A Threshold of Objectively-Assessed Daily Sedentary Time for All-Cause Mortality in Older Adults: A Meta-Regression of Prospective Cohort Studies
Abstract
:1. Introduction
2. Experimental Section
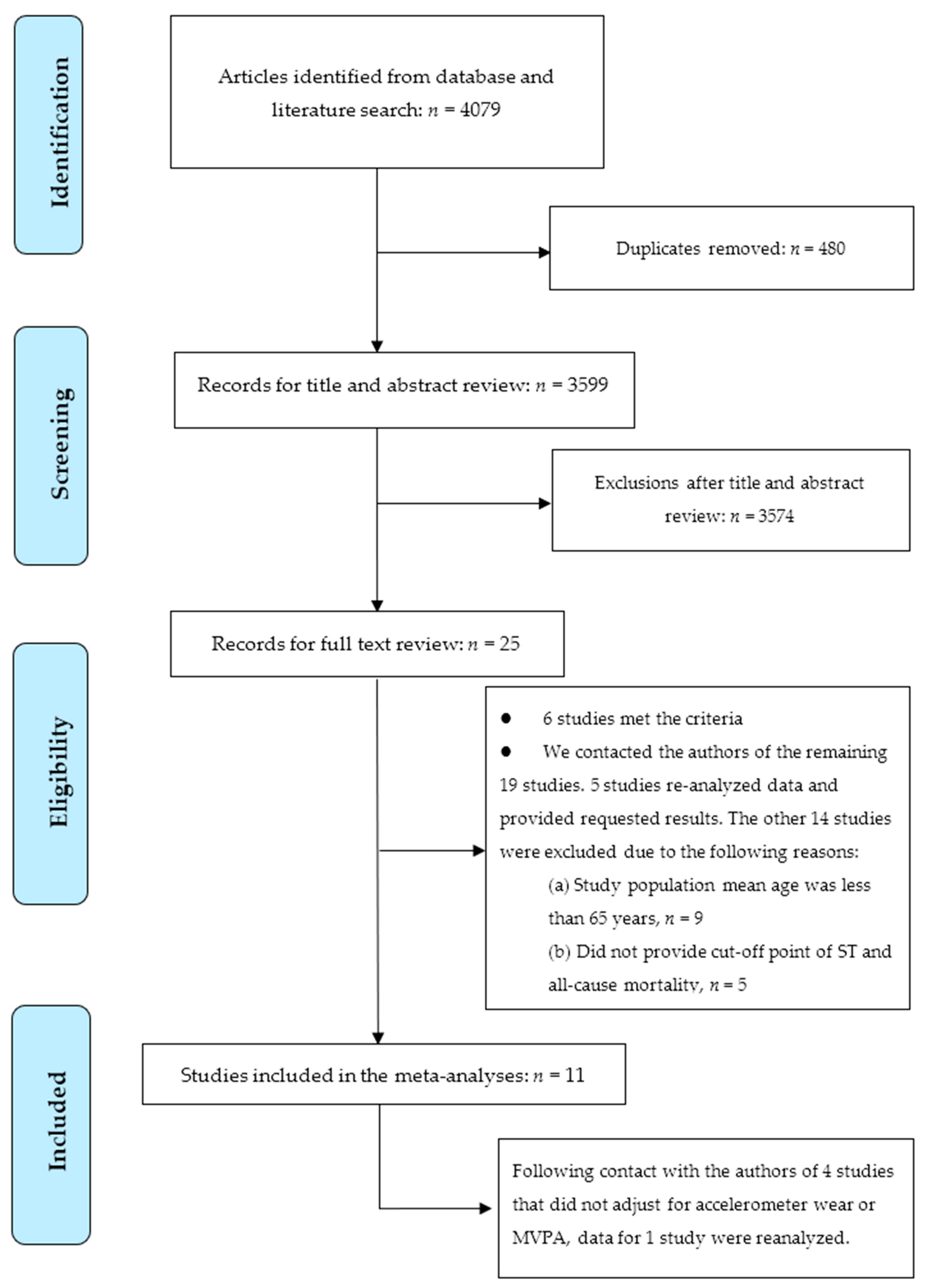
2.1. Study Selection
2.2. Study Inclusion and Exclusion Criteria
2.3. Quality Assessment
2.4. Data Extraction
2.5. Publication Bias
2.6. Statistical Analysis
3. Results
3.1. Study Characteristics
3.2. Sedentary Time and Mortality: Dose-Response Meta-Regression
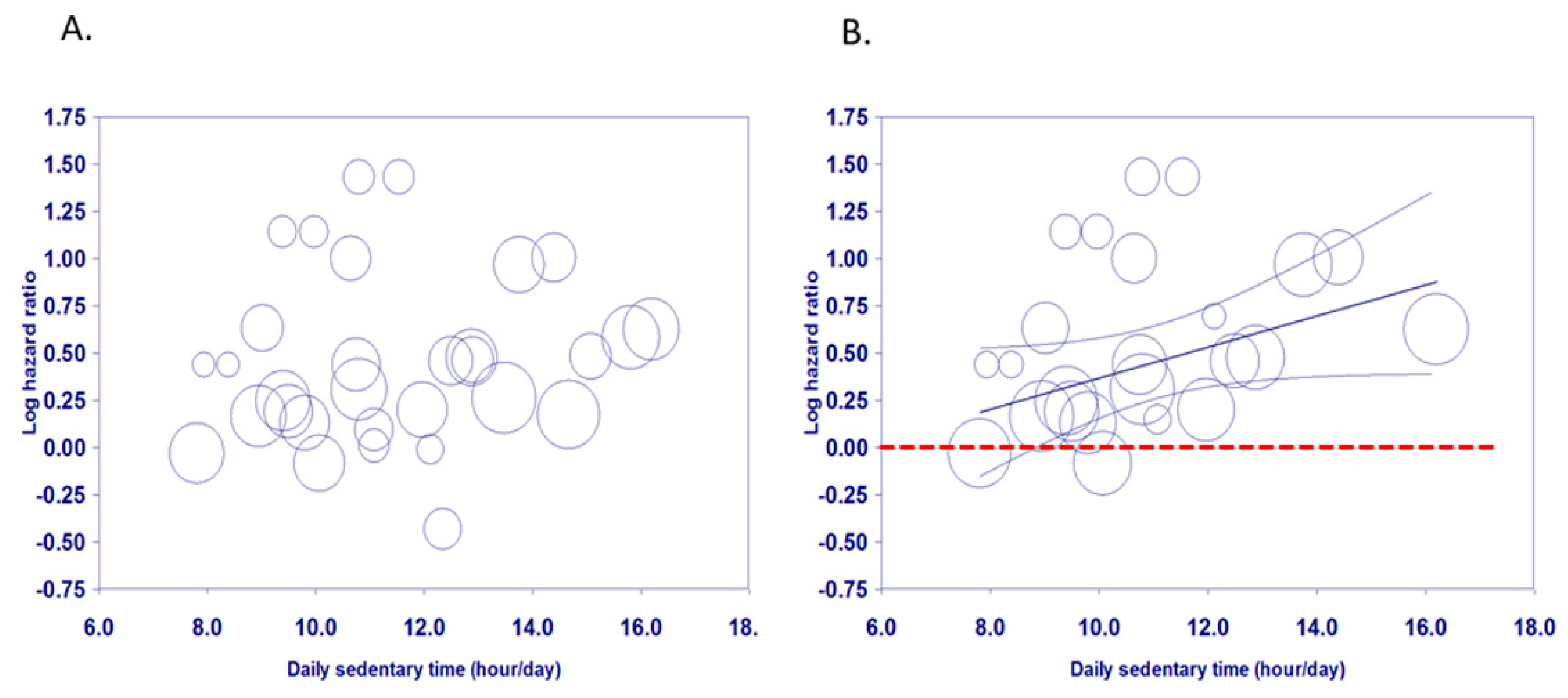
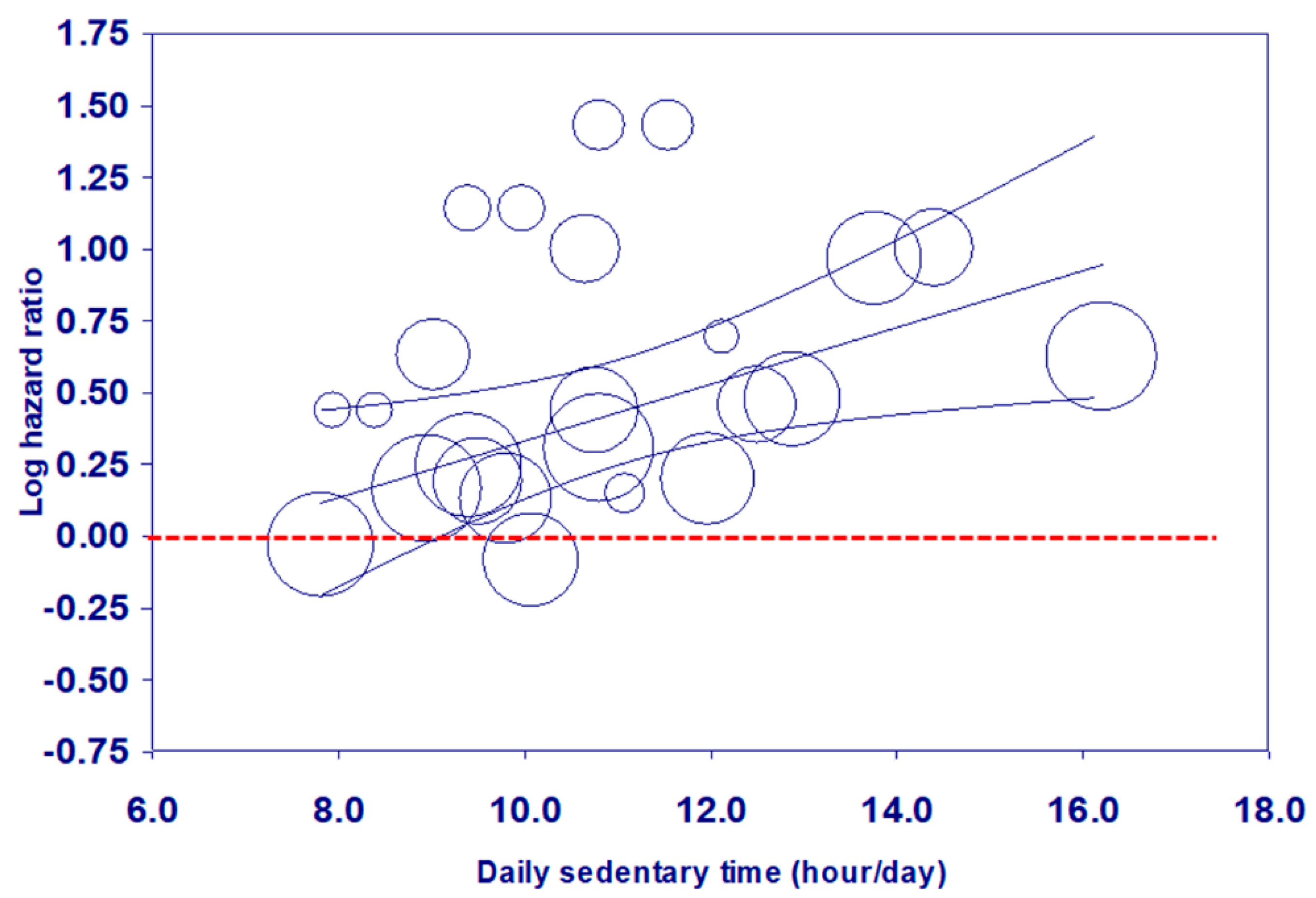
3.3. Visual Assessment of Dose-Response Relationships
