The Effects of High- Versus Moderate-Intensity Exercise on Fatigue in Sarcoidosis
Abstract
:1. Introduction
2. Material and Methods
2.1. Study Design and Subjects
2.2. Background Variables
2.3. Exercise Sessions
2.4. Outcome Variables
2.4.1. Fatigue
2.4.2. Other Variables
2.5. Statistical Analyses
3. Results
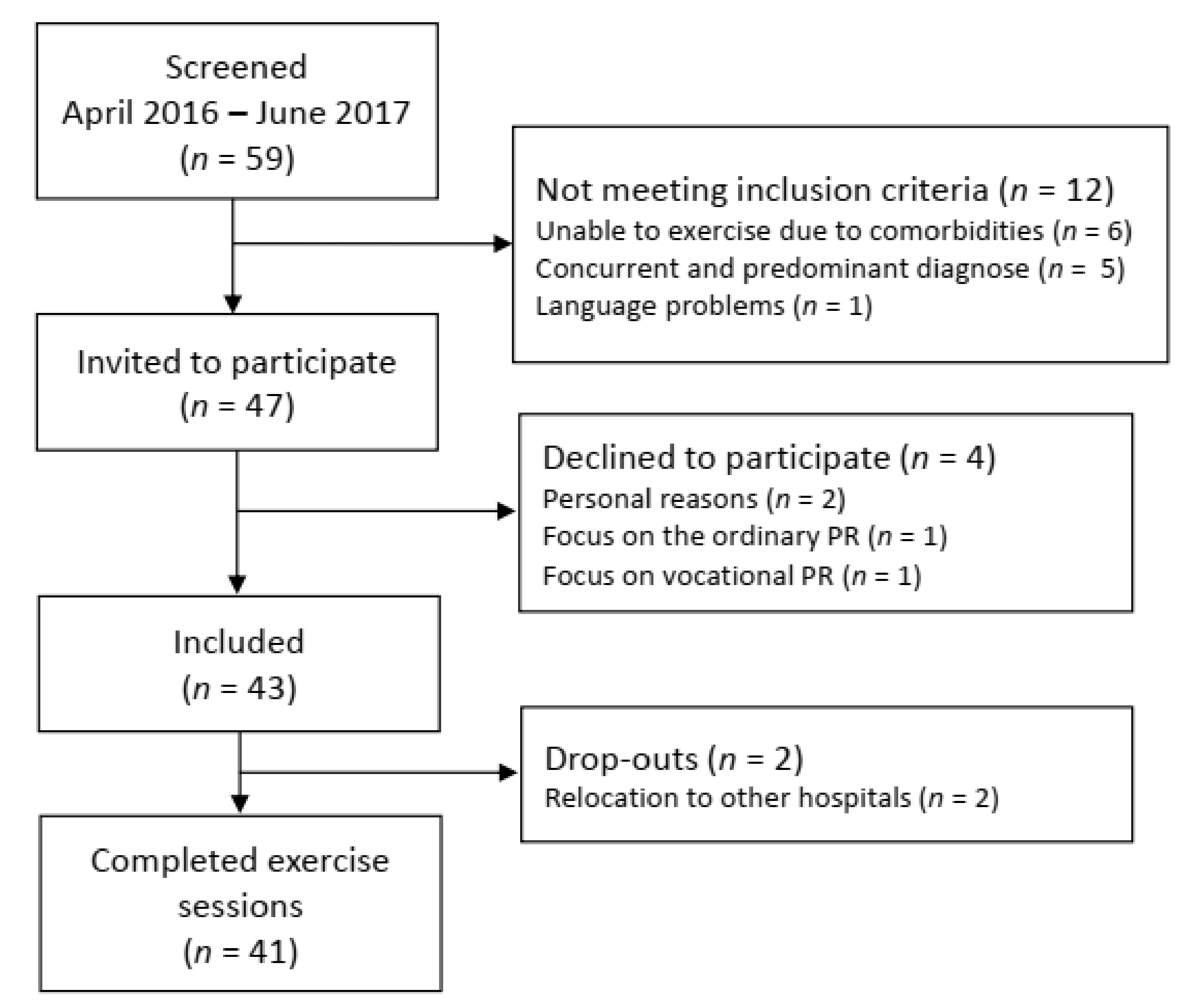
3.1. Flowchart and Baseline Characteristics
3.2. Fatigue
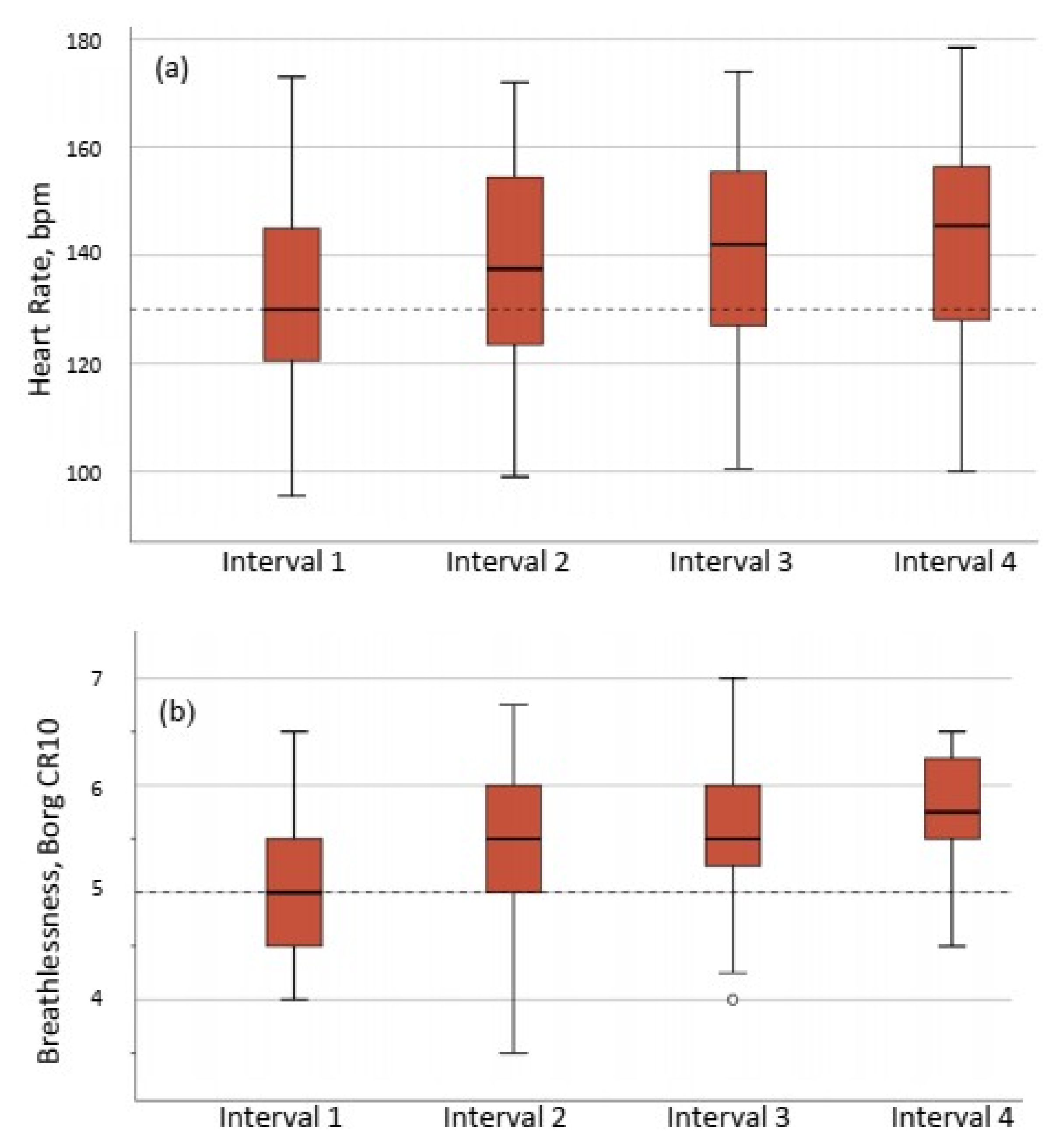
3.3. Feasibility of HIIT
4. Discussion
Strength and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hunninghake, G.W.; Costabel, U.; Ando, M.; Baughman, R.; Cordier, J.F.; du Bois, R.; Eklund, A.; Kitaichi, M.; Lynch, J.; Rizzato, G.; et al. ATS/ERS/WASOG statement on sarcoidosis. American Thoracic Society/European Respiratory Society/World Association of Sarcoidosis and other Granulomatous Disorders. Sarcoidosis Vasc. Diffuse Lung Dis. 1999, 16, 149–173. [Google Scholar]
- De Kleijn, W.P.; De Vries, J.; Lower, E.E.; Elfferich, M.D.; Baughman, R.P.; Drent, M. Fatigue in sarcoidosis: A systematic review. Curr. Opin. Pulm. Med. 2009, 15, 499–506. [Google Scholar] [CrossRef]
- Drent, M.; Lower, E.E.; De Vries, J. Sarcoidosis-associated fatigue. Eur. Respir. J. 2012, 40, 255–263. [Google Scholar] [CrossRef] [Green Version]
- Marcellis, R.G.; Lenssen, A.F.; de Vries, J.; Drent, M. Reduced muscle strength, exercise intolerance and disabling symptoms in sarcoidosis. Curr. Opin. Pulm. Med. 2013, 19, 524–530. [Google Scholar] [CrossRef]
- Strookappe, B.; Swigris, J.; De Vries, J.; Elfferich, M.; Knevel, T.; Drent, M. Benefits of Physical Training in Sarcoidosis. Lung 2015, 193, 701–708. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Strookappe, B.; Elfferich, M.; Swigris, J.; Verschoof, A.; Veschakelen, J.; Knevel, T.; Drent, M. Benefits of physical training in patients with idiopathic or end-stage sarcoidosis-related pulmonary fibrosis: A pilot study. Sarcoidosis Vasc. Diffuse Lung Dis. 2015, 32, 43–52. [Google Scholar] [PubMed]
- Marcellis, R.; Van der Veeke, M.; Mesters, I.; Drent, M.; De Bie, R.; De Vries, G.; Lenssen, A. Does physical training reduce fatigue in sarcoidosis? Sarcoidosis Vasc. Diffuse Lung Dis. 2015, 32, 53–62. [Google Scholar] [PubMed]
