Cardiovascular Health Benefits of Exercise Training in Persons Living with Type 1 Diabetes: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Search Strategy
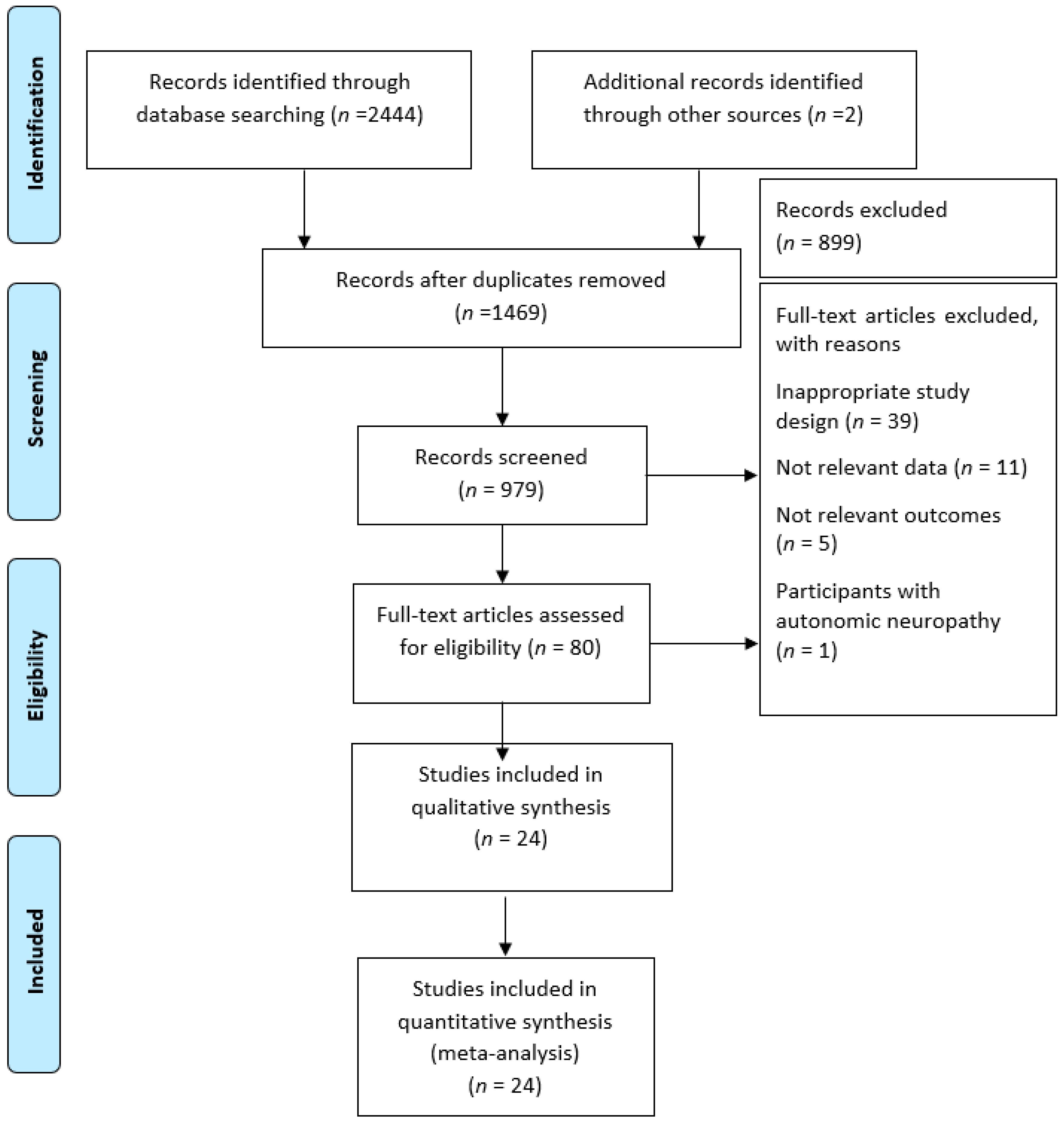
2.2. Study Selection
2.3. Data Extraction and Quality Assessment
2.4. Data Synthesis and Analysis
3. Results
3.1. Study Characteristics
3.2. Participants and Exercise Intervention
3.3. Aerobic Fitness
3.4. Glycemic Control
3.5. Daily Insulin Dosage
3.6. Lipid Profiles
3.7. Body Mass Index, Blood Pressure, and Quality of Life
3.8. Adverse Events
4. Discussion
4.1. Aerobic Fitness
4.2. Glycemic Control
4.3. Daily Insulin Dosage
4.4. Lipid Profiles
4.5. Body Mass Index, Blood Pressure, and Quality of Life
4.6. Adverse Events
4.7. Management Options
4.8. Hyperglycemia, Dyslipidemia, and Obesity
4.9. Comparison with Existing Literature
4.10. Strengths and Limitations
4.11. Future Research
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Mathis, D.; Vence, L.; Benoist, C. Beta-Cell death during progression to diabetes. Nature 2001, 414, 792–798. [Google Scholar] [CrossRef] [PubMed]
- Salem, M.A.; AboElAsrar, M.A.; Elbarbary, N.S.; ElHilaly, R.A.; Refaat, Y.M. Is exercise a therapeutic tool for improvement of cardiovascular risk factors in adolescents with type 1 diabetes mellitus? A randomized controlled trial. Diabetol. Metab. Syndr. 2010, 2, 47. [Google Scholar] [CrossRef] [PubMed]
- International Diabetes Federation Diabetes Atlas. Available online: http://www.diabetesatlas.org/ (accessed on 11 October 2018).
