Clinical and Gait Parameters Related to Pelvic Retraction in Patients with Spastic Hemiplegia
Abstract
1. Introduction
2. Experimental Section
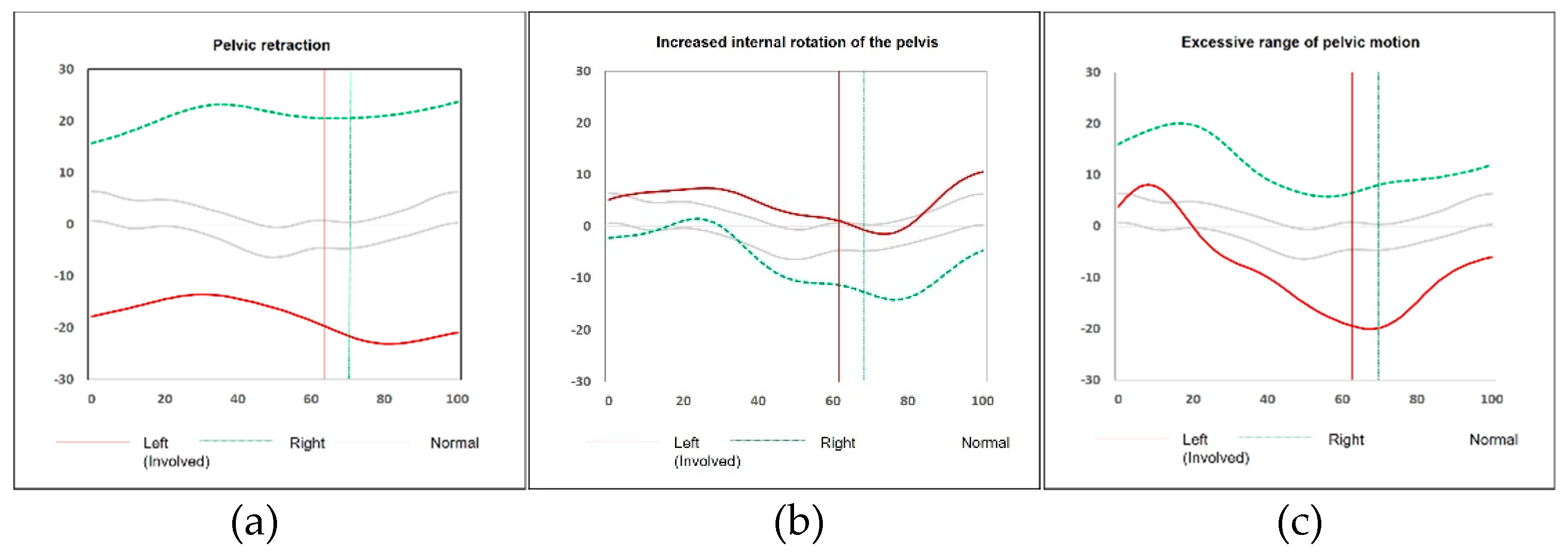
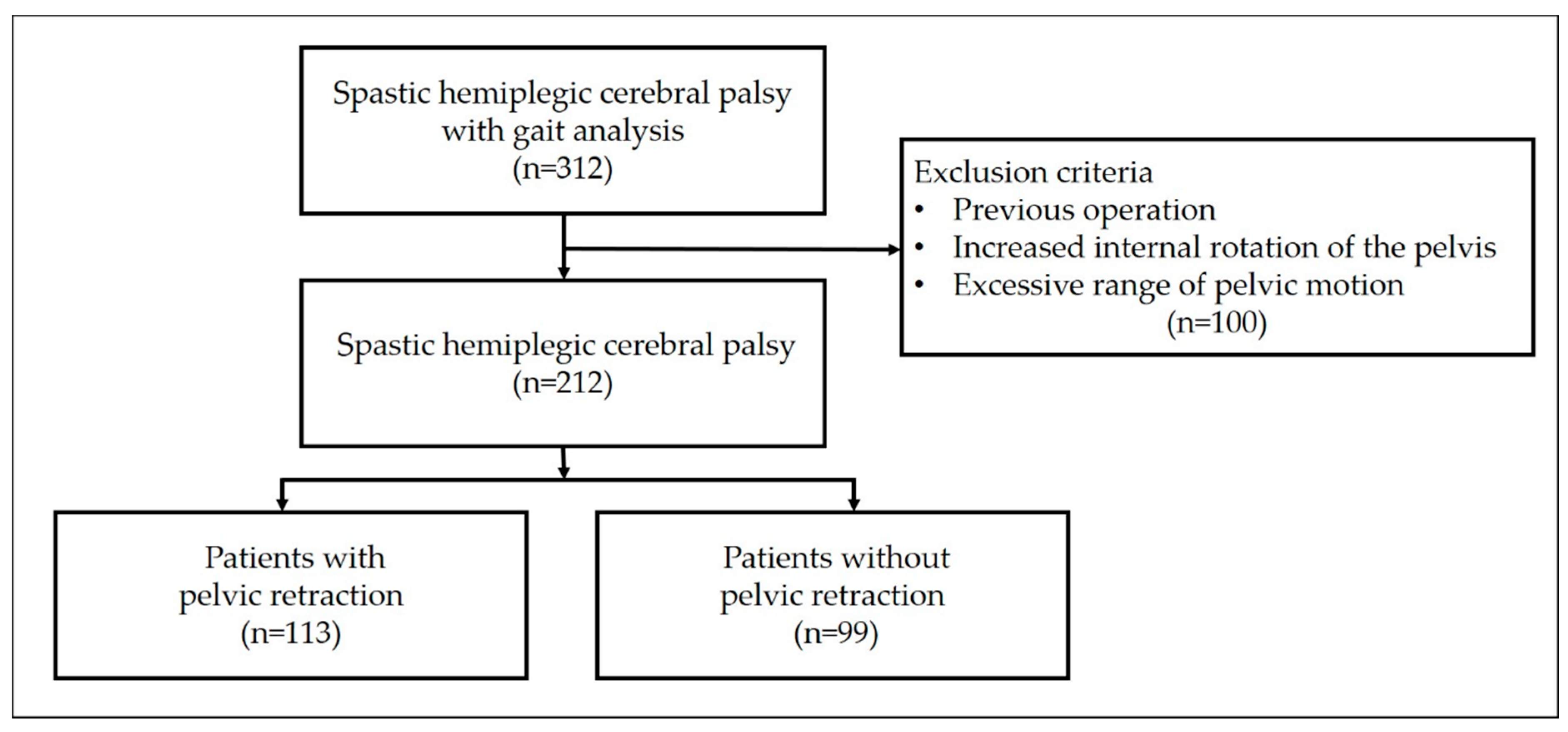
2.1. Subjects
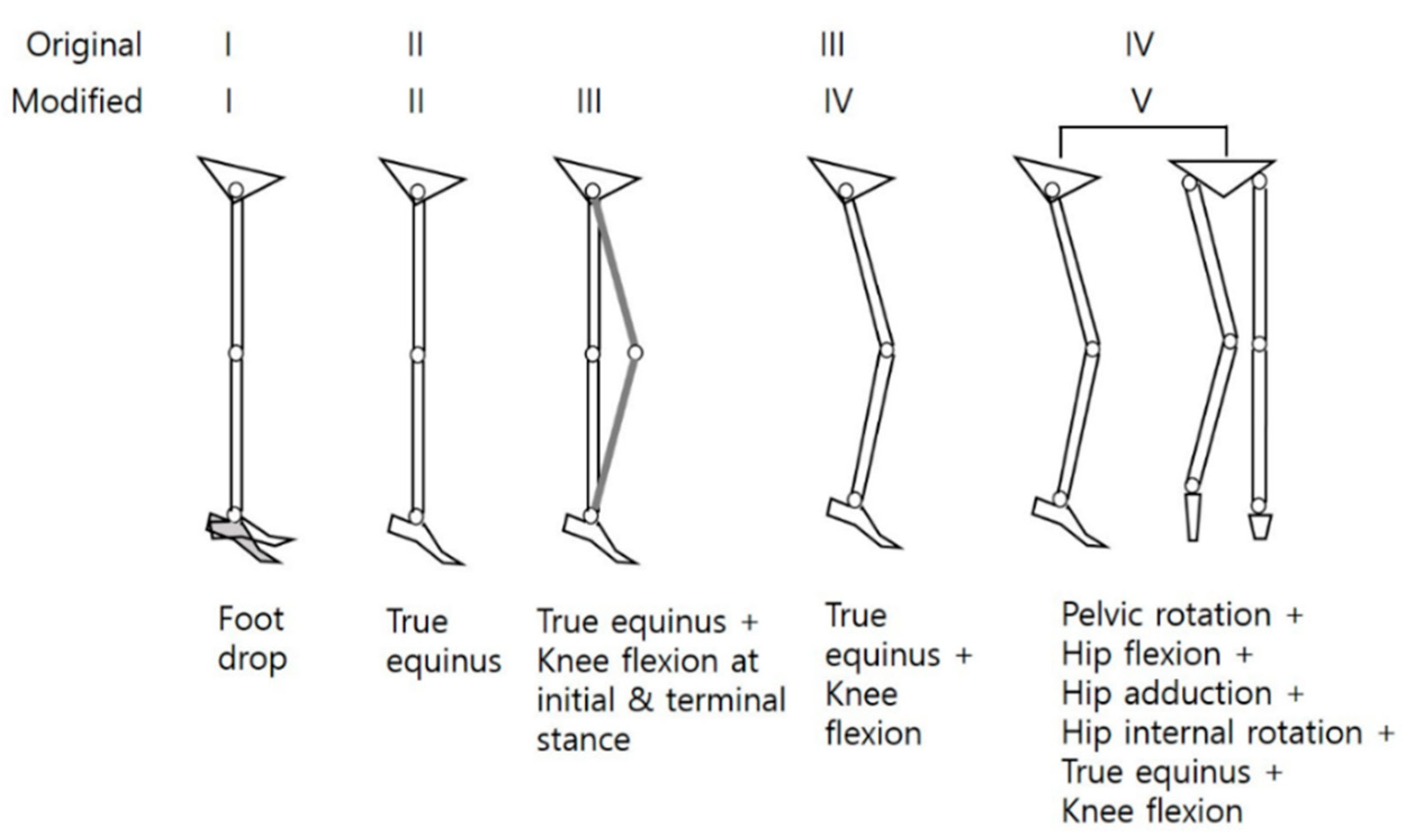
2.2. Clinical and Gait Parameters
2.3. Statistical Analyses
3. Results
3.1. Comparisons between the Groups (Group I vs Group II)
3.2. Gait Factors Classified by Clustering Technique
3.3. Multivariate Logistic Regression Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Gage, J.R.; Schwartz, M.H. Normal gait. In The Identification and Treatment of Gait Problems in Cerebral Palsy, 2nd ed.; Gage, J.R., Schwartz, M.H., Koop, S.E., Novacheck, T.F., Eds.; Mac Keith: London, UK, 2009; pp. 31–64. [Google Scholar]
- O’Sullivan, R.; Walsh, M.; Jenkinson, A.; O’Brien, T. Factors associated with pelvic retraction during gait in cerebral palsy. Gait Posture 2007, 25, 425–431. [Google Scholar] [CrossRef] [PubMed]
- DeLuca, P.A.; Davis, R.B., 3rd; Ounpuu, S.; Rose, S.; Sirkin, R. Alterations in surgical decision making in patients with cerebral palsy based on three-dimensional gait analysis. J. Pediatr. Orthop. 1997, 17, 608–614. [Google Scholar] [CrossRef]
- Aktas, S.; Aiona, M.D.; Orendurff, M. Evaluation of rotational gait abnormality in the patients cerebral palsy. J. Pediatr. Orthop. 2000, 20, 217–220. [Google Scholar] [CrossRef] [PubMed]
- De Morais Filho, M.C.; Kawamura, C.M.; Andrade, P.H.; Dos Santos, M.B.; Pickel, M.R.; Neto, R.B. Factors associated with pelvic asymmetry in transverse plane during gait in patients with cerebral palsy. J. Pediatr. Orthop. B 2009, 18, 320–324. [Google Scholar] [CrossRef]