- Naz, I.; Ozalevli, S.; Ozkan, S.; Sahin, H. Efficacy of a Structured Exercise Program for Improving Functional Capacity and Quality of Life in Patients with Stage 3 and 4 Sarcoidosis: A RANDOMIZED CONTROLLED TRIAL. J. Cardiopulm. Rehabil. Prev. 2018, 38, 124–130. [Google Scholar] [CrossRef] [PubMed]
- Atkins, C.; Wilson, A.M. Managing fatigue in sarcoidosis—A systematic review of the evidence. Chronic Respir. Dis. 2017, 14, 161–173. [Google Scholar] [CrossRef] [PubMed]
- Gibala, M.J.; Little, J.P.; Macdonald, M.J.; Hawley, J.A. Physiological adaptations to low-volume, high-intensity interval training in health and disease. J. Physiol. 2012, 590, 1077–1084. [Google Scholar] [CrossRef] [Green Version]
- Ramos, J.S.; Dalleck, L.C.; Tjonna, A.E.; Beetham, K.S.; Coombes, J.S. The impact of high-intensity interval training versus moderate-intensity continuous training on vascular function: A systematic review and meta-analysis. Sports Med. 2015, 45, 679–692. [Google Scholar] [CrossRef]
- Hannan, A.L.; Hing, W.; Simas, V.; Climstein, M.; Coombes, J.S.; Jayasinghe, R.; Byrnes, J.; Furness, J. High-intensity interval training versus moderate-intensity continuous training within cardiac rehabilitation: A systematic review and meta-analysis. Open Access J. Sports Med. 2018, 9, 1–17. [Google Scholar] [CrossRef]
- Hussain, S.R.; Macaluso, A.; Pearson, S.J. High-Intensity Interval Training Versus Moderate-Intensity Continuous Training in the Prevention/Management of Cardiovascular Disease. Cardiol. Rev. 2016, 24, 273–281. [Google Scholar] [CrossRef] [Green Version]
- Tomlinson, D.; Diorio, C.; Beyene, J.; Sung, L. Effect of exercise on cancer-related fatigue: A meta-analysis. Am. J. Phys. Med. Rehabil. 2014, 93, 675–686. [Google Scholar] [CrossRef]
- Larun, L.; Brurberg, K.G.; Odgaard-Jensen, J.; Price, J.R. Exercise therapy for chronic fatigue syndrome. Cochrane Database Syst. Rev. 2017, 4, CD003200. [Google Scholar] [CrossRef]
- Sandler, C.X.; Lloyd, A.R.; Barry, B.K. Fatigue Exacerbation by Interval or Continuous Exercise in Chronic Fatigue Syndrome. Med. Sci. Sports Exerc. 2016, 48, 1875–1885. [Google Scholar] [CrossRef]
- Wanger, J.; Clausen, J.L.; Coates, A.; Pedersen, O.F.; Brusasco, V.; Burgos, F.; Casaburi, R.; Crapo, R.; Enright, P.; Van Der Grinten, C.P.M.; et al. Standardisation of the measurement of lung volumes. Eur. Respir. J. 2005, 26, 511–522. [Google Scholar] [CrossRef] [Green Version]
