Music Interventions for Anxiety in Pregnant Women: A Systematic Review and Meta-Analysis of Randomized Controlled Trials
Abstract
:1. Introduction
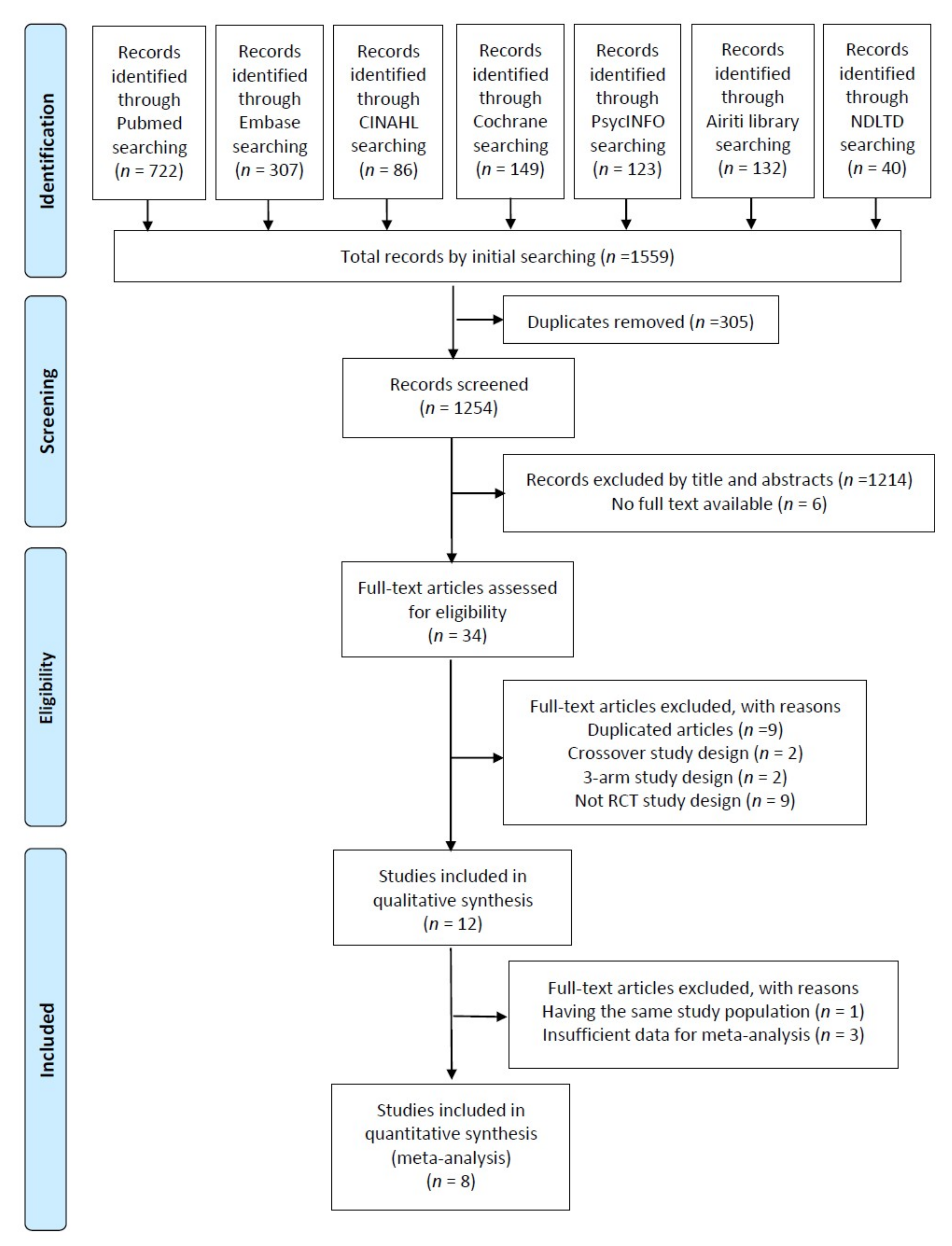
2. Experimental Section
2.1. Search Strategy
2.2. Inclusion and Exclusion Criteria
2.3. Data Extraction and Quality Assessment
2.4. Statistical Analysis
3. Results
3.1. Description of Studies and Quality Assessment
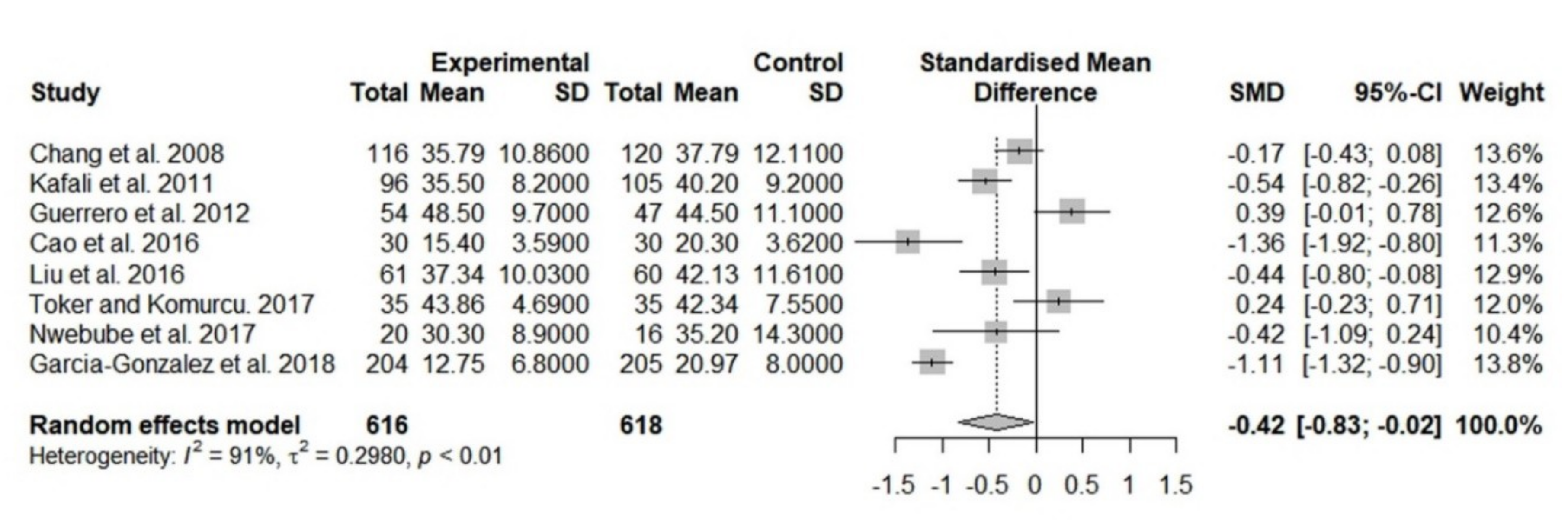
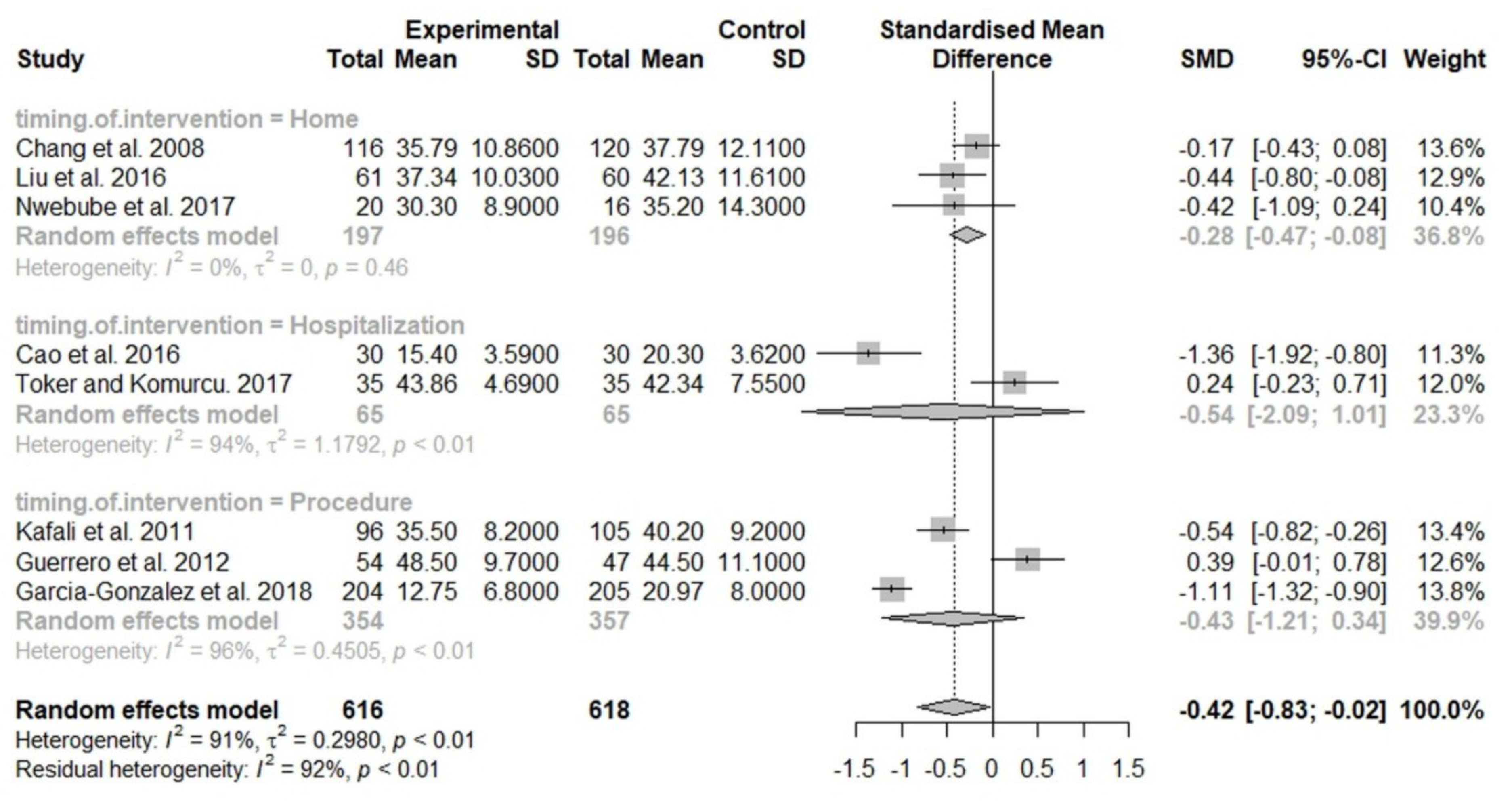
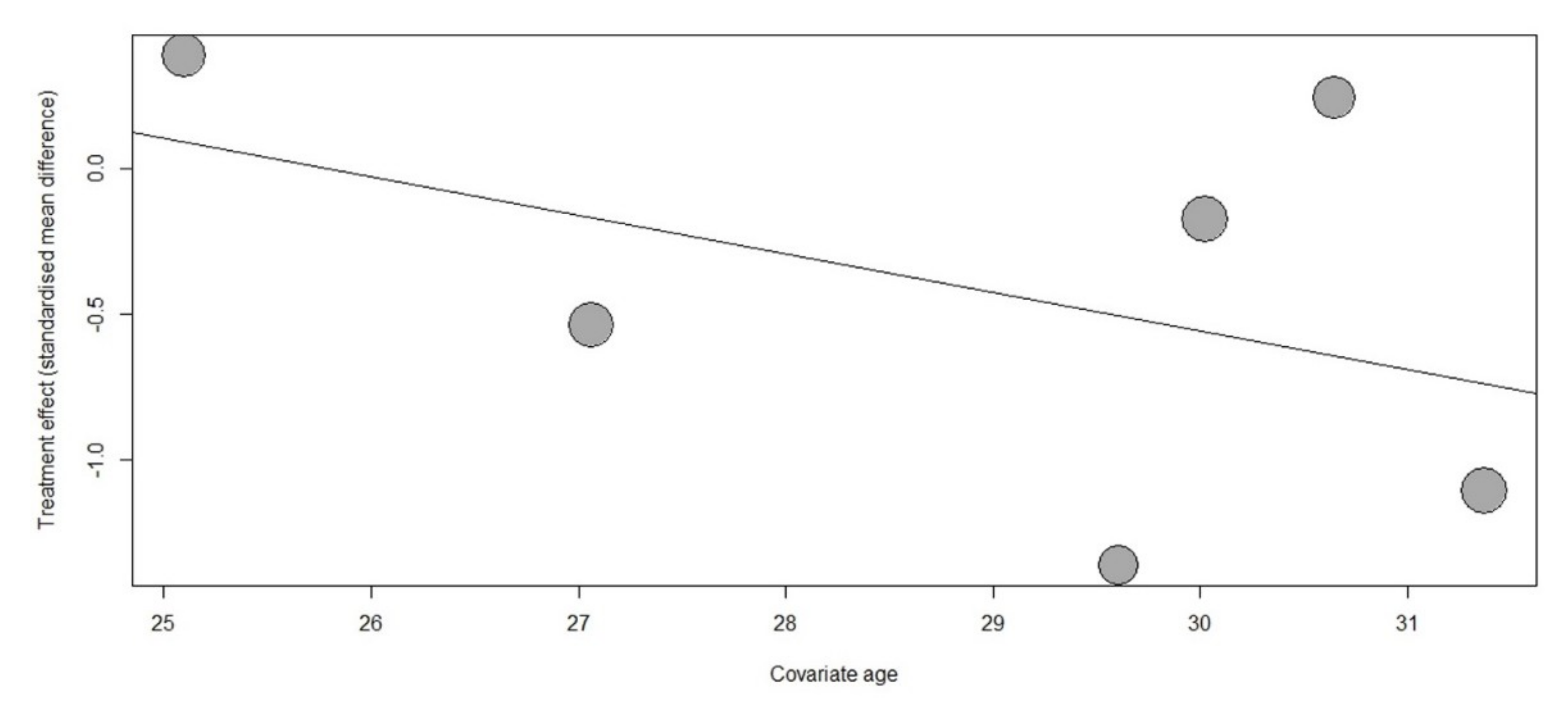
3.2. Data Synthesis and Meta-Analyses
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Dennis, C.L.; Falah-Hassani, K.; Shiri, R. Prevalence of antenatal and postnatal anxiety: Systematic review and meta-analysis. Br. J. Psychiatry 2017, 210, 315–323. [Google Scholar] [CrossRef] [PubMed]
- Rees, S.; Channon, S.; Waters, C.S. The impact of maternal prenatal and postnatal anxiety on children’s emotional problems: A systematic review. Eur. Child Adolesc. Psychiatry 2019, 28, 257–280. [Google Scholar] [CrossRef] [PubMed]
- Staneva, A.; Bogossian, F.; Pritchard, M.; Wittkowski, A. The effects of maternal depression, anxiety and perceived stress during pregnancy on preterm birth: A systematic review. Women Birth 2015, 28, 179–193. [Google Scholar] [CrossRef] [PubMed]