- Park, C.I.; Park, E.S.; Kim, H.W.; Rha, D.W. Soft tissue surgery for equinus deformity in spastic hemiplegic cerebral palsy: Effects on kinematic and kinetic parameters. Yonsei Med. J. 2006, 47, 657–666. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Carty, C.P.; Walsh, H.P.; Gillett, J.G.; Phillips, T.; Edwards, J.M.; deLacy, M.; Boyd, R.N. The effect of femoral derotation osteotomy on transverse plane hip and pelvic kinematics in children with cerebral palsy: A systematic review and meta-analysis. Gait Posture 2014, 40, 333–340. [Google Scholar] [CrossRef]
- Aminian, A.; Vankoski, S.J.; Dias, L.; Novak, R.A. Spastic hemiplegic cerebral palsy and the femoral derotation osteotomy: Effect at the pelvis and hip in the transverse plane during gait. J. Pediatr. Orthop. 2003, 23, 314–320. [Google Scholar] [CrossRef]
- Saraph, V.; Zwick, E.B.; Zwick, G.; Dreier, M.; Steinwender, G.; Linhart, W. Effect of derotation osteotomy of the femur on hip and pelvis rotations in hemiplegic and diplegic children. J. Pediatr. Orthop. B 2002, 11, 159–166. [Google Scholar] [PubMed]
- Park, J.; Seeley, M.K.; Francom, D.; Reese, C.S.; Hopkins, J.T. Functional vs. traditional analysis in biomechanical gait data: An alternative statistical approach. J. Hum. Kinet. 2017, 60, 39–49. [Google Scholar] [CrossRef]
- Miller, F. Cerebral Palsy, 1st ed.; Springer: New York, NY, USA, 2005; pp. 335–340. [Google Scholar]
- Cimolin, V.; Galli, M.; Tenore, N.; Albertini, G.; Crivellini, M. Gait strategy of uninvolved limb in children with spastic hemiplegia. Eura Medicophys. 2007, 43, 303–310. [Google Scholar] [PubMed]
- O’Malley, M.J.; Abel, M.F.; Damiano, D.L.; Vaughan, C.L. Fuzzy clustering of children with cerebral palsy based on temporal-distance gait parameters. IEEE Trans. Rehabil. Eng. 1997, 5, 300–309. [Google Scholar] [CrossRef] [PubMed]
- Carriero, A.; Zavatsky, A.; Stebbins, J.; Theologis, T.; Shefelbine, S.J. Determination of gait patterns in children with spastic diplegic cerebral palsy using principal components. Gait Posture 2009, 29, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Salazar-Torres, J.J.; McDowell, B.C.; Kerr, C.; Cosgrove, A.P. Pelvic kinematics and their relationship to gait type in hemiplegic cerebral palsy. Gait Posture 2011, 33, 620–624. [Google Scholar] [CrossRef]