- Quanjer, P.H.; Tammeling, G.J.; Cotes, J.E.; Fabbri, L.M.; Matthys, H.; Pedersen, O.F.; Peslin, R.; Roca, J.; Sterk, P.J.; Ulmer, W.T.; et al. Symbols, abbreviations and units. Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Eur. Respir. J. Suppl. 1993, 16, 85–100. [Google Scholar] [CrossRef]
- Edvardsen, E.; Hansen, B.H.; Holme, I.M.; Dyrstad, S.M.; Anderssen, S.A. Reference values for cardiorespiratory response and fitness on the treadmill in a 20- to 85-year-old population. Chest 2013, 144, 241–248. [Google Scholar] [CrossRef]
- ATS Committee on Proficiency Standards for Clinical Pulmonary Function Laboratories. ATS statement: Guidelines for the six-minute walk test. Am. J. Respir. Crit. Care Med. 2002, 166, 111–117. [Google Scholar] [CrossRef]
- De Vries, J.; Michielsen, H.; Van Heck, G.L.; Drent, M. Measuring fatigue in sarcoidosis: The Fatigue Assessment Scale (FAS). Br. J. Health Psychol. 2004, 9 Pt 3, 279–291. [Google Scholar] [CrossRef] [Green Version]
- Michielsen, H.J.; de Vries, J.; van Heck, G.L.; van de Vijver, F.J.R.; Sijtsma, K. Examination of the dimensionality of fatigue: The construction of the Fatigue Assessment Scale (FAS). Eur. J. Psychol. Assess. 2004, 20, 39–48. [Google Scholar] [CrossRef]
- Borg, G.A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 1982, 14, 377–381. [Google Scholar] [CrossRef] [PubMed]
- Roos, L.; Taube, W.; Beeler, N.; Wyss, T. Validity of sports watches when estimating energy expenditure during running. BMC Sports Sci. Med. Rehabil. 2017, 9, 22. [Google Scholar] [CrossRef] [PubMed]
- Braam, A.W.; de Haan, S.N.; Vorselaars, A.D.; Rijkers, G.T.; Grutters, J.C.; van den Elshout, F.J.; Korenromp, I. Influence of repeated maximal exercise testing on biomarkers and fatigue in sarcoidosis. Brain Behav. Immun. 2013, 33, 57–64. [Google Scholar] [CrossRef] [PubMed]
- Baydur, A.; Alavy, B.; Nawathe, A.; Liu, S.; Louie, S.; Sharma, O.P. Fatigue and plasma cytokine concentrations at rest and during exercise in patients with sarcoidosis. Clin. Respir. J. 2011, 5, 156–164. [Google Scholar] [CrossRef] [PubMed]