- Glover, V. Maternal depression, anxiety and stress during pregnancy and child outcome; what needs to be done. Best Pract. Res. Clin. Obstet. Gynaecol. 2014, 28, 25–35. [Google Scholar] [CrossRef] [PubMed]
- Dubber, S.; Reck, C.; Muller, M.; Gawlik, S. Postpartum bonding: The role of perinatal depression, anxiety and maternal-fetal bonding during pregnancy. Arch. Womens Ment. Health 2015, 18, 187–195. [Google Scholar] [CrossRef] [PubMed]
- Littleton, H.L.; Breitkopf, C.R.; Berenson, A.B. Correlates of anxiety symptoms during pregnancy and association with perinatal outcomes: A meta-analysis. Am. J. Obstet. Gynecol. 2007, 196, 424–432. [Google Scholar] [CrossRef]
- Sujan, A.C.; Rickert, M.E.; Oberg, A.S.; Quinn, P.D.; Hernandez-Diaz, S.; Almqvist, C.; Lichtenstein, P.; Larsson, H.; D’Onofrio, B.M. Associations of maternal antidepressant use during the first trimester of pregnancy with preterm birth, small for gestational age, autism spectrum disorder, and attention-deficit/hyperactivity disorder in offspring. JAMA 2017, 317, 1553–1562. [Google Scholar] [CrossRef]
