Hospitalization Length after Myocardial Infarction: Risk-Assessment-Based Time of Hospital Discharge vs. Real Life Practice
Abstract
1. Introduction
2. Experimental Section
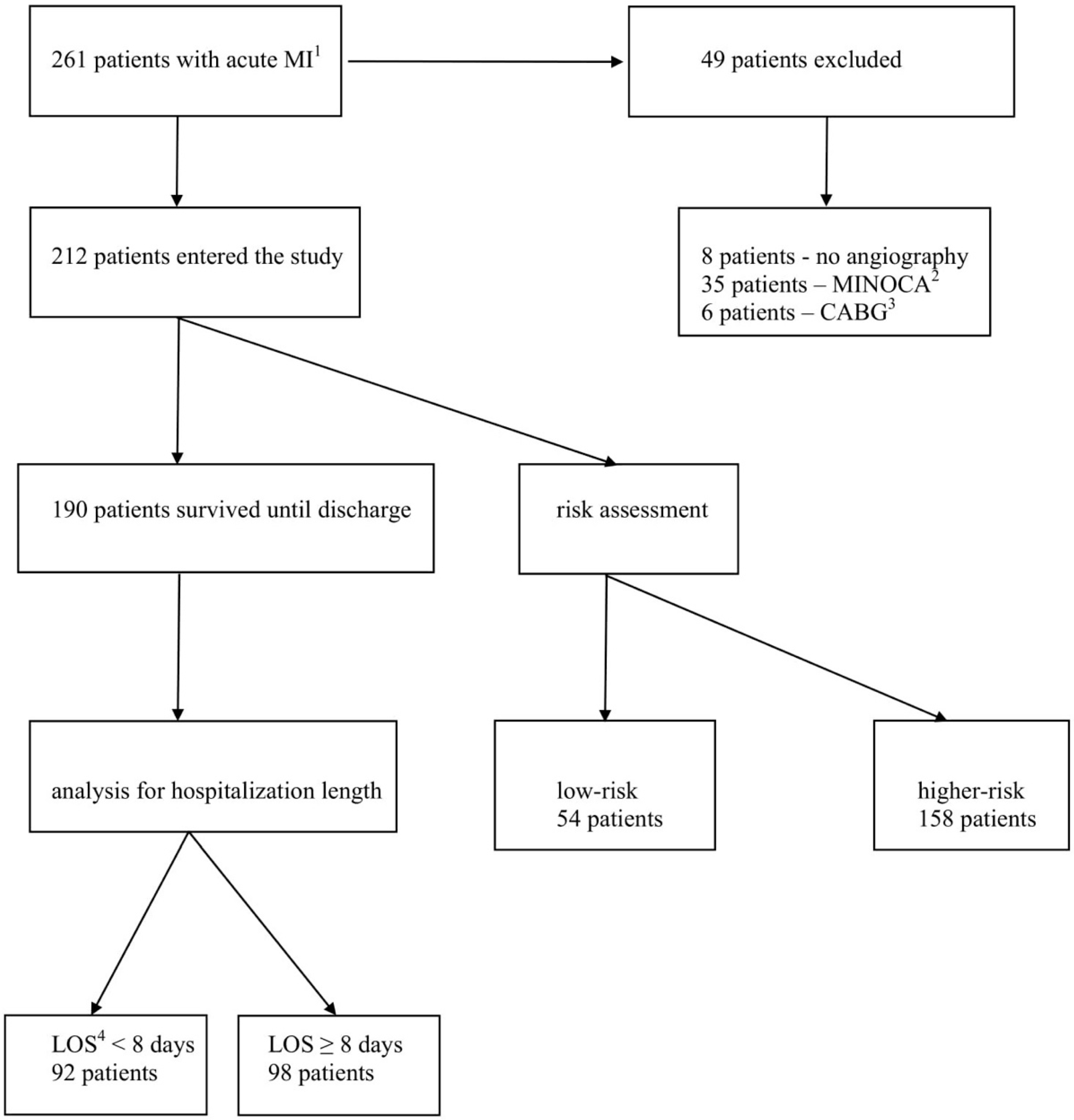
2.1. Study Population
2.2. Statistical Analysis
3. Results
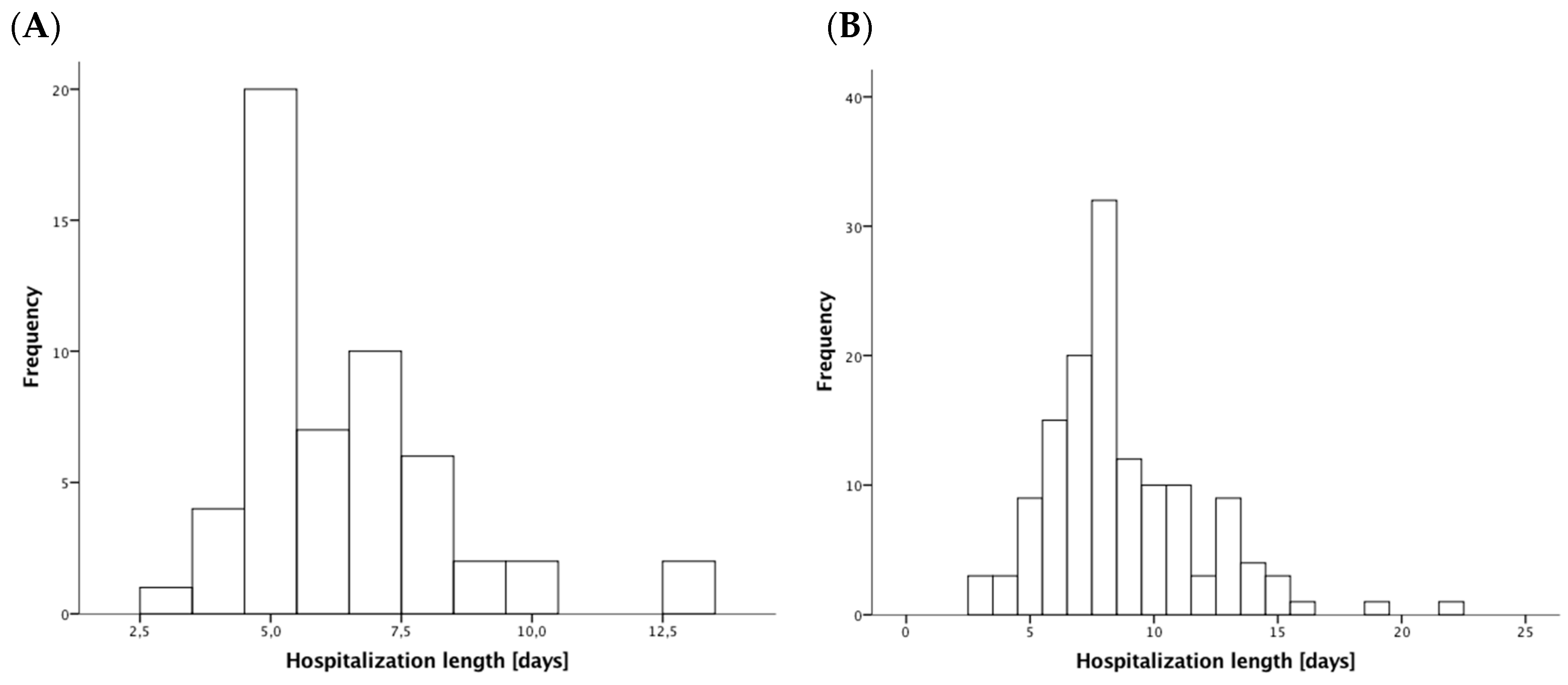
3.1. Patients’ Characteristics
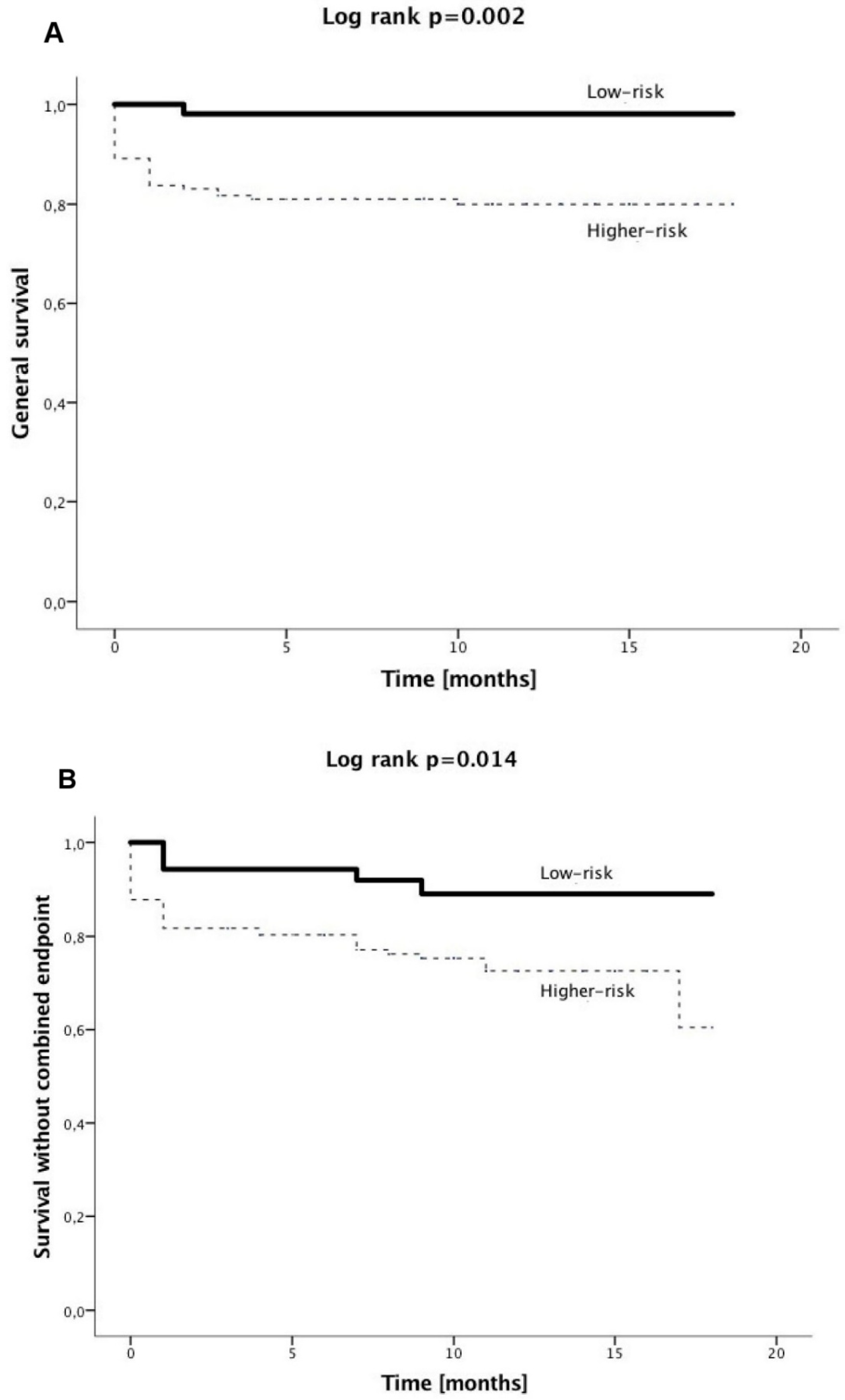
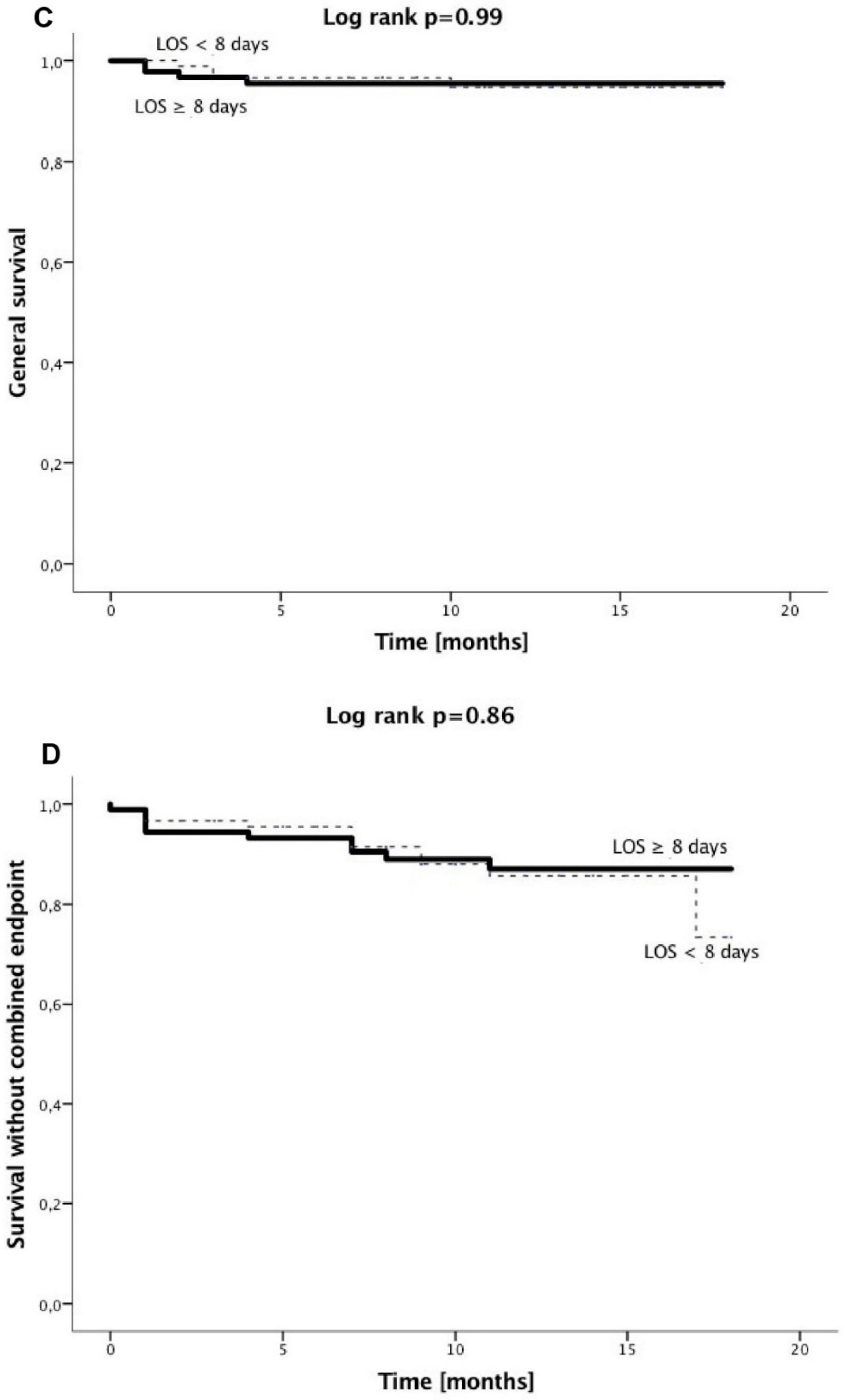
3.2. Clinical Outcome
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Azzalini, L.; Solé, E.; Sans, J.; Vila, M.; Durán, A.; Gil-Alonso, D.; Santaló, M.; Garcia-Moll, X.; Sionis, A. Feasibility and safety of an early discharge strategy after low-risk acute myocardial infarction treated with primary percutaneous coronary intervention: The EDAMI pilot trial. Cardiology 2015, 130, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Melberg, T.; Jørgensen, M.; Ørn, S.; Solli, T.; Edland, U.; Dickstein, K. Safety and health status following early discharge in patients with acute myocardial infarction treated with primary PCI: A randomized trial. Eur. J. Prev. Cardiol. 2015, 22, 1427–1434. [Google Scholar] [CrossRef] [PubMed]
- Noman, A.; Zaman, A.G.; Schechter, C.; Balasubramaniam, K.; Das, R. Early discharge after primary percutaneous coronary intervention for ST-elevation myocardial infarction. Eur. Heart J. Acute Cardiovasc. Care 2013, 2, 262–269. [Google Scholar] [CrossRef] [PubMed]
- Jones, D.A.; Rathod, K.S.; Howard, J.P.; Gallagher, S.; Antoniou, S.; De Palma, R.; Guttmann, O.; Cliffe, S.; Colley, J.; Butler, J.; et al. Safety and feasibility of hospital discharge 2 days following primary percutaneous intervention for ST-segment elevation myocardial infarction. Heart 2012, 98, 1722–1727. [Google Scholar] [CrossRef] [PubMed]
