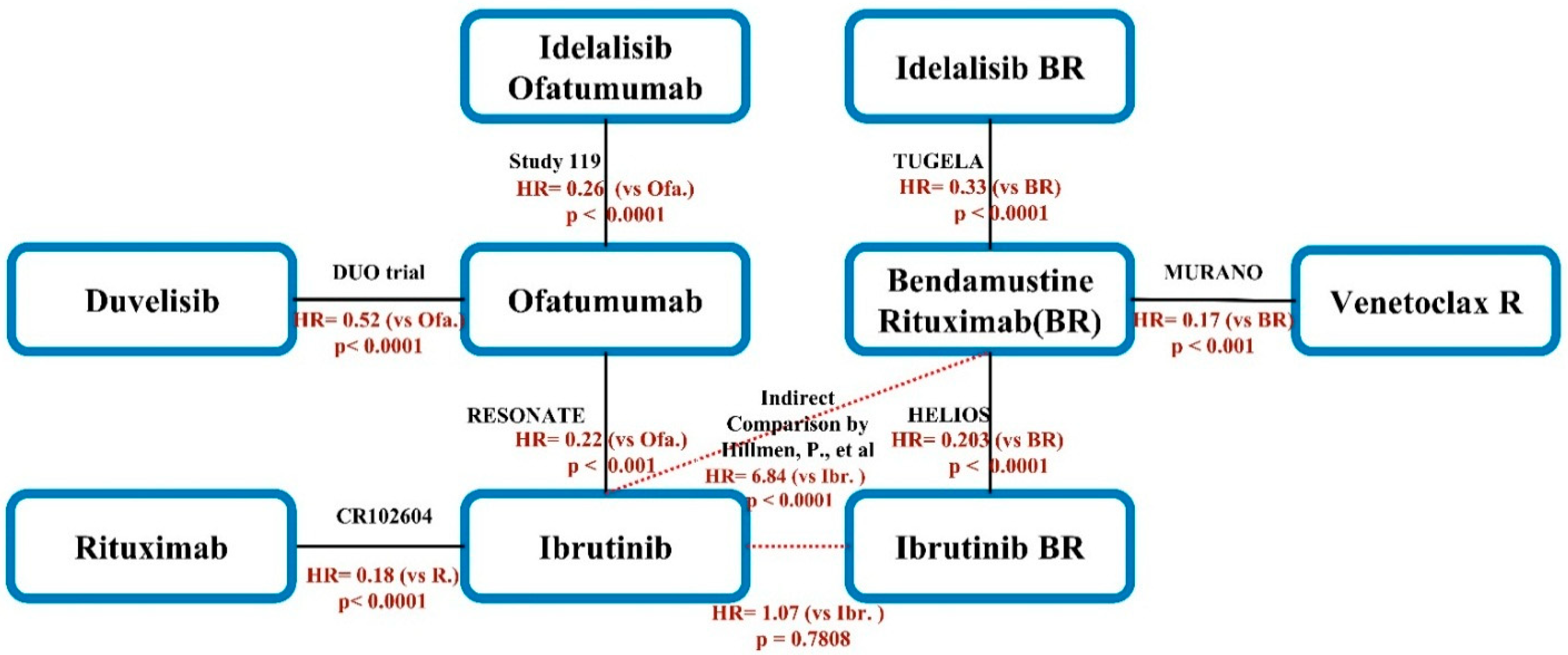
3.3. Network Meta-Analysis
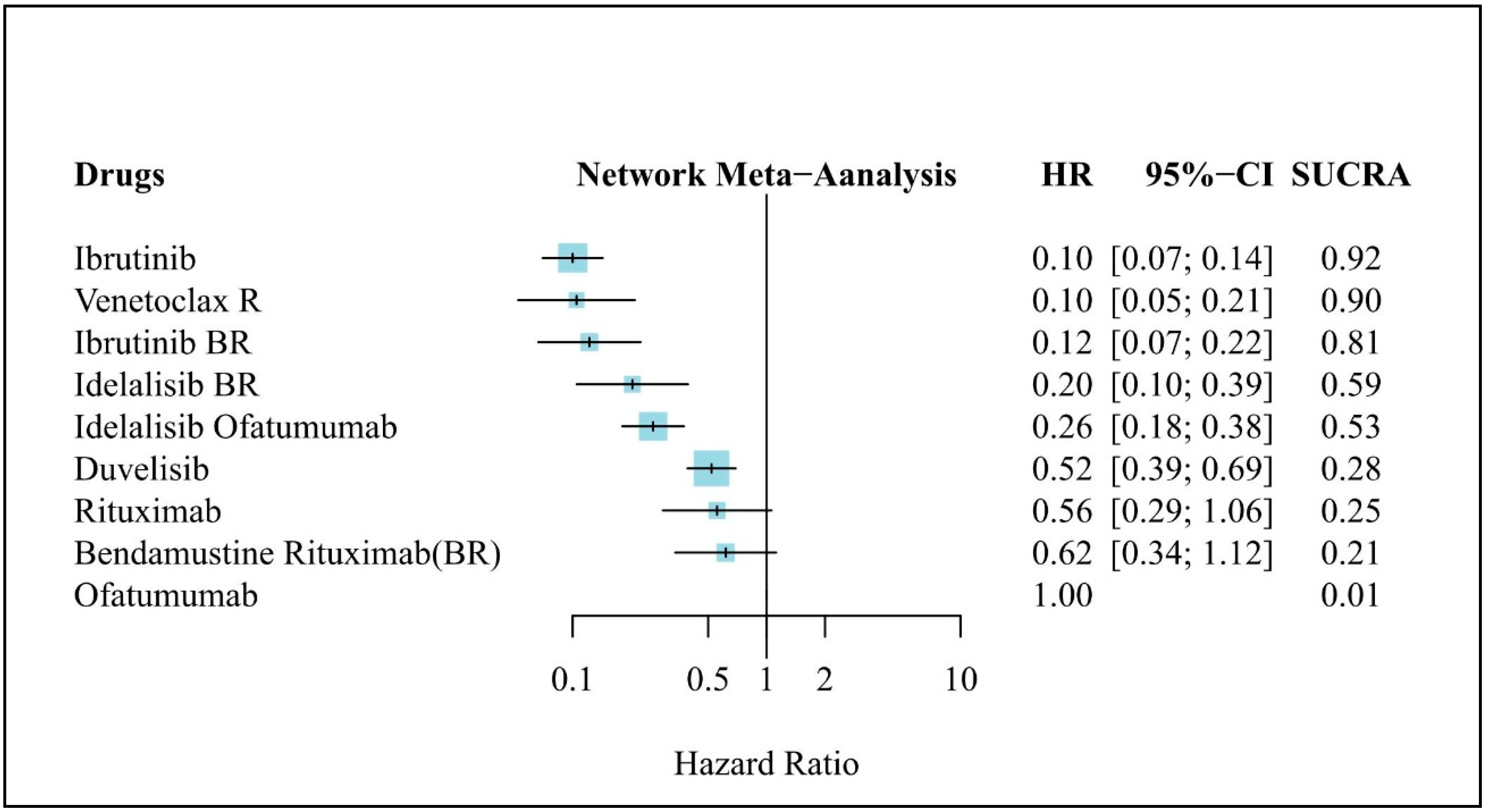
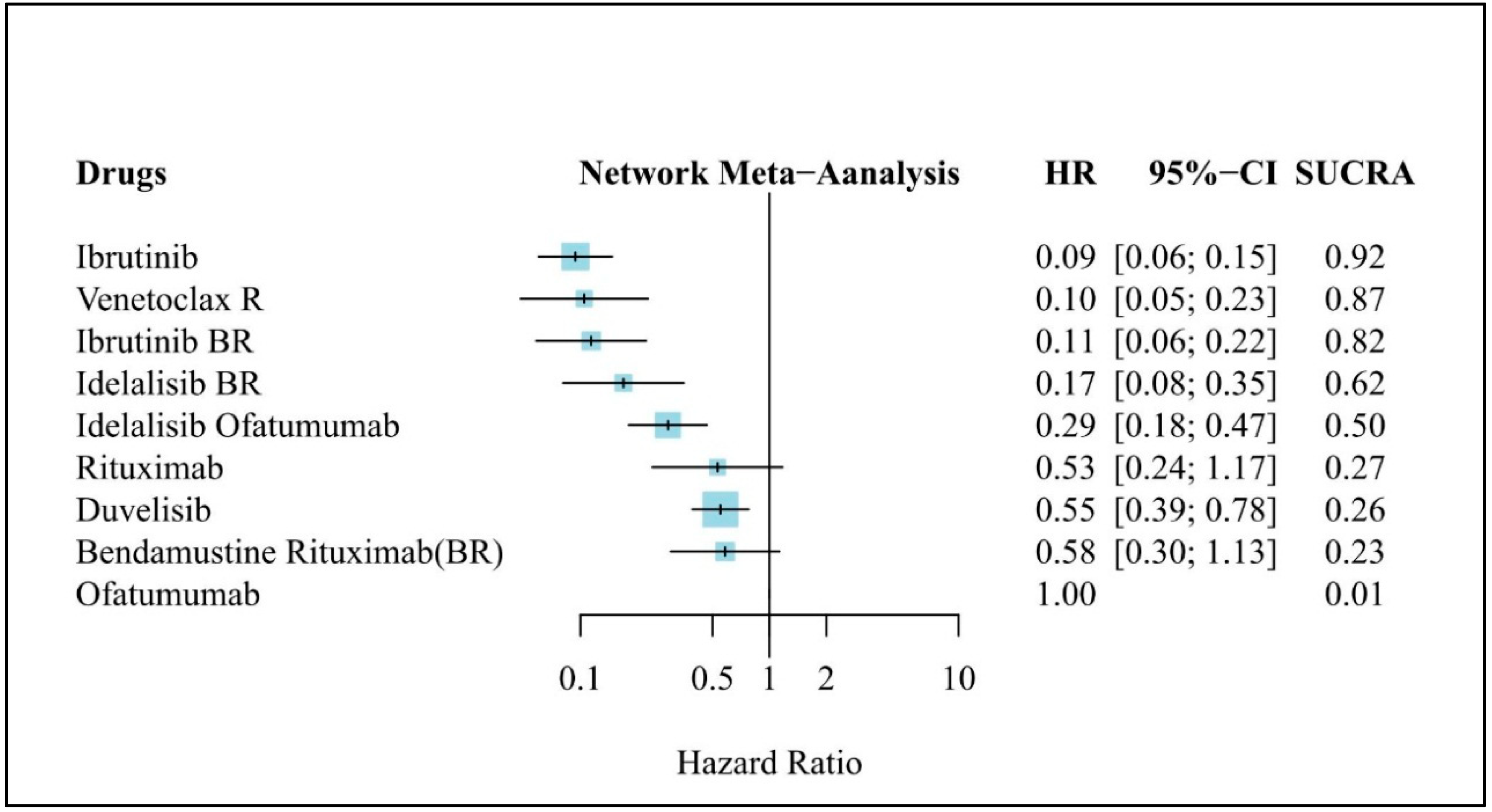
3.4. Clinical Efficacy (PFS)
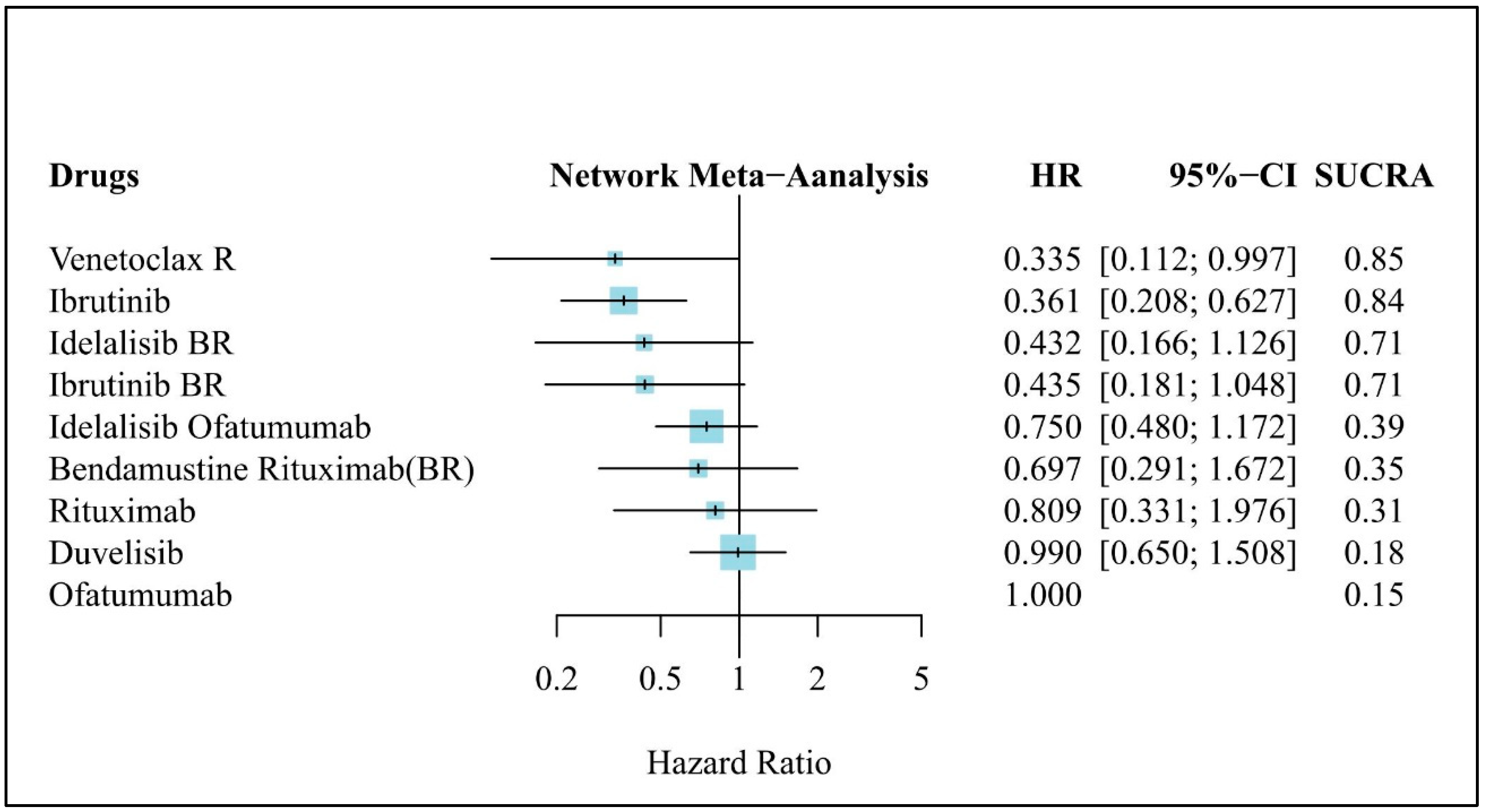
3.5. Clinical Efficacy (OS)
3.6. Clinical Efficacy (PFS in Patients without del(17p))
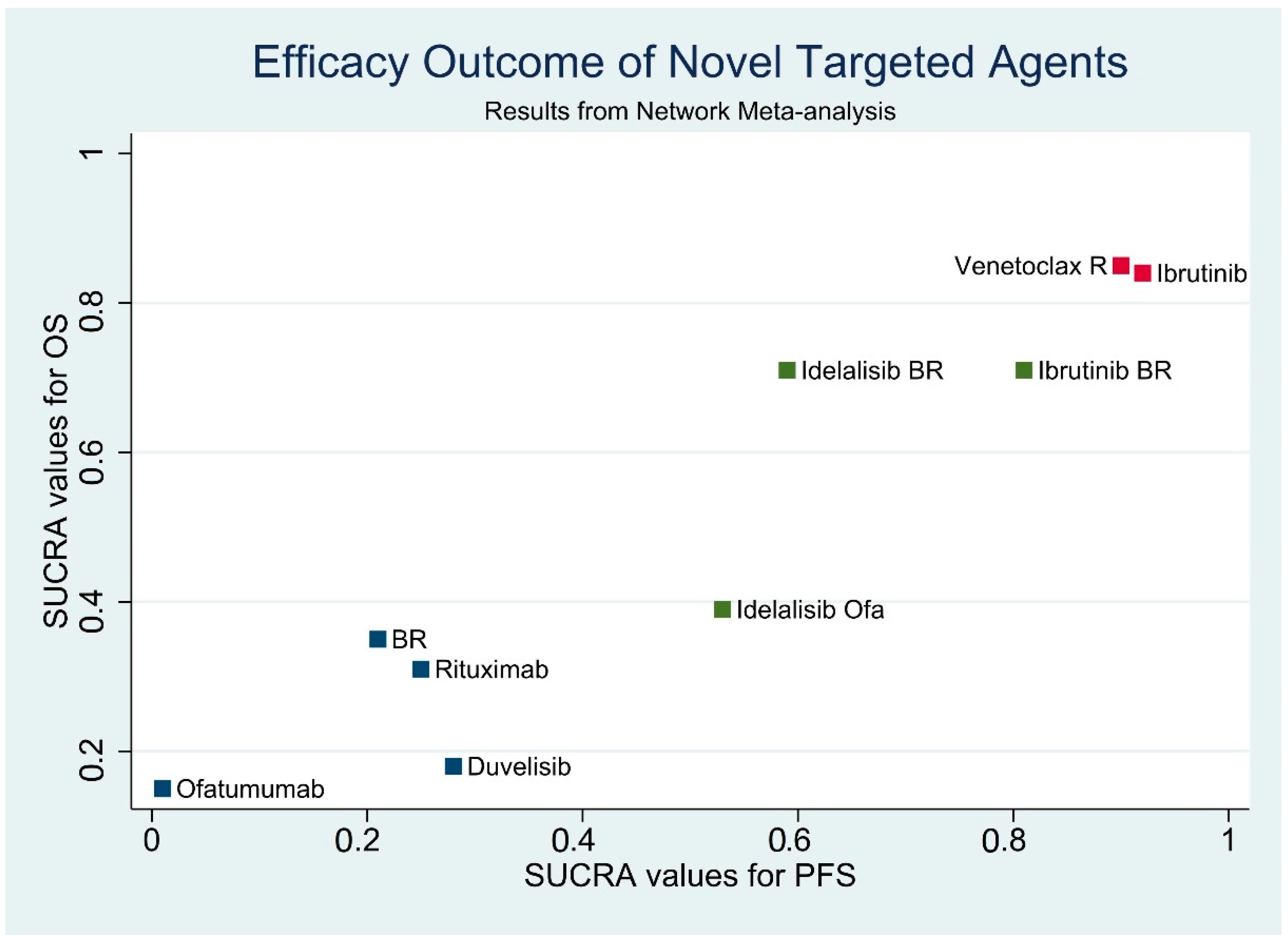
3.7. Results of Efficacy Outcome Synthesis
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Eichhorst, B.; Robak, T.; Montserrat, E.; Ghia, P.; Hillmen, P.; Hallek, M.; Buske, C. Chronic Lymphocytic Leukaemia: Esmo Clinical Practice Guidelines for Diagnosis, Treatment and Follow-Up. Ann. Oncol. 2015, 26 (Suppl. 5), v78–v84. [Google Scholar] [CrossRef]
- Stilgenbauer, S.; Schnaiter, A.; Paschka, P.; Zenz, T.; Rossi, M.; Dohner, K.; Buhler, A.; Bottcher, S.; Ritgen, M.; Kneba, M.; et al. Gene Mutations and Treatment Outcome in Chronic Lymphocytic Leukemia: Results from the Cll8 Trial. Blood 2014, 123, 3247–3254. [Google Scholar] [CrossRef]
- Goede, V.; Fischer, K.; Bosch, F.; Follows, G.; Frederiksen, H.; Cuneo, A.; Ludwig, H.; Crompton, N.; Maurer, J.; Uguen, M.; et al. Updated Survival Analysis from the Cll11 Study: Obinutuzumab Versus Rituximab in Chemoimmunotherapy-Treated Patients with Chronic Lymphocytic Leukemia. Blood 2015, 126, 1733. [Google Scholar]