- Yonkers, K.A.; Gilstad-Hayden, K.; Forray, A.; Lipkind, H.S. Association of panic disorder, generalized anxiety disorder, and benzodiazepine treatment during pregnancy with risk of adverse birth outcomes. JAMA Psychiatry 2017, 74, 1145–1152. [Google Scholar] [CrossRef]
- Freeman, M.P.; Goez-Mogollon, L.; McInerney, K.A.; Davies, A.C.; Church, T.R.; Sosinsky, A.Z.; Noe, O.B.; Viguera, A.C.; Cohen, L.S. Obstetrical and neonatal outcomes after benzodiazepine exposure during pregnancy: Results from a prospective registry of women with psychiatric disorders. Gen. Hosp. Psychiatry 2018, 53, 73–79. [Google Scholar] [CrossRef]
- Guetin, S.; Portet, F.; Picot, M.C.; Pommie, C.; Messaoudi, M.; Djabelkir, L.; Olsen, A.L.; Cano, M.M.; Lecourt, E.; Touchon, J. Effect of music therapy on anxiety and depression in patients with alzheimer’s type dementia: Randomised, controlled study. Dement. Geriatr. Cogn. Disord. 2009, 28, 36–46. [Google Scholar]
- Bradt, J.; Dileo, C.; Potvin, N. Music for stress and anxiety reduction in coronary heart disease patients. Cochrane Database Syst. Rev. 2013, 12. [Google Scholar] [CrossRef] [PubMed]
- Bradt, J.; Dileo, C.; Magill, L.; Teague, A. Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database Syst. Rev. 2016, 8. [Google Scholar] [CrossRef] [PubMed]