- Strookappe, B.; De Vries, J.; Elfferich, M.; Kuijpers, P.; Knevel, T.; Drent, M. Predictors of fatigue in sarcoidosis: The value of exercise testing. Respir. Med. 2016, 116, 49–54. [Google Scholar] [CrossRef] [PubMed]
- Rohekar, G.; Pope, J. Test-retest reliability of patient global assessment and physician global assessment in rheumatoid arthritis. J. Rheumatol. 2009, 36, 2178–2182. [Google Scholar] [CrossRef]
- Yates, H.; Adamali, H.I.; Maskell, N.; Barratt, S.; Sharp, C. Visual analogue scales for interstitial lung disease: A prospective validation study. QJM Mon. J. Assoc. Physicians 2018. [Google Scholar] [CrossRef]
- Wolfe, F.; Michaud, K.; Pincus, T. Preliminary evaluation of a visual analog function scale for use in rheumatoid arthritis. J. Rheumatol. 2005, 32, 1261–1266. [Google Scholar] [PubMed]
- Wells, G.; Li, T.; Maxwell, L.; MacLean, R.; Tugwell, P. Determining the minimal clinically important differences in activity, fatigue, and sleep quality in patients with rheumatoid arthritis. J. Rheumatol. 2007, 34, 280–289. [Google Scholar] [PubMed]
- Allen, J.; Sun, Y.; Woods, J.A. Exercise and the Regulation of Inflammatory Responses. Prog. Mol. Biol. Transl. Sci. 2015, 135, 337–354. [Google Scholar] [CrossRef] [PubMed]
- Strookappe, B.; Saketkoo, L.A.; Elfferich, M.; Holland, A.; De Vries, J.; Knevel, T.; Drent, M. Physical activity and training in sarcoidosis: Review and experience-based recommendations. Expert Rev. Respir. Med. 2016, 10, 1057–1068. [Google Scholar] [CrossRef] [PubMed]
- Garber, C.E.; Blissmer, B.; Deschenes, M.R.; Franklin, B.A.; Lamonte, M.J.; Lee, I.M.; Nieman, D.C.; Swain, D.P. American College of Sports Medicine position stand. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: Guidance for prescribing exercise. Med. Sci. Sports Exerc. 2011, 43, 1334–1359. [Google Scholar] [CrossRef]
- Spruit, M.A.; Thomeer, M.J.; Gosselink, R.; Troosters, T.; Kasran, A.; Debrock, A.J.; Demedts, M.G.; Decramer, M. Skeletal muscle weakness in patients with sarcoidosis and its relationship with exercise intolerance and reduced health status. Thorax 2005, 60, 32–38. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jastrzebski, D.; Ziora, D.; Lubecki, M.; Zieleznik, K.; Maksymiak, M.; Hanzel, J.; Początek, A.; Kolczyńska, A.; Thi, L.N.; Żebrowska, A.; et al. Fatigue in sarcoidosis and exercise tolerance, dyspnea, and quality of life. Adv. Exp. Med. Biol. 2015, 833, 31–36. [Google Scholar] [CrossRef]