- Brown, J.R.; Hillmen, P.; O’Brien, S.; Barrientos, J.C.; Reddy, N.M.; Coutre, S.E.; Tam, C.S.; Mulligan, S.P.; Jaeger, U.; Barr, P.M.; et al. Extended Follow-up and Impact of High-Risk Prognostic Factors from the Phase 3 Resonate Study in Patients with Previously Treated Cll/Sll. Leukemia 2018, 32, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Byrd, J.C.; Brown, J.R.; O’Brien, S.; Barrientos, J.C.; Kay, N.E.; Reddy, N.M.; Coutre, S.; Tam, C.S.; Mulligan, S.P.; Jaeger, U.; et al. Ibrutinib Versus Ofatumumab in Previously Treated Chronic Lymphoid Leukemia. N. Engl. J. Med. 2014, 371, 213–223. [Google Scholar] [CrossRef]
- Chanan-Khan, A.; Cramer, P.; Demirkan, F.; Fraser, G.; Silva, R.S.; Grosicki, S.; Pristupa, A.; Janssens, A.; Mayer, J.; Bartlett, N.L.; et al. Ibrutinib Combined with Bendamustine and Rituximab Compared with Placebo, Bendamustine, and Rituximab for Previously Treated Chronic Lymphocytic Leukaemia or Small Lymphocytic Lymphoma (Helios): A Randomised, Double-Blind, Phase 3 Study. Lancet Oncol. 2016, 17, 200–211. [Google Scholar] [CrossRef]
- Flinn, I.W.; Hillmen, P.; Montillo, M.; Nagy, Z.; Illes, A.; Etienne, G.; Delgado, J.; Kuss, B.J.; Tam, C.S.; Gasztonyi, Z.; et al. The Phase 3 Duo Trial: Duvelisib Vs Ofatumumab in Relapsed and Refractory Cll/Sll. Blood 2018, 132, 2446–2455. [Google Scholar] [CrossRef] [PubMed]
