Sex Differences in the Relation between Waist Circumference within the Normal Range and Development of Reflux Esophagitis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Population
2.2. Measurements
2.3. Statistical Analysis
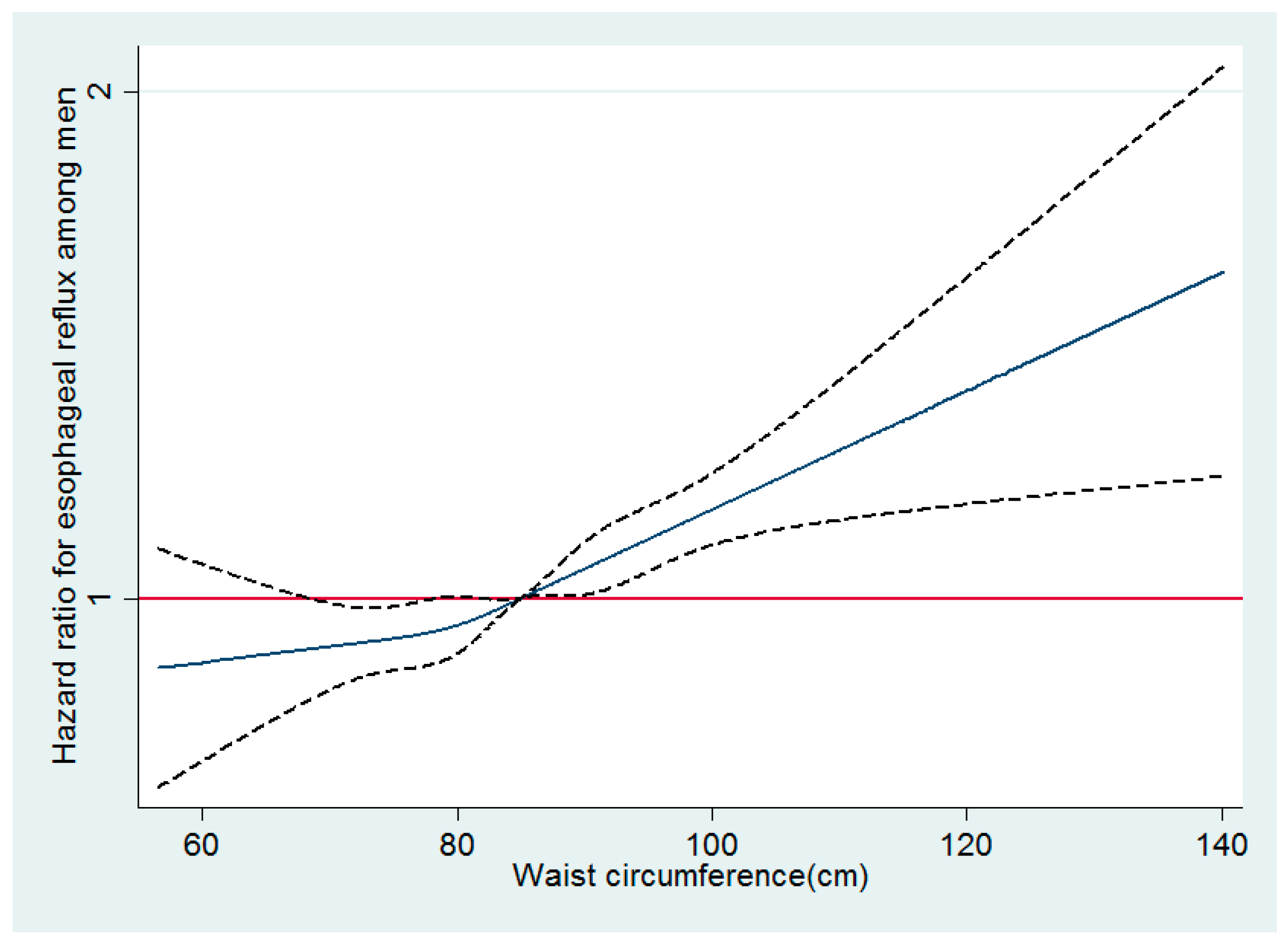
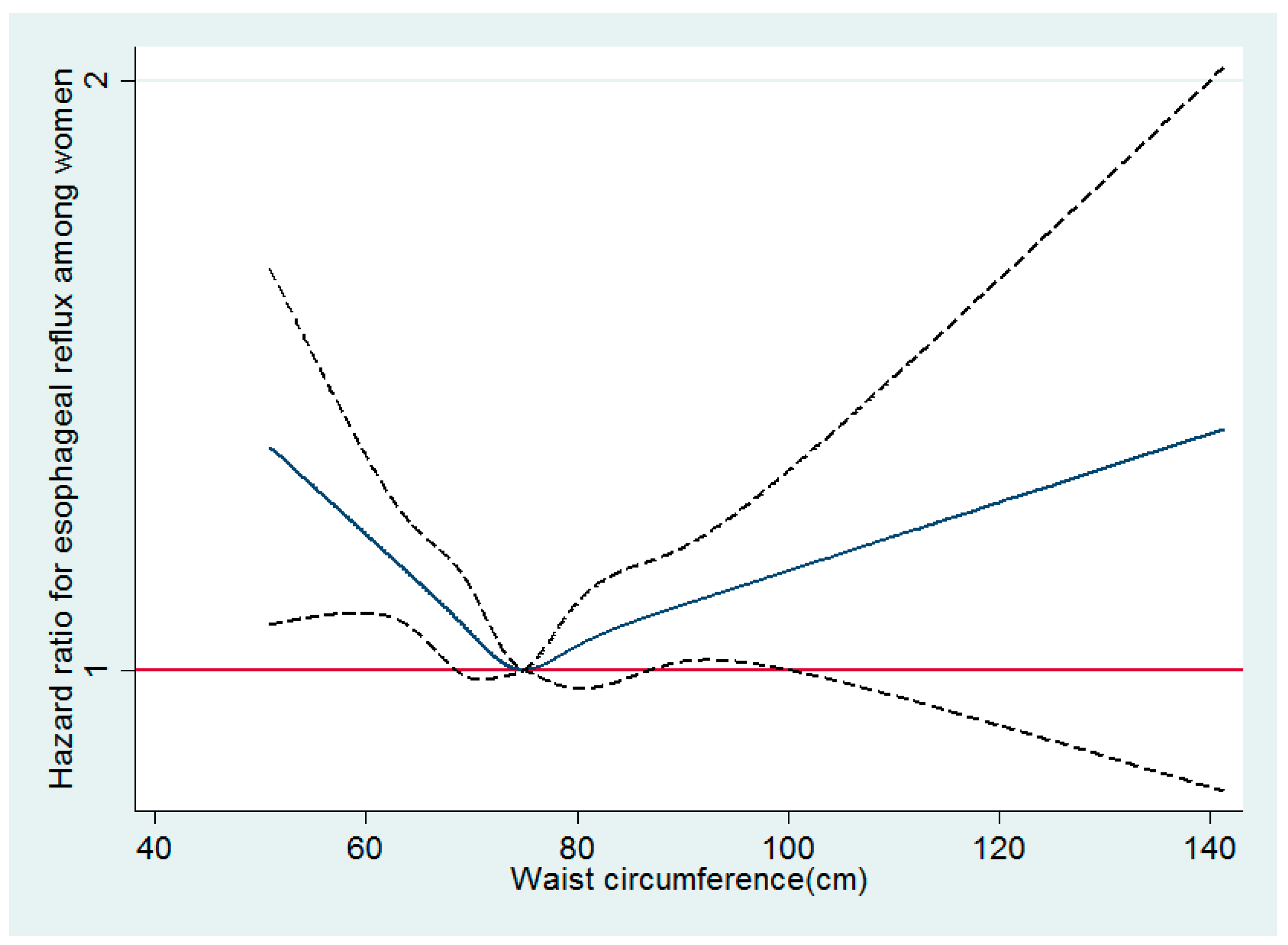
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Peery, A.F.; Dellon, E.S.; Lund, J.; Crockett, S.D.; McGowan, C.E.; Bulsiewicz, W.J.; Gangarosa, L.M.; Thiny, M.T.; Stizenberg, K.; Morgan, D.R.; et al. Burden of gastrointestinal disease in the United States: 2012 update. Gastroenterology 2012, 143, 1179–1187. [Google Scholar] [CrossRef] [PubMed]
- Fock, K.M.; Talley, N.; Goh, K.L.; Sugano, K.; Katelaris, P.; Holtmann, G.; Pandolfino, J.E.; Sharma, P.; Ang, T.L.; Hongo, M.; et al. Asia-Pacific consensus on the management of gastro-oesophageal reflux disease: An update focusing on refractory reflux disease and Barrett’s oesophagus. Gut 2016, 65, 1402–1415. [Google Scholar] [CrossRef] [PubMed]
- Corley, D.A.; Kubo, A.; Zhao, W. Abdominal obesity, ethnicity and gastro-oesophageal reflux symptoms. Gut 2007, 56, 756–762. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Singh, S.; Sharma, A.N.; Murad, M.H.; Buttar, N.S.; El-Serag, H.B.; Katzka, D.A.; Iyer, P.G. Central adiposity is associated with increased risk of esophageal inflammation, metaplasia, and adenocarcinoma: A systematic review and meta-analysis. Clin. Gastroenterol. Hepatol. 2013, 11, 1399.e7–1412.e7. [Google Scholar] [CrossRef] [PubMed]
- Nam, S.Y.; Choi, I.J.; Ryu, K.H.; Park, B.J.; Kim, H.B.; Nam, B.H. Abdominal visceral adipose tissue volume is associated with increased risk of erosive esophagitis in men and women. Gastroenterology 2010, 139, 1902–1911. [Google Scholar] [CrossRef] [PubMed]
- Pandolfino, J.E.; El-Serag, H.B.; Zhang, Q.; Shah, N.; Ghosh, S.K.; Kahrilas, P.J. Obesity: A challenge to esophagogastric junction integrity. Gastroenterology 2006, 130, 639–649. [Google Scholar] [CrossRef] [PubMed]