- Bradt, J.; Dileo, C.; Shim, M. Music interventions for preoperative anxiety. Cochrane Database Syst. Rev. 2013, 6. [Google Scholar] [CrossRef] [PubMed]
- Corbijn van Willenswaard, K.; Lynn, F.; McNeill, J.; McQueen, K.; Dennis, C.-L.; Lobel, M.; Alderdice, F. Music interventions to reduce stress and anxiety in pregnancy: A systematic review and meta-analysis. BMC Psychiatry 2017, 17. [Google Scholar] [CrossRef] [PubMed]
- Cao, S.; Sun, J.; Wang, Y.; Zhao, Y.; Sheng, Y.; Xu, A. Music therapy improves pregnancy-induced hypertension treatment efficacy. Int. J. Clin. Exp. Med. 2016, 9, 8833–8838. [Google Scholar]
- Garcia-Gonzalez, J.; Ventura-Miranda, M.I.; Requena-Mullor, M.; Parron-Carreño, T.; Alarcon-Rodriguez, R. State-trait anxiety levels during pregnancy and foetal parameters following intervention with music therapy. J. Affect. Disord. 2018, 232, 17–22. [Google Scholar] [CrossRef]
- Liu, Y.-H.; Lee, C.S.; Yu, C.-H.; Chen, C.-H. Effects of music listening on stress, anxiety and sleep quality for sleep-disturbed pregnant women. Women Health 2016, 56, 296–311. [Google Scholar] [CrossRef]