- Niklasch, M.; Doderlein, L.; Klotz, M.C.; Braatz, F.; Wolf, S.I.; Dreher, T. Asymmetric pelvic and hip rotation in children with bilateral cerebral palsy: Uni- or bilateral femoral derotation osteotomy? Gait Posture 2015, 41, 670–675. [Google Scholar] [CrossRef]
- Ansari, N.N.; Naghdi, S.; Arab, T.K.; Jalaie, S. The interrater and intrarater reliability of the Modified Ashworth Scale in the assessment of muscle spasticity: Limb and muscle group effect. NeuroRehabilitation 2008, 23, 231–237. [Google Scholar]
- Davids, J.R.; Benfanti, P.; Blackhurst, D.W.; Allen, B.L. Assessment of femoral anteversion in children with cerebral palsy: Accuracy of the trochanteric prominence angle test. J. Pediar. Orthop. 2002, 22, 173–178. [Google Scholar] [CrossRef]
- Sangeux, M.; Mahy, J.; Graham, H.K. Do physical examination and CT-scan measures of femoral neck. A anteversion and tibial torsion relate to each other? Gait Posture 2014, 39, 12–16. [Google Scholar] [CrossRef]
- Ounpuu, S.; DeLuca, P.; Davis, R.; Romness, M. Long-term effects of femoral derotation osteotomies: An evaluation using three-dimensional gait analysis. J. Pediatr. Orthop. 2002, 22, 139–145. [Google Scholar] [CrossRef]
- Graham, H.K.; Baker, R.; Dobson, F.; Morris, M.E. Multilevel orthopaedic surgery in group IV spastic hemiplegia. J. Bone Joint Surg. Br. 2005, 87, 548–555. [Google Scholar] [CrossRef][Green Version]
- Carriero, A.; Zavatsky, A.; Stebbins, J.; Theologis, T.; Shefelbine, S.J. Correlation between lower limb bone morphology and gait characteristics in children with spastic diplegic cerebral palsy. J. Pediatr. Orthop. 2009, 29, 73–79. [Google Scholar] [CrossRef] [PubMed]
- Winters, T.F., Jr.; Gage, J.R.; Hicks, R. Gait patterns in spastic hemiplegia in children and young adults. J. Bone Joint Surg. Am. 1987, 69, 437–441. [Google Scholar]