- Robertson, E.V.; Derakhshan, M.H.; Wirz, A.A.; Lee, Y.Y.; Seenan, J.P.; Ballantyne, S.A.; Hanvey, S.L.; Kelman, A.W.; Going, J.J.; McColl, K.E. Central obesity in asymptomatic volunteers is associated with increased intrasphincteric acid reflux and lengthening of the cardiac mucosa. Gastroenterology 2013, 145, 730–739. [Google Scholar] [CrossRef] [PubMed]
- Rieder, F.; Biancani, P.; Harnett, K.; Yerian, L.; Falk, G.W. Inflammatory mediators in gastroesophageal reflux disease: Impact on esophageal motility, fibrosis, and carcinogenesis. Am. J. Physiol. Gastrointest. Liver Physiol. 2010, 298, G571–G581. [Google Scholar] [CrossRef] [PubMed]
- Zagari, R.M.; Fuccio, L.; Wallander, M.A.; Johansson, S.; Fiocca, R.; Casanova, S.; Farahmand, B.Y.; Winchester, C.C.; Roda, E.; Bazzoli, F. Gastro-oesophageal reflux symptoms, oesophagitis and Barrett’s oesophagus in the general population: The Loiano-Monghidoro study. Gut 2008, 57, 1354–1359. [Google Scholar] [CrossRef]
- Labenz, J.; Jaspersen, D.; Kulig, M.; Leodolter, A.; Lind, T.; Meyer-Sabellek, W.; Stolte, M.; Vieth, M.; Willich, S.; Malfertheiner, P. Risk factors for erosive esophagitis: A multivariate analysis based on the ProGERD study initiative. Am. J. Gastroenterol. 2004, 99, 1652–1656. [Google Scholar] [CrossRef]
- Masaka, T.; Iijima, K.; Endo, H.; Asanuma, K.; Ara, N.; Ishiyama, F.; Asano, N.; Koike, T.; Imatani, A.; Shimosegawa, T. Gender differences in oesophageal mucosal injury in a reflux oesophagitis model of rats. Gut 2013, 62, 6–14. [Google Scholar] [CrossRef]
- Yasuhara, H.; Miyake, Y.; Toyokawa, T.; Matsumoto, K.; Takahara, M.; Imada, T.; Yagi, S.; Miyatake, H.; Nakatsu, M.; Ando, M.; et al. Large waist circumference is a risk factor for reflux esophagitis in Japanese males. Digestion 2010, 81, 181–187. [Google Scholar] [CrossRef] [PubMed]
- Fujiwara, Y.; Higuchi, K.; Shiba, M.; Yamamori, K.; Watanabe, Y.; Sasaki, E.; Tominaga, K.; Watanabe, T.; Oshitani, N.; Arakawa, T. Differences in clinical characteristics between patients with endoscopy-negative reflux disease and erosive esophagitis in Japan. Am. J. Gastroenterol. 2005, 100, 754–758. [Google Scholar] [CrossRef] [PubMed]
- Hongo, M.; Miwa, H.; Kusano, M.; J-FAST group. Symptoms and quality of life in underweight gastroesophageal reflux disease patients and therapeutic responses to proton pump inhibitors. J. Gastroenterol. Hepatol. 2012, 27, 913–918. [Google Scholar] [CrossRef] [PubMed]