- Toker, E.; Kömürcü, N. Effect of turkish classical music on prenatal anxiety and satisfaction: A randomized controlled trial in pregnant women with pre-eclampsia. Complement. Ther. Med. 2017, 30, 1–9. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The prisma statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. Ann. Intern. Med. 2009, 151, 65–94. [Google Scholar] [CrossRef]
- Spielberger, C.D.; Gorsuch, R.L.; Lushene, R.; Vagg, P.R.; Jacobs, G.A. STAI Manual for the Stait-Trait Anxiety Inventory (“Self-Evaluation Questionnaire”); Consulting Psychologists Press: Palo Alto, CA, USA, 1983. [Google Scholar]
- Chang, M.; Chen, C.; Huang, K. Effects of music therapy on psychological health of women during pregnancy. J. Clin. Nurs. 2008, 17, 2580–2587. [Google Scholar] [CrossRef]
- Yang, M.; Li, L.; Zhu, H.; Alexander, I.; Liu, S.; Zhou, W.; Ren, X. Music therapy to relieve anxiety in pregnant women on bedrest: A randomized, controlled trial. MCN Am. J. Matern. Child Nurs. 2009, 34, 316–323. [Google Scholar] [CrossRef] [PubMed]
- Hamilton, M. The assessment of anxiety states by rating. Br. J. Med. Psychol. 1959, 32, 50–55. [Google Scholar] [CrossRef] [PubMed]
- A Revised Cochrane Risk-of-Bias Tool for Randomized Rrials (Rob 2.0). Available online: https://methods.cochrane.org/bias/resources/rob-2-revised-cochrane-risk-bias-tool-randomized-trials (accessed on 21 September 2019).