- Graham, H.K.; Thomason, P.; Novacheck, T.F. Cerebral Palsy. In Lovell & Winter’s Pediatric Orthopaedics, 7th ed.; Weinstein, S.L., Flynn, J.M., Eds.; Wolters Kluwer: Philadelphia, PA, USA, 2014; Volume 1, pp. 488–489. [Google Scholar]
- Carlson, M.G.; Hearns, K.A.; Inkellis, E.; Leach, M.E. Early results of surgical intervention for elbow deformity in cerebral palsy based on degree of contracture. J. Hand Surg. Am. 2012, 37, 1665–1671. [Google Scholar] [CrossRef]
- Rodda, J.; Graham, H.K. Classification of gait patterns in spastic hemiplegia and spastic diplegia: A basis for a management algorithm. Eur. J. Neurol. 2001, 8 (Suppl. 5), 98–108. [Google Scholar] [CrossRef]
- Kay, R.M.; Rethlefsen, S.; Reed, M.; Do, K.P.; Skaggs, D.L.; Wren, T.A. Changes in pelvic rotation after soft tissue and bony surgery in ambulatory children with cerebral palsy. J. Pediatr. Orthop. 2004, 24, 278–282. [Google Scholar] [CrossRef]
- Jiang, N.; Peng, L.; Al-Qwbani, M.; Xie, G.P.; Yang, Q.M.; Chai, Y.; Zhang, Q.; Yu, B. Femoral version, neck-shaft angle, and acetabular anteversion in Chinese Han population: A retrospective analysis of 466 healthy adults. Medicine 2015, 94, e891. [Google Scholar] [CrossRef] [PubMed]
- Kristiansen, L.P.; Gunderson, R.B.; Steen, H.; Reikeras, O. The normal development of tibial torsion. Skeletal Radiol. 2001, 30, 519–522. [Google Scholar] [CrossRef]
- Brunner, R.; Dreher, T.; Romkes, J.; Frigo, C. Effects of plantarflexion on pelvis and lower limb kinematics. Gait Posture 2008, 28, 150–156. [Google Scholar] [CrossRef]
- Rutz, E.; Passmore, E.; Baker, R.; Graham, H.K. Multilevel surgery improves gait in spastic hemiplegia but does not resolve hip dysplasia. Clin. Orthop. Relat. Res. 2012, 470, 1294–1302. [Google Scholar] [CrossRef]
- Riad, J.; Haglund-Akerlind, Y.; Miller, F. Classification of spastic hemiplegic cerebral palsy in children. J. Pediatr. Orthop. 2007, 27, 758–764. [Google Scholar] [CrossRef]