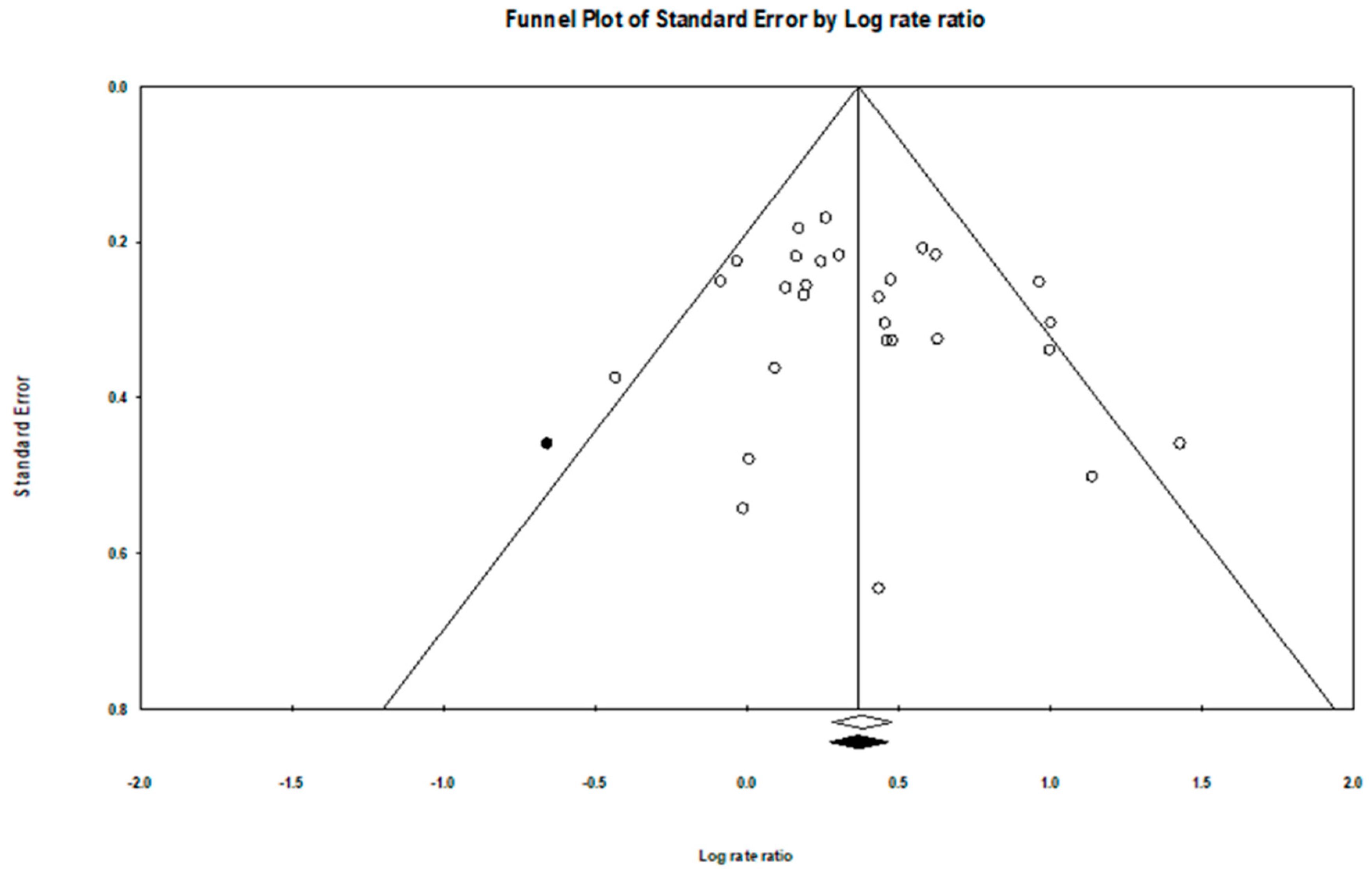
3.4. Evaluation of Publication Bias
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Harvey, J.A.; Chastin, S.F.; Skelton, D.A. How sedentary are older people? A systematic review of the amount of sedentary behavior. J. Aging Phys. Act. 2015, 23, 471–487. [Google Scholar] [CrossRef]
- Manas, A.; Del Pozo-Cruz, B.; Garcia-Garcia, F.J.; Guadalupe-Grau, A.; Ara, I. Role of objectively measured sedentary behaviour in physical performance, frailty and mortality among older adults: A short systematic review. Eur. J. Sport Sci. 2017, 17, 940–953. [Google Scholar] [CrossRef] [PubMed]
- De Rezende, L.F.; Sá, T.H.; Mielke, G.I.; Viscondi, J.Y.K.; Rey-López, J.P.; Garcia, L.M.T. All-cause mortality attributable to sitting time: Analysis of 54 countries worldwide. Am. J. Prev. Med. 2016, 51, 253–263. [Google Scholar] [CrossRef]
- UK Department of Health. Start Active, Stay Active: A Report on Physical Activity from the Four Home Countries’ Chief Medical Officers; Department of Health: London, UK, 2011.
- Australian Department of Health. Australia’s Physical Activity and Sedentary Behaviour Guidelines; Australian Department of Health: Canberra, Australia, 2017.