- Rstudio Software. Available online: https://www.rstudio.com/products/rstudio/download (accessed on 21 September 2019).
- Higgins, J.P.; Thompson, S.G.; Deeks, J.J.; Altman, D.G. Measuring inconsistency in meta-analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef] [Green Version]
- Egger, M.; Davey Smith, G.; Schneider, M.; Minder, C. Bias in meta-analysis detected by a simple, graphical test. BMJ 1997, 315, 629–634. [Google Scholar] [CrossRef] [Green Version]
- Kafali, H.; Derbent, A.; Keskin, E.; Simavli, S.; Gözdemir, E. Effect of maternal anxiety and music on fetal movements and fetal heart rate patterns. J. Matern.-Fetal Neonatal Med. 2011, 24, 461–464. [Google Scholar] [CrossRef]
- Guerrero, J.M.; Castano, P.M.; Schmidt, E.O.; Rosario, L.; Westhoff, C.L. Music as an auxiliary analgesic during first trimester surgical abortion: A randomized controlled trial. Contraception 2012, 86, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Chaplin, W.; Amico, J.; Butler, M.; Ojie, M.J.; Hennedy, D.; Clemow, L. Music for surgical abortion care study: A randomized controlled pilot study. Contraception 2012, 85, 496–502. [Google Scholar] [CrossRef]
- Nwebube, C.; Glover, V.; Stewart, L. Prenatal listening to songs composed for pregnancy and symptoms of anxiety and depression: A pilot study. BMC Complement. Altern. Med. 2017, 17, 256. [Google Scholar] [CrossRef]
- Teckenberg-Jansson, P.; Turunen, S.; Pölkki, T.; Lauri-Haikala, M.-J.; Lipsanen, J.; Henelius, A.; Aitokallio-Tallberg, A.; Pakarinen, S.; Leinikka, M.; Huotilainen, M. Effects of live music therapy on heart rate variability and self-reported stress and anxiety among hospitalized pregnant women: A randomized controlled trial. Nord. J. Music Ther. 2019, 28, 7–26. [Google Scholar] [CrossRef]
- García González, J.; Ventura Miranda, M.I.; Requena Mullor, M.; Parron Carreño, T.; Alarcón Rodriguez, R.; García González, J.; Parron Carreño, T.; Alarcón Rodriguez, R. Effects of prenatal music stimulation on state/trait anxiety in full-term pregnancy and its influence on childbirth: A randomized controlled trial. J. Matern. Fetal Neonatal Med. 2018, 31, 1058–1065. [Google Scholar] [CrossRef] [PubMed]
- Lin, H.H.; Chang, Y.C.; Chou, H.H.; Chang, C.P.; Huang, M.Y.; Liu, S.J.; Tsai, C.H.; Lei, W.T.; Yeh, T.L. Effect of music interventions on anxiety during labor: A systematic review and meta-analysis of randomized controlled trials. PeerJ 2019, 7. [Google Scholar] [CrossRef] [PubMed]
- Kuhlmann, A.Y.R.; de Rooij, A.; Kroese, L.F.; van Dijk, M.; Hunink, M.G.M.; Jeekel, J. Meta-analysis evaluating music interventions for anxiety and pain in surgery. Br. J. Surg. 2018, 105, 773–783. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Abdelhakim, A.M.; Samy, A.; Abbas, A.M. Effect of music in reducing patient anxiety during colposcopy: A systematic review and meta-analysis of randomized controlled trials. J. Gynecol. Obstet. Hum. Reprod. 2019, in press. [Google Scholar] [CrossRef] [PubMed]
- Bowen, A.; Bowen, R.; Maslany, G.; Muhajarine, N. Anxiety in a socially high-risk sample of pregnant women in Canada. Can. J. Psychiatry 2008, 53, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.M.; Lam, S.K.; Sze Mun Lau, S.M.; Chong, C.S.; Chui, H.W.; Fong, D.Y. Prevalence, course and risk factors for antenatal anxiety and depression. Obstet. Gynecol. 2007, 110, 1102–1112. [Google Scholar] [CrossRef]
- Rubertsson, C.; Hellstrom, J.; Cross, M.; Sydsjo, G. Anxiety in early pregnancy: Prevalence and contributing factors. Arch. Womens Ment. Health 2014, 17, 221–228. [Google Scholar] [CrossRef]