- Topol, E.J.; Burek, K.; O’Neill, W.W.; Kewman, D.G.; Kander, N.H.; Shea, M.J.; Schork, M.A.; Kirscht, J.; Juni, J.E.; Pitt, B. A randomized controlled trial of hospital discharge three days after myocardial infarction in the era of reperfusion. N. Engl. J. Med. 1988, 318, 1083–1088. [Google Scholar] [CrossRef] [PubMed]
- Bogaty, P.; Dumont, S.; O’Hara, G.E.; Boyer, L.; Auclair, L.; Jobin, J.; Boudreault, J.R. Randomized trial of a noninvasive strategy to reduce hospital stay for patients with low-risk myocardial infarction. J. Am. Coll. Cardiol. 2001, 37, 1289–1296. [Google Scholar] [CrossRef]
- Chen, E.; Naylor, C.D. Variation in hospital length of stay for acute myocardial infarction in Ontario, Canada. Med. Care 1994, 32, 420–435. [Google Scholar] [CrossRef] [PubMed]
- Every, N.R.; Spertus, J.; Fihn, S.D.; Hlatky, M.; Martin, J.S.; Weaver, W.D. Length of hospital stay after acute myocardial infarction in the Myocardial Infarction Triage and Intervention (MITI) Project registry. J. Am. Coll. Cardiol. 1996, 28, 287–293. [Google Scholar] [CrossRef]
- Kinjo, K.; Sato, H.; Nakatani, D.; Mizuno, H.; Shimizu, M.; Hishida, E.; Ezumi, A.; Hoshida, S.; Koretsune, Y.; Hori, M.; et al. Predictors of length of hospital stay after acute myocardial infarction in Japan. Circ. J. 2004, 68, 809–815. [Google Scholar] [CrossRef] [PubMed]
- Grines, C.L.; Marsalese, D.L.; Brodie, B.; Griffin, J.; Donohue, B.; Costantini, C.R.; Balestrini, C.; Stone, G.; Wharton, T.; Esente, P.; et al. Safety and cost-effectiveness of early discharge after primary angioplasty in low risk patients with acute myocardial infarction. J. Am. Coll. Cardiol. 1998, 31, 967–972. [Google Scholar] [CrossRef]
- Hutter, A.M., Jr.; Sidel, V.W.; Shine, K.I.; De Sanctis, R.W. Early hospital discharge after myocardial infarction. N. Engl. J. Med. 1973, 288, 1141–1144. [Google Scholar] [CrossRef] [PubMed]