- Stamatakis, E.; Ekelund, U.; Ding, D.; Hamer, M.; Bauman, A.E.; Lee, I.-M. Is the time right for quantitative public health guidelines on sitting? A narrative review of sedentary behaviour research paradigms and findings. Br. J. Sports Med. 2019, 53, 377–382. [Google Scholar] [CrossRef]
- Rezende, L.F.M.; Rey-López, J.P.; Matsudo, V.K.R.; Luiz, O.C. Sedentary behavior and health outcomes among older adults: A systematic review. BMC Public Health 2014, 14, 333. [Google Scholar] [CrossRef]
- Klenk, J.; Dallmeier, D.; Denkinger, M.D.; Rapp, K.; Koenig, W.; Rothenbacher, D.; Group, A.S. Objectively measured walking duration and sedentary behaviour and four-year mortality in older people. PLoS ONE 2016, 11, e0153779. [Google Scholar] [CrossRef] [PubMed]
- Fox, K.R.; Ku, P.-W.; Hillsdon, M.; Davis, M.G.; Simmonds, B.A.; Thompson, J.L.; Stathi, A.; Gray, S.F.; Sharp, D.J.; Coulson, J.C. Objectively assessed physical activity and lower limb function and prospective associations with mortality and newly diagnosed disease in uk older adults: An opal four-year follow-up study. Age Ageing 2015, 44, 261–268. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.; Rowe, D.A. Issues and challenges in sedentary behavior measurement. Meas. Phys. Educ. Exerc. Sci. 2015, 19, 105–115. [Google Scholar] [CrossRef]
- Diaz, K.M.; Howard, V.J.; Hutto, B.; Colabianchi, N.; Vena, J.E.; Safford, M.M.; Blair, S.N.; Hooker, S.P. Patterns of sedentary behavior and mortality in us middle-aged and older adults: A national cohort study. Ann. Intern. Med. 2017, 167, 465–475. [Google Scholar] [CrossRef] [PubMed]
- Jefferis, B.J.; Parsons, T.J.; Sartini, C.; Ash, S.; Lennon, L.T.; Papacosta, O.; Morris, R.W.; Wannamethee, S.G.; Lee, I.-M.; Whincup, P.H. Objectively measured physical activity, sedentary behaviour and all-cause mortality in older men: Does volume of activity matter more than pattern of accumulation? Br. J. Sports Med. 2018, 0, 1–8. [Google Scholar] [CrossRef]
- Lee, I.-M.; Shiroma, E.J.; Evenson, K.R.; Kamada, M.; LaCroix, A.Z.; Buring, J.E. Accelerometer-measured physical activity and sedentary behavior in relation to all-cause mortality: The women’s health study. Circulation 2018, 137, 203–205. [Google Scholar] [CrossRef]
- Schmid, D.; Ricci, C.; Leitzmann, M.F. Associations of objectively assessed physical activity and sedentary time with all-cause mortality in us adults: The nhanes study. PLoS ONE 2015, 10, e0119591. [Google Scholar] [CrossRef]
- Ensrud, K.E.; Blackwell, T.L.; Cauley, J.A.; Dam, T.-T.L.; Cawthon, P.M.; Schousboe, J.T. Objective measures of activity level and mortality in older men. J. Am. Geriatr. Soc. 2014, 62, 2079–2087. [Google Scholar] [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The prisma statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- Dohrn, M.; Sjöström, M.; Kwak, L.; Oja, P.; Hagströmer, M. Accelerometer-measured sedentary time and physical activity—A 15 year follow-up of mortality in a swedish population-based cohort. J. Sci. Med. Sport 2018, 21, 702–707. [Google Scholar] [CrossRef]
- Edwards, M.K.; Loprinzi, P.D. All-cause mortality risk as a function of sedentary behavior, moderate-to-vigorous physical activity and cardiorespiratory fitness. Phys. Sportsmed. 2016, 44, 223–230. [Google Scholar] [CrossRef]
- Evenson, K.R.; Herring, A.H.; Wen, F. Accelerometry-assessed latent class patterns of physical activity and sedentary behavior with mortality. Am. J. Prev. Med. 2017, 52, 135–143. [Google Scholar] [CrossRef]
- Evenson, K.R.; Wen, F.; Herring, A.H. Associations of accelerometry-assessed and self-reported physical activity and sedentary behavior with all-cause and cardiovascular mortality among us adults. Am. J. Epidemiol. 2016, 184, 621–632. [Google Scholar] [CrossRef]
- Koolhaas, C.M.; Dhana, K.; van Rooij, F.J.; Kocevska, D.; Hofman, A.; Franco, O.H.; Tiemeier, H. Sedentary time assessed by actigraphy and mortality: The rotterdam study. Prev. Med. 2017, 95, 59–65. [Google Scholar] [CrossRef]
- Koster, A.; Caserotti, P.; Patel, K.V.; Matthews, C.E.; Berrigan, D.; Domelen, D.R.; Brychta, R.J.; Chen, K.Y.; Harris, T.B. Association of sedentary time with mortality independent of moderate to vigorous physical activity. PLoS ONE 2012, 7, e37696. [Google Scholar] [CrossRef]
- Lee, P.H. Examining non-linear associations between accelerometer-measured physical activity, sedentary behavior, and all-cause mortality using segmented cox regression. Front. Physiol. 2016, 7, 272. [Google Scholar] [CrossRef] [PubMed]