- Gibala, M.J.; McGee, S.L. Metabolic adaptations to short-term high-intensity interval training: A little pain for a lot of gain? Exerc. Sport Sci. Rev. 2008, 36, 58–63. [Google Scholar] [CrossRef]
- Bartlett, J.D.; Close, G.L.; MacLaren, D.P.; Gregson, W.; Drust, B.; Morton, J.P. High-intensity interval running is perceived to be more enjoyable than moderate-intensity continuous exercise: Implications for exercise adherence. J. Sports Sci. 2011, 29, 547–553. [Google Scholar] [CrossRef]
- Ungprasert, P.; Wijarnpreecha, K.; Cheungpasitporn, W.; Thongprayoon, C.; Manatsathit, W.; Kroner, P.T. Inpatient Prevalence, Expenditures, and Comorbidities of Sarcoidosis: Nationwide Inpatient Sample 2013–2014. Lung 2019. [Google Scholar] [CrossRef]
- Kostorz, S.; Jastrzebski, D.; Sikora, M.; Zebrowska, A.; Margas, A.; Stepanik, D.; Swinder, H.; Ziora, D. Predominance of Comorbidities in the Detriment of Daily Activity in Sarcoidosis Patients. Adv. Exp. Med. Biol. 2018, 1040, 7–12. [Google Scholar] [CrossRef]
- Rognmo, O.; Hetland, E.; Helgerud, J.; Hoff, J.; Slordahl, S.A. High intensity aerobic interval exercise is superior to moderate intensity exercise for increasing aerobic capacity in patients with coronary artery disease. Eur. J. Cardiovasc. Prev. Rehabil. 2004, 11, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Tjonna, A.E.; Lee, S.J.; Rognmo, O.; Stolen, T.O.; Bye, A.; Haram, P.M.; Loennechen, J.P.; Al-Share, Q.Y.; Skogvoll, E.; Slørdahl, S.A.; et al. Aerobic interval training versus continuous moderate exercise as a treatment for the metabolic syndrome: A pilot study. Circulation 2008, 118, 346–354. [Google Scholar] [CrossRef] [PubMed]
- Wisloff, U.; Stoylen, A.; Loennechen, J.P.; Bruvold, M.; Rognmo, O.; Haram, P.M.; Tjønna, A.E.; Helgerud, J.; Slørdahl, S.A.; Lee, S.J.; et al. Superior cardiovascular effect of aerobic interval training versus moderate continuous training in heart failure patients: A randomized study. Circulation 2007, 115, 3086–3094. [Google Scholar] [CrossRef] [PubMed]
| Characteristics | n = 41 |
|---|---|
| Gender (M/F) | 20/21 |
| Age (years) | 53 (11) |