- Wenger, N.K.; Hellerstein, H.K.; Blackburn, H.; Castranova, S.J. Uncomplicated myocardial infarction. Current physician practice in patient management. JAMA 1973, 224, 511–514. [Google Scholar] [CrossRef] [PubMed]
- Ahlmark, G.; Ahlberg, G.; Saetre, H.; Haglund, I.; Korsgren, M. A controlled study of early discharge after uncomplicated myocardial infarction. Acta Med. Scand. 1979, 206, 87–91. [Google Scholar] [CrossRef] [PubMed]
- McNeer, J.F.; Wagner, G.S.; Ginsburg, P.B.; Wallace, A.G.; McCants, C.B.; Conley, M.J.; Rosati, R.A. Hospital discharge one week after acute myocardial infarction. N. Engl. J. Med. 1978, 298, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Morrow, D.A.; Antman, E.M.; Charlesworth, A.; Cairns, R.; Murphy, S.A.; de Lemos, J.A.; Giugliano, R.P.; McCabe, C.H.; Braunwald, E. TIMI risk score for ST-elevation myocardial infarction: A convenient, bedside, clinical score for risk assessment at presentation: An intravenous nPA for treatment of infarcting myocardium early II trial substudy. Circulation 2000, 102, 2031–2037. [Google Scholar] [CrossRef] [PubMed]
- Fox, K.A.; Anderson, F.A., Jr.; Dabbous, O.H.; Steg, P.G.; López-Sendón, J.; Van de Werf, F.; Gurfinkel, E.P.; Goodman, S.G.; Brieger, D. Intervention in acute coronary syndromes: Do patients undergo intervention on the basis of their risk characteristics? The Global Registry of Acute Coronary Events (GRACE). Heart 2007, 93, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.L.; Woodlief, L.H.; Topol, E.J.; Weaver, W.D.; Betriu, A.; Col, J.; Simoons, M.; Aylward, P.; Van de Werf, F.; Califf, R.M. Predictors of 30-day mortality in the era of reperfusion for acute myocardial infarction. Results from an international trial of 41,021 patients. Circulation 1995, 91, 1659–1668. [Google Scholar] [CrossRef] [PubMed]