- Huang, X.; Qiu, L.; Jin, J.; Zhou, D.; Chen, X.; Hou, M.; Hu, J.; Hu, Y.; Ke, X.; Li, J.; et al. Ibrutinib Versus Rituximab in Relapsed or Refractory Chronic Lymphocytic Leukemia or Small Lymphocytic Lymphoma: A Randomized, Open-Label Phase 3 Study. Cancer Med. 2018, 7, 1043–1055. [Google Scholar] [CrossRef] [PubMed]
- Jones, J.A.; Robak, T.; Brown, J.R.; Awan, F.T.; Badoux, X.; Coutre, S.; Loscertales, J.; Taylor, K.; Vandenberghe, E.; Wach, M.; et al. Efficacy and Safety of Idelalisib in Combination with Ofatumumab for Previously Treated Chronic Lymphocytic Leukaemia: An Open-Label, Randomised Phase 3 Trial. Lancet Haematol. 2017, 4, e114–e126. [Google Scholar] [CrossRef]
- Seymour, J.F.; Kipps, T.J.; Eichhorst, B.; Hillmen, P.; D’Rozario, J.; Assouline, S.; Owen, C.; Gerecitano, J.; Robak, T.; de la Serna, J.; et al. Venetoclax–Rituximab in Relapsed or Refractory Chronic Lymphocytic Leukemia. N. Engl. J. Med. 2018, 378, 1107–1120. [Google Scholar] [CrossRef]
- Zelenetz, A.D.; Barrientos, J.C.; Brown, J.R.; Coiffier, B.; Delgado, J.; Egyed, M.; Ghia, P.; Illes, A.; Jurczak, W.; Marlton, P.; et al. Idelalisib or Placebo in Combination with Bendamustine and Rituximab in Patients with Relapsed or Refractory Chronic Lymphocytic Leukaemia: Interim Results from a Phase 3, Randomised, Double-Blind, Placebo-Controlled Trial. Lancet Oncol. 2017, 18, 297–311. [Google Scholar] [CrossRef]