- Snell-Bergeon, J.K.; Nadeau, K. Cardiovascular Disease Risk in Young People with Type 1 Diabetes. J. Cardiovasc. Trans. Res. 2012, 5, 446–462. [Google Scholar] [CrossRef] [PubMed]
- Wadén, J.; Forsblom, C.; Thorn, L.M.; Saraheimo, M.; Rosengård-Bärlund, M.; Heikkilä, O.; Lakka, T.A.; Tikkanen, H.; Groop, P.H.; FinnDiane Study Group. Physical activity and diabetes complications in patients with type 1 diabetes: The Finnish Diabetic Nephropathy (FinnDiane) Study. Diabetes Care 2008, 31, 230–232. [Google Scholar]
- Fuentes-Antras, J.; Picatoste, B.; Gomez-Hernandez, A.; Egido, J.; Tunon, J.; Lorenzo, O. Updating experimental models of diabetic cardiomyopathy. J. Diabetes Res. 2015, 2015, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Gourgari, E.; Dabelea, D.; Rother, K. Modifiable Risk Factors for Cardiovascular Disease in Children with Type 1 Diabetes: Can Early Intervention Prevent Future Cardiovascular Events? Curr. Diabetes Rep. 2017, 17, 134. [Google Scholar] [CrossRef] [PubMed]
- Groop, P.H.; Thomas, M.C.; Moran, J.L.; Wadèn, J.; Thorn, L.M.; Mäkinen, V.P.; Rosengård-Bärlund, M.; Saraheimo, M.; Hietala, K.; Heikkilä, O.; et al. The presence and severity of chronic kidney disease predicts all-cause mortality in type 1 diabetes. Diabetes 2009, 58, 1651–1658. [Google Scholar] [CrossRef]
- Warburton, D.E.; Nicol, C.W.; Bredin, S.S. Health benefits of physical activity: The evidence. CMAJ 2006, 174, 801–809. [Google Scholar] [CrossRef]
- Warburton, D.E.; Bredin, S.S. Health benefits of physical activity: A systematic review of current systematic reviews. Curr. Opin. Cardiol. 2017, 32, 541–556. [Google Scholar] [CrossRef]
- Yardley, J.E.; Kenny, G.P.; Perkins, B.A.; Riddell, M.C.; Balaa, N.; Malcolm, J.; Boulay, P.; Khandwala, F.; Sigal, R.J. Resistance Versus Aerobic Exercise: Acute effects on glycemia in type 1 diabetes. Diabetes Care 2013, 36, 537–542. [Google Scholar] [CrossRef]
- Codella, R.; Terruzzi, I.; Luzi, L. Why should people with type 1 diabetes exercise regularly? Acta Diabetol. 2017, 54, 615–630. [Google Scholar] [CrossRef] [PubMed]
- Warburton, D.E.; Bredin, S.S. Lost in Translation: What Does the Physical Activity and Health Evidence Actually Tell Us? In Lifestyle in Heart Health and Disease; Elsevier: San Diego, CA, USA, 2018; pp. 175–186. [Google Scholar]
- Warburton, D.E.; Bredin, S.S. Reflections on physical activity and health: What should we recommend? Can. J. Cardiol. 2016, 32, 495–504. [Google Scholar] [CrossRef] [PubMed]
- Vanhees, L.; Geladas, N.; Hansen, D.; Kouidi, E.; Niebauer, J.; Reiner, Ž.; Cornelissen, V.; Adamopoulos, S.; Prescott, E.; Börjesson, M. Importance of characteristics and modalities of physical activity and exercise in the management of cardiovascular health in individuals with cardiovascular risk factors: Recommendations from the EACPR (Part II). Eur. J. Prev. Cardiol. 2012, 19, 1005–1033. [Google Scholar] [CrossRef] [PubMed]
- Moy, C.S.; Songer, T.J.; LaPorte, R.E.; Dorman, J.S.; Kriska, A.M.; Orchard, T.J.; Becker, D.J.; Drash, A.L. Insulin-dependent diabetes mellitus, physical activity, and death. Am. J. Epidemiol. 1993, 137, 74–81. [Google Scholar] [CrossRef] [PubMed]
- LaPorte, R.; Dorman, J.; Tajima, N.; Cruickshanks, K.; Orchard, T.; Cavender, D.; Becker, D.; Drash, A. Pittsburgh insulin-dependent diabetes mellitus morbidity and mortality study: Physical activity and diabetic complications. Pediatrics 1986, 78, 1027–1033. [Google Scholar] [PubMed]
- Chudyk, A.; Petrella, R.J. Effects of exercise on cardiovascular risk factors in type 2 diabetes: A meta-analysis. Diabetes Care 2011, 34, 1228–1237. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; Group, P. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef]
- International Prospective Register of Systematic Reviews. Available online: https ://www.crd.york.ac.uk/PROSPERO (accessed on 11 October 2018).
- Current Controlled Trials. Available online: www.controlled-trails.com (accessed on 11 October 2018).
- ClinicalTrials.gov. Available online: www.clinicaltrials.gov (accessed on 11 October 2018).
- PEDro Scare. Available online: https://www.pedro.org.au/ (accessed on 11 October 2018).
- Campaigne, B.N.; Gilliam, T.B.; Spencer, M.L.; Lampman, R.M.; Schork, M.A. Effects of a physical activity program on metabolic control and cardiovascular fitness in children with insulin-dependent diabetes mellitus. Diabetes Care 1984, 7, 57–62. [Google Scholar] [CrossRef]
- Gusso, S.; Pinto, T.; Baldi, J.C.; Derraik, J.G.B.; Cutfield, W.S.; Hornung, T.; Hofman, P.L. Exercise Training Improves but Does Not Normalize Left Ventricular Systolic and Diastolic Function in Adolescents with Type 1 Diabetes. Diabetes Care 2017, 40, 1264–1272. [Google Scholar] [CrossRef]
- Aouadi, R.; Khalifa, R.; Aouidet, A.; Ben Mansour, A.; Ben Rayana, M.; Mdini, F.; Bahri, S.; Stratton, G. Aerobic training programs and glycemic control in diabetic children in relation to exercise frequency. J. Sports Med. Phys. Fitness 2011, 51, 393–400. [Google Scholar]
- Brazeau, A.S.; Gingras, V.; Leroux, C.; Suppere, C.; Mircescu, H.; Desjardins, K.; Briand, P.; Ekoe, J.M.; Rabasa-Lhoret, R. A pilot program for physical exercise promotion in adults with type 1 diabetes: The PEP-1 program. Appl. Physiol. Nutr. Metab. 2014, 39, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Campaigne, B.N.; Landt, K.W.; Mellies, M.J.; James, F.W.; Glueck, C.J.; Sperling, M.A. The Effects of Physical Training on Blood Lipid Profiles in Adolescents with Insulin-Dependent Diabetes Mellitus. Phys. Sportsmed. 1985, 13, 83–89. [Google Scholar] [CrossRef] [PubMed]
- D’hooge, R.; Hellinckx, T.; Van Laethem, C.; Stegen, S.; De Schepper, J.; Van Aken, S.; Dewolf, D.; Calders, P. Influence of combined aerobic and resistance training on metabolic control, cardiovascular fitness and quality of life in adolescents with type 1 diabetes: A randomized controlled trial. Clin. Rehabil. 2011, 25, 349–359. [Google Scholar] [CrossRef] [PubMed]
