Optimized Treatment for Infantile Spasms: Vigabatrin versus Prednisolone versus Combination Therapy
Abstract
1. Introduction
2. Experimental Section
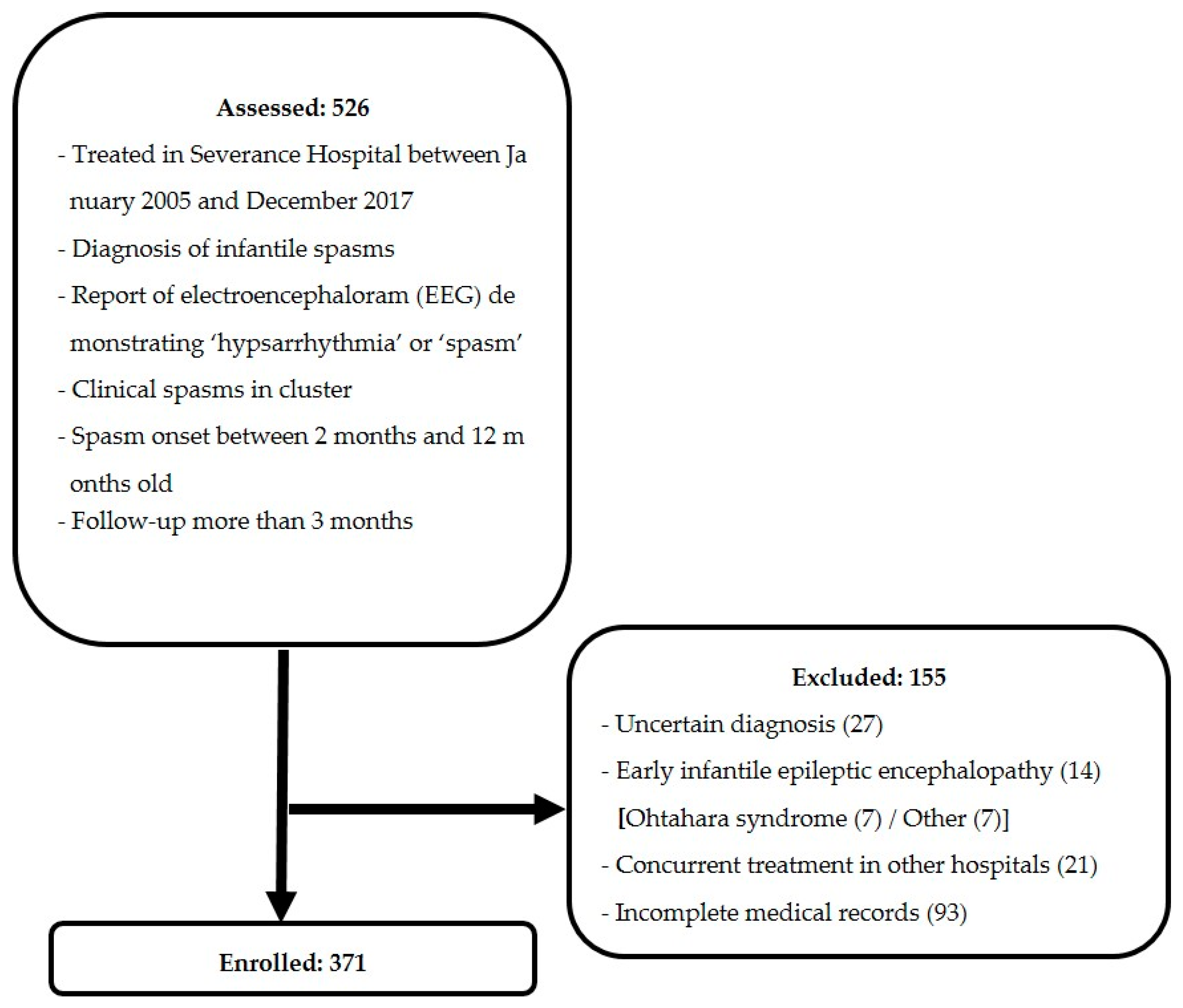
2.1. Study Design and Subjects
2.2. Outcome Measurement
2.3. Statistical Analysis
3. Results
3.1. Patient Characteristics
3.2. First-Line Treatment
3.3. Second-Line Treatment
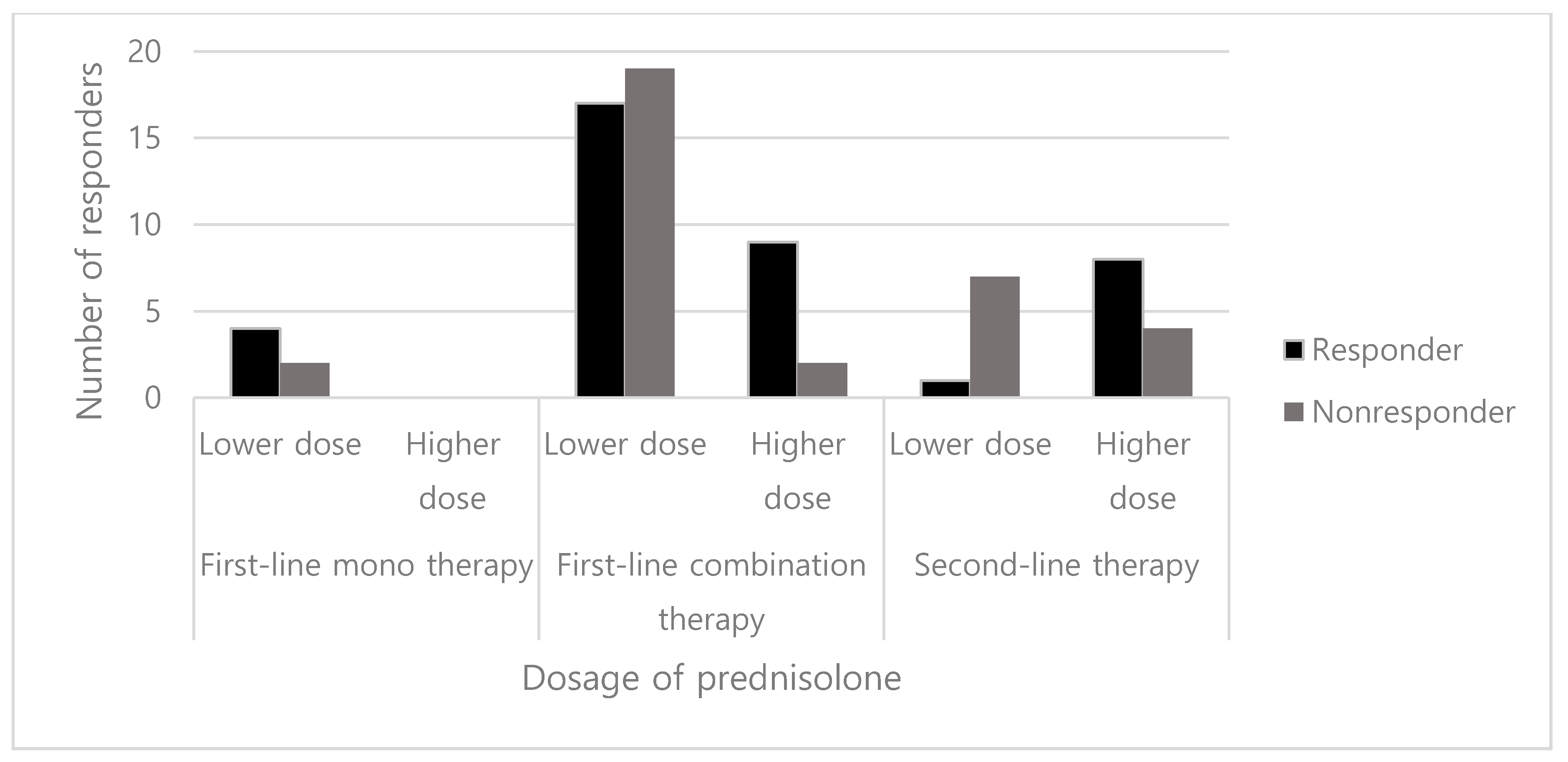
3.4. Dosage of Prednisolone
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hancock, E.C.; Osborne, J.P.; Edwards, S.W. Treatment of infantile spasms. Cochrane Database Syst. Rev. 2013, CD001770. [Google Scholar] [CrossRef] [PubMed]
- Pellock, J.M.; Hrachovy, R.; Shinnar, S.; Baram, T.Z.; Bettis, D.; Dlugos, D.J.; Gaillard, W.D.; Gibson, P.A.; Holmes, G.L.; Nordl, D.R.; et al. Infantile spasms: A U.S. consensus report. Epilepsia 2010, 51, 2175–2189. [Google Scholar] [CrossRef] [PubMed]
- D’Alonzo, R.; Rigante, D.; Mencaroni, E.; Esposito, S. West Syndrome: A Review and Guide for Paediatricians. Clin. Drug Investig. 2018, 38, 113–124. [Google Scholar] [CrossRef] [PubMed]
- O’Callaghan, F.J.; Lux, A.L.; Darke, K.; Edwards, S.W.; Hancock, E.; Johnson, A.L.; Kennedy, C.R.; Newton, R.W.; Verity, C.M.; Osborne, J.P. The effect of lead time to treatment and of age of onset on developmental outcome at 4 years in infantile spasms: Evidence from the United Kingdom Infantile Spasms Study. Epilepsia 2011, 52, 1359–1364. [Google Scholar] [CrossRef] [PubMed]
- Wilmshurst, J.M.; Gaillard, W.D.; Vinayan, K.P.; Tsuchida, T.N.; Plouin, P.; Van Bogaert, P.; Carrizosa, J.; Elia, M.; Craiu, D.; Jovic, N.J.; et al. Summary of recommendations for the management of infantile seizures: Task Force Report for the ILAE Commission of Pediatrics. Epilepsia 2015, 56, 1185–1197. [Google Scholar] [CrossRef] [PubMed]