- Ponader, S.; Chen, S.S.; Buggy, J.J.; Balakrishnan, K.; Gandhi, V.; Wierda, W.G.; Keating, M.J.; O’Brien, S.; Chiorazzi, N.; Burger, J.A. The Bruton Tyrosine Kinase Inhibitor Pci-32765 Thwarts Chronic Lymphocytic Leukemia Cell Survival and Tissue Homing in Vitro and in Vivo. Blood 2012, 119, 1182–1189. [Google Scholar] [CrossRef]
- Souers, A.J.; Leverson, J.D.; Boghaert, E.R.; Ackler, S.L.; Catron, N.D.; Chen, J.; Dayton, B.D.; Ding, H.; Enschede, S.H.; Fairbrother, W.J.; et al. Abt-199, a Potent and Selective Bcl-2 Inhibitor, Achieves Antitumor Activity While Sparing Platelets. Nat. Med. 2013, 19, 202–208. [Google Scholar] [CrossRef]
- Yang, Q.; Modi, P.; Newcomb, T.; Queva, C.; Gandhi, V. Idelalisib: First-in-Class Pi3k Delta Inhibitor for the Treatment of Chronic Lymphocytic Leukemia, Small Lymphocytic Leukemia, and Follicular Lymphoma. Clin. Cancer Res. 2015, 21, 1537–1542. [Google Scholar] [CrossRef]
- Winkler, D.G.; Faia, K.L.; DiNitto, J.P.; Ali, J.A.; White, K.F.; Brophy, E.E.; Pink, M.M.; Proctor, J.L.; Lussier, J.; Martin, C.M.; et al. Pi3k-Delta and Pi3k-Gamma Inhibition by Ipi-145 Abrogates Immune Responses and Suppresses Activity in Autoimmune and Inflammatory Disease Models. Chem. Biol. 2013, 20, 1364–1374. [Google Scholar] [CrossRef]