- De Luca, G.; Suryapranata, H.; van’t Hof, A.W.; de Boer, M.J.; Hoorntje, J.C.; Dambrink, J.H.; Gosselink, A.T.; Ottervanger, J.P.; Zijlstra, F. Prognostic assessment of patients with acute myocardial infarction treated with primary angioplasty: Implications for early discharge. Circulation 2004, 109, 2737–2743. [Google Scholar] [CrossRef] [PubMed]
- Ibanez, B.; James, S.; Agewall, S.; Antunes, M.J.; Bucciarelli-Ducci, C.; Bueno, H.; Caforio, A.L.P.; Crea, F.; Goudevenos, J.A.; Halvorsen, S.; et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur. Heart J. 2018, 39, 119–177. [Google Scholar] [CrossRef] [PubMed]
- Spencer, F.A.; Lessard, D.; Gore, J.M.; Yarzebski, J.; Goldberg, R.J. Declining length of hospital stay for acute myocardial infarction and postdischarge outcomes: A community-wide perspective. Arch. Int. Med. 2004, 164, 733–740. [Google Scholar] [CrossRef] [PubMed]
- Berger, A.K.; Duval, S.; Jacobs, D.R., Jr.; Barber, C.; Vazquez, G.; Lee, S.; Luepker, R.V. Relation of length of hospital stay in acute myocardial infarction to postdischarge mortality. Am. J. Cardiol. 2008, 101, 428–434. [Google Scholar] [CrossRef] [PubMed]
- Rogers, W.J.; Canto, J.G.; Lambrew, C.T.; Tiefenbrunn, A.J.; Kinkaid, B.; Shoultz, D.A.; Frederick, P.D.; Every, N. Temporal trends in the treatment of over 1.5 million patients with myocardial infarction in the US from 1990 through 1999: The National Registry of Myocardial Infarction 1, 2 and 3. J. Am. Coll. Cardiol. 2000, 36, 2056–2063. [Google Scholar] [CrossRef]
- Alonso Salinas, G.L.; Sanmartin, M.; Pascual Izco, M.; Rincon, L.M.; Martin-Acuna, A.; Pastor Pueyo, P.; Del Val Martín, D.; Marco Del Castillo, Á.; Recio-Mayoral, A.; Martin-Asenjo, R.; et al. The role of frailty in acute coronary syndromes in the elderly. Gerontology 2018, 64, 422–429. [Google Scholar] [CrossRef] [PubMed]
| Patients Surviving until Hospital Discharge (n = 190) | All Patients (n = 212) | |||||
|---|---|---|---|---|---|---|