- Tsao, C.Y. Current trends in the treatment of infantile spasms. Neuropsychiatr. Dis. Treat. 2009, 5, 289–299. [Google Scholar] [CrossRef][Green Version]
- Lerner, J.T.; Salamon, N.; Sankar, R. Clinical profile of vigabatrin as monotherapy for treatment of infantile spasms. Neuropsychiatr. Dis. Treat. 2010, 6, 731–740. [Google Scholar] [CrossRef][Green Version]
- Lux, A.L.; Edwards, S.W.; Hancock, E.; Johnson, A.L.; Kennedy, C.R.; Newton, R.W.; O’Callaghan, F.J.K.; Verity, C.M.; Osborne, J.P. The United Kingdom Infantile Spasms Study comparing vigabatrin with prednisolone or tetracosactide at 14 days: A multicentre, randomised controlled trial. Lancet 2004, 364, 1773–1778. [Google Scholar] [CrossRef]
- Go, C.Y.; Mackay, M.T.; Weiss, S.K.; Stephens, D.; Adams-Webber, T.; Ashwal, S.; Snead, O.C., 3rd. Evidence-based guideline update: Medical treatment of infantile spasms. Report of the Guideline Development Subcommittee of the American Academy of Neurology and the Practice Committee of the Child Neurology Society. Neurology 2012, 78, 1974–1980. [Google Scholar] [CrossRef]
- Lux, A.L.; Edwards, S.W.; Hancock, E.; Johnson, A.L.; Kennedy, C.R.; Newton, R.W.; O’Callaghan, F.J.K.; Verity, C.M.; Osborne, J.P. The United Kingdom Infantile Spasms Study (UKISS) comparing hormone treatment with vigabatrin on developmental and epilepsy outcomes to age 14 months: A multicentre randomised trial. Lancet Neurol. 2005, 4, 712–717. [Google Scholar] [CrossRef]
- Mohamed, B.P.; Scott, R.C.; Desai, N.; Gutta, P.; Patil, S. Seizure outcome in infantile spasms—A retrospective study. Epilepsia 2011, 52, 746–752. [Google Scholar] [CrossRef]
- Hahn, J.; Lee, H.; Kang, H.-C.; Lee, J.S.; Kim, H.D.; Kim, S.H.; Chang, M.J. Clobazam as an adjunctive treatment for infantile spasms. Epilepsy & Behavior 2019, 95, 161–165. [Google Scholar]