- Riad, J.; Coleman, S.; Miller, F. Arm posturing during walking in children with spastic hemiplegic cerebral palsy. J. Pediatr. Orthop. 2007, 27, 137–141. [Google Scholar] [CrossRef]

| Group I | Group II | *p | |
|---|---|---|---|
| Limb length discrepancy, mm | 6.8 ± 7.0 | 6.7 ± 7.2 | 0.881 |
| Limb length discrepancy (by scanogram), mm | 6.61 ± 4.67 | 7.16 ± 6.30 | 0.521 |
| Femoral anteversion, degrees | 28.8 ± 11.7 | 26.6 ± 13.0 | 0.182 |
| Femoral anteversion (by CT) (1), degrees | 29.25 ± 11.88 | 26.22 ± 12.43 | 0.105 |
| Tibial torsion, degrees | 29.4 ± 12.1 | 26.5 ± 9.4 | 0.061 |
| Tibial torsion (by CT) (2), degrees | 29.09 ± 10.54 | 27.51 ± 10.00 | 0.371 |
| Hip flexion, degrees | 120.78 ± 5.55 | 120.43 ± 2.41 | 0.565 |
| Hip external rotation, degrees | 45.37 ± 9.96 | 48.12 ± 13.32 | 0.159 |
| Hip internal rotation, degrees | 42.26 ± 9.79 | 42.39 ± 12.88 | 0.943 |
| Popliteal angle, degrees | 21.49 ± 13.85 | 21.55 ± 12.33 | 0.977 |
| Rectus femoris tightness, grade | 0(32), 1(24), 2(3), 3(0) | 0(43), 1(16), 2(2), 3(1) | 0.153 |
| Gastrocnemius tightness, degrees | 83.87 ± 17.15 | 90.64 ± 8.34 | <0.001 * |
| Achilles tendon tightness, degrees | 91.03 ± 17.30 | 98.35 ± 9.29 | <0.001 * |
| Group I | Group II | *p | |
|---|---|---|---|
| Recurvatum gait | Yes (50) vs. No (63) | Yes (35) vs. No (64) | 0.187 |
| Pes equinovarus | Yes (44) vs. No (68) | Yes (23) vs. No (76) | 0.028 * |
| Asymmetrical posturing of the upper extremity | Yes (50) vs. No (63) | Yes (50) vs. No (63) | <0.001 * |
| Modified Winters classification | I(17) II(45) III(23) IV(24) V(4) | I(34) II(30) III(21) IV(12) V(2) | 0.011 * |
| Group I | Group II | *p | |
|---|---|---|---|
| Cadence, steps/min | 123.81 ± 26.33 | 123.86 ± 19.64 | 0.987 |
| Step time, s | 0.54 ± 0.17 | 0.51 ± 0.11 | 0.127 |
| Stride time, s | 1.03 ± 0.27 | 0.99 ± 0.16 | 0.223 |
| Step length, m | 0.39 ± 0.11 | 0.45 ± 0.09 | <0.001 * |
| Stride length, m | 0.79 ± 0.22 | 0.88 ± 0.22 | 0.005 * |
| Walking speed, m/s | 0.8 ± 0.25 | 0.89 ± 0.23 | 0.008 * |