- Dahl-Jørgensen, K.; Meen, H.D.; Hanssen, K.F.; Aagenaes, O. The effect of exercise on diabetic control and hemoglobin A1 (HbA1) in children. Acta Paediatr. Scand. Suppl. 1980, 283, 53–56. [Google Scholar] [CrossRef] [PubMed]
- Durak, E.P.; Jovanovic-Peterson, L.; Peterson, C.M. Randomized crossover study of effect of resistance training on glycemic control, muscular strength, and cholesterol in type I diabetic men. Diabetes Care 1990, 13, 1039–1043. [Google Scholar] [CrossRef] [PubMed]
- Fuchsjager-Mayrl, G.; Pleiner, J.; Wiesinger, G.F.; Sieder, A.E.; Quittan, M.; Nuhr, M.J.; Francesconi, C.; Seit, H.P.; Francesconi, M.; Schmetterer, L.; et al. Exercise training improves vascular endothelial function in patients with type 1 diabetes. Diabetes Care 2002, 25, 1795–1801. [Google Scholar] [CrossRef] [PubMed]
- Heyman, E.; Toutain, C.; Delamarche, P.; Berthon, P.; Briard, D.; Youssef, H.; Dekerdanet, M.; Gratas-Delamarche, A. Exercise training and cardiovascular risk factors in type 1 diabetic adolescent girls. Pediatr. Exerc. Sci. 2007, 19, 408–419. [Google Scholar] [CrossRef]
- Huttunen, N.P.; Lankela, S.L.; Knip, M.; Lautala, P.; Kaar, M.L.; Laasonen, K.; Puukka, R. Effect of once-a-week training program on physical fitness and metabolic control in children with IDDM. Diabetes Care 1989, 12, 737–740. [Google Scholar] [CrossRef]
- Laaksonen, D.E.; Atalay, M.; Niskanen, L.K.; Mustonen, J.; Sen, C.K.; Lakka, T.A.; Uusitupa, M.I. Aerobic exercise and the lipid profile in type 1 diabetic men: A randomized controlled trial. Med. Sci. Sports Exerc. 2000, 32, 1541–1548. [Google Scholar] [CrossRef]
- Landt, K.W.; Campaigne, B.N.; James, F.W.; Sperling, M.A. Effects of exercise training on insulin sensitivity in adolescents with type I diabetes. Diabetes Care 1985, 8, 461–465. [Google Scholar] [CrossRef]
- Maggio, A.B.; Rizzoli, R.R.; Marchand, L.M.; Ferrari, S.; Beghetti, M.; Farpour-Lambert, N.J. Physical activity increases bone mineral density in children with type 1 diabetes. Med. Sci. Sports Exerc. 2012, 44, 1206–1211. [Google Scholar] [CrossRef] [PubMed]
- Newton, K.H.; Wiltshire, E.J.; Elley, C.R. Pedometers and text messaging to increase physical activity: Randomized controlled trial of adolescents with type 1 diabetes. Diabetes Care 2009, 32, 813–815. [Google Scholar] [CrossRef] [PubMed]
- Perry, T.L.; Mann, J.I.; Lewis-Barned, N.J.; Duncan, A.W.; Waldron, M.A.; Thompson, C. Lifestyle intervention in people with insulin-dependent diabetes mellitus (IDDM). Eur. J. Clin. Nutr. 1997, 51, 757–763. [Google Scholar] [CrossRef] [PubMed]
- Roberts, L.; Jones, T.; Fournier, P. Exercise training and glycemic control in adolescents with poorly controlled type 1 diabetes mellitus. J. Pediatr. Endocrinol. Metab. 2002, 15, 621–627. [Google Scholar] [CrossRef] [PubMed]
- Rowland, T.W.; Swadba, L.A.; Biggs, D.E.; Burke, E.J.; Reiter, E.O. Glycemic control with physical training in insulin-dependent diabetes mellitus. Am. J. Dis. Child. 1985, 139, 307–310. [Google Scholar] [CrossRef] [PubMed]
- Stratton, R.; Wilson, D.P.; Endres, R.K.; Goldstein, D.E. Improved glycemic control after supervised 8-wk exercise program in insulin-dependent diabetic adolescents. Diabetes Care 1987, 10, 589–593. [Google Scholar] [CrossRef] [PubMed]
- Tunar, M.; Ozen, S.; Goksen, D.; Asar, G.; Bediz, C.S.; Darcan, S. The effects of Pilates on metabolic control and physical performance in adolescents with type 1 diabetes mellitus. J. Diabetes Complic. 2012, 26, 348–351. [Google Scholar] [CrossRef]
- Wallberg-Henriksson, H.; Gunnarsson, R.; Rössner, S.; Wahren, J. Long-term physical training in female type 1 (insulin-dependent) diabetic patients: Absence of significant effect on glycaemic control and lipoprotein levels. Diabetologia 1986, 29, 53–57. [Google Scholar] [CrossRef]
- Wong, C.H.; Chiang, Y.C.; Wai, J.P.; Lo, F.S.; Yeh, C.H.; Chung, S.C.; Chang, C.W. Effects of a home-based aerobic exercise programme in children with type 1 diabetes mellitus. J. Clin. Nurs. 2011, 20, 681–691. [Google Scholar] [CrossRef]
- Yki-Järvinen, H.; DeFronzo, R.A.; Koivisto, V.A. Normalization of insulin sensitivity in type I diabetic subjects by physical training during insulin pump therapy. Diabetes Care 1984, 7, 520–527. [Google Scholar] [CrossRef]
- Al Khalifah, R.; Suppère, C.; Haidar, A.; Rabasa-Lhoret, R.; Ladouceur, M.; Legault, L. Association of aerobic fitness level with exercise-induced hypoglycaemia in Type 1 diabetes. Diabet. Med. 2016, 33, 1686–1690. [Google Scholar] [CrossRef] [PubMed]
- Martin, B.-J.; Arena, R.; Haykowsky, M.; Hauer, T.; Austford, L.D.; Knudtson, M.; Aggarwal, S.; Stone, J.A. Cardiovascular Fitness and Mortality after Contemporary Cardiac Rehabilitation. Mayo Clin. Proc. 2013, 88, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Kokkinos, P.; Myers, J.; Faselis, C.; Panagiotakos, D.B.; Doumas, M.; Pittaras, A.; Manolis, A.; Kokkinos, J.P.; Karasik, P.; Greenberg, M. Exercise capacity and mortality in older men: A 20-year follow-up study. Circulation 2010, 122, 790–797. [Google Scholar] [CrossRef] [PubMed]
- Eijsvogels, T.M.; Molossi, S.; Lee, D.-c.; Emery, M.S.; Thompson, P.D. Exercise at the extremes: The amount of exercise to reduce cardiovascular events. J. Am. Coll. Cardiol. 2016, 67, 316–329. [Google Scholar] [CrossRef] [PubMed]
- Nathan, D.M.; Cleary, P.A.; Backlund, J.Y.; Genuth, S.M.; Lachin, J.M.; Orchard, T.J.; Raskin, P.; Zinman, B.; Diabetes Control and Complications Trial/Epidemiology of Diabetes Interventions and Complications (DCCT/EDIC) Study Research Group. Intensive diabetes treatment and cardiovascular disease in patients with type 1 diabetes. N. Engl. J. Med. 2005, 353, 2643–2653. [Google Scholar] [PubMed]