| LOS 8 <8 Days (92 Patients) | LOS ≥8 Days (98 Patients) | p-Value | Higher-Risk (158 Patients) | Low-Risk (54 Patients) | p-Value | |
| Baseline presentation | ||||||
| ST-elevation MI 1 (%) | 22 | 37 | 0.03 | 33 | 24 | 0.24 |
| Age (years) | 64 ± 11 | 69 ± 12 | 0.003 | 71±11 | 57 ± 8 | <0.001 |
| Male gender (%) | 71 | 64 | 0.36 | 63 | 76 | 0.097 |
| Hypertension history (%) | 82 | 82 | 1.0 | 79 | 78 | 0.85 |
| Diabetes history (%) | 29 | 41 | 0.13 | 41 | 24 | 0.03 |
| COPD history 2 (%) | 9 | 14 | 0.26 | 13 | 7 | 0.45 |
| Smoking (%) | 48 | 45 | 0.77 | 38 | 65 | 0.001 |
| Stroke history (%) | 8 | 11 | 0.46 | 11 | 2 | 0.048 |
| MI history (%) | 29 | 23 | 0.41 | 27 | 22 | 0.59 |
| In-hospital characteristics | ||||||
| LVEF 3 (%) | 55 (Q1: 45; Q3: 60) | 45 (Q1: 38; Q3: 55) | <0.001 | 45 (Q1: 37 Q3: 52) | 56 (Q1: 50 Q3: 60) | <0.001 |
| LAD 4 culprit (%) | 29 | 40 | 0.17 | 39 | 30 | 0.25 |
| Multi-vessel disease (%) | 23 | 48 | <0.001 | 48 | 0 | <0.001 |
| Staged revascularization (%) | 14 | 33 | 0.003 | 28 | 4 | <0.001 |
| Ventricular arrhythmia (%) | 9 | 16 | 0.13 | 11 | 0 | 0.008 |
| GFR 5 (mL/min/1.73 m2) | 85 ± 28 | 77 ± 34 | 0.08 | 72 ± 33 | 92 ± 23 | <0.001 |
| RBC 6 transfusion (%) | 2 | 4 | 0.68 | 4 | 2 | 0.68 |
| Respiratory infections (%) | 6 | 20 | 0.006 | 19 | 6 | 0.017 |
| ACEI/ARB 7 (%) | 88 | 88 | 1.0 | 78 | 91 | 0.04 |
| B-blocker (%) | 88 | 90 | 0.82 | 80 | 89 | 0.21 |
| Loop diuretics (%) | 24 | 42 | 0.009 | 47 | 9 | <0.001 |
| Aldosterone antagonists (%) | 13 | 33 | 0.002 | 28 | 6 | <0.001 |
| ST-Elevation MI 1 (65 Patients) | Non-ST-Elevation MI (147 Patients) | p-Value | |
|---|---|---|---|
| Baseline presentation | |||
| Age (years) | 67 ± 13 | 67 ± 11 | 0.93 |
| Male gender (%) | 60 | 69 | 0.21 |
| Hypertension history (%) | 71 | 82 | 0.07 |
| Diabetes history (%) | 35 | 37 | 0.88 |
| COPD history 2 (%) | 11 | 12 | 1.0 |
| Smoking (%) | 48 | 43 | 0.65 |
| Stroke history (%) | 6 | 9 | 0.59 |