| Group I | Group II | *p | |
|---|---|---|---|
| Average anterior pelvic tilt | 19.20 ± 6.04 | 15.76 ± 5.67 | <0.001 * |
| Average pelvic rotation | −13.17 ± 5.75 | −0.81 ± 3.77 | <0.001 * |
| Pelvic rotation at initial contact | −8.45 ± 7.29 | 1.84 ± 5.47 | <0.001 * |
| Average pelvic obliquity | −1.97 ± 4.5 | −0.51 ± 2.68 | 0.004 * |
| Maximum hip extension | 6.70 ± 11.32 | −0.59 ± 7.98 | <0.001 * |
| Average hip rotation | 1.37 ± 9.86 | −1.57 ± 8.04 | 0.017 * |
| Maximum knee flexion | 41.55 ± 10.00 | 45.78 ± 9.20 | 0.002 * |
| Maximum ankle dorsiflexion | 3.39 ± 13.48 | 10.46 ± 7.64 | <0.001 * |
| Ankle dorsiflexion at initial contact | −11.16 ± 10.07 | −6.90 ± 7.44 | <0.001 * |
| Average ankle rotation | 5.95 ± 14.10 | −0.63 ± 10.43 | <0.001 * |
| Factor1 | Factor2 | Factor3 | Factor4 | Factor5 | Factor6 | Factor7 | Factor8 | |
|---|---|---|---|---|---|---|---|---|
| Age | 0.058 | 0.573 | 0.345 | 0.007 | 0.260 | 0.012 | 0.074 | −0.052 |
| Cadence | −0.055 | −0.083 | −0.962 * | 0.005 | 0.041 | −0.039 | 0.009 | 0.002 |
| Stride time | −0.001 | −0.004 | 0.993 * | 0.019 | −0.021 | 0.011 | −0.028 | −0.004 |
| Step time | 0.013 | −0.008 | 0.962 * | 0.030 | −0.043 | 0.003 | −0.014 | 0.025 |
| Stride length | −0.017 | 0.922 * | 0.164 | −0.016 | −0.052 | 0.045 | −0.041 | −0.001 |
| Step length | −0.078 | 0.924 * | 0.044 | 0.003 | −0.042 | −0.011 | −0.062 | −0.021 |
| Walking speed | 0.006 | 0.858 * | −0.323 | −0.019 | −0.066 | 0.045 | 0.001 | 0.017 |
| ROM of pelvic sagittal motion | −0.261 | −0.076 | 0.144 | 0.061 | −0.181 | 0.013 | 0.372 | 0.168 |
| Avg. pelvic anterior tilt | 0.032 | −0.074 | −0.093 | 0.002 | 0.017 | 0.011 | 0.902 * | −0.032 |
| ROM of pelvic coronal motion | 0.003 | 0.232 | −0.034 | −0.043 | −0.361 | 0.166 | 0.516 | 0.068 |
| Avg. pelvic obliquity | −0.013 | −0.130 | 0.039 | 0.182 | 0.205 | 0.736 * | −0.350 | −0.197 |
| Min. hip sagittal angle | −0.048 | −0.104 | 0.136 | −0.019 | 0.464 | −0.038 | 0.641 | −0.039 |