- Chang, Y.; Ryu, S.; Choi, Y.; Zhang, Y.; Cho, J.; Kwon, M.J.; Hyun, Y.Y.; Lee, K.B.; Kim, H.; Jung, H.S.; et al. Metabolically Healthy Obesity and Development of Chronic Kidney Disease: A Cohort Study. Ann. Intern. Med. 2016, 164, 305–312. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.J.; Chang, Y.; Park, S.K.; Jung, Y.S.; Park, J.H.; Park, D.I.; Cho, Y.K.; Ryu, S.; Sohn, C.I. Nonalcoholic Fatty Liver Disease Is Associated with Increased Risk of Reflux Esophagitis. Dig. Dis. Sci. 2017, 62, 3605–3613. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization; Regional Office for the Western Pacific. The Asia-Pacific Perspective: Redefining Obesity and its Treatment; Health Communications Australia: Sydney, Australia, 2000. [Google Scholar]
- Alberti, K.G.; Eckel, R.H.; Grundy, S.M.; Zimmet, P.Z.; Cleeman, J.I.; Donato, K.A.; Fruchart, J.C.; James, W.P.; Loria, C.M.; Smith, S.C., Jr.; et al. Harmonizing the metabolic syndrome: A joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 2009, 120, 1640–1645. [Google Scholar] [CrossRef]
- Lee, S.; Park, H.; Kim, S.; Kwon, H.; Kim, D.; Kim, D.; Cho, G.; Han, J.; Kim, S.; Park, C.; et al. Cut-off points of waist circumference for defining abdominal obesity in the Korean population. Korean J. Obes. 2006, 15, 1–9. [Google Scholar]
- Hoshihara, Y. [Endoscopic findings of GERD]. Nihon Rinsho. Jpn. J. Clin. Med. 2004, 62, 1459–1464. [Google Scholar]
- Royston, P.; Parmar, M.K. Flexible parametric proportional-hazards and proportional-odds models for censored survival data, with application to prognostic modelling and estimation of treatment effects. Stat. Med. 2002, 21, 2175–2197. [Google Scholar] [CrossRef]
- Sogabe, M.; Okahisa, T.; Kimura, Y.; Hibino, S.; Yamanoi, A. Visceral fat predominance is associated with erosive esophagitis in Japanese men with metabolic syndrome. Eur. J. Gastroenterol. Hepatol. 2012, 24, 910–916. [Google Scholar] [CrossRef] [PubMed]