| MI history (%) | 12 | 31 | 0.003 |
| Low-risk (%) | 20 | 28 | 0.24 |
| In-hospital characteristics | |||
| Length of hospital stay (d) | 8 (Q1: 7; Q3: 9) | 7 (Q1: 6; Q3: 10) | 0.19 |
| LVEF 3 (%) | 45 (Q1: 38; Q3: 55) | 50 (Q1: 40; Q3: 55) | 0.14 |
| LAD 4 culprit (%) | 45 | 33 | 0.12 |
| Multi-vessel disease (%) | 31 | 38 | 0.35 |
| Staged revascularization (%) | 20 | 22 | 0.86 |
| Ventricular arrhythmia (%) | 11 | 7 | 0.41 |
| GFR 5 (mL/min/1.73 m2) | 87 ± 35 | 73 ± 30 | 0.006 |
| RBC 6 transfusion (%) | 5 | 3 | 0.7 |
| Respiratory infections (%) | 15 | 16 | 1.0 |
| ACEI/ARB 7 (%) | 78 | 83 | 0.44 |
| B-blocker (%) | 80 | 84 | 0.56 |
| Loop diuretics (%) | 36 | 38 | 0.76 |
| Aldosterone antagonists (%) | 31 | 18 | 0.04 |
| Multi-Vessel Disease (76 Patients) | No Multi-Vessel Disease (136 Patients) | p-Value | |
|---|---|---|---|
| Baseline presentation | |||
| ST-elevation MI 1 (%) | 26 | 33 | 0.35 |
| Age (years) | 67 ± 10 | 67 ± 12 | 0.72 |
| Male gender (%) | 71 | 64 | 0.36 |
| Hypertension history (%) | 72 | 82 | 0.11 |
| Diabetes history (%) | 41 | 34 | 0.37 |
| COPD history 2 (%) | 8 | 13 | 0.27 |
| Smoking (%) | 46 | 44 | 0.89 |
| Stroke history (%) | 7 | 10 | 0.61 |
| MI history (%) | 24 | 26 | 0.74 |
| Low-risk (%) | 0 | 40 | <0.001 |
| In-hospital characteristics | |||
| Length of hospital stay (d) | 8 (Q1: 7; Q3: 10) | 7 (Q1: 5; Q3: 9) | <0.001 |
| LVEF 3 (%) | 45 (Q1: 39; Q3: 55) | 50 (Q1: 40; Q3: 58) | 0.14 |
| LAD 4 culprit (%) | 34 | 38 | 0.66 |
| Staged revascularization (%) | 54 | 4 | <0.001 |
| Ventricular arrhythmia (%) | 9 | 7 | 0.61 |
| GFR 5 (mL/min/1.73 m2) | 81 ± 35 | 76 ± 30 | 0.31 |
| RBC 6 transfusion (%) | 3 | 4 | 0.71 |
| Respiratory infections (%) | 16 | 15 | 1.0 |
| ACEI/ARB 7 (%) | 77 | 84 | 0.27 |
| B-blocker (%) | 83 | 82 | 1.0 |
| Loop diuretics (%) | 33 | 40 | 0.37 |
| Aldosterone antagonists (%) | 17 | 24 | 0.29 |