| BMI (kg/m2) | 30 (6) |
| FVC (% predicted) | 93 (21) |
| FEV1 (% predicted) | 82 (22) |
| TLC (% predicted) | 93 (17) |
| DLCO (% predicted) | 96 (17) |
| VO2peak (mL· kg−1·min−1) | 24.6 (6.8) |
| VO2peak (% predicted) | 72 (19) |
| 6MWD (meter) | 580 (81) |
| Fatigue, FAS (points) | 30 (6) |
| Medication | |
| Prednisolon (n (%)) | 11 (27) |
| Methotrexate (n (%)) | 6 (15) |
| VAS-F | VAS-F from T0 to T1 | VAS-F from T0 to T2 | |||||||
|---|---|---|---|---|---|---|---|---|---|
| T0 | T1 | T2 | Mean Change | ∆ Group Diff. | Mean Change | ∆ Group Diff. | |||
| Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | Mean (SD) | p-Value | Mean (SD) | Mean (SD) | p-Value | |
| HIIT | 22.6 (18.8) | 26.2 (20.7) | 30.9 (21.9) | 3.6 (13.5) | 8.2 (17.0) * | ||||
| MICT | 26.9 (23.7) | 28.3 (21.4) | 29.0 (21.6) | 1.4 (13.5) | 2.2 (14.3) | 0.326 | 2.1 (17.1) | 6.1 (23.8) | 0.106 |
| HIIT n = 41 | MICT n = 41 | p-Value | |
|---|---|---|---|
| Energy expenditure, kcal | 185 (65) | 187 (65) | 0.28 |
| Breathlessness, Borg CR10 | 5.8 (0.6) | 3.1 (0.8) | <0.0001 |
| Heart rate, %HRpeak | 90 (8) | 73 (6) | <0.0001 |
| Blood lactate, mmol·L | 5.8 (2.7) | 2.2 (0.8) | <0.0001 |
| Time, min:s | 26.00 | 37:43 | <0.0001 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grongstad, A.; Vøllestad, N.K.; Oldervoll, L.M.; Spruit, M.A.; Edvardsen, A. The Effects of High- Versus Moderate-Intensity Exercise on Fatigue in Sarcoidosis. J. Clin. Med. 2019, 8, 460. https://doi.org/10.3390/jcm8040460
Grongstad A, Vøllestad NK, Oldervoll LM, Spruit MA, Edvardsen A. The Effects of High- Versus Moderate-Intensity Exercise on Fatigue in Sarcoidosis. Journal of Clinical Medicine. 2019; 8(4):460. https://doi.org/10.3390/jcm8040460
Chicago/Turabian StyleGrongstad, Anita, Nina K. Vøllestad, Line M. Oldervoll, Martijn A. Spruit, and Anne Edvardsen. 2019. "The Effects of High- Versus Moderate-Intensity Exercise on Fatigue in Sarcoidosis" Journal of Clinical Medicine 8, no. 4: 460. https://doi.org/10.3390/jcm8040460
APA StyleGrongstad, A., Vøllestad, N. K., Oldervoll, L. M., Spruit, M. A., & Edvardsen, A. (2019). The Effects of High- Versus Moderate-Intensity Exercise on Fatigue in Sarcoidosis. Journal of Clinical Medicine, 8(4), 460. https://doi.org/10.3390/jcm8040460