- Tai, C.M.; Lee, Y.C.; Tu, H.P.; Huang, C.K.; Wu, M.T.; Chang, C.Y.; Lee, C.T.; Wu, M.S.; Lin, J.T.; Wang, W.M. The relationship between visceral adiposity and the risk of erosive esophagitis in severely obese Chinese patients. Obesity 2010, 18, 2165–2169. [Google Scholar] [CrossRef] [PubMed]
- Koo, J.S.; Lee, S.W.; Park, S.M.; Jung, S.W.; Yim, H.J.; Park, J.J.; Chun, H.J.; Lee, H.S.; Choi, J.H.; Kim, C.D.; et al. Abdominal obesity as a risk factor for the development of erosive esophagitis in subjects with a normal esophago-gastric junction. Gut Liver 2009, 3, 276–284. [Google Scholar] [CrossRef] [PubMed]
- Xi, B.; Mi, J.; Zhao, M.; Zhang, T.; Jia, C.; Li, J.; Zeng, T.; Steffen, L.M.; Public Health Youth Collaborative and Innovative Study Group of Shandong University. Trends in abdominal obesity among U.S. children and adolescents. Pediatrics 2014, 134, e334–e339. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.E.; Han, K.; Kang, Y.M.; Kim, S.O.; Cho, Y.K.; Ko, K.S.; Park, J.Y.; Lee, K.U.; Koh, E.H.; Taskforce Team of Diabetes Fact Sheet of the Korean Diabetes Association. Trends in the prevalence of metabolic syndrome and its components in South Korea: Findings from the Korean National Health Insurance Service Database (2009–2013). PLoS ONE 2018, 13, e0194490. [Google Scholar] [CrossRef]
- Zhang, Y.X.; Wang, Z.X.; Zhao, J.S.; Chu, Z.H. The current prevalence and regional disparities in general and central obesity among children and adolescents in Shandong, China. Int. J. Cardiol. 2017, 227, 89–93. [Google Scholar] [CrossRef] [PubMed]
- Mitchell, D.R.; Derakhshan, M.H.; Wirz, A.A.; Ballantyne, S.A.; McColl, K.E.L. Abdominal Compression by Waist Belt Aggravates Gastroesophageal Reflux, Primarily by Impairing Esophageal Clearance. Gastroenterology 2017, 152, 1881–1888. [Google Scholar] [CrossRef] [Green Version]
- Derakhshan, M.H.; Robertson, E.V.; Fletcher, J.; Jones, G.R.; Lee, Y.Y.; Wirz, A.A.; McColl, K.E. Mechanism of association between BMI and dysfunction of the gastro-oesophageal barrier in patients with normal endoscopy. Gut 2012, 61, 337–343. [Google Scholar] [CrossRef]
- Lee, Y.Y.; Wirz, A.A.; Whiting, J.G.; Robertson, E.V.; Smith, D.; Weir, A.; Kelman, A.W.; Derakhshan, M.H.; McColl, K.E. Waist belt and central obesity cause partial hiatus hernia and short-segment acid reflux in asymptomatic volunteers. Gut 2014, 63, 1053–1060. [Google Scholar] [CrossRef]