- Maahs, D.M.; Daniels, S.R.; de Ferranti, S.D.; Dichek, H.L.; Flynn, J.; Goldstein, B.I.; Kelly, A.S.; Nadeau, K.J.; Martyn-Nemeth, F.; Osganian, S.K.; et al. Cardiovascular disease risk factors in youth with diabetes mellitus: A scientific statement from the American Heart Association. Circulation 2014, 130, 1532–1558. [Google Scholar] [CrossRef] [PubMed]
- Haskell, W.L.; Lee, I.-M.; Pate, R.R.; Powell, K.E.; Blair, S.N.; Franklin, B.A.; Macera, C.A.; Heath, G.W.; Thompson, P.D.; Bauman, A. Physical activity and public health: Updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Circulation 2007, 116, 1081. [Google Scholar] [CrossRef] [PubMed]
- Minges, K.E.; Whittemore, R.; Weinzimer, S.A.; Irwin, M.L.; Redeker, N.S.; Grey, M. Correlates of overweight and obesity in 5529 adolescents with type 1 diabetes: The T1D Exchange Clinic Registry. Diabetes Res. Clin. Pract. 2017, 126, 68–78. [Google Scholar] [CrossRef]
- Nørgaard, K.; Feldt-Rasmussen, B.; Borch-Johnsen, K.; Saelan, H.; Deckert, T. Prevalence of hypertension in type 1 (insulin-dependent) diabetes mellitus. Diabetologia 1990, 33, 407–410. [Google Scholar] [CrossRef]
- Whelton, S.P.; Chin, A.; Xin, X.; He, J. Effect of aerobic exercise on blood pressure: A meta-analysis of randomized, controlled trials. Ann. Intern. Med. 2002, 136, 493–503. [Google Scholar] [CrossRef]
- Lima, L.C.; Assis, G.V.; Hiyane, W.; Almeida, W.S.; Arsa, G.; Baldissera, V.; Campbell, C.S.; Simões, H.G. Hypotensive effects of exercise performed around anaerobic threshold in type 2 diabetic patients. Diabetes Res. Clin. Pract. 2008, 81, 216–222. [Google Scholar] [CrossRef] [PubMed]
- Kalyva, E.; Malakonaki, E.; Eiser, C.; Mamoulakis, D. Health-related quality of life (HRQoL) of children with type 1 diabetes mellitus (T1DM): Self and parental perceptions. Pediatr. Diabetes 2011, 12, 34–40. [Google Scholar] [CrossRef] [PubMed]
- Cai, H.; Li, G.; Zhang, P.; Xu, D.; Chen, L. Effect of exercise on the quality of life in type 2 diabetes mellitus: A systematic review. Qual. Life Res. 2017, 26, 515–530. [Google Scholar] [CrossRef] [PubMed]
- Riddell, M.C.; Gallen, I.W.; Smart, C.E.; Taplin, C.E.; Adolfsson, P.; Lumb, A.N.; Kowalski, A.; Rabasa-Lhoret, R.; McCrimmon, R.J.; Hume, C. Exercise management in type 1 diabetes: A consensus statement. Lancet Diabetes Endocrinol. 2017, 5, 377–390. [Google Scholar] [CrossRef]
- Khunti, K.; Davies, M.; Majeed, A.; Thorsted, B.L.; Wolden, M.L.; Paul, S.K. Hypoglycemia and risk of cardiovascular disease and all-cause mortality in insulin-treated people with type 1 and type 2 diabetes: A cohort study. Diabetes Care 2015, 38, 316–322. [Google Scholar] [CrossRef] [PubMed]
- Desouza, C.V.; Bolli, G.B.; Fonseca, V. Hypoglycemia, diabetes, and cardiovascular events. Diabetes Care 2010, 33, 1389–1394. [Google Scholar] [CrossRef] [PubMed]
- Zoungas, S.; Patel, A.; Chalmers, J.; De Galan, B.E.; Li, Q.; Billot, L.; Woodward, M.; Ninomiya, T.; Neal, B.; MacMahon, S. Severe hypoglycemia and risks of vascular events and death. N. Engl. J. Med. 2010, 363, 1410–1418. [Google Scholar] [CrossRef]
- Giménez, M.; López, J.J.; Castell, C.; Conget, I. Hypoglycaemia and cardiovascular disease in Type 1 Diabetes. Results from the Catalan National Public Health registry on insulin pump therapy. Diabetes Res. Clin. Pract. 2012, 96, e23–e25. [Google Scholar] [CrossRef]
- Johnson, S.; Cooper, M.; Davis, E.; Jones, T. Hypoglycaemia, fear of hypoglycaemia and quality of life in children with Type 1 diabetes and their parents. Diabet. Med. 2013, 30, 1126–1131. [Google Scholar] [CrossRef]
- Kacerovsky, M.; Jones, J.; Schmid, A.I.; Barosa, C.; Lettner, A.; Kacerovsky-Bielesz, G.; Szendroedi, J.; Chmelik, M.; Nowotny, P.; Chandramouli, V. Postprandial and fasting hepatic glucose fluxes in longstanding type 1 diabetes. Diabetes 2011, 60, 1752–1758. [Google Scholar] [CrossRef]
- Yardley, J.E.; Iscoe, K.E.; Sigal, R.J.; Kenny, G.P.; Perkins, B.A.; Riddell, M.C. Insulin pump therapy is associated with less post-exercise hyperglycemia than multiple daily injections: An observational study of physically active type 1 diabetes patients. Diabetes Technol. Ther. 2013, 15, 84–88. [Google Scholar] [CrossRef] [PubMed]
- Skyler, J.S.; Bergenstal, R.; Bonow, R.O.; Buse, J.; Deedwania, P.; Gale, E.A.; Howard, B.V.; Kirkman, M.S.; Kosiborod, M.; Reaven, P. Intensive glycemic control and the prevention of cardiovascular events: Implications of the ACCORD, ADVANCE, and VA diabetes trials: A position statement of the American Diabetes Association and a scientific statement of the American College of Cardiology Foundation and the American Heart Association. J. Am. Coll. Cardiol. 2009, 53, 298–304. [Google Scholar]
- Haffner, S.M. Dyslipidemia management in adults with diabetes. Diabetes Care 2004, 27, S68. [Google Scholar] [CrossRef]
- Gruberg, L.; Weissman, N.J.; Waksman, R.; Fuchs, S.; Deible, R.; Pinnow, E.E.; Ahmed, L.M.; Kent, K.M.; Pichard, A.D.; Suddath, W.O.; et al. The impact of obesity on the short-term and long-term outcomes after percutaneous coronary intervention: The obesity paradox? J. Am. Coll. Cardiol. 2002, 39, 578–584. [Google Scholar] [CrossRef]
- Iliodromiti, S.; Celis-Morales, C.A.; Lyall, D.M.; Anderson, J.; Gray, S.R.; Mackay, D.F.; Nelson, S.M.; Welsh, P.; Pell, J.P.; Gill, J.M. The impact of confounding on the associations of different adiposity measures with the incidence of cardiovascular disease: A cohort study of 296 535 adults of white European descent. Eur. Heart J. 2018, 39, 1514–1520. [Google Scholar] [CrossRef] [PubMed]
- Quirk, H.; Blake, H.; Tennyson, R.; Randell, T.L.; Glazebrook, C. Physical activity interventions in children and young people with Type 1 diabetes mellitus: A systematic review with meta-analysis. Diabet. Med. 2014, 31, 1163–1173. [Google Scholar] [CrossRef] [PubMed]