| Univariate Analysis | Multivariate Analysis | |||||
|---|---|---|---|---|---|---|
| OR 7 | 95% CI 8 | p-Value | OR | 95% CI | p-Value | |
| Baseline characteristics | ||||||
| Age (per one year increase) | 1.04 | 1.01–1.07 | 0.004 | 1.04 | 1.01–1.07 | 0.016 |
| Female gender | 1.3 | 0.7–2.4 | 0.35 | |||
| Arterial hypertension | 1.0 | 0.48–2.1 | 0.98 | |||
| Diabetes mellitus | 1.7 | 0.91–3.0 | 0.1 | |||
| History of MI 1 | 0.74 | 0.4–1.4 | 0.36 | |||
| History of CABG 2 | 0.69 | 0.15–3.2 | 0.64 | |||
| History of stroke | 1.5 | 0.57–4.1 | 0.4 | |||
| Smoking | 0.89 | 0.5–1.6 | 0.69 | |||
| Hyperlipidemia | 0.87 | 0.47–1.6 | 0.64 | |||
| COPD 3 | 1.75 | 0.7–4.4 | 0.23 | |||
| Atrial fibrillation | 2.1 | 0.97–4.7 | 0.06 | |||
| Hemodialysis | 1.9 | 0.34–10.7 | 0.46 | |||
| In hospital characteristics | ||||||
| ST-elevation MI | 2.09 | 1.1–4.0 | 0.025 | 2.3 | 1.1–4.7 | 0.02 |
| LVEF 4 (per 1% increase) | 0.95 | 0.93–0.98 | 0.001 | 0.97 | 0.94–0.99 | 0.016 |
| Multi-vessel disease | 3.1 | 1.7–5.8 | <0.001 | 3.4 | 1.7–6.6 | <0.001 |
| Ventricular arrhythmia | 2.2 | 0.7–7.5 | 0.2 | |||
| RBC 5 transfusion | 1.9 | 0.3–10.7 | 0.46 | |||
| Pneumonia | 3.7 | 1.4– 9.6 | 0.008 | |||
| GFR 6 (per 1 mL/min/1.73 m2 increase) | 0.9 | 0.98–1.0 | 0.09 | |||
| Patients Surviving until Hospital Discharge (n = 190) | All Patients (n = 212) | |||||
|---|---|---|---|---|---|---|
| LOS 2 <8 Days (92 Patients) | LOS ≥8 Days (98 Patients) | p-Value | Higher-Risk (158 Patients) | Low-Risk (54 Patients) | p-Value | |
| In hospital outcomes | ||||||
| All-cause mortality (%) | - | - | - | 14 | 0 | 0.001 |
| Cardiovascular mortality (%) | - | - | - | 14 | 0 | 0.001 |
| All recurrent MI 1 (%) | 0 | 0 | - | 0 | 0 | - |
| Non-fatal recurrent MI (%) | 0 | 0 | - | 0 | 0 | - |
| All stroke (%) | 1 | 1 | 1.0 | 2 | 0 | 0.57 |
| Non-fatal stroke (%) | 1 | 1 | 1.0 | 1 | 0 | 1.0 |