- Vartanian, L.R.; Dey, S. Self-concept clarity, thin-ideal internalization, and appearance-related social comparison as predictors of body dissatisfaction. Body Image 2013, 10, 495–500. [Google Scholar] [CrossRef]
- Kim, T.J.; Oh, J.H.; Pyo, J.H.; Lee, H.; Min, Y.W.; Min, B.-H.; Lee, J.H.; Rhee, P.-L.; Kim, J.J.K. Sarcopenia as a Leading Risk Factor of Erosive Esophagitis. Gastroenterology 2018, 154. [Google Scholar] [CrossRef]
| Characteristics | Overall | Quartiles of Waist Circumference (cm) | p Value | |||
|---|---|---|---|---|---|---|
| Quartile 1 (56.5–80) | Quartile 2 (80.1–85) | Quartile 3 (85.1–90) | Quartile 4 (90.1–140.1) | |||
| Number | 77,245 | 20,065 | 20,239 | 18,855 | 18,086 | <0.001 |
| Age (years) 1 | 39.0 (8.1) | 37.8 (7.8) | 39.0 (8.1) | 39.7 (8.3) | 39.5 (8.2) | <0.001 |
| Obesity (%) | 38.8 | 1.8 | 17.2 | 51.4 | 90.9 | <0.001 |
| Current smoker (%) | 36.5 | 34.9 | 34.8 | 37.1 | 39.8 | <0.001 |
| Alcohol intake (%) 2 | 30.0 | 22.6 | 28.4 | 32.4 | 37.2 | <0.001 |
| Vigorous exercise (%) 3 | 15.8 | 16.9 | 16.6 | 15.4 | 14.0 | <0.001 |
| High education level (%) 4 | 88.8 | 89.4 | 89.4 | 88.5 | 87.7 | <0.001 |
| Diabetes (%) | 3.9 | 1.9 | 3.2 | 4.3 | 6.4 | <0.001 |
| Hypertension (%) | 16.0 | 8.5 | 13.1 | 17.7 | 25.7 | <0.001 |
| Medication for dyslipidemia (%) | 2.0 | 0.8 | 1.6 | 2.1 | 3.4 | <0.001 |
| BMI (kg/m2) | 24.4 (2.8) | 21.6 (1.7) | 23.6 (1.4) | 25.1 (1.5) | 27.7 (2.3) | <0.001 |
| Systolic BP (mmHg) 1 | 115.1 (11.7) | 111.7 (11.1) | 114.1 (11.3) | 115.8 (11.4) | 119.1 (11.7) | <0.001 |
| Diastolic BP (mmHg) 1 | 74.7 (9.1) | 72.4 (8.5) | 74.0 (8.8) | 75.3 (9.0) | 77.3 (9.2) | <0.001 |
| Glucose (mg/dL) 1 | 95.5 (15.3) | 92.3 (13.1) | 94.8 (14.1) | 96.5 (15.2) | 98.9 (18.0) | <0.001 |
| Uric acid (mg/dL) 1 | 6.2 (1.2) | 5.8 (1.1) | 6.1 (1.2) | 6.3 (1.2) | 6.5 (1.3) | <0.001 |
| Total cholesterol (mg/dL) 1 | 198.1 (33.8) | 188.2 (31.4) | 197.6 (32.9) | 202.1 (34.2) | 205.3 (34.5) | <0.001 |
| LDL-C (mg/dL) 1 | 123.1 (30.5) | 122.6 (28.3) | 122.8 (29.6) | 126.9 (30.3) | 130.8 (31.1) | <0.001 |