| Avg. hip sagittal angle | 0.012 | 0.027 | −0.015 | 0.052 | 0.538 | −0.034 | 0.678 | −0.082 |
| Max. hip coronal angle | −0.031 | 0.099 | 0.034 | −0.035 | −0.091 | 0.879 * | 0.174 | 0.068 |
| Avg. hip coronal angle | 0.021 | 0.034 | 0.012 | −0.056 | 0.056 | 0.944 * | 0.089 | 0.018 |
| Max. hip transverse angle | 0.034 | −0.001 | −0.068 | 0.069 | 0.032 | −0.057 | 0.005 | 0.940 * |
| Avg. hip transverse angle | 0.014 | −0.072 | 0.084 | 0.054 | 0.091 | 0.032 | −0.009 | 0.929 * |
| Min. knee sagittal angle | −0.028 | 0.185 | −0.082 | −0.077 | 0.954 * | 0.041 | −0.119 | 0.046 |
| ROM of knee sagittal motion | 0.148 | 0.178 | −0.129 | 0.175 | −0.673 | −0.007 | 0.039 | −0.173 |
| Knee sagittal angle at IC | 0.137 | −0.069 | −0.203 | 0.287 | 0.525 | 0.100 | 0.171 | −0.037 |
| Avg. knee transverse angle | 0.034 | 0.528 | 0.067 | 0.139 | 0.130 | −0.418 | 0.046 | −0.109 |
| Max. ankle sagittal angle | 0.935 * | −0.002 | 0.016 | −0.016 | −0.029 | −0.003 | −0.049 | −0.013 |
| Min. ankle sagittal angle | 0.898 * | −0.059 | 0.126 | −0.069 | −0.067 | −0.047 | 0.033 | 0.010 |
| Avg. ankle sagittal angle | 0.962 * | 0.001 | 0.031 | −0.038 | −0.029 | −0.008 | 0.009 | 0.008 |
| Ankle sagittal angle at IC | 0.949 * | −0.012 | −0.067 | 0.046 | 0.016 | 0.038 | −0.017 | 0.054 |
| Avg. ankle transverse angle | −0.095 | −0.156 | 0.089 | 0.846 * | −0.233 | −0.018 | 0.079 | −0.217 |
| Max. foot progression angle | −0.047 | 0.089 | −0.008 | 0.921 * | 0.052 | −0.006 | −0.026 | 0.173 |
| Avg. foot progression angle | 0.024 | 0.074 | −0.004 | 0.947 * | 0.061 | 0.011 | −0.043 | 0.162 |
| Estimate | Standard Error | 95% Wald | Pr > k2 | |||
|---|---|---|---|---|---|---|
| Confidence | Limits | |||||
| Factor 1 (Ankle dorsiflexion) | 0.382 | 0.350 | 0.192 | 0.757 | 0.006 * | |
| Factor 2 (Walking speed, stride & step length) | 0.689 | 0.236 | 0.434 | 1.094 | 0.114 | |
| Factor 3 (Cadence, stride & step time) | 1.013 | 0.219 | 0.660 | 1.555 | 0.953 | |