- Hutton, B.; Salanti, G.; Caldwell, D.M.; Chaimani, A.; Schmid, C.H.; Cameron, C.; Ioannidis, J.P.; Straus, S.; Thorlund, K.; Jansen, J.P.; et al. The Prisma Extension Statement for Reporting of Systematic Reviews Incorporating Network Meta-Analyses of Health Care Interventions: Checklist and Explanations. Ann. Intern. Med. 2015, 162, 777–784. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; Prisma-P Group. Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (Prisma-P) 2015: Elaboration and Explanation. BMJ 2015, 349, g7647. [Google Scholar] [CrossRef] [PubMed]
- Hallek, M.; Cheson, B.D.; Catovsky, D.; Caligaris-Cappio, F.; Dighiero, G.; Dohner, H.; Hillmen, P.; Keating, M.J.; Montserrat, E.; Rai, K.R.; et al. Guidelines for the Diagnosis and Treatment of Chronic Lymphocytic Leukemia: A Report from the International Workshop on Chronic Lymphocytic Leukemia Updating the National Cancer Institute-Working Group 1996 Guidelines. Blood 2008, 111, 5446–5456. [Google Scholar] [CrossRef]
- Higgins, J.P.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. The Cochrane Collaboration. Available online: http://handbook.cochrane.org/ (accessed on 15 March 2019).