- Knupp, K.G.; Leister, E.; Coryell, J.; Nickels, K.C.; Ryan, N.; Juarez-Colunga, E.; Gaillard, W.D.; Mytinger, J.R.; Berg, A.T.; Millichap, J.; et al. Response to second treatment after initial failed treatment in a multicenter prospective infantile spasms cohort. Epilepsia 2016, 57, 1834–1842. [Google Scholar] [CrossRef]
- Rajaraman, R.R.; Lay, J.; Alayari, A.; Anderson, K.; Sankar, R.; Hussain, S.A. Prevention of infantile spasms relapse: Zonisamide and topiramate provide no benefit. Epilepsia 2016, 57, 1280–1287. [Google Scholar] [CrossRef]
- Zhu, X.; Chen, O.; Zhang, D.; Jin, R.; Li, F.; Wang, Y.; Sun, R. A prospective study on the treatment of infantile spasms with first-line topiramate followed by low-dose ACTH. Epilepsy Res. 2011, 93, 149–154. [Google Scholar] [CrossRef]
- Lawlor, K.M.; Devlin, A.M. Levetiracetam in the treatment of infantile spasms. Eur. J. Paediatr. Neurol. 2005, 9, 19–22. [Google Scholar] [CrossRef]
- Suzuki, Y.; Nagai, T.; Ono, J.; Imai, K.; Otani, K.; Tagawa, T.; Abe, J.; Shiomi, M.; Okada, S. Zonisamide monotherapy in newly diagnosed infantile spasms. Epilepsia 1997, 38, 1035–1038. [Google Scholar] [CrossRef]
- O’Callaghan, F.J.K.; Edwards, S.W.; Alber, F.D.; Hancock, E.; Johnson, A.L.; Kennedy, C.R.; Likeman, M.; Lux, A.L.; Mackay, M.; Mallick, A.A.; et al. Safety and effectiveness of hormonal treatment versus hormonal treatment with vigabatrin for infantile spasms (ICISS): A randomised, multicentre, open-label trial. Lancet Neurol. 2017, 16, 33–42. [Google Scholar] [CrossRef]
- Knupp, K.G. Hormonal therapy with vigabatrin is superior to hormonal therapy alone in infantile spasms. J. Pediatrics 2017, 184, 235–238. [Google Scholar] [CrossRef]
- Sakakihara, Y. Treatment of West syndrome. Brain Dev. 2011, 33, 202–206. [Google Scholar] [CrossRef]