- Fancourt, D.; Ockelford, A.; Belai, A. The psychoneuroimmunological effects of music: A systematic review and a new model. Brain Behav. Immun. 2014, 36, 15–26. [Google Scholar] [CrossRef]
- Thoma, M.V.; La Marca, R.; Bronnimann, R.; Finkel, L.; Ehlert, U.; Nater, U.M. The effect of music on the human stress response. PLoS ONE 2013, 8. [Google Scholar] [CrossRef]
| Study | Country | Participants | Intervention | Music Type | Outcome Assessment | Main Findings |
|---|---|---|---|---|---|---|
| Chang et al. 2008 [21] | Taiwan | 236 women, mean age 30 yrs, GA 18–22 wks or 30–34 wks, medically low risk | Intervention (n = 116): receiving music at home for at least 30 min a day for 2 wks; Control (n = 120): usual care | Chosen by patient from four types of recorded CD | Before and after the 2-week program: S-STAI, PSS, EPDS | Significantly more reduced S-STAI after the intervention (35.8 ± 10.9) compared with that at baseline (37.9 ± 9.8), p < 0.05 |
| Yang et al. 2009 [22] | China | 120 women, most (96.7%) aged under 35 yrs, GA 28–36 wks, admitted with high-risk pregnancies | Intervention (n = 60): receiving music on the 3rd day of hospitalization, 30 min a day for 3 days; Control (n = 60): usual care | Chosen by patient from three types of recorded CD | Before and 2 h after the final session: S-STAI, maternal vital signs (HR, RR, BP), FHR | Significantly more improved S-STAI in the music group (preat–post difference 14.1 ± 5.8) than that in the control group (0.1 ± 2.8), p < 0.01 |
| Kafali et al. 2011 [28] | Turkey | 201 women, mean age 27.1 yrs, GA 36 wks, medically low risk | Intervention (n = 96): receiving music during NST; Control (n = 105): no music during NST | Patient’s own music or chosen from three types of recorded files | Before and after NST: STAI, baseline FHR, fetal movement, NST findings | Significantly lower posttest STAI in the music group (35.5 ± 8.2) than in the control group (40.2 ± 9.2), p < 0.001 |
| Guerrero et al. 2012 [29] | USA | 101 women, mean age 25.1 yrs, GA <14 wks, for vacuum aspiration abortion | Intervention (n = 54): receiving music during the procedure; Control (n = 47): no music during the procedure | Chosen by patient from 10 preloaded playlists | Before and after the procedure: S-STAI, pain on VAS, maternal BP, maternal HR | Both groups had higher S-STAI after the procedure than at baseline (music group pre–post difference 3.5 ± 10.8 vs. control group 1.2 ± 9.0), p = 0.25 |
| Wu et al. 2012 [30] | USA | 26 women, mean age 25.1 yrs, mean GA 8.3 wks based on ultrasound, for surgical abortion | Intervention (n = 13): receiving music during the procedure; Control (n = 13): no music during the procedure | Chosen by patient from five preloaded playlists | Assessed at five time points: baseline, prior to the pelvic exam, during uterine evacuation, just after speculum removal, 30 min after the procedure: 11-point verbal numerical scales of anxiety and pain | Nonsignificant trend toward a faster decline in anxiety immediately after the procedure in the music group, p = 0.06 |
| Cao et al. 2016 [15] | China | 60 women, mean age 29.6 yrs, admitted with pregnancy-induced hypertension | Intervention (n = 30): receiving music for 30–60 min a day for 4 wks; Control (n = 30): conventional treatment | Patient’s own music or chosen from a recorded CD | Before and after the intervention: HAM-A, HAM-D, SF-36 scale, maternal BP, serum angiotensin II level | Significantly lower posttest HAM-A in the music group (15.4 ± 3.6) than in the control group (20.3 ± 3.6), p < 0.05 |