- MacMillan, F.; Kirk, A.; Mutrie, N.; Matthews, L.; Robertson, K.; Saunders, D.H. A systematic review of physical activity and sedentary behavior intervention studies in youth with type 1 diabetes: Study characteristics, intervention design, and efficacy. Pediatr. Diabetes 2014, 15, 175–189. [Google Scholar] [CrossRef]
- Tonoli, C.; Heyman, E.; Roelands, B.; Buyse, L.; Cheung, S.S.; Berthoin, S.; Meeusen, R. Effects of different types of acute and chronic (training) exercise on glycaemic control in type 1 diabetes mellitus. Sports Med. 2012, 42, 1059–1080. [Google Scholar] [CrossRef]
- Kennedy, A.; Nirantharakumar, K.; Chimen, M.; Pang, T.T.; Hemming, K.; Andrews, R.C.; Narendran, P. Does exercise improve glycaemic control in type 1 diabetes? A systematic review and meta-analysis. PLoS ONE 2013, 8, e58861. [Google Scholar] [CrossRef]
- Ostman, C.; Jewiss, D.; King, N.; Smart, N. Clinical outcomes to exercise training in type 1 diabetes: A systematic review and meta-analysis. Diabetes Res. Clin. Pract. 2018, 139, 380–391. [Google Scholar] [CrossRef]
| Study, Year (Ref.) | Participants (Age, Simple Size, Diabetes Duration) | Intervention | Outcome Measures | PEDro Score | |||
|---|---|---|---|---|---|---|---|
| N | Mean Age ± SD/Age Range (Years) | Duration of T1D (Years) | (Exercise Frequency, Intensity, Type of Exercise, Time Duration per Session) | Program Duration | |||
| Aouadi et al. 2011 a [26] | EG: 11 CG: 11 | EG: 12.2 ± 1.5; CG: 12.9 ± 1.3 | EG: 3.6 ± 0.8; CG: 3.2 ± 0.54 | EG: 2×/week, 50–55% HRmax at weeks 1–2; 55–60% HRmax at weeks 3–4; 60–65% HRmax at weeks 5–24; 10–15 min WU and CD + 40–50 min aerobic exercise CG: continued with normal PA behavior | 24 weeks | BMI  in both groups in both groups HDL-C ↑ significantly in EG Triglyceride ↓ significantly in EG Daily insulin dosage ↓ in EG | 6 |
| Aouadi et al. 2011 b [26] | EG: 11 CG: 11 | EG: 13.5 ± 0.8; CG: 12.9 ± 1.3 | EG: 4.1 ± 1.3; CG: 3.2 ± 0.54 | EG: 4×/week, 50–55% HRmax at weeks 1–2; 55–60% HRmax at weeks 3–4; 60–65% HRmax at weeks 5–24; 10–15 min WU and CD + 40–50 min aerobic exercise CG: continued with normal PA behavior | 24 weeks | BMI  in EG, CG in EG, CG HbA1c ↓ significantly in EG HDL-C ↑ significantly in EG Triglycerides ↓ significantly in EG LDL-C ↓ significantly in EG Daily insulin dosage ↓ in EG | 6 |
| Brazeau et al. 2014 [27] | EG: 23 (12 F; 11 M) CG: 25 (14 F; 11 M) | EG: 45.1 ± 14.5; CG: 44.2 ± 12.5 | EG: 20.3 ± 12.9; CG: 24.4 ± 13.6 | EG: leaflet on PA promotion with exercise 1×/week, 60 min of various activities (endurance, resistance, flexibility) + 30 min of counselling (PA and introduced glycemic management related to PA) CG: received leaflet on PA promotion and carried out normal PA | 12 weeks | Weight ↓ significantly in EG BMI  in both groups in both groups HbA1c  in both groups in both groups VO2peak ↑ significantly in EG SBP ↓ significantly in EG DBP ↓ significantly in EG | 7 |
| Campaigne et al. 1984 [24] | EG: 9 CG: 10 | EG: 9.0 ± 0.47 (SEM); CG: 8.5 ± 0.57 (SEM) | EG: 5.1 ± 0.95 (SEM); CG: 3.89 ± 0.70 (SEM) | EG: 3×/week, HR ≥ 160 bpm, 30 min of vigorous exercise (running, movement to music), supervised aerobic exercise CG: continued with normal PA behavior | 12 weeks | Weight ↑ significantly in EG Weight ↑ in CG FBG ↓ significantly in EG, significantly lower than CG HbA1c ↓ significantly in EG, significantly lower than CG Daily insulin dosage  in both groups in both groups VO2peak ↑ significantly in EG | 5 |
| Campaigne et al. 1985 [28] | EG: 9 (6 F; 3 M) CG: 5 (3 M; 2 F) | EG: 16.0 ± 1 (SEM); CG: 15 ± 0.4 (SEM) | EG: 6.6 ± 1.1 (SEM); CG: 6.2 ± 1.1 (SEM); | EG: 3×/week, HR > 160 bpm intensity, 10 min WU + 25 min aerobic movement to music + 10 min CD, supervised aerobic exercise CG: continued with normal PA behavior | 12 weeks | Weight  in both groups in both groups Lean body mass ↑ in EG,  in CG in CG VO2peak ↑ significantly in EG,  in CG in CG LDL-C ↓ significantly in EG,  in CG in CG Total cholesterol, triglyceride, HDL-C  in both groups in both groups HbA1  in both groups in both groups Daily insulin dosage  in both groups in both groups | 5 |
| D’ hooge et al. 2011 [29] | EG: 8 CG: 8 | EG: 14.1 (10.1–16.8); CG: 13.2 (10.1–15.3) | EG: 5.4 (3.4–7.3); CG: 5.3 (2.9–5.9) | EG: 2×/week, 60% HRR increased to 70% HRR after 6 weeks, 75% HRR after 12 weeks; 5 min WU + 30 min strength training (upper limbs, lower limbs, and abdominal muscles, 10 min each) + 30 min aerobic training (cycling, running and stepping, 10 min each) + 5 min CD. Strength training: first 12 sessions: 2 sets of 15 reps at 20 RM; next 12 sessions: 2 sets of 12 reps at 17 RM; final 8 weeks: 3 sets of 10 reps at 12 RM; 60 s rest between 2 sets; supervised aerobic exercise and strength training CG: normal activity | 20 weeks | Weight  in both groups in both groups BMI  in both groups in both groups VO2peak  in both groups in both groups Muscle fatigue score, number of sit to stand, upper and lower limb strength, 6 min walking distance ↑ significantly in EG HbA1c  in both groups in both groups FBG  in both groups in both groups Daily insulin dosage ↓ significantly in EG,  in CG in CG Quality of life (SF-36)  in both groups in both groups | 7 |
| Dahl-Jorgensen et al. 1980 [30] | EG: 14 CG: 8 | 9–15 | 5 | EG: 2×/week, 60 min; supervised exercise; and supplemented by a weekly home exercise experience CG: did not participate in any standardized exercise regime | 20 weeks | VO2peak  in both groups in both groups Daily insulin dosage  in both groups in both groups HbA1c ↓ significantly in EG,  in CG in CG | 5 |