- Matthews, C.E.; Keadle, S.K.; Troiano, R.P.; Kahle, L.; Koster, A.; Brychta, R.; Van Domelen, D.; Caserotti, P.; Chen, K.Y.; Harris, T.B. Accelerometer-measured dose-response for physical activity, sedentary time, and mortality in us adults. Am. J. Clin. Nutr. 2016, 104, 1424–1432. [Google Scholar] [CrossRef]
- Fishman, E.I.; Steeves, J.A.; Zipunnikov, V.; Koster, A.; Berrigan, D.; Harris, T.A.; Murphy, R. Association between objectively measured physical activity and mortality in nhanes. Med. Sci. Sports Exerc. 2016, 48, 1303–1311. [Google Scholar] [CrossRef]
- Schmid, D.; Ricci, C.; Baumeister, S.E.; Leitzmann, M.F. Replacing sedentary time with physical activity in relation to mortality. Med. Sci. Sports Exerc. 2016, 48, 1312–1319. [Google Scholar] [CrossRef] [PubMed]
- Borgundvaag, E.; Janssen, I. Objectively measured physical activity and mortality risk among American adults. Am. J. Prev. Med. 2017, 52, e25–e31. [Google Scholar] [CrossRef]
- Loprinzi, P.D. Light-intensity physical activity and all-cause mortality. Am. J. Health Promot. 2017, 31, 340–342. [Google Scholar] [CrossRef]
- Theou, O.; Blodgett, J.M.; Godin, J.; Rockwood, K. Association between sedentary time and mortality across levels of frailty. CMAJ 2017, 189, E1056–E1064. [Google Scholar] [CrossRef]
- Dohrn, I.M.; Kwak, L.; Oja, P.; Sjöström, M.; Hagströmer, M. Replacing sedentary time with physical activity: A 15-year follow-up of mortality in a national cohort. Clin. Epidemiol. 2018, 10, 179–186. [Google Scholar] [CrossRef]
- LaMonte, M.J.; Buchner, D.M.; Rillamas-Sun, E.; Di, C.; Evenson, K.R.; Bellettiere, J.; Lewis, C.E.; Lee, I.M.; Tinker, L.F.; Seguin, R.; et al. Accelerometer-measured physical activity and mortality in women aged 63 to 99. J. Am. Geriatr. Soc. 2018, 66, 886–894. [Google Scholar] [CrossRef]
- Diaz, K.M.; Duran, A.T.; Colabianchi, N.; Judd, S.E.; Howard, V.J.; Hooker, S.P. Potential effects on mortality of replacing sedentary time with short sedentary bouts or physical activity: A national cohort study. Am. J. Epidemiol. 2019, 188, 537–544. [Google Scholar] [CrossRef]
- Shiroma, E.J.; Lee, I.M.; Schepps, M.A.; Kamada, M.; Harris, T.B. Physical activity patterns and mortality: The weekend warrior and activity bouts. Med. Sci. Sports Exerc. 2019, 51, 35–40. [Google Scholar] [CrossRef]
- Loprinzi, P.D.; Loenneke, J.P.; Ahmed, H.M.; Blaha, M.J. Joint effects of objectively-measured sedentary time and physical activity on all-cause mortality. Prev. Med. 2016, 90, 47–51. [Google Scholar] [CrossRef]
- Kmet, L.M.; Lee, R.C.; Cook, L.S. Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields; Alberta Heritage Foundation for Medical Research Edmonton: Edmonton, AB, Canada, 2004; Volume 22. [Google Scholar]
- Ekelund, U.; Steene-Johannessen, J.; Brown, W.J.; Fagerland, M.W.; Owen, N.; Powell, K.E.; Bauman, A.; Lee, I.M. Does physical activity attenuate, or even eliminate, the detrimental association of sitting time with mortality? A harmonised meta-analysis of data from more than 1 million men and women. Lancet 2016, 388, 1302–1310. [Google Scholar] [CrossRef]
- Egger, M.; Smith, G.D.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef]
- Duval, S.; Tweedie, R. A nonparametric “trim and fill” method of accounting for publication bias in meta-analysis. J. Am. Stat. Assoc. 2000, 95, 89–98. [Google Scholar]
- Borenstein, M.; Hedges, L.V.; Higgins, J.; Rothstein, H.R. Introduction to Meta-Analysis; Wiley Online Library: Chichester, UK, 2009. [Google Scholar]
- Aune, D.; Chan, D.S.; Lau, R.; Vieira, R.; Greenwood, D.C.; Kampman, E.; Norat, T. Dietary fibre, whole grains, and risk of colorectal cancer: Systematic review and dose-response meta-analysis of prospective studies. BMJ 2011, 343, d6617. [Google Scholar] [CrossRef]
- Grosso, G.; Micek, A.; Godos, J.; Pajak, A.; Sciacca, S.; Galvano, F.; Giovannucci, E.L. Dietary flavonoid and lignan intake and mortality in prospective cohort studies: Systematic review and dose-response meta-analysis. Am. J. Epidemiol. 2017, 185, 1304–1316. [Google Scholar] [CrossRef]
- Berretta, M.; Micek, A.; Lafranconi, A.; Rossetti, S.; Di Francia, R.; De Paoli, P.; Rossi, P.; Facchini, G. Coffee consumption is not associated with ovarian cancer risk: A dose-response meta-analysis of prospective cohort studies. Oncotarget 2018, 9, 20807–20815. [Google Scholar] [CrossRef] [PubMed]