- Lux, A.L.; Osborne, J.P. A proposal for case definitions and outcome measures in studies of infantile spasms and West syndrome: Consensus statement of the West Delphi group. Epilepsia 2004, 45, 1416–1428. [Google Scholar] [CrossRef] [PubMed]
- Kleinman, L.C.; Norton, E.C. What’s the Risk? A simple approach for estimating adjusted risk measures from nonlinear models including logistic regression. Health Serv. Res. 2009, 44, 288–302. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.A. Treatment of infantile spasms. Epilepsia Open 2018, 3, 143–154. [Google Scholar] [CrossRef]
- Ko, A.; Youn, S.E.; Chung, H.J.; Kim, S.H.; Lee, J.S.; Kim, H.D.; Kang, H.C. Vigabatrin and high-dose prednisolone therapy for patients with West syndrome. Epilepsy research 2018, 145, 127–133. [Google Scholar] [CrossRef]
- Chellamuthu, P.; Sharma, S.; Jain, P.; Kaushik, J.S.; Seth, A.; Aneja, S. High dose (4 mg/kg/day) versus usual dose (2 mg/kg/day) oral prednisolone for treatment of infantile spasms: An open-label, randomized controlled trial. Epilepsy Res. 2014, 108, 1378–1384. [Google Scholar] [CrossRef]
- Kossoff, E.H.; Hartman, A.L.; Rubenstein, J.E.; Vining, E.P. High-dose oral prednisolone for infantile spasms: An effective and less expensive alternative to ACTH. Epilepsy Behav. 2009, 14, 674–676. [Google Scholar] [CrossRef]
- Kelley, S.A.; Knupp, K.G. Infantile Spasms-Have We Made Progress? Curr. Neurol. Neurosci. Rep. 2018, 18, 27. [Google Scholar] [CrossRef]
- Pavone, P.; Striano, P.; Falsaperla, R.; Pavone, L.; Ruggieri, M. Infantile spasms syndrome, West syndrome and related phenotypes: What we know in 2013. Brain Dev. 2014, 36, 739–751. [Google Scholar] [CrossRef]
| Characteristic | Treatment Group a | p Value | ||||
|---|---|---|---|---|---|---|
| Vigabatrin n = 271 | Prednisolone n = 6 | Vigabatrin + Prednisolone n = 47 | Non-Standard n = 47 | Total n = 371 | ||