| Factor 4 (Internal rotation of foot and ankle) | 0.935 | 0.236 | 0.589 | 1.484 | 0.776 | |
| Factor 5 (Knee extension) | 1.411 | 0.332 | 0.736 | 2.706 | 0.299 | |
| Factor 6 (Pelvic obliquity and hip abduction) | 1.037 | 0.257 | 0.627 | 1.715 | 0.889 | |
| Factor 7 (Anterior pelvic tilt) | 2.305 | 0.263 | 1.376 | 3.861 | 0.002 * | |
| Factor 8 (Hip internal rotation) | 1.540 | 0.217 | 1.006 | 2.358 | 0.047 * | |
| Modified Winters classification | 5 vs 1 | 0.015 | 1.590 | <0.001 | 0.841 | 0.021 * |
| 4 vs 1 | 0.844 | 0.584 | 0.190 | 3.754 | 0.548 | |
| 3 vs 1 | 1.540 | 0.552 | 0.452 | 5.253 | 0.084 | |
| 2 vs 1 | 3.785 | 0.658 | 1.202 | 11.921 | 0.005 * | |
| Gastrocnemius tightness | 1.001 | 0.034 | 0.936 | 1.070 | 0.986 | |
| Achilles tendon tightness | 0.998 | 0.033 | 0.935 | 1.065 | 0.947 | |
| Pes equinovarus | 2.381 | 0.266 | 0.838 | 6.763 | 0.103 | |
| Asymmetrical posturing of the upper extremity | 3.440 | 0.295 | 1.081 | 10.941 | 0.036 * | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Park, K.-B.; Park, H.; Park, B.K.; Abdel-Baki, S.W.; Kim, H.W. Clinical and Gait Parameters Related to Pelvic Retraction in Patients with Spastic Hemiplegia. J. Clin. Med. 2019, 8, 679. https://doi.org/10.3390/jcm8050679
Park K-B, Park H, Park BK, Abdel-Baki SW, Kim HW. Clinical and Gait Parameters Related to Pelvic Retraction in Patients with Spastic Hemiplegia. Journal of Clinical Medicine. 2019; 8(5):679. https://doi.org/10.3390/jcm8050679
Chicago/Turabian StylePark, Kun-Bo, Hoon Park, Byoung Kyu Park, Sharkawy Wagih Abdel-Baki, and Hyun Woo Kim. 2019. "Clinical and Gait Parameters Related to Pelvic Retraction in Patients with Spastic Hemiplegia" Journal of Clinical Medicine 8, no. 5: 679. https://doi.org/10.3390/jcm8050679
APA StylePark, K.-B., Park, H., Park, B. K., Abdel-Baki, S. W., & Kim, H. W. (2019). Clinical and Gait Parameters Related to Pelvic Retraction in Patients with Spastic Hemiplegia. Journal of Clinical Medicine, 8(5), 679. https://doi.org/10.3390/jcm8050679