| Liu et al. 2016 [17] | Taiwan | 121 women, over 18 yrs, GA 18–34 wks with poor sleep quality | Intervention (n = 61): receiving music for at least 30 min a day at bedtime at home for 2 wks; Control (n = 60): usual care | Patient’s own music or chosen from five types of recorded CD | Before and after the 2-week program: S-STAI, PSQI, PSS | Significantly lower posttest S-STAI in the music group (37.3 ± 10.0) than in the control group (42.1 ± 11.6), p < 0.05 |
| Toker and Kömürcü. 2017 [18] | Turkey | 70 women, mean age 30.6 yrs, GA over 30 wks, admitted with pre-eclampsia | Intervention (n = 35): receiving music for 30 min a day for 7 days; Control (n = 35): usual care | Chosen by patient from recorded playlists | Before and after (the 5th day of the intervention): S-STAI, Newcastle Satisfaction with Nursing Scale, maternal HR, fetal movement, FHR | No significant difference in posttest S-STAI between the groups (music group 43.9 ± 4.7 vs. control group 42.3 ± 7.6), p = 0.32 |
| Nwebube et al. 2017 [31] | UK | 36 women, over 18 yrs, recruited online (from multiple countries) | Intervention (n = 20): receiving music for at least 20 min a day for 12 wks at home; Control (n = 16): usual care | Recorded files by investigator | Before and after the 12-week program: S-STAI, EPDS | Significantly reduced S-STAI after the intervention (30.3 ± 8.9) than at baseline (37.1 ± 12.1), p = 0.02 |
| Garcia-Gonzalez et al. 2018 [16] | Spain | 409 primiparous women, mean age 31.4 yrs, third trimester of pregnancy, medically low risks | Intervention (n = 204): receiving music at home (40 min per session, 14 sessions, 3 times/week) and during NST (40 min); Control (n = 205): usual care and no music during NST | Recorded CD by investigator | Before and after NST: S-STAI, birthing process, newborn parameters | Significantly lower posttest S-STAI in the music group (12.8 ± 6.8) than in the control group (21.0 ± 8.0), p < 0.001 |
| Teckenberg-Jansson et al. 2019 [32] | Finland | 102 women, mean age 31 yrs, admitted with pregnancy-related complications | Intervention (n = 52): music therapy for 30 min a day for 3 days; Control (n = 50): conventional treatment | Playing of two lyre instruments and humming at bedside by the music therapist | Before and after the intervention: symptoms of S-STAI, PSS, FHR variability | Significantly more improved anxiety level in the music group than in the control group, p = 0.02 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Lin, C.-J.; Chang, Y.-C.; Chang, Y.-H.; Hsiao, Y.-H.; Lin, H.-H.; Liu, S.-J.; Chao, C.-A.; Wang, H.; Yeh, T.-L. Music Interventions for Anxiety in Pregnant Women: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. J. Clin. Med. 2019, 8, 1884. https://doi.org/10.3390/jcm8111884
Lin C-J, Chang Y-C, Chang Y-H, Hsiao Y-H, Lin H-H, Liu S-J, Chao C-A, Wang H, Yeh T-L. Music Interventions for Anxiety in Pregnant Women: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Journal of Clinical Medicine. 2019; 8(11):1884. https://doi.org/10.3390/jcm8111884
Chicago/Turabian StyleLin, Chien-Ju, Yu-Chen Chang, Yu-Han Chang, Yu-Hsuan Hsiao, Hsin-Hui Lin, Shu-Jung Liu, Chi-An Chao, Hsuan Wang, and Tzu-Lin Yeh. 2019. "Music Interventions for Anxiety in Pregnant Women: A Systematic Review and Meta-Analysis of Randomized Controlled Trials" Journal of Clinical Medicine 8, no. 11: 1884. https://doi.org/10.3390/jcm8111884
APA StyleLin, C.-J., Chang, Y.-C., Chang, Y.-H., Hsiao, Y.-H., Lin, H.-H., Liu, S.-J., Chao, C.-A., Wang, H., & Yeh, T.-L. (2019). Music Interventions for Anxiety in Pregnant Women: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Journal of Clinical Medicine, 8(11), 1884. https://doi.org/10.3390/jcm8111884