- Roberts, C.; Torgerson, D.J. Understanding Controlled Trials: Baseline Imbalance in Randomised Controlled Trials. BMJ 1999, 319, 185. [Google Scholar] [CrossRef] [PubMed]
- Review Manager (Revman) [Computer Program]. Version 5.3; The Nordic Cochrane Centre, The Cochrane Collaboration: Copenhagen, Denmark, 2014.
- Salanti, G. Indirect and Mixed-Treatment Comparison, Network, or Multiple-Treatments Meta-Analysis: Many Names, Many Benefits, Many Concerns for the Next Generation Evidence Synthesis Tool. Res. Synth. Methods 2012, 3, 80–97. [Google Scholar] [CrossRef]
- Rucker, G.; Schwarzer, G.; Krahn, U.; König, J. Netmeta: Network Meta-Analysis Using Frequentist Methods. R Package Version 0.7-0. Available online: http://cran.at.r-project.org/web/packages/netmeta/ (accessed on 15 December 2018).
- Wierda, W.G.; Kipps, T.J.; Mayer, J.; Stilgenbauer, S.; Williams, C.D.; Hellmann, A.; Robak, T.; Furman, R.R.; Hillmen, P.; Trneny, M.; et al. Ofatumumab as Single-Agent Cd20 Immunotherapy in Fludarabine-Refractory Chronic Lymphocytic Leukemia. J. Clin. Oncol. 2010, 28, 1749–1755. [Google Scholar] [CrossRef] [PubMed]
- Hillmen, P.; Fraser, G.; Jones, J.; Rule, S.; Brien, S.; Dilhuydy, M.S.; Jaeger, U.; Grosicki, S.; Cymbalista, F.; Sun, S.; et al. Comparing Single-Agent Ibrutinib, Bendamustine Plus Rituximab (Br) and Ibrutinib Plus Br in Patients with Previously Treated Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma (Cll/Sll): An Indirect Comparison of the Resonate and Helios Trials. Blood 2015, 126, 2944. [Google Scholar]
- Efthimiou, O.; Mavridis, D.; Debray, T.P.; Samara, M.; Belger, M.; Siontis, G.C.; Leucht, S.; Salanti, G. Combining Randomized and Non-Randomized Evidence in Network Meta-Analysis. Stat. Med. 2017, 36, 1210–1226. [Google Scholar] [CrossRef] [PubMed]
- Leyva, F.; Plummer, C.J. National Institute for Health and Care Excellence 2014 Guidance on Cardiac Implantable Electronic Devices: Health Economics Reloaded. Europace 2015, 17, 339–342. [Google Scholar] [CrossRef][Green Version]
- Krahn, U.; Binder, H.; Konig, J. A Graphical Tool for Locating Inconsistency in Network Meta-Analyses. BMC Med. Res. Methodol. 2013, 13, 35. [Google Scholar] [CrossRef] [PubMed]
- Jackson, D.; White, I.R.; Riley, R.D. Quantifying the Impact of between-Study Heterogeneity in Multivariate Meta-Analyses. Stat. Med. 2012, 31, 3805–3820. [Google Scholar] [CrossRef] [PubMed]
- Chaimani, A.; Higgins, J.P.; Mavridis, D.; Spyridonos, P.; Salanti, G. Graphical Tools for Network Meta-Analysis in Stata. PLoS ONE 2013, 8, e76654. [Google Scholar] [CrossRef] [PubMed]
- Jansen, J.P.; Trikalinos, T.; Cappelleri, J.C.; Daw, J.; Andes, S.; Eldessouki, R.; Salanti, G. Indirect Treatment Comparison/Network Meta-Analysis Study Questionnaire to Assess Relevance and Credibility to Inform Health Care Decision Making: An Ispor-Amcp-Npc Good Practice Task Force Report. Value Health 2014, 17, 157–173. [Google Scholar] [CrossRef] [PubMed]
- Salanti, G.; del Giovane, C.; Chaimani, A.; Caldwell, D.M.; Higgins, J.P. Evaluating the Quality of Evidence from a Network Meta-Analysis. PLoS ONE 2014, 9, e99682. [Google Scholar] [CrossRef] [PubMed]
- Sorensen, S.; Wildgust, M.; Sengupta, N.; Trambitas, C.; Diels, J.; van Sanden, S.; Xu, Y.; Dorman, E. Indirect Treatment Comparisons of Ibrutinib Versus Physician’s Choice and Idelalisib Plus Ofatumumab in Patients with Previously Treated Chronic Lymphocytic Leukemia. Clin. Ther. 2017, 39, 178–189.e5. [Google Scholar] [CrossRef]
- National Comprehensive Cancer Network. Chronic Lymphocytic Leukemia/Small Lymphocytic Lymphoma (Version 2.2019). Available online: https://www.nccn.org/professionals/physician_gls/pdf/cll.pdf (accessed on 5 February 2019).