| HDL-C (mg/dL) 1 | 52.6 (12.0) | 57.6 (12.8) | 53.1 (11.7) | 50.7 (10.9) | 48.3 (10.3) | <0.001 |
| Triglycerides (mg/dL) 5 | 114 (81–164) | 87 (66–119) | 110 (80–154) | 126 (90–178) | 144 (104–201) | <0.001 |
| ALT (U/L) 5 | 24 (18–35) | 19 (15–25) | 23 (17–31) | 27 (20–37) | 33 (24–48) | <0.001 |
| HOMA-IR 5 | 1.58 (1.03–2.23) | 1.24 (0.75–1.76) | 1.47 (0.96–2.04) | 1.68 (1.15–2.33) | 2.05 (1.43–2.89) | <0.001 |
| hsCRP (mg/L) 5 | 0.5 (0.3–1.0) | 0.3 (0.2–0.6) | 0.5 (0.3–0.9) | 0.6 (0.3–1.1) | 0.8 (0.5–1.5) | <0.001 |
| Characteristics | Overall | Quartiles of Waist Circumference (cm) | p Value | |||
|---|---|---|---|---|---|---|
| Quartile 1 (50.9–69.2) | Quartile 2 (69.3–74.0) | Quartile 3 (74.1–79.5) | Quartile 4 (79.6–141.2) | |||
| Number | 65,434 | 16,423 | 16,778 | 16,061 | 16,172 | <0.001 |
| Age (years) 1 | 38.7 (8.3) | 36.1 (6.6) | 37.7 (7.2) | 39.3 (8.1) | 41.8 (9.9) | <0.001 |
| Obesity (%) | 12.5 | <0.001 | 0.6 | 5.0 | 44.8 | <0.001 |
| Current smoker (%) | 3.0 | 3.1 | 2.9 | 2.7 | 3.2 | 0.930 |
| Alcohol intake (%) 2 | 4.4 | 3.2 | 4.4 | 4.4 | 5.8 | <0.001 |
| Vigorous exercise (%) 3 | 13.5 | 12.0 | 13.2 | 13.9 | 14.9 | <0.001 |
| High education level (%) 4 | 75.8 | 83.2 | 79.6 | 75.0 | 65.4 | <0.001 |
| Diabetes (%) | 1.6 | 0.4 | 0.7 | 1.3 | 3.9 | <0.001 |
| Hypertension (%) | 5.9 | 1.9 | 3.0 | 5.8 | 13.1 | <0.001 |
| Medication for dyslipidemia (%) | 1.2 | 0.3 | 0.7 | 1.0 | 2.9 | <0.001 |
| BMI (kg/m2) | 21.7 (3.0) | 19.2 (1.5) | 20.7 (1.5) | 22.0 (1.7) | 25.1 (2.9) | <0.001 |
| Systolic BP (mmHg) 1 | 104.1 (12.4) | 101.2 (10.9) | 102.4 (11.5) | 104.2 (12.2) | 108.8 (13.5) | <0.001 |
| Diastolic BP (mmHg) 1 | 66.9 (8.9) | 65.4 (8.0) | 66.0 (8.5) | 66.9 (8.9) | 69.4 (9.6) | <0.001 |
| Glucose (mg/dL) 1 | 90.8 (11.4) | 88.1 (8.4) | 89.5 (8.9) | 91.0 (10.6) | 94.7 (15.4) | <0.001 |
| Uric acid (mg/dL) 1 | 4.2 (0.9) | 4.0 (0.8) | 4.1 (0.8) | 4.2 (0.8) | 4.5 (0.9) | <0.001 |
| Total cholesterol (mg/dL) 1 | 186.2 (32.1) | 179.8 (28.8) | 182.9 (30.5) | 187.4 (32.1) | 195.1 (34.6) | <0.001 |
| LDL-C (mg/dL) 1 | 107.4 (28.6) | 97.9 (24.1) | 103.3 (26.5) | 109.6 (28.2) | 119.1 (30.7) | <0.001 |