| Combined endpoint (%) | 1 | 1 | 1.0 | 15 | 0 | 0.001 |
| Long-term outcomes | ||||||
| All-cause mortality (%) | 4 | 4 | 1.0 | 18 | 2 | 0.001 |
| Cardiovascular mortality (%) | 0 | 2 | 0.5 | 15 | 0 | 0.001 |
| All recurrent MI (%) | 11 | 7 | 0.45 | 8 | 9 | 0.77 |
| Non-fatal recurrent MI (%) | 11 | 6 | 0.3 | 7 | 9 | 0.56 |
| All stroke (%) | 2 | 2 | 1.0 | 4 | 0 | 0.34 |
| Non-fatal stroke (%) | 2 | 2 | 1.0 | 2 | 0 | 0.57 |
| Combined endpoint (%) | 12 | 10 | 0.82 | 24 | 9 | 0.02 |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Węgiel, M.; Dziewierz, A.; Wojtasik-Bakalarz, J.; Sorysz, D.; Surdacki, A.; Bartuś, S.; Dudek, D.; Rakowski, T. Hospitalization Length after Myocardial Infarction: Risk-Assessment-Based Time of Hospital Discharge vs. Real Life Practice. J. Clin. Med. 2018, 7, 564. https://doi.org/10.3390/jcm7120564
Węgiel M, Dziewierz A, Wojtasik-Bakalarz J, Sorysz D, Surdacki A, Bartuś S, Dudek D, Rakowski T. Hospitalization Length after Myocardial Infarction: Risk-Assessment-Based Time of Hospital Discharge vs. Real Life Practice. Journal of Clinical Medicine. 2018; 7(12):564. https://doi.org/10.3390/jcm7120564
Chicago/Turabian StyleWęgiel, Michał, Artur Dziewierz, Joanna Wojtasik-Bakalarz, Danuta Sorysz, Andrzej Surdacki, Stanisław Bartuś, Dariusz Dudek, and Tomasz Rakowski. 2018. "Hospitalization Length after Myocardial Infarction: Risk-Assessment-Based Time of Hospital Discharge vs. Real Life Practice" Journal of Clinical Medicine 7, no. 12: 564. https://doi.org/10.3390/jcm7120564
APA StyleWęgiel, M., Dziewierz, A., Wojtasik-Bakalarz, J., Sorysz, D., Surdacki, A., Bartuś, S., Dudek, D., & Rakowski, T. (2018). Hospitalization Length after Myocardial Infarction: Risk-Assessment-Based Time of Hospital Discharge vs. Real Life Practice. Journal of Clinical Medicine, 7(12), 564. https://doi.org/10.3390/jcm7120564