- Lafranconi, A.; Micek, A.; Galvano, F.; Rossetti, S.; Del Pup, L.; Berretta, M.; Facchini, G. Coffee decreases the risk of endometrial cancer: A dose-response meta-analysis of prospective cohort studies. Nutrients 2017, 9, 1223. [Google Scholar] [CrossRef] [PubMed]
- Qiang, Y.; Li, Q.; Xin, Y.; Fang, X.; Tian, Y.; Ma, J.; Wang, J.; Wang, Q.; Zhang, R.; Wang, J.; et al. Intake of dietary one-carbon metabolism-related b vitamins and the risk of esophageal cancer: A dose-response meta-analysis. Nutrients 2018, 10, 835. [Google Scholar] [CrossRef]
- Kelly, P.; Kahlmeier, S.; Gotschi, T.; Orsini, N.; Richards, J.; Roberts, N.; Scarborough, P.; Foster, C. Systematic review and meta-analysis of reduction in all-cause mortality from walking and cycling and shape of dose response relationship. Int. J. Behav. Nutr. Phys. Act. 2014, 11, 132. [Google Scholar] [CrossRef]
- Yao, B.; Fang, H.; Xu, W.; Yan, Y.; Xu, H.; Liu, Y.; Mo, M.; Zhang, H.; Zhao, Y. Dietary fiber intake and risk of type 2 diabetes: A dose-response analysis of prospective studies. Eur. J. Epidemiol. 2014, 29, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Grosso, G.; Micek, A.; Castellano, S.; Pajak, A.; Galvano, F. Coffee, tea, caffeine and risk of depression: A systematic review and dose-response meta-analysis of observational studies. Mol. Nutr. Food Res. 2016, 60, 223–234. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Thompson, S.G. Quantifying heterogeneity in a meta-analysis. Stat. Med. 2002, 21, 1539–1558. [Google Scholar] [CrossRef]
- Burgers, A.M.G.; Biermasz, N.R.; Schoones, J.W.; Pereira, A.M.; Renehan, A.G.; Zwahlen, M.; Egger, M.; Dekkers, O.M. Meta-analysis and dose-response metaregression: Circulating insulin-like growth factor I (IGF-I) and mortality. J. Clin. Endocrinol. Metab. 2011, 96, 2912–2920. [Google Scholar] [CrossRef] [PubMed]
- Bagnardi, V.; Zambon, A.; Quatto, P.; Corrao, G. Flexible meta-regression functions for modeling aggregate dose-response data, with an application to alcohol and mortality. Am. J. Epidemiol. 2004, 159, 1077–1086. [Google Scholar] [CrossRef] [PubMed]
- Wood, A.M.; Kaptoge, S.; Butterworth, A.S.; Willeit, P.; Warnakula, S.; Bolton, T.; Paige, E.; Paul, D.S.; Sweeting, M.; Burgess, S. Risk thresholds for alcohol consumption: Combined analysis of individual-participant data for 599 912 current drinkers in 83 prospective studies. Lancet 2018, 391, 1513–1523. [Google Scholar] [CrossRef]
- Borenstein, M.; Hedges, L.; Higgins, J.; Rothstein, H. Comprehensive Meta-Analysis Version 3; Biostat: Englewood, NJ, USA, 2014. [Google Scholar]
- Discacciati, A.; Crippa, A.; Orsini, N. Goodness of fit tools for dose-response meta-analysis of binary outcomes. Res. Synth. Methods 2017, 8, 149–160. [Google Scholar] [CrossRef] [PubMed]
- Il’yasova, D.; Hertz-Picciotto, I.; Peters, U.; Berlin, J.A.; Poole, C. Choice of exposure scores for categorical regression in meta-analysis: A case study of a common problem. Cancer Causes Control CCC 2005, 16, 383–388. [Google Scholar] [CrossRef] [PubMed]
- Bagnardi, V.; Rota, M.; Botteri, E.; Tramacere, I.; Islami, F.; Fedirko, V.; Scotti, L.; Jenab, M.; Turati, F.; Pasquali, E.; et al. Alcohol consumption and site-specific cancer risk: A comprehensive dose-response meta-analysis. Br. J. Cancer 2015, 112, 580–593. [Google Scholar] [CrossRef]
- Berlin, J.A.; Longnecker, M.P.; Greenland, S. Meta-analysis of epidemiologic dose-response data. Epidemiology 1993, 4, 218–228. [Google Scholar] [CrossRef]
- Shao, C.; Tang, H.; Zhao, W.; He, J. Nut intake and stroke risk: A dose-response meta-analysis of prospective cohort studies. Sci. Rep. 2016, 6, 30394. [Google Scholar] [CrossRef] [PubMed]
- Knapp, G.; Hartung, J. Improved tests for a random effects meta-regression with a single covariate. Stat. Med. 2003, 22, 2693–2710. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Ku, P.-W.; Steptoe, A.; Liao, Y.; Hsueh, M.-C.; Chen, L.-J. A cut-off of daily sedentary time and all-cause mortality in adults: A meta-regression analysis involving more than 1 million participants. BMC Med. 2018, 16, 74. [Google Scholar] [CrossRef]
- Van Dyck, D.; Cerin, E.; De Bourdeaudhuij, I.; Hinckson, E.; Reis, R.S.; Davey, R.; Sarmiento, O.L.; Mitas, J.; Troelsen, J.; MacFarlane, D. International study of objectively-measured physical activity and sedentary time with body mass index and obesity: Ipen adult study. Int. J. Obes. 2015, 39, 199–207. [Google Scholar] [CrossRef]