| HDL-C (mg/dL) 1 | 63.4 (14.2) | 68.2 (14.1) | 65.3 (13.9) | 62.3 (13.7) | 57.8 (13.1) | <0.001 |
| Triglycerides (mg/dL) 5 | 72 (55–97) | 62 (50–79) | 67 (53–89) | 73 (57–98) | 90 (66–126) | <0.001 |
| ALT (U/L) 5 | 14 (11–18) | 13 (10–17) | 13 (10–17) | 14 (11–18) | 16 (12–23) | <0.001 |
| HOMA-IR 5 | 1.34 (0.83–1.93) | 1.20 (0.72–1.72) | 1.21 (0.76–1.76) | 1.31 (0.84–1.90) | 1.66 (1.10–2.39) | <0.001 |
| hsCRP (mg/L) 5 | 0.3 (0.2–0.6) | 0.2 (0.1–0.4) | 0.2 (0.2–0.5) | 0.3 (0.2–0.6) | 0.6 (0.3–1.2) | <0.001 |
| Quartiles of Waist Circumference (cm) | Person-Years | Incident Case | Incidence Density (Per 1000 Person-Years) | Age-Adjusted HR (95% CI) | Multivariate HR 1 (95% CI) | |
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | |||||
| Men | ||||||
| Quartile 1 (56.5-80) | 86,074.6 | 5027 | 58.4 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| Quartile 2 (80.1-85) | 81,053.4 | 4967 | 61.3 | 1.08 (1.04–1.13) | 1.03 (0.99–1.07) | 1.02 (0.98–1.07) |
| Quartile 3 (85.1-90) | 72,998.0 | 4777 | 65.4 | 1.17 (1.13–1.22) | 1.08 (1.04–1.12) | 1.07 (1.02–1.12) |
| Quartile 4 (90.1-140.1) | 64,878.3 | 4790 | 73.8 | 1.34 (1.29–1.40) | 1.15 (1.10–1.19) | 1.13 (1.06–1.21) |
| p for trend | <0.001 | <0.001 | <0.001 | |||
| Women | ||||||
| Quartile 1 (50.9–69.2) | 68,561.4 | 2723 | 39.7 | 0.91 (0.86–0.96) | 1.10 (1.04–1.17) | 1.07 (1.01–1.14) |
| Quartile 2 (69.3–74.0) | 64,214.7 | 2530 | 39.4 | 0.95 (0.90–1.01) | 1.03 (0.98–1.10) | 1.02 (0.96–1.08) |
| Quartile 3 (74.1–79.5) | 58,297.0 | 2309 | 39.6 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| Quartile 4 (79.6–141.2) | 55,800.4 | 2386 | 42.8 | 1.15 (1.09–1.22) | 1.07 (1.01–1.13) | 1.10 (1.03–1.17) |
| p for quadratic | 0.046 | <0.001 | 0.002 | |||
| Quartiles of Waist Circumference (cm) | Person-Years | Incident Case | Incidence Density (Per 1000 Person-Years) | Age-Adjusted HR (95% CI) | Multivariate HR 1 (95% CI) | |
|---|---|---|---|---|---|---|
| Model 1 | Model 2 | |||||
| Men | ||||||
| Q1 (56.5~78.3) | 62,817.9 | 3610 | 57.5 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| Q2 (78.4~82.5) | 59,991.6 | 3686 | 61.4 | 1.10 (1.05–1.15) | 1.05 (1.00–1.10) | 1.04 (0.99–1.10) |