| Durak et al. 1990(crossover) [31] | EG: 8 CG: 8 | EG: 31 ± 3.5 CG: 31 ± 3.5 | EG: 12.3 ± 9.8 CG: 12.3 ± 9.8 | EG: 3×/week, 6 upper-body exercises and 4 lower-body exercises (maximum 12 reps), 3–7 sets, total 40–50 sets, rest interval: 30 s–2 min; 60 min, supervised heavy resistance training concentrating on the strengthening of major muscle groups CG: rest | 10 weeks | HbA1c ↓ significantly in EG Total cholesterol ↓ significantly in EG Blood glucose ↓ significantly in EG Triglyceride, LDL-C ↓ in EG HDL-C  in EG in EG Weight  in both in both Strength, endurance ↑ significantly in EG | 2 |
| Fuchsjager-Maryle et al. 2002 [32] | EG: 18 (11 F; 7 M) CG: 8 (3 F; 5 M) | EG: 42 ± 10; CG: 33 ± 11 | EG: 20 ± 10; CG: 20 ± 10 | EG: 2×/week at weeks 1–2; 3×/week at weeks 3–16; stationary cycling with increasing resistance till 60–70% HR; 3–5 min WU + 40 min + 5 min CD, supervised exercise CG: no training intervention | 16 weeks | Weight  in EG in EG BMI  in EG in EG VO2max ↑ significantly in EG HbA1c, LDL-C, HDL-C, triglycerides  in EG in EG Total cholesterol tended ↓ in EG Daily insulin dosage ↓ significantly in EG Isometric muscle strength of both legs ↑ significantly in EG | 3 |
| Gusso et al. 2017 [25] | EG: 38 CG: 15 | EG: 15.6 ± 1.3; CG: 15.5 ± 0.9 | EG: 5.4 ± 3.4; CG: 7.5 ± 4.0 | EG: 4×/week; (3×aerobic sessions + 1×resistance)/week at weeks 1–12, 4× circuit training/week at weeks 12–20; aerobic exercise: progressively to 85% HRmax at weeks 1–4; 85% HRmax at weeks 5–20; 40 min/session; resistance training: weight training and core exercise; 60 min exercise sessions per week (including WU and CD), supervised exercise CG: no training intervention | 20 weeks | Body weight ↑ significantly in both groups Body fat percentage ↓ in EG, ↑ in CG Fat-free mass ↑ in EG HbA1c  in both groups in both groups VO2peak ↑ in EG DBP (resting) ↓ significantly in EG Daily insulin dosage ↓ in EG | 7 |
| Heyman et al. 2007 [33] | EG: 9 (F) CG: 7 (F) | EG: 15.9 ± 1.5; CG: 16.3 ± 1.2 | EG: 6.3 ± 4.4; CG: 8.4 ± 4.5 | EG: 2×/week; 80–90% of HRR (measured by monitors); one 2-h supervised session + one 1-h unsupervised session, combined aerobic and strength sessions in ratio of 2:1 CG: spent equal amount of time on activities that did not require physical effort | 24 weeks | Body weight ↑ significantly in both groups Fat mass  in EG, tended ↑ in CG in EG, tended ↑ in CG Fat-free mass ↑ significantly in EG,  in CG in CG Daily insulin dosage  in both groups in both groups PWC170 (aerobic fitness) in watts ↑ significantly in EG Total cholesterol, LDL-C, HDL-C, triglycerides  in both groups in both groups Quality of life (DQOL) ↑ in EG | 4 |
| Huttunen et al. 1989 [34] | EG: 16 CG: 16 | EG: 11.9 (8.2–16.9) CG: 11.9 (8.2–16.9) | EG: 4.7 (0.6–12.0); CG: 5.6 (2.0–13.1) | EG: 1×/week, HR >150 bpm, 60 min, aerobic exercise (jogging, running, gymnastics and various kinds of active games) CG: continued with normal PA behavior | 13 weeks | VO2peak ↑ significantly in EG,  in CG in CG HbA1c ↑ significantly in EG | 5 |
| Laaksonen et al. 2000 [35] | EG: 20 CG: 22 | EG: 32.5 ± 5.7; CG: 29.5 ± 6.3 | EG: 13.8 ± 9.2; CG: 10.8 ± 5.8 | EG: 3×/week, 50–60% VO2peak, 20–30 min, at week 1, gradually increased to 4–5×/week, 60–80% VO2peak, 30–60 min at weeks 2–16, aerobic training CG: continued with normal PA behavior | 12–16 weeks | VO2peak ↑ significantly in EG; HbA1c, daily insulin dosage, BMI, body fat percentage  in both groups in both groups Total cholesterol, LDL-C ↓ in EG; HDL-C ↑ in CG; Triglycerides changes significantly greater in EG than CG | 4 |
| Landt et al. 1985 [36] | EG: 9 (6 F; 3 M) CG: 6 (2 F; 4 M) | EG: 16.1 ± 0.8; CG: 15.9 ± 0.3 | EG: 6.7 ± 1.1; CG: 7.7 ± 1.5 | EG: 3×/week, HR ≥160 bpm, 10 min WU + 25 min aerobic movement + 10 min CD, supervised exercise CG: continued with normal PA behavior | 12 weeks | Daily insulin dosage  in both in both VO2max ↑ in EG Lean body mass ↑ in EG Insulin sensitivity ↑ in EG HbA1c  in both groups in both groups | 4 |
| Maggio et al. 2011 [37] | EG: 15 (7 F; 8 M) CG: 12 (7 F: 5M) | EG: 10.5 ± 2.0 CG: 10.5 ± 2.9 | EG: 3.1 ± 2.7 CG: 3.4 ± 1.7 | EG: 2×/week; HR ≥140 bpm, 10 min WU + 10 min drop jump (height of platform from 20 cm for the first 3 months to 40 cm in last 6 months) + 60 min weight-bearing activities + 10 min CD; weight-bearing: ball games, jumping, rope skipping, and gymnastics supervised exercise CG: relatively inactive | 36 weeks | BMI  in both groups in both groups Boy weight  in both groups in both groups | 8 |
| Newton et al. 2009 [38] | EG: 38 (16 F; 22 M) CG: 40 (20 F; 20 M) | EG: 11–18 years CG: 11–18 years | EG: wore open pedometer daily with a goal of 10,000 steps/day and received weekly text messages (reminding them to wear pedometer and be active) CG: received usual care for 12 weeks | 12 weeks | HbA1c  in both groups in both groups SBP  in both groups in both groups DBP  in both groups in both groups BMI Z score  in both groups in both groups Quality of life (SQOL)  in both groups in both groups | 7 | |
| Perry et al. 1997 a 666crossover [39] | EG: 31 CG: 31 | EG: 41.5 ± 11; CG: 41.5 ± 11 | EG: 14.1 ± 11.9; CG: 14.1 ± 11.9 | EG: intensive lifestyle education with ≥3×/week, intensity and duration were based on individual fitness level and goals (walking, cycling, running, weight training); non-supervised and individualized aerobic PA CG: received standard care | 24 weeks | Weight ↓ significantly in EG HbA1 ↓ not significantly in EG Triglycerides, total cholesterol, LDL-C  in EG in EG HDL-C ↑ in EG VO2max ↑ in EG BP  in EG in EG | 5 |
| Perry et al. 1997 b [39] crossover | EG: 30 CG: 30 | EG: 42.8 ± 12.6; CG: 42.8 ± 12.6 | EG: 16.8 ± 13; CG: 16.8 ± 13 | EG: intensive lifestyle education with ≥3×/week, intensity and duration were based on individual fitness level and goals (walking, cycling, running, weight training); non-supervised and individualized aerobic PA CG: received standard care | 24 weeks | HbA1 ↓ not significantly in EG BP  in EG in EG Total, LDL-C ↓ significantly in EG Total, HDL-C  in EG in EG | 5 |