| Sex Male Female | 163 (60.1) 108 (39.9) | 1 (16.7) 5 (83.3) | 21 (44.7) 26 (55.3) | 30 (63.8) 17 (36.2) | 215 (58.0) 156 (42.0) | 0.032 †,* |
| Presence of seizure history | 97 (35.8) | 0 (0.0) | 16 (34.0) | 15 (31.9) | 128 (34.5) | 0.320 † |
| Age at spasm onset, mo. | 5.8 (4.4, 7.3) | 7.7 (5.1, 8.7) | 5.7 (4.4, 6.7) | 5.7 (4.4, 7.4) | 5.8 (4.4, 7.3) | 0.719 ‡ |
| Age at treatment, mo. | 6.6 (5.3, 8.1) | 8.1 (5.4, 8.9) | 6.6 (5.5, 8.0) | 7.1 (5.3, 8.8) | 6.6 (5.3, 8.2) | 0.804 ‡ |
| Lag time from spasm onset to treatment, days | 12.0 (5.0, 29.0) | 7.0 (4.3, 19.5) | 20.0 (11.5, 43.0) | 20.0 (7.0, 56.0) | 14.0 (5.0, 32.0) | 0.012 ‡,* |
| Etiology Structural Metabolic Infection Genetic Unknown | 87 (32.1) 23 (8.5) 6 (2.2) 7 (2.6) 148 (54.6) | 1 (16.7) 0 (0) 0 (0) 0 (0) 5 (83.3) | 15 (31.9) 2 (4.3) 0 (0) 1 (2.1) 29 (61.7) | 12 (25.5) 2 (4.3) 1 (2.1) 1 (2.1) 31 (66.0) | 115 (31.0) 27 (7.3) 7 (1.9) 9 (2.4) 213 (57.4) | 0.938 § |
| Response to Initial treatment a | Time to Cessation of Spasms (days) b | Relapse Rate a | ||
|---|---|---|---|---|
| Treatment | Response n = 141 | Non-Response n = 230 | ||
| Vigabatrin | 106 (39.1) | 165 (60.9) | 5 (3, 9) | 8 (7.5) |
| Prednisolone | 4 (66.7) | 2 (33.3) | 4 (3, 7) | 1 (25.0) |
| Vigabatrin + prednisolone | 26 (55.3) | 21 (44.7) | 5 (2, 9) | 3 (11.5) |
| Non-standard | 5 (10.6) | 42 (89.4) | 4 (2, 7) | 2 (40.0) |
| Characteristic | Responders n (%) | p value † | Crude Risk Ratio (95% CI) | Adjusted a Risk Ratio (95% CI) | Adjusted b Risk Ratio (95% CI) |
|---|---|---|---|---|---|
| Treatment | |||||
| Vigabatrin | 106 (39.1) | REF | REF | REF | |
| Prednisolone | 4 (66.7) | 0.219 | 3.113 (0.560, 17.296) | 2.602 (0.465, 14.560) | 2.980 (0.523, 16.975) |
| Vigabatrin + prednisolone | 26 (55.3) | 0.037 * | 1.927 (1.032, 3.599) | 1.929 (1.028, 3.620) | 2.139 (1.124, 4.069) |