- Levine, T.R.; Asada, K.J.; Carpenter, C. Sample sizes and effect sizes are negatively correlated in meta-analyses: Evidence and implications of a publication bias against nonsignificant findings. Commun. Monogr. 2009, 76, 286–302. [Google Scholar] [CrossRef]
- Chau, J.Y.; Grunseit, A.C.; Chey, T.; Stamatakis, E.; Brown, W.J.; Matthews, C.E.; Bauman, A.E.; van der Ploeg, H.P. Daily sitting time and all-cause mortality: A meta-analysis. PloS ONE 2013, 8, e80000. [Google Scholar] [CrossRef] [PubMed]
- Schisterman, E.F.; Cole, S.R.; Platt, R.W. Overadjustment bias and unnecessary adjustment in epidemiologic studies. Epidemiology 2009, 20, 488–495. [Google Scholar] [CrossRef] [PubMed]
| Author (Year), Country | Study Population | Follow-Up Years Mean | ST Measure (Mean or Median Time) | Covariates (Number of Covariates) | Cut-off (h/d) | Cox Regression HR (95% CIs) | Quality | ||
|---|---|---|---|---|---|---|---|---|---|
| n (Death) | Age Mean (±SD) | Male (%) | |||||||
| Koster et al., 2012, USA [22] | 1091 (126) | ≥65 M = 74.7 (±6.5) | 68.8% | 2.8 y | Objectively measured SB < 100 counts/1 min [AM-7164 ActiGraph] (ST median: male = 9.18, female = 8.68 h) | Age, sex, race/ethnicity, education, BMI, diabetes, coronary heart disease, congestive heart failure, cancer, stroke, mobility limitation, smoking, alcohol, MVPA, accelerometer wear time (15) | Quartile: male/female | 1.0 | |
| <7.6/<7.2 (ref.) | 1.00 | ||||||||
| >7.6–≤9.18/ > 7.2–≤8.68 | 1.55 (0.44–5.54) | ||||||||
| >9.18–≤10.75/ >8.68–≤10.09 | 3.13 (1.17–8.39) * | ||||||||
| >10.75/>10.09 | 4.18 (1.70–10.31) * | ||||||||
| Ensrud et al., 2014, USA [15] | 2918 (409) | ≥71 M = 79 (±5.2) | 100% | 4.5 y | Objectively measured SB ≤ 1.50 METs [sensewear pro armband] (ST median = 14.08 h) | Age, sex, race, education, marital status, site, season, health status, comorbidity burden, depressive symptoms, cognitive function, body fat %, number of instrumental activity of daily living impairments, smoking, sleep time, gait speed, self-reported total PA (17) ¶ | ≤12.86 (ref.) | 1.00 † | 0.95 |
| 12.87–14.08 | 1.30 (0.93–1.81) | ||||||||
| 14.09–15.24 | 1.19 (0.83–1.70) | ||||||||
| >15.24 | 1.79 (1.19–2.70) * | ||||||||
| § Fox et al., 2015, UK [9] | 208 (32) | ≥70 M = 78 (±5.7) | 51.2% | 4.3 y | Objectively measured SB < 100 counts/1 min [Actigraph GT1Ms] (ST median = 11.03 h) | Age, sex, educational, index of multiple deprivation, weight status, general practitioner system, number of self-reported chronic illnesses at baseline, lower limb function (9) ¶; Re-analysis further including MVPA & accelerometer wear time = 11) | <10.55 (ref.) | 1.00 | 1.0 |
| ≥10.55–11.59 | 1.01 (0.39–2.56) | ||||||||
| ≥11.6 | 0.99 (0.34–2.86) | ||||||||
| Schmid et al., 2015, USA [14] | 1677 (112) | ≥50 M = 67.2 ‡ | 49% | 2.9 y | Objectively measured SB < 100 counts/1 min [AM-7164 ActiGraph] (ST median = 8.6 h) | Age, sex, education, ethnicity, history of diabetes, cardiovascular disease, cancer, mobility limitations, BMI, smoking, alcohol, light PA, MVPA (13) ¶ | <8.60 (ref.) | 1.00 | 0.95 |
| ≥8.60 | 1.59 (0.84–3.03) †† | ||||||||
| Lee, 2016, USA [23] | 1768 (453) | ≥65 M = 74.7 (±6.5) | 51.8% | 6.3 y | Objectively measured SB < 100 counts/1 min [AM-7164 ActiGraph] (ST median = 10.0 h) | Age, sex, education, income, BMI, self-reported general health, condition, high blood pressure, high cholesterol, type 2 diabetes, history of heart attack, stroke, cancer, energy intake by 24-h dietary recall, binge drinking, smoking, MVPA, accelerometer wear time (18) | Quartile | 1.0 | |
| ≥4.6–<8.8 (ref.) | 1.00 | ||||||||
| ≥8.8–<10.0 | 1.28 (0.82–1.99) | ||||||||
| ≥10.0–<11.6 | 1.36 (0.89–2.09) | ||||||||
| ≥11.6–<20.8 | 1.87 (1.22–2.86) * | ||||||||
| Klenk et al., 2016, Southern Germany [8] | 1271 (100) | ≥65 M = 75.6 (±6.51) | 46.4% | 4 y | Objectively measured lying or sitting activPAL (ST median = 11.75 h) | Age, sex, education, BMI, diabetes, hypertension, cardiovascular disease, cancer, chronic kidney disease, blood glucose. smoking, alcohol, walking time (which includes light, moderate and vigorous intensity physical activity) (13) ¶ | 5.85–<10.4 (ref.) | 1.00 | 0.95 |
| ≥10.4–<11.75 | 1.10 (0.54–2.24) | ||||||||
| ≥11.75–<12.94 | 0.65 (0.31–1.35) | ||||||||
| ≥12.94–<17.21 | 1.62 (0.85–3.07) | ||||||||
| Diaz et al., 2017, USA [11] | 7985 (340) | ≥45 M = 69.8 ‡ | 45.8% | 4 y | Objectively measured SB < 50 counts/1 min [Actical-Philips Respironics] (ST median = 12.44 h) | Age, sex, race, region of residence, education, season, BMI, diabetes, hypertension, dyslipidemia, estimated glomerular filtration rate < 60 mL/min/1.73 m2, atrial fibrillation, history of coronary heart disease, stroke, smoking, alcohol, MVPA, standardized 16 h of accelerometer wear (18) | <11.50 (ref.) | 1.00 † | 1.0 |