- Burger, J.A.; Sivina, M.; Jain, N.; Kim, E.; Kadia, T.; Estrov, Z.; Nogueras-Gonzalez, G.M.; Huang, X.; Jorgensen, J.; Li, J.; et al. Randomized Trial of Ibrutinib Versus Ibrutinib Plus Rituximab in Patients with Chronic Lymphocytic Leukemia. Blood 2019, 133, 1011–1019. [Google Scholar] [CrossRef]
- Winqvist, M.; Andersson, P.O.; Asklid, A.; Karlsson, K.; Karlsson, C.; Lauri, B.; Lundin, J.; Mattsson, M.; Norin, S.; Sandstedt, A.; et al. Long-Term Real-World Results of Ibrutinib Therapy in Patients with Relapsed or Refractory Chronic Lymphocytic Leukemia: 30-Month Follow-up of the Swedish Compassionate Use Cohort. Haematologica 2018, 104, e208. [Google Scholar] [CrossRef]
- Brien, S.M.; Furman, R.R.; Coutre, S.E.; Flinn, I.W.; Burger, J.; Blum, K.; Sharman, J.; Wierda, W.G.; Jones, J.; Zhao, W.; et al. Five-Year Experience with Single-Agent Ibrutinib in Patients with Previously Untreated and Relapsed/Refractory Chronic Lymphocytic Leukemia/Small Lymphocytic Leukemia. Blood 2016, 128, 233. [Google Scholar]
- Mato, A.R.; Hill, B.T.; Lamanna, N.; Barr, P.M.; Ujjani, C.S.; Brander, D.M.; Howlett, C.; Skarbnik, A.P.; Cheson, B.D.; Zent, C.S.; et al. Optimal Sequencing of Ibrutinib, Idelalisib, and Venetoclax in Chronic Lymphocytic Leukemia: Results from a Multicenter Study of 683 Patients. Ann. Oncol. 2017, 28, 1050–1056. [Google Scholar] [CrossRef] [PubMed]
- Mato, A.R.; Thompson, M.; Allan, J.N.; Brander, D.M.; Pagel, J.M.; Ujjani, C.S.; Hill, B.T.; Lamanna, N.; Lansigan, F.; Jacobs, R.; et al. Real-World Outcomes and Management Strategies for Venetoclax-Treated Chronic Lymphocytic Leukemia Patients in the United States. Haematologica 2018, 103, 1511–1517. [Google Scholar] [CrossRef] [PubMed]
- Roberts, A.W.; Davids, M.S.; Pagel, J.M.; Kahl, B.S.; Puvvada, S.D.; Gerecitano, J.F.; Kipps, T.J.; Anderson, M.A.; Brown, J.R.; Gressick, L.; et al. Targeting Bcl2 with Venetoclax in Relapsed Chronic Lymphocytic Leukemia. N. Engl. J. Med. 2016, 374, 311–322. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Jackson, D.; Barrett, J.K.; Lu, G.; Ades, A.E.; White, I.R. Consistency and Inconsistency in Network Meta-Analysis: Concepts and Models for Multi-Arm Studies. Res. Synth. Methods 2012, 3, 98–110. [Google Scholar] [CrossRef]
- Mato, A.R.; Nabhan, C.; Barr, P.M.; Ujjani, C.S.; Hill, B.T.; Lamanna, N.; Skarbnik, A.P.; Howlett, C.; Pu, J.J.; Sehgal, A.R.; et al. Outcomes of Cll Patients Treated with Sequential Kinase Inhibitor Therapy: A Real World Experience. Blood 2016, 128, 2199. [Google Scholar] [CrossRef] [PubMed]
- Woyach, J.A.; Ruppert, A.S.; Guinn, D.; Lehman, A.; Blachly, J.S.; Lozanski, A.; Heerema, N.A.; Zhao, W.; Coleman, J.; Jones, D.; et al. Btkc481s-Mediated Resistance to Ibrutinib in Chronic Lymphocytic Leukemia. J. Clin. Oncol. 2017, 35, 1437–1443. [Google Scholar] [CrossRef]
- Cheson, B.D.; Enschede, S.H.; Cerri, E.; Desai, M.; Potluri, J.; Lamanna, N.; Tam, C. Tumor Lysis Syndrome in Chronic Lymphocytic Leukemia with Novel Targeted Agents. Oncologist 2017, 22, 1283–1291. [Google Scholar] [CrossRef]
| Trial Name NCT Number | First Author Published Year | Trial Design | Experimental Arm | Control Arm | Mean Age | Rai Stage > III (%) | Number of Prior Therapies | Del(17p) Mutation (%) |
|---|---|---|---|---|---|---|---|---|
| Study 119 (NCT01659021) | Jones, J.A. 2017 | OP, RCT Phase III | Idelalisib Ofatumumab a (Ide: 150 mg bid po) | Ofatumumab b | 67.7 | 63.70% | 3 vs. 3 | 40% vs. 38% |