| Non-standard | 5 (10.6) | <0.001 * | 0.185 (0.071, 0.483) | 0.179 (0.068, 0.468) | 0.205 (0.078, 0.539) |
| Seizure history | |||||
| No | 102 (42.0) | 0.030 * | REF | REF | - |
| Yes | 39 (30.5) | 0.606 (0.385, 0.954) | 0.593 (0.371, 0.949) | - | |
| Lag time | |||||
| ≤4 weeks | 116 (43.8) | <0.001 * | REF | - | REF |
| >4 weeks | 25 (23.6) | 0.396 (0.238, 0.660) | - | 0.406 (0.239, 0.689) |
| Second-Line Treatment | Vigabatrin | Prednisolone | Non-Standard | |
|---|---|---|---|---|
| First-Line Treatment | ||||
| Vigabatrin | 5/5, 100% (up-titration) | 9/20, 45% | 24/140, 17% | |
| Prednisolone | 2/2, 100% | - | - | |
| Vigabatrin + prednisolone | 1/1, 100% (up-titration) | - | 2/20, 10% | |
| Non-standard | 13/31, 42% | 0/1, 0% | 2/10, 20% | |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hahn, J.; Park, G.; Kang, H.-C.; Lee, J.S.; Kim, H.D.; Kim, S.H.; Chang, M.J. Optimized Treatment for Infantile Spasms: Vigabatrin versus Prednisolone versus Combination Therapy. J. Clin. Med. 2019, 8, 1591. https://doi.org/10.3390/jcm8101591
Hahn J, Park G, Kang H-C, Lee JS, Kim HD, Kim SH, Chang MJ. Optimized Treatment for Infantile Spasms: Vigabatrin versus Prednisolone versus Combination Therapy. Journal of Clinical Medicine. 2019; 8(10):1591. https://doi.org/10.3390/jcm8101591
Chicago/Turabian StyleHahn, Jongsung, Gyunam Park, Hoon-Chul Kang, Joon Soo Lee, Heung Dong Kim, Se Hee Kim, and Min Jung Chang. 2019. "Optimized Treatment for Infantile Spasms: Vigabatrin versus Prednisolone versus Combination Therapy" Journal of Clinical Medicine 8, no. 10: 1591. https://doi.org/10.3390/jcm8101591
APA StyleHahn, J., Park, G., Kang, H.-C., Lee, J. S., Kim, H. D., Kim, S. H., & Chang, M. J. (2019). Optimized Treatment for Infantile Spasms: Vigabatrin versus Prednisolone versus Combination Therapy. Journal of Clinical Medicine, 8(10), 1591. https://doi.org/10.3390/jcm8101591





