Etiology of Minor Troponin Elevations in Patients with Atrial Fibrillation at Emergency Department–Tropo-AF Study
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
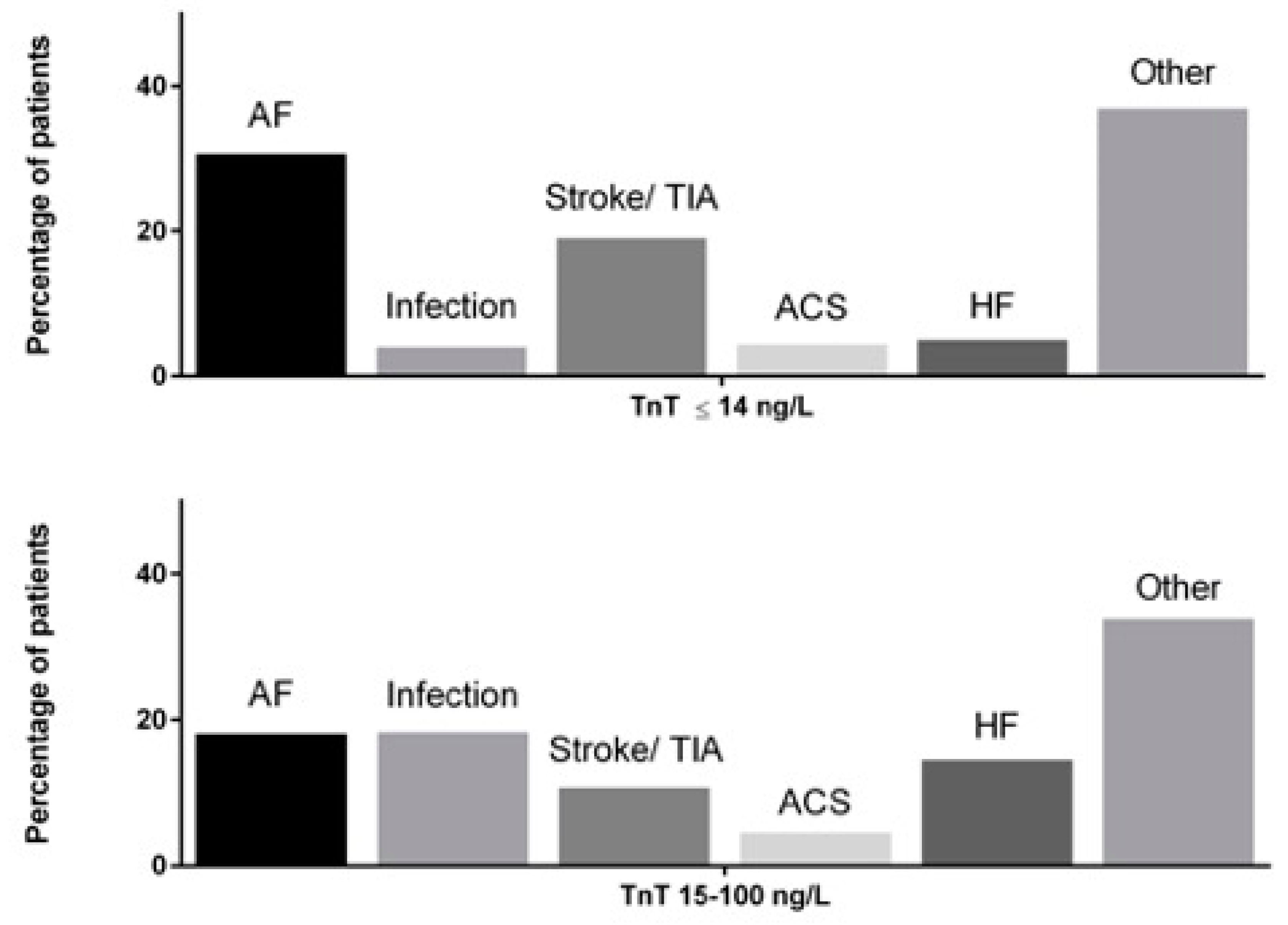
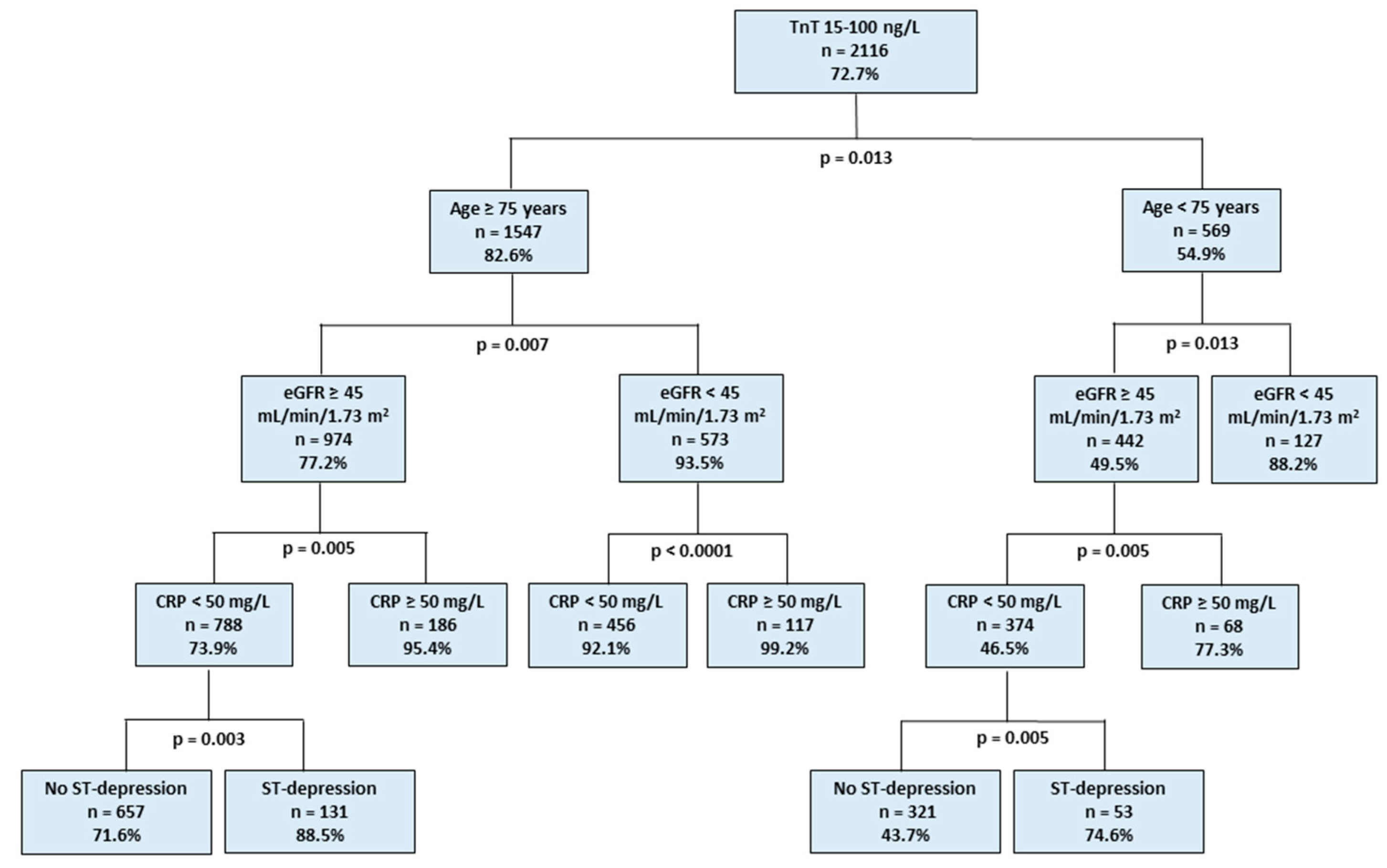
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Steinberg, B.A.; Kim, S.; Fonarow, G.C.; Thomas, L.; Ansell, J.; Kowey, P.R.; Mahaffey, K.W.; Gersh, B.J.; Hylek, E.; Naccarelli, G.; et al. Drivers of hospitalization for patients with atrial fibrillation: Results from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT-AF). Am. Heart J. 2014, 167, 735–742. [Google Scholar] [CrossRef] [PubMed]
- Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; Chaitman, B.R.; Bax, J.J.; Morrow, D.A.; White, H.D.; Thygesen, K.; Alpert, J.S.; Jaffe, A.S.; et al. Fourth universal definition of myocardial infarction (2018). Eur. Heart J. 2018, 138, 618–651. [Google Scholar]
- Carlsson, A.C.; Bandstein, N.; Roos, A.; Hammarsten, O.; Holzmann, M.J. High-sensitivity cardiac troponin T levels in the emergency department in patients with chest pain but no myocardial infarction. Int. J. Cardiol. 2017, 228, 253–259. [Google Scholar] [CrossRef] [PubMed]
- Shave, R.; Baggish, A.; George, K.; Wood, M.; Scharhag, J.; Whyte, G.; Gaze, D.; Thompson, P.D. Exercise-Induced Cardiac Troponin Elevation: Evidence, Mechanisms, and Implications. J. Am. Coll. Cardiol. 2010, 56, 169–176. [Google Scholar] [CrossRef]
- Paana, T.; Jaakkola, S.; Bamberg, K.; Saraste, A.; Tuunainen, E.; Wittfooth, S.; Kallio, P.; Heinonen, O.J.; Knuuti, J.; Pettersson, K.; et al. Cardiac troponin elevations in marathon runners. Role of coronary atherosclerosis and skeletal muscle injury. The MaraCat Study. Int. J. Cardiol. 2019, 295, 25–28. [Google Scholar] [CrossRef]
- Januzzi, J.L.; Filippatos, G.; Nieminen, M.; Gheorghiade, M. Troponin elevation in patients with heart failure: On behalf of the third Universal Definition of Myocardial Infarction Global Task Force: Heart Failure Section. Eur. Heart J. 2012, 33, 2265–2271. [Google Scholar] [CrossRef]