| DUO trial (NCT02004522) | Flinn, I.W. 2018 | OP, RCT Phase III | Duvelisib (25 mg bid po) | Ofatumumab b | 69 | 56% | 2 vs. 2 | 21% vs. 28% |
| RESONATE (NCT01578707) | Brown, J.R. 2018 | OP, RCT Phase III | Ibrutinib (420 mg qd po) | Ofatumumab b | 66.8 | 57.30% | 3 vs. 2 | 32% vs. 33% |
| CR102604 (NCT01973387) | Huang, X. 2018 | OP, RCT Phase III | Ibrutinib (420 mg qd po) | Rituximab c | 63.6 | 77.70% | 2 vs. 2 | 27.1% vs. 24.1% |
| HELIOS (NCT01611090) | Chanan-Khan, A. 2016 | DB, RCT Phase III | Ibrutinib BR d (Ibr 420 mg qd po) | BR d | 63.5 | 42.50% | 2 vs. 2 | 0% vs. 0% |
| MURANO (NCT02005471) | Seymour, J.F. 2018 | OP, RCT Phase III | Venetoclax R e | BR d | 65.3 | 18% | 2 vs. 2 | 23.7% vs. 23.6% |
| TUGELA (NCT01569295) | Zelenetz, A.D. 2017 | DB, RCT Phase III | Idelalisib BR d (Ide.: 150 mg bid po) | BR d | 63 | 45.50% | 2 vs. 2 | 18% vs. 19% |
| Trial Name/ID Number | Experimental Arm | Control Arm | Patient Numbers | Median Follow-Up | Overall Response Rate | Median PFS | Hazard Ratio (95% CI), PFS | Median OS | Hazard Ratio (95% CI), OS |
|---|---|---|---|---|---|---|---|---|---|
| Study 119 | Idelalisib Ofatumumab | Ofatumumab | 174 vs. 87 | 16.1 vs. 5.8 months | 75.3% vs. 18.4% | 16.4 vs. 8.0 months | 0.26 (0.18 to 0.38) | NR vs NR | 0.750 (0.48 to 1.18) |
| DUO trial | Duvelisib | Ofatumumab | 160 vs. 159 | 22.4 months | 73.8% vs. 45.3% | 13.3 vs. 9.9 months | 0.52 (0.39 to 0.7) | NR vs NR | 0.99 (0.65 to 1.5) |
| RESONATE | Ibrutinib | Ofatumumab | 195 vs. 196 | 19 months | 90% vs. 25% | NR vs. 8.1 months | 0.10 (0.07 to 0.15) | NR vs NR | 0.361 (0.208 to 0.628) |
| CR102604 | Ibrutinib | Rituximab | 106 vs. 54 | 17.8 months | 67.9% vs. 7.4% | NR vs. 8.3 months | 0.18 (0.105 to 0.308) | NR vs 26.1 months | 0.446 (0.221 to 0.9) |
| HELIOS | Ibrutinib BR | BR | 289 vs. 289 | 17 months | 86% vs. 69% | NR vs. 13.3 months | 0.203 (0.15 to 0.276) | NR vs NR | 0.628 (0.385 to 1.024) |
| MURANO | Venetoclax R | BR | 194 vs. 195 | 23.8 months | 93.3% vs. 67.7% | NR vs. 17 months | 0.17 (0.12 to 0.26) | NR vs NR | 0.48 (0.25 to 0.9) |
| TUGELA | Idelalisib BR | BR | 207 vs. 209 | 14 months | 70% vs. 45% | 20.8 vs. 11.1 months | 0.33 (0.25 to 0.44) | NR vs 31.6 months | 0.62 (0.42 to 0.92) |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chen, P.-H.; Ho, C.-L.; Lin, C.; Wu, Y.-Y.; Huang, T.-C.; Tu, Y.-K.; Lee, C.-H. Treatment Outcomes of Novel Targeted Agents in Relapse/Refractory Chronic Lymphocytic Leukemia: A Systematic Review and Network Meta-Analysis. J. Clin. Med. 2019, 8, 737. https://doi.org/10.3390/jcm8050737
Chen P-H, Ho C-L, Lin C, Wu Y-Y, Huang T-C, Tu Y-K, Lee C-H. Treatment Outcomes of Novel Targeted Agents in Relapse/Refractory Chronic Lymphocytic Leukemia: A Systematic Review and Network Meta-Analysis. Journal of Clinical Medicine. 2019; 8(5):737. https://doi.org/10.3390/jcm8050737
Chicago/Turabian StyleChen, Po-Huang, Ching-Liang Ho, Chin Lin, Yi-Ying Wu, Tzu-Chuan Huang, Yu-Kang Tu, and Cho-Hao Lee. 2019. "Treatment Outcomes of Novel Targeted Agents in Relapse/Refractory Chronic Lymphocytic Leukemia: A Systematic Review and Network Meta-Analysis" Journal of Clinical Medicine 8, no. 5: 737. https://doi.org/10.3390/jcm8050737
APA StyleChen, P.-H., Ho, C.-L., Lin, C., Wu, Y.-Y., Huang, T.-C., Tu, Y.-K., & Lee, C.-H. (2019). Treatment Outcomes of Novel Targeted Agents in Relapse/Refractory Chronic Lymphocytic Leukemia: A Systematic Review and Network Meta-Analysis. Journal of Clinical Medicine, 8(5), 737. https://doi.org/10.3390/jcm8050737