| Roberts et al. 2002 [40] | EG: 12 CG: 12 | 14 ± 1.2 | 5.0 ± 3.1 | EG: 3×/week, 45 min/session, HR ≥ 160 bpm, aerobic and anaerobic component in a ratio of 7:3; activities: running, light training circuits, games and aerobics; supervised exercise CG: unsupervised training | 12 weeks | Aerobic power score ↑ significantly in EG,  in CG in CG HbA1  in both groups in both groups BMI  in both groups in both groups Body mass  in both groups in both groups | 3 |
| Rowland et al. 1985 crossover [41] | EG: 14 CG: 14 | (9–14) | 4.2 (0.5–9.5) | EG: 3×/week, 10 min stretching + 20 min alternating 5-min walking/running increased to 30 min running 60% of HRR (160 bpm) + 5 min CD; recreational swim for 15 min twice weekly CG: rest | 12 weeks | VO2max ↑ in EG HbA1c  in both groups in both groups | 6 |
| Salem et al. 2010 a [2] | EG: 75 CG: 48 | EG: 14.7 ± 2.2; CG: 15 ± 2.35 | EG: 3.6 ± 1.8; CG: 4.9 ± 1.9 | EG: 1×/week, 65 min; supervised exercise (1) Aerobic exercise (cycling/treadmill) at 65–85% HRmax (2) Anaerobic exercise (treadmill interval running at 85–95% HRmax for 1–2 min) (3) Leg extension and leg curl exercises (progressive resistive exercises, 10RM) (4) Different free strength and endurance exercises (10 min, 10 reps/set, number of sets increasing gradually) (5) Flexibility exercises (5 min stretching) (6) Neuromuscular exercises (5 min coordination exercises, 10 reps balance exercise regime on firm surface for 10 min, 10 reps which increased from 1 set to 3 sets after 6 sessions. CG: continued with normal PA behavior | 24 weeks | HbA1c ↓ significantly in EG BMI (SDS) ↓ significantly in EG,  in CG in CG Daily insulin dosage ↓ significantly in EG HDL-C ↑ significantly in EG,  in CG in CG Triglycerides, total cholesterol, LDL-C ↓ in EG | 4 |
| Salem et al. 2010 b [2] | EG: 73 CG: 48 | EG: 14.5 ± 2.4; CG: 15 ± 2.35 | EG: 5.5 ± 2; CG: 4.9 ± 1.9 | EG: 3×/week, 65 min; supervised exercise (1) Aerobic exercise (cycling/treadmill) at 65–85% HRmax (2) Anaerobic exercise (treadmill interval running at 85–95% HRmax for 1–2 min) (3) Leg extension and leg curl exercises (progressive resistive exercises, 10RM) (4) Different free strength and endurance exercises (10 min, 10 reps/set, number of sets increasing gradually) (5) Flexibility exercises (5 min stretching) (6) Neuromuscular exercises (5 min coordination exercises, 10 reps balance exercise regime on firm surface for 10 min, 10 reps which increased from 1 set to 3 sets after 6 sessions. CG: continued with normal PA behavior | 24 weeks | HbA1c ↓ significantly in EG Daily insulin dosage ↓ in EG BMI (SDS) ↓ significantly in EG,  in CG in CG DBP percentile ↓ in EG Triglycerides, total cholesterol, LDL-C HDL-C ↑ significantly in EG,  in CG in CG | 4 |
| Stratton et al. 1987 [42] | EG: 8 (4 F; 4 M) CG: 8 | EG: 15.1 ± 1.2 CG: 15.5 ± 0.9 | EG: 3.7 ± 2.1; CG: 5.5 ± 3.3 | EG: 3×/week, 30–45 min of supervised highly aerobic activities (treadmill jogging, cycle ergometer) on 2 of the 3 days; on 1 of the 3 days, activities: basketball, swimming, or resistance exercise machines (mostly aerobic); diet advice once a week, supervised exercise CG: were encouraged to exercise and given an outline exercise program | 8 weeks | Daily insulin dosage ↓ in EG Bruce treadmill time, submaximal exercise heart rates ↑ in EG HbA1c, total cholesterol, triglycerides, HDL-C  in both groups in both groups | 6 |
| Tunar et al. 2012 [43] | EG: 17 (11 F; 6 M) CG: 14 (5 F; 9 M) | EG: 14.2 ± 2.2; CG: 14.3 ± 1.8 | EG: 5.3 ± 4.1; CG: 6 ± 4.2 | EG: 3×/week, 45 min, mat-based Pilates CG: continued with normal PA behavior | 12 weeks | BMI SDS  in both groups in both groups HbA1c, daily insulin dosage  in both groups in both groups HDL-C ↑ in CG LDL-C, total cholesterol, triglycerides  in both groups in both groups Peak power, mean power, flexibility, vertical jump ↑ significantly in EG | 5 |
| Wallberg-Henriksson et al. 1986 [44] | EG: 6 (F) CG: 7 (F) | EG: 36 ± 2 (SEM); CG: 35 ± 2 (SEM); | EG: 14 ± 4 (SEM); CG: 13 ± 2 (SEM) | EG: 7×/week, 5 min low intensity WU + 15 min high intensity cycling at 60–70% VO2max for first month, 70–80% VO2max for the second and third month, 75–90% VO2max for last 2 months) CG: continued with normal PA behavior | 20 weeks | VO2max ↑ significantly in EG HbA1c  in both groups in both groups Total cholesterol ↓ in both groups LDL-C, total triglycerides, blood glucose, HDL-C  in both groups in both groups | 4 |
| Wong et al. 2011 [45] | Home-based EG: 12 Self-directed EG: 5CG:11 | Home-based EG: 11.62 ± 2.12; Self-directed EG: 13.44 ± 2.23 CG: 12.77 ± 1.79 | Home-based EG: 4.42 ± 2.58; Self-directed EG: 3.42 ± 3.48; CG: 3.82 ± 2.87 | Home-based EG: 3×/week, 10–30% HRR during WU and CD; 40–60% HRR during aerobic exercises; 10–20 min at week 1 to 20–30 min at weeks 3–12, delivered via VCR and/or phone; aid compliance and a handbook to provide guidance and exercise log, Self-directed EG: self-directed exercise CG: continued with normal PA behavior | 12 weeks | HbA1c  in home-based EG, self-directed EG, CG at each study point; in home-based EG, self-directed EG, CG at each study point; Self-directed EG had higher HbA1c than home-based EG; CG had higher HbA1c than self-directed EG at 9-month follow-up; VO2peak  in all groups in all groups | 6 |
| Yki-Jarvinen et al. 1984 [46] | EG: 7 (1 F; 6 M) CG: 6 (2 F; 4 M) | EG: 26 ± 1; CG: 24 ± 1 | EG: 7 ± 1; CG: 9 ± 1 | EG: 4×/week, 150–160 bpm, 60 min (4 × 15 min with 5-min rest intervals) CG: sedentary activity | 6 weeks | VO2max ↑ significantly in EG HbA1c  in EG in EG Daily insulin dosage ↓ significantly in EG,  in CG in CG Triglycerides, total cholesterol, HDL-C, LDL-C  | 1 |
 = no changes; a, b data in the study included more than one condition.