- Vaduganathan, M.; Bhatt, D.L. Cardiac Troponins in Chronic Kidney Disease: A Marker of Global Cardiovascular Risk. Am. J. Nephrol. 2017, 45, 301–303. [Google Scholar] [CrossRef]
- Douketis, J.D.; Crowther, M.A.; Stanton, E.B.; Ginsberg, J.S. Elevated Cardiac Troponin Levels in Patients With Submassive Pulmonary Embolism. Arch. Intern. Med. 2002, 162, 79–81. [Google Scholar] [CrossRef]
- Yaghi, S.; Chang, A.D.; Ricci, B.A.; Jayaraman, M.V.; McTaggart, R.A.; Hemendinger, M.; Narwal, P.; Dakay, K.; Mac Grory, B.; Cutting, S.M.; et al. Early Elevated Troponin Levels After Ischemic Stroke Suggests a Cardioembolic Source. Stroke 2018, 49, 121–126. [Google Scholar] [CrossRef]
- Frencken, J.F.; Donker, D.W.; Spitoni, C.; Koster-Brouwer, M.E.; Soliman, I.W.; Ong, D.S.Y.; Horn, J.; van der Poll, T.; van Klei, W.A.; Bonten, M.J.M.; et al. Myocardial Injury in Patients With Sepsis and Its Association With Long-Term Outcome. Circ. Cardiovasc. Qual. Outcomes 2018, 11, 004040. [Google Scholar] [CrossRef]
- Hijazi, Z.; Wallentin, L.; Siegbahn, A.; Andersson, U.; Alexander, J.H.; Atar, D.; Gersh, B.J.; Hanna, M.; Harjola, V.P.; Horowitz, J.D.; et al. High-Sensitivity Troponin T and Risk Stratification in Patients With Atrial Fibrillation During Treatment With Apixaban or Warfarin. J. Am. Coll. Cardiol. 2014, 63, 52–61. [Google Scholar] [CrossRef] [PubMed]
- Naffaa, M.E.; Nasser, R.; Manassa, E.; Younis, M.; Azzam, Z.S.; Aronson, D. Cardiac troponin-I as a predictor of mortality in patients with first episode acute atrial fibrillation. QJM An. Int. J. Med. 2017, 110, 507–511. [Google Scholar] [CrossRef][Green Version]
- Costabel, J.P.; Burgos, L.M.; Trivi, M. The Significance Of Troponin Elevation In Atrial Fibrillation. J. Atr. Fibrillation 2017, 9, 1530. [Google Scholar] [CrossRef]
- Jaakkola, S.; Kiviniemi, T.O.; Nuotio, I.; Hartikainen, J.; Mustonen, P.; Palomäki, A.; Jaakkola, J.; Ylitalo, A.; Hartikainen, P.; Airaksinen, K.E.J. Usefulness of the CHA 2 DS 2 -VASc and HAS-BLED Scores in Predicting the Risk of Stroke Versus Intracranial Bleeding in Patients With Atrial Fibrillation (from the FibStroke Study). Am. J. Cardiol. 2018, 121, 1182–1186. [Google Scholar] [CrossRef]