| Q3 (82.6~86.0) | 60,832.1 | 3780 | 62.1 | 1.12 (1.07–1.18) | 1.05 (1.01–1.10) | 1.05 (0.99–1.10) |
| Q4 (86.1~89.9) | 51,213.0 | 3375 | 65.9 | 1.21 (1.15–1.27) | 1.09 (1.04–1.15) | 1.08 (1.02–1.15) |
| Abdominal obesity (≥90) | 70,149.7 | 5110 | 72.8 | 1.35 (1.30–1.41) | 1.16 (1.11–1.21) | 1.14 (1.06–1.22) |
| p for trend | <0.001 | <0.001 | <0.001 | |||
| Women | ||||||
| Q1 (50.9~68.8) | 61,497.0 | 2467 | 40.1 | 0.93 (0.87–0.98) | 1.10 (1.04–1.17) | 1.06 (1.00–1.14) |
| Q2 (68.9~73.0) | 58,559.5 | 2266 | 38.7 | 0.94 (0.89–0.99) | 1.02 (0.96–1.08) | 1.01 (0.95–1.07) |
| Q3 (73.1~77.4) | 51,177.0 | 2024 | 39.5 | 1.00 (reference) | 1.00 (reference) | 1.00 (reference) |
| Q4 (77.5~84.9) | 51,625.9 | 2137 | 41.4 | 1.10 (0.98–1.16) | 1.04 (0.98–1.11) | 1.06 (1.00–1.13) |
| Abdominal obesity (≥85) | 24,014.2 | 1054 | 43.9 | 1.22 (0.99–1.33) | 1.07 (0.99–1.15) | 1.14 (1.03–1.25) |
| p for quadratic | <0.001 | 0.001 | 0.004 | |||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yang, H.-J.; Chang, Y.; Park, S.-K.; Jung, Y.S.; Park, J.H.; Park, D.I.; Ryu, S.; Sohn, C.I. Sex Differences in the Relation between Waist Circumference within the Normal Range and Development of Reflux Esophagitis. J. Clin. Med. 2019, 8, 67. https://doi.org/10.3390/jcm8010067
Yang H-J, Chang Y, Park S-K, Jung YS, Park JH, Park DI, Ryu S, Sohn CI. Sex Differences in the Relation between Waist Circumference within the Normal Range and Development of Reflux Esophagitis. Journal of Clinical Medicine. 2019; 8(1):67. https://doi.org/10.3390/jcm8010067
Chicago/Turabian StyleYang, Hyo-Joon, Yoosoo Chang, Soo-Kyung Park, Yoon Suk Jung, Jung Ho Park, Dong Il Park, Seungho Ryu, and Chong Il Sohn. 2019. "Sex Differences in the Relation between Waist Circumference within the Normal Range and Development of Reflux Esophagitis" Journal of Clinical Medicine 8, no. 1: 67. https://doi.org/10.3390/jcm8010067
APA StyleYang, H.-J., Chang, Y., Park, S.-K., Jung, Y. S., Park, J. H., Park, D. I., Ryu, S., & Sohn, C. I. (2019). Sex Differences in the Relation between Waist Circumference within the Normal Range and Development of Reflux Esophagitis. Journal of Clinical Medicine, 8(1), 67. https://doi.org/10.3390/jcm8010067