= no changes; a, b data in the study included more than one condition.| Outcome | Moderator Variable | Subgroups | No. of Trials | No. of Participants | Pooled Meta-Analysis | Heterogeneity | Subgroup Differences | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean Difference | 95% (Confidence Interval) | p (Overall Effect) | I2 (%) | Chi2 | p | I2 | Chi2 | p | |||||
| Maximal Aerobic Power (mL·kg−1·min−1) | Total | 11 | 303 | 3.01 | (0.94 to 5.07) | <0.01 | 80 | 50.68 | <0.01 | ||||
| Age groups | Children and adolescents | 6 | 161 | 2.98 | (0.96 to 5.00) | <0.01 | 0 | 2.54 | 0.77 | 0.0 | 0.02 | 0.89 | |
| Adults | 5 | 142 | 3.24 | (0.10 to 6.38) | 0.04 | 91 | 46.08 | <0.01 | |||||
| Exercise frequency | ≥3 times/week | 9 | 223 | 4.45 | (3.37 to 5.52) | <0.01 | 0 | 6.48 | 0.59 | 97.7 | 44.01 | <0.01 | |
| <3 times/week | 2 | 80 | −0.17 | (−1.01 to 0.67) | 0.69 | 0 | 0.19 | 0.69 | |||||
| Type of exercise | Aerobic exercise | 9 | 202 | 4.25 | (3.16 to 5.34) | <0.01 | 0 | 7.36 | 0.50 | 0.0 | 0.43 | 0.51 | |
| Combined aerobic and resistance training | 2 | 101 | 2.32 | (−3.36 to 8.00) | 0.42 | 85 | 6.68 | 0.01 | |||||
| Program duration | >12 weeks | 4 | 134 | 5.05 | (3.81 to 6.29) | <0.01 | 0 | 2.22 | 0.53 | 96.7 | 30.44 | <0.01 | |
| ≤12 weeks | 7 | 169 | 0.48 | (−0.37 to 1.53) | 0.37 | 5 | 6.34 | 0.39 | |||||
| HbA1c (%) | Total | 24 | 862 | −0.45 | (−0.73 to −0.17) | <0.01 | 76 | 97.69 | <0.01 | ||||
| Age groups | Children and adolescents | 17 | 595 | −0.60 | (−1.07 to −0.14) | 0.01 | 74 | 61.03 | <0.01 | 72.4 | 3.62 | 0.06 | |
| Adults | 7 | 267 | −0.10 | (−0.33 to 0.13) | 0.40 | 54 | 13.06 | 0.04 | |||||
| Exercise frequency | ≥3 times/week | 16 | 561 | −0.53 | (−0.88 to −0.17) | <0.01 | 69 | 47.64 | <0.01 | 0 | 0.27 | 0.60 | |
| <3 times/week | 8 | 301 | −0.34 | (−0.93 to 0.24) | 0.25 | 85 | 46.91 | <0.01 | |||||
| Type of exercise | Aerobic exercise | 14 | 316 | −0.39 | (−0.84 to 0.06) | 0.09 | 74 | 50.36 | <0.01 | 0 | 2.29 | 0.51 | |
| Combined aerobic and resistance training | 8 | 499 | −0.56 | (−1.05 to −0.08) | 0.02 | 84 | 43.66 | <0.01 | |||||
| Resistance training | 1 | 16 | −1.10 | (−2.25 to 0.05) | 0.06 | - | - | - | |||||
| Pilates | 1 | 31 | −0.10 | (−1.08 to 1.28) | 0.87 | - | - | - | |||||
| Program duration | >12 weeks | 14 | 620 | −0.56 | (−0.95 to −0.17) | <0.01 | 83 | 76.76 | <0.01 | 40 | 1.67 | 0.20 | |
| ≤12 weeks | 10 | 242 | −0.19 | (−0.59 to 0.22) | 0.38 | 27 | 12.35 | 0.19 | |||||
| Daily Insulin Dosage (U·kg−1·day−1) | Total | 6 | 355 | −0.88 | (−1.27 to −0.48) | <0.01 | 98 | 276.52 | <0.01 | ||||
| Age groups | Children and adolescents | 4 | 297 | −1.69 | (−2.43 to −0.95) | <0.01 | 99 | 256.38 | <0.01 | 94.4 | 17.81 | <0.01 | |
| Adults | 2 | 58 | −0.09 | (−0.19 to 0.02) | 0.11 | 56 | 2.25 | 0.13 | |||||
| Exercise frequency | ≥3 times/week | 4 | 210 | −1.54 | (−2.21 to −0.88) | <0.01 | 99 | 270.57 | <0.01 | 93.1 | 14.44 | <0.01 | |
| <3 times/weeks | 2 | 145 | −0.19 | (−0.40 to 0.01) | 0.07 | 83 | 5.71 | 0.02 | |||||
| Type of exercise | Aerobic exercise | 3 | 80 | −0.09 | (−0.15 to −0.03) | <0.01 | 12 | 2.26 | 0.32 | 99.2 | 253.33 | <0.01 | |
| Combined aerobic and resistance training | 2 | 244 | −0.40 | (−0.60 to −0.20) | <0.01 | 76 | 4.22 | 0.04 | |||||
| Pilates | 1 | 31 | −7.7 | (−8.65 to −6.75) | <0.01 | - | - | - | |||||
| Program duration | >12 weeks | 5 | 324 | −0.20 | (−0.35 to −0.06) | <0.01 | 89 | 34.82 | <0.01 | 99.6 | 234.66 | <0.01 | |
| ≤12 weeks | 1 | 31 | −7.70 | (−8.65 to −6.75) | <0.01 | - | - | - | |||||
| Total Cholesterol (mmol L−1) | Total | 15 | 588 | −0.38 | (−0.71 to −0.04) | 0.03 | 89 | 125.08 | <0.01 | ||||
| Age groups | Children and adolescents | 7 | 343 | −0.84 | (−1.22 to −0.46) | <0.01 | 75 | 24.32 | <0.01 | 92.4 | 13.08 | <0.01 | |
| Adults | 8 | 245 | −0. 02 | (−0.25 to 0.21) | 0.86 | 57 | 16.31 | 0.02 | |||||
| Exercise frequency | ≥3 times/week | 13 | 451 | −0.25 | (−0.54 to 0.03) | 0.08 | 80 | 59.51 | <0.01 | 71.1 | 3.46 | 0.06 | |
| <3 times/week | 2 | 137 | −0. 96 | (−1.65 to −0.27) | <0.01 | 81 | 5.21 | 0.02 | |||||
| Type of exercise | Aerobic exercise | 9 | 190 | −0.10 | (−0.37 to 0.16) | 0.43 | 66 | 23.75 | <0.01 | 62.5 | 5.34 | 0.07 | |
| Combined aerobic and resistance training | 5 | 382 | −0.71 | (−1.15 to −0.27) | <0.01 | 84 | 24.67 | <0.01 | |||||
| Resistance training | 1 | 16 | −0.30 | (−1.28 to 0.68) | 0.55 | - | - | - | |||||
| Program duration | >12 weeks | 10 | 498 | −0.40 | (−0.76 to −0.04) | 0.03 | 90 | 89.96 | <0.01 | 0.0 | 0.07 | 0.78 | |
| ≤12 weeks | 5 | 90 | −0.29 | (−0.95 to 0.37) | 0.38 | 58 | 9.49 | 0.05 | |||||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, N.; Bredin, S.S.D.; Guan, Y.; Dickinson, K.; Kim, D.D.; Chua, Z.; Kaufman, K.; Warburton, D.E.R. Cardiovascular Health Benefits of Exercise Training in Persons Living with Type 1 Diabetes: A Systematic Review and Meta-Analysis. J. Clin. Med. 2019, 8, 253. https://doi.org/10.3390/jcm8020253
Wu N, Bredin SSD, Guan Y, Dickinson K, Kim DD, Chua Z, Kaufman K, Warburton DER. Cardiovascular Health Benefits of Exercise Training in Persons Living with Type 1 Diabetes: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine. 2019; 8(2):253. https://doi.org/10.3390/jcm8020253
Chicago/Turabian StyleWu, Nana, Shannon S.D. Bredin, Yanfei Guan, Kyra Dickinson, David D. Kim, Zongyu Chua, Kai Kaufman, and Darren E.R. Warburton. 2019. "Cardiovascular Health Benefits of Exercise Training in Persons Living with Type 1 Diabetes: A Systematic Review and Meta-Analysis" Journal of Clinical Medicine 8, no. 2: 253. https://doi.org/10.3390/jcm8020253
APA StyleWu, N., Bredin, S. S. D., Guan, Y., Dickinson, K., Kim, D. D., Chua, Z., Kaufman, K., & Warburton, D. E. R. (2019). Cardiovascular Health Benefits of Exercise Training in Persons Living with Type 1 Diabetes: A Systematic Review and Meta-Analysis. Journal of Clinical Medicine, 8(2), 253. https://doi.org/10.3390/jcm8020253