- Nuotio, I.; Hartikainen, J.E.K.; Grönberg, T.; Biancari, F.; Airaksinen, K.E.J. Time to Cardioversion for Acute Atrial Fibrillation and Thromboembolic Complications. JAMA 2014, 312, 647–649. [Google Scholar] [CrossRef] [PubMed]
- Airaksinen, K.E.J.; Grönberg, T.; Nuotio, I.; Nikkinen, M.; Ylitalo, A.; Biancari, F.; Hartikainen, J.E.K. Thromboembolic complications after cardioversion of acute atrial fibrillation: The FinCV (Finnish CardioVersion) study. J. Am. Coll. Cardiol. 2013, 62, 1187–1192. [Google Scholar] [CrossRef]
- von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P. STROBE Initiative The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Lancet (Lond. Engl.) 2007, 370, 1453–1457. [Google Scholar] [CrossRef]
- Roffi, M.; Patrono, C.; Collet, J.-P.; Mueller, C.; Valgimigli, M.; Andreotti, F.; Bax, J.J.; Borger, M.A.; Brotons, C.; Chew, D.P.; et al. 2015 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur. Heart J. 2016, 37, 267–315. [Google Scholar] [CrossRef]
- Twerenbold, R.; Boeddinghaus, J.; Nestelberger, T.; Wildi, K.; Rubini Gimenez, M.; Badertscher, P.; Mueller, C. Clinical Use of High-Sensitivity Cardiac Troponin in Patients With Suspected Myocardial Infarction. J. Am. Coll. Cardiol. 2017, 70, 996–1012. [Google Scholar] [CrossRef]
- Shah, A.S.V.; Anand, A.; Strachan, F.E.; Ferry, A.V.; Lee, K.K.; Chapman, A.R.; Sandeman, D.; Stables, C.L.; Adamson, P.D.; Andrews, J.P.M.; et al. High-sensitivity troponin in the evaluation of patients with suspected acute coronary syndrome: A stepped-wedge, cluster-randomised controlled trial. Lancet 2018, 392, 919–928. [Google Scholar] [CrossRef]
- Makam, A.N.; Nguyen, O.K. Use of Cardiac Biomarker Testing in the Emergency Department. JAMA Intern. Med. 2015, 175, 67–75. [Google Scholar] [CrossRef] [PubMed]
- Yiadom, M.Y.; Jarolim, P.; Jenkins, C.; Melanson, S.E.F.; Conrad, M.; Kosowsky, J.M. Diagnostic implications of an elevated troponin in the emergency department. Dis. Markers 2015, 2015, 157812. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.K.; Noaman, A.; Vaswani, A.; Gibbins, M.; Griffiths, M.; Chapman, A.R.; Strachan, F.; Anand, A.; McAllister, D.A.; Newby, D.E.; et al. Prevalence, Determinants, and Clinical Associations of High-Sensitivity Cardiac Troponin in Patients Attending Emergency Departments. Am. J. Med. 2019, 132, 8–21. [Google Scholar] [CrossRef] [PubMed]