| ≥11.50–<12.44 | 1.22 (0.74–2.02) | ||||||||
| ≥12.44–<13.32 | 1.61 (0.99–2.63) | ||||||||
| ≥13.32 | 2.63 (1.60–4.30) * | ||||||||
| Dohrn et al., 2017, Sweden [17] | 851 (79) | ≥35 M = 66.7 (±10.2) | 44.1% | 14.2 y | Objectively measured SB < 100 counts/1 min [AM-7164ActiGraph] (ST mean = 8.20 h) | Age, sex, education, hypertension, heart disease, cancer, diabetes, BMI, smoking, MVPA, accelerometer wear time (11) | 6.55–<8.20 (ref.) | 1.00 | 1.0 |
| 8.20–<9.83 | 1.88 (0.99–3.55) | ||||||||
| ≥9.83 | 2.72 (1.40–5.30) * | ||||||||
| Koolhaas et al., 2017, The Netherlands [21] | 650 (148) | 65–98 M = 72.6 a | 47.4% | 11 y | Objectively measured SB ≤ 199 counts/1 min [Actiwatch model AW4] (ST mean = 9.28 h [1.86]; median = 9.20 h) | Age, sex, education, number of comorbidities, the 24 h activity rhythm, activities of daily living score, smoking, alcohol, MVPA, cohort and time awake (10) | <8 (ref.) | 1.00 | 0.95 |
| 8–<11 | 1.21 (0.71–2.04) | ||||||||
| ≥11 | 1.58 (0.87–2.88) | ||||||||
| Jefferis et al., 2018, UK [12] | 1181 (194) | 71–92 M = 78.4 (±4.6) | 100% | 5.0 y | Objectively measured SB < 100 counts/1 min [ActiGraph GT3X] (ST mean = 10.3 h) | Age, sex, region of residence, living alone, season of wear, social class, BMI, mobility disability, alcohol, smoking, sleep time, MVPA, accelerometer wear time (13) | 4.9–<9.3 (ref.) | 1.00 | 1.0 |
| ≥9.3–<10.3 | 1.14 (0.69–1.91) | ||||||||
| ≥10.3–<11.2 | 1.55 (0.91–2.64) | ||||||||
| ≥11.2–<17.6 | 2.73 (1.50–4.95) * | ||||||||
| Lee et al., 2018, USA [13] | 16,741 (207) | M = 72.0 (±5.7) | 0% | 2.3 y | Objectively measured SB < 200 counts/1 min [ActiGraph Corp] (ST mean = 8.4 h) | Age, sex, hormone therapy, parental history of myocardial infarction, family history of cancer, general health, cardiovascular disease, cancer, cancer screening, smoking, alcohol, intakes of saturated fat/fiber/fruits/ vegetables, MVPA, accelerometer wear time (14) | <7.24 (ref.) | 1.00 | 1.0 |
| ≥7.24–<8.38 | 0.97 (0.62–1.50) | ||||||||
| ≥8.38–<9.51 | 1.18 (0.77–1.82) | ||||||||
| ≥9.51 | 0.92 (0.56–1.50) | ||||||||
| Average of total n (death) = 3303 (200) Total n = 36,341/ Deceased n = 2200 | Total sample M (±SD) age = 73.5 (±4.3) y Total follow-up M (±SD) year = 5.6 (±3.7) y | Total weighted average of ST = 10.08 h | M = 0.98 | ||||||
| Models | Number of ES | Coefficients (SE) | t | p Value |
|---|---|---|---|---|
| Model 1 | 31 | |||
| Sedentary time | 0.04 (0.03) | 1.49 | 0.15 | |
| Model 2 | 24 | |||
| Sedentary time | 0.08 (0.03) | 2.49 | 0.02 | |
| Model 3 | 24 | |||
| Sedentary time | 0.10 (0.03) | 3.65 | 0.002 | |
| Sample size (n) (≥1000 = 1 vs. <1000) | −0.43 (0.14) | −3.16 | 0.01 | |
| Model 4 (sensitivity analysis 1) | 31 | |||
| Sedentary time | 0.04 (0.02) | 1.91 | 0.07 | |
| Model 5 (sensitivity analysis 2) | 24 | |||
| Sedentary time | 0.08 (0.03) | 3.12 | 0.01 | |
| Model 6 (sensitivity analysis 3) | 24 | |||
| Sedentary time | 0.09 (0.02) | 3.84 | 0.001 | |
| Sample size (n) (≥1000 = 1 vs. <1000) | −0.41 (0.14) | −2.96 | 0.01 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ku, P.-W.; Steptoe, A.; Liao, Y.; Hsueh, M.-C.; Chen, L.-J. A Threshold of Objectively-Assessed Daily Sedentary Time for All-Cause Mortality in Older Adults: A Meta-Regression of Prospective Cohort Studies. J. Clin. Med. 2019, 8, 564. https://doi.org/10.3390/jcm8040564
Ku P-W, Steptoe A, Liao Y, Hsueh M-C, Chen L-J. A Threshold of Objectively-Assessed Daily Sedentary Time for All-Cause Mortality in Older Adults: A Meta-Regression of Prospective Cohort Studies. Journal of Clinical Medicine. 2019; 8(4):564. https://doi.org/10.3390/jcm8040564
Chicago/Turabian StyleKu, Po-Wen, Andrew Steptoe, Yung Liao, Ming-Chun Hsueh, and Li-Jung Chen. 2019. "A Threshold of Objectively-Assessed Daily Sedentary Time for All-Cause Mortality in Older Adults: A Meta-Regression of Prospective Cohort Studies" Journal of Clinical Medicine 8, no. 4: 564. https://doi.org/10.3390/jcm8040564
APA StyleKu, P.-W., Steptoe, A., Liao, Y., Hsueh, M.-C., & Chen, L.-J. (2019). A Threshold of Objectively-Assessed Daily Sedentary Time for All-Cause Mortality in Older Adults: A Meta-Regression of Prospective Cohort Studies. Journal of Clinical Medicine, 8(4), 564. https://doi.org/10.3390/jcm8040564