- Shah, A.S.V.; Sandoval, Y.; Noaman, A.; Sexter, A.; Vaswani, A.; Smith, S.W.; Gibbins, M.; Griffiths, M.; Chapman, A.R.; Strachan, F.E.; et al. Patient selection for high sensitivity cardiac troponin testing and diagnosis of myocardial infarction: Prospective cohort study. BMJ 2017, 359, j4788. [Google Scholar] [CrossRef] [PubMed]
- Morrow, D.A. Clinician’s Guide to Early Rule-Out Strategies With High-Sensitivity Cardiac Troponin. Circulation 2017, 135, 1612–1616. [Google Scholar] [CrossRef] [PubMed]
- Morrow, D.A.; Cannon, C.P.; Jesse, R.L.; Newby, L.K.; Ravkilde, J.; Storrow, A.B.; Wu, A.H.B.; Christenson, R.H. National Academy of Clinical Biochemistry National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines: Clinical Characteristics and Utilization of Biochemical Markers in Acute Coronary Syndromes. Circulation 2007, 115, 356–375. [Google Scholar]
- Mahajan, V.S.; Jarolim, P. How to interpret elevated cardiac troponin levels. Circulation 2011, 124, 2350–2354. [Google Scholar] [CrossRef]
- Thelin, J.; Melander, O. Dynamic high-sensitivity troponin elevations in atrial fibrillation patients might not be associated with significant coronary artery disease. BMC Cardiovasc. Disord. 2017, 17, 169. [Google Scholar] [CrossRef]
- Wettersten, N.; Maisel, A. Role of Cardiac Troponin Levels in Acute Heart Failure. Card. Fail. Rev. 2015, 1, 102–106. [Google Scholar] [CrossRef]
- Zochios, V.; Valchanov, K. Raised cardiac troponin in intensive care patients with sepsis, in the absence of angiographically documented coronary artery disease: A systematic review. J. Intensive Care Soc. 2015, 16, 52–57. [Google Scholar] [CrossRef]
- Becattini, C.; Vedovati, M.C.; Agnelli, G. Prognostic Value of Troponins in Acute Pulmonary Embolism. Circulation 2007, 116, 427–433. [Google Scholar] [CrossRef] [PubMed]
- Upadhyay, A.; Lopez-Mattei, J.; Kim, P.; Iliescu, C.; Durand, J.-B.; Palaskas, N.; Hassan, S.; Thompson, K.; Mouhayar, E. Diagnostic perfomance of high sensitivity troponin in cancer patients. J. Am. Coll. Cardiol. 2019, 73, 209. [Google Scholar] [CrossRef]
- Mochmann, H.-C.; Scheitz, J.F.; Petzold, G.C.; Haeusler, K.G.; Audebert, H.J.; Laufs, U.; Schneider, C.; Landmesser, U.; Werner, N.; Endres, M.; et al. Coronary Angiographic Findings in Acute Ischemic Stroke Patients With Elevated Cardiac Troponin: The Troponin Elevation in Acute Ischemic Stroke (TRELAS) Study. Circulation 2016, 133, 1264–1271. [Google Scholar] [CrossRef] [PubMed]
- Agewall, S.; Giannitsis, E.; Jernberg, T.; Katus, H. Troponin elevation in coronary vs. non-coronary disease. Eur. Heart J. 2011, 32, 404–411. [Google Scholar] [CrossRef]
- Hammarsten, O.; Mair, J.; Möckel, M.; Lindahl, B.; Jaffe, A.S. Possible mechanisms behind cardiac troponin elevations. Biomarkers 2018, 23, 725–734. [Google Scholar] [CrossRef] [PubMed]
- Katus, H.A.; Remppis, A.; Scheffold, T.; Diederich, K.W.; Kuebler, W. Intracellular compartmentation of cardiac troponin T and its release kinetics in patients with reperfused and nonreperfused myocardial infarction. Am. J. Cardiol. 1991, 67, 1360–1367. [Google Scholar] [CrossRef]
- Eggers, K.M.; Jernberg, T.; Lindahl, B. Cardiac Troponin Elevation in Patients Without a Specific Diagnosis. J. Am. Coll. Cardiol. 2019, 73, 1–9. [Google Scholar] [CrossRef]
| Characteristic | TnT ≤ 14 ng/L (n = 795) | TnT 15–100 ng/L (n = 2116) | |
|---|---|---|---|
| No. (%) | No. (%) | p | |
| Age, median (IQR), y | 72.0 (14) | 81.0 (12) | <0.001 |
| Women | 431 (54.3) | 1026 (48.5) | 0.005 |
| CHA2DS2-VASc, mean (SD) | 3.30 (1.85) | 4.11 (1.68) | <0.001 |
| Heart failure | 86 (10.8) | 524 (24.8) | <0.001 |
| Hypertension | 505 (63.5) | 1485 (70.2) | 0.001 |
| Diabetes mellitus | 155 (19.5) | 590 (27.9) | <0.001 |
| Prior stroke | 119 (15.0) | 346 (16.4) | 0.39 |
| Prior myocardial infarction | 99 (12.5) | 350 (16.5) | 0.007 |
| Hypercholesterolemia | 340 (42.8) | 811 (38.3) | 0.03 |
| Coronary artery disease | 186 (23.4) | 683 (32.3) | <0.001 |
| Heart rate at admission, median (IQR), bpm | 81 (66–102) | 87 (72–109) | <0.001 |
| Systolic blood pressure, median (IQR), mm Hg * | 144 (126–163) | 140 (122–160) | 0.002 |
| ST depression in admission ECG *,† | 42 (5.8) | 305 (15.9) | <0.001 |
| Laboratory tests at admission | |||
| TnT, median (IQR), ng/L | 9 (6–11) | 30 (21–48) | <0.001 |
| Hemoglobin, median (IQR), g/dL | 13.8 (12.8–14.7) | 12.8 (11.5–14.2) | <0.001 |
| Creatinine, median (IQR), μmol/L | 79.6 (70.7–97.2) | 97.2 (79.6–124) | <0.001 |
| eGFR, median (IQR), mL/min/1.73 m2 | 71.3 (58.8–83.8) | 55.1 (40.0–72.3) | <0.001 |
| ProBNP, median (IQR), ng/L * | 998 (454–2335) | 3370 (1580–6355) | <0.001 |
| CRP, median (IQR), mg/L | 3 (2–7) | 10 (3–37) | <0.001 |
| Univariable | Odds Ratio (95% CI) | p | Multivariable | Odds Ratio (95% CI) | p |
|---|---|---|---|---|---|
| Age ≥ 75 years | 3.89 (3.28–4.62) | <0.001 | Age ≥ 75 years | 4.77 (3.77–6.04) | <0.001 |
| Male gender | 1.26 (1.07–1.49) | 0.005 | Male gender | 2.54 (2.01–3.21) | <0.001 |
| Heart failure | 2.71 (2.13–3.47) | <0.001 | Chest pain | 0.58 (0.44–0.76) | <0.001 |
| Hypertension | 1.35 (1.14–1.61) | 0.001 | ST depression in admission ECG * | 2.71 (1.85–3.97) | <0.001 |
| Diabetes mellitus | 1.60 (1.31–1.95) | <0.001 | Ventricular rate ≥ 100 bpm at admission | 1.71 (1.36–2.17) | <0.001 |
| Prior stroke or TIA | 0.98 (0.80–1.20) | 0.83 | eGFR < 45 mL/min/1.73 m2 | 5.06 (3.58–7.14) | <0.001 |
| Hypercholesterolemia | 0.83 (0.71–0.98) | 0.03 | CRP ≥ 50 mg/L | 3.79 (2.49–5.77) | <0.001 |
| Coronary artery disease | 1.56 (1.29–1.89) | <0.001 | Hemoglobin < 10.0 g/dL | 4.95 (2.33–10.55) | <0.001 |
| Active malignancy | 1.30 (0.85–1.98) | 0.23 | |||
| Chest pain | 0.44 (0.36–0.54) | <0.001 | |||
| ST depression in admission ECG *,† | 3.06 (2.19–4.27) | <0.001 | |||
| Ventricular rate ≥ 100 bpm at admission | 1.37 (1.14–1.64) | 0.001 | |||
| AF at admission | 1.79 (1.51–2.12) | <0.001 | |||
| eGFR < 45 mL/min/1.73 m2 | 6.40 (4.82–8.51) | <0.001 | |||
| CRP ≥ 50 mg/L † | 5.04 (3.46–7.35) | <0.001 | |||
| Hemoglobin < 10.0 g/dL | 6.19 (3.34–11.4) | <0.001 |
| Univariable Predictors | Odds Ratio (95% CI) | p | Multivariable Predictors | Odds Ratio (95% CI) | p |
|---|---|---|---|---|---|
| Age ≥ 75 years | 0.88 (0.56–1.37) | 0.561 | Chest pain | 8.29 (5.20–13.2) | <0.001 |
| Male gender | 1.73 (1.13–2.66) | 0.012 | Coronary artery disease | 2.33 (1.42–3.81) | 0.001 |
| Hypertension | 1.43 (0.88–2.33) | 0.148 | eGFR < 45 mL/min/1.73 m2 * | 1.65 (1.04–2.63) | 0.035 |
| Diabetes mellitus | 1.69 (1.11–2.59) | 0.015 | |||
| Hypercholesterolemia | 2.52 (1.66–3.84) | <0.001 | |||
| Prior myocardial infarction | 3.83 (2.50–5.87) | <0.001 | |||
| Prior stroke or TIA | 0.67 (0.37–1.21) | 0.186 | |||
| Coronary artery disease | 4.68 (3.01–7.26) | <0.001 | |||
| Heart failure | 0.91 (0.56–1.48) | 0.711 | |||
| Chest pain | 11.1 (7.19–17.1) | <0.001 | |||
| eGFR < 45 mL/min/1.73 m2 | 1.57 (1.03–2.37) | 0.035 | |||
| CRP ≥ 50 mg/L | 0.38 (0.18–0.80) | 0.009 | |||
| Troponin T, ≥100% change | 1.86 (0.99–3.48) | 0.054 | |||
| Hemoglobin < 100 g/L | 1.06 (0.51–2.23) | 0.873 | |||
| ST depression in ECG * | 0.73 (0.37–1.43) | 0.355 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jaakkola, S.; Paana, T.; Nuotio, I.; Kiviniemi, T.O.; Pouru, J.-P.; Porela, P.; Biancari, F.; Airaksinen, K.E.J. Etiology of Minor Troponin Elevations in Patients with Atrial Fibrillation at Emergency Department–Tropo-AF Study. J. Clin. Med. 2019, 8, 1963. https://doi.org/10.3390/jcm8111963
Jaakkola S, Paana T, Nuotio I, Kiviniemi TO, Pouru J-P, Porela P, Biancari F, Airaksinen KEJ. Etiology of Minor Troponin Elevations in Patients with Atrial Fibrillation at Emergency Department–Tropo-AF Study. Journal of Clinical Medicine. 2019; 8(11):1963. https://doi.org/10.3390/jcm8111963
Chicago/Turabian StyleJaakkola, Samuli, Tuomas Paana, Ilpo Nuotio, Tuomas O. Kiviniemi, Jussi-Pekka Pouru, Pekka Porela, Fausto Biancari, and K. E. Juhani Airaksinen. 2019. "Etiology of Minor Troponin Elevations in Patients with Atrial Fibrillation at Emergency Department–Tropo-AF Study" Journal of Clinical Medicine 8, no. 11: 1963. https://doi.org/10.3390/jcm8111963
APA StyleJaakkola, S., Paana, T., Nuotio, I., Kiviniemi, T. O., Pouru, J.-P., Porela, P., Biancari, F., & Airaksinen, K. E. J. (2019). Etiology of Minor Troponin Elevations in Patients with Atrial Fibrillation at Emergency Department–Tropo-AF Study. Journal of Clinical Medicine, 8(11), 1963. https://doi.org/10.3390/jcm8111963





