Propensity Score-Matched Analysis of the Survival Benefit from Kidney Transplantation in Patients with End-Stage Renal Disease
Abstract
1. Introduction
2. Materials and Methods
2.1. Data Source
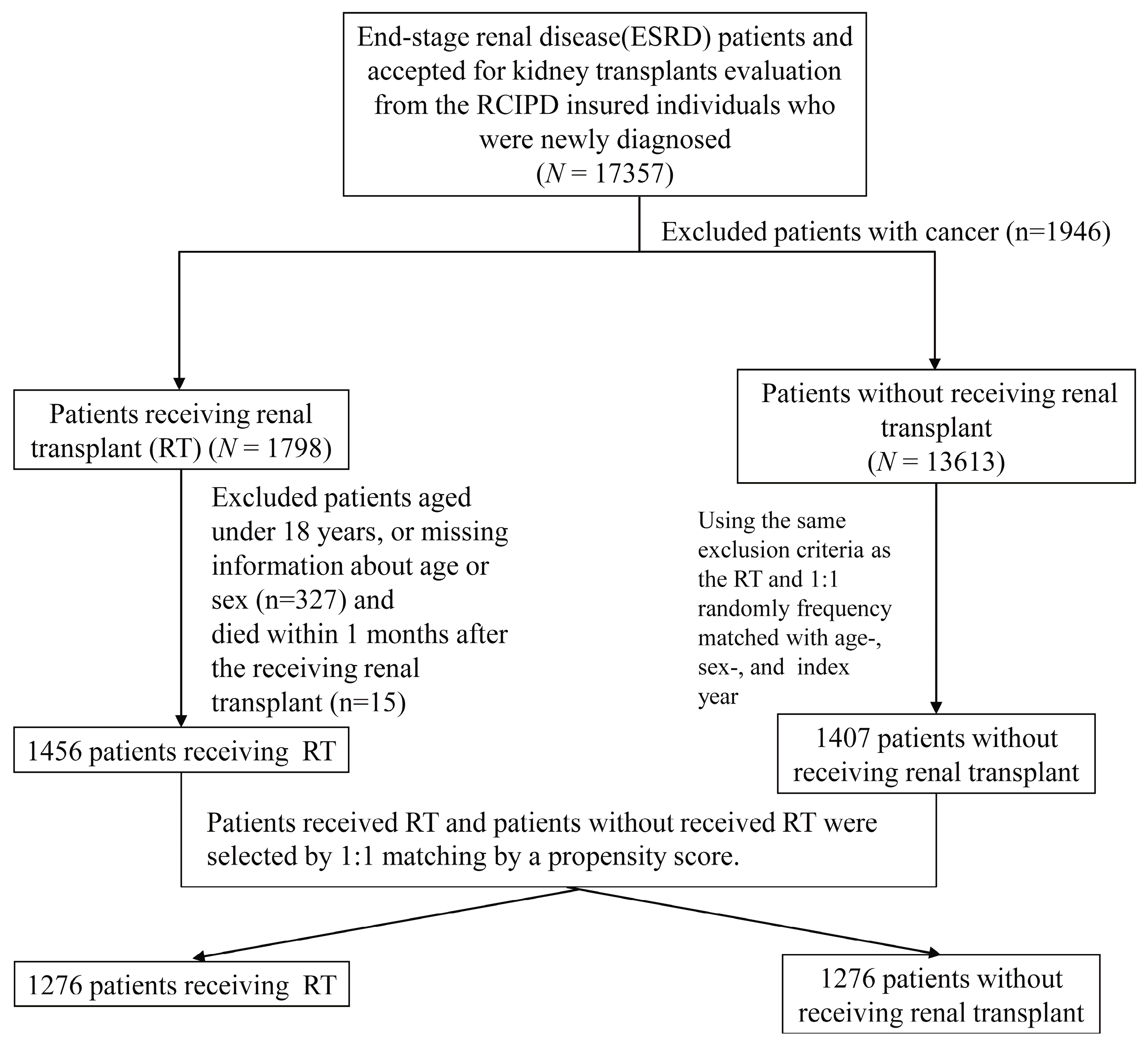
2.2. Study Enrollees
2.3. Statistical Analysis
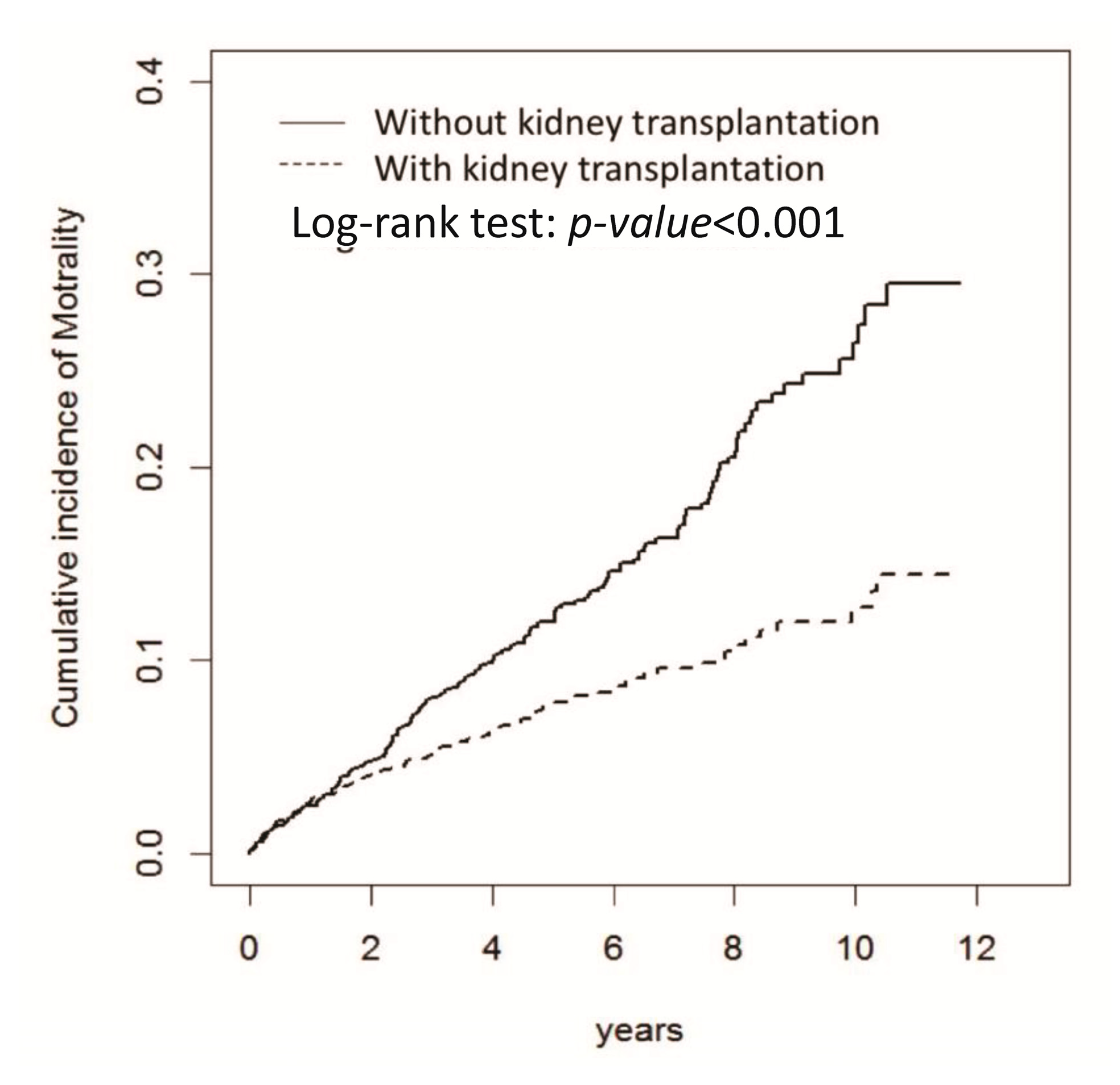
3. Results
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Jager, K.J.; Fraser, S.D.S. The ascending rank of chronic kidney disease in the global burden of disease study. Nephrol. Dial. Transpl. 2017, 32, ii121–ii128. [Google Scholar] [CrossRef] [PubMed]
- Schnuelle, P.; Lorenz, D.; Trede, M.; Van Der Woude, F.J. Impact of renal cadaveric transplantation on survival in end-stage renal failure: Evidence for reduced mortality risk compared with hemodialysis during long-term follow-up. J. Am. Soc. Nephrol. 1998, 9, 2135–2141. [Google Scholar] [PubMed]
- Pascual, J.; Zamora, J.; Pirsch, J.D. A systematic review of kidney transplantation from expanded criteria donors. Am. J. Kidney Dis. 2008, 52, 553–586. [Google Scholar] [CrossRef] [PubMed]
- Merion, R.M.; Ashby, V.B.; Wolfe, R.A.; Distant, D.A.; Hulbert-Shearon, T.E.; Metzger, R.A.; Ojo, A.O.; Port, F.K. Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA 2005, 294, 2726–2733. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.B.; Eddinger, K.C.; Locke, J.E.; Forde, K.A.; Reese, P.P.; Sawinski, D.L. Survival Benefit of Transplantation with a Deceased Diabetic Donor Kidney Compared with Remaining on the Waitlist. Clin. J. Am. Soc. Nephrol. 2017, 12, 974–982. [Google Scholar] [CrossRef] [PubMed]
- Jay, C.L.; Washburn, K.; Dean, P.G.; Helmick, R.A.; Pugh, J.A.; Stegall, M.D. Survival Benefit in Older Patients Associated with Earlier Transplant with High KDPI Kidneys. Transplantation 2017, 101, 867–872. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, J.P.; Combs, S.A.; Teitelbaum, I. Peritoneal dialysis: Update on patient survival. Clin. Nephrol. 2015, 83, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Rigoni, M.; Torri, E.; Nollo, G.; Zarantonello, D.; Laudon, A.; Sottini, L.; Guarrera, G.M.; Brunori, G. Survival and time-to-transplantation of peritoneal dialysis versus hemodialysis for end-stage renal disease patients: Competing-risks regression model in a single Italian center experience. J. Nephrol. 2017, 30, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.J.; Lo, Y.C.; Lan, J.L.; Yu, T.M.; Shu, K.H.; Chen, D.Y.; Ho, H.C.; Lin, C.H.; Chang, S.N. Outcome of lupus nephritis after entering into end-stage renal disease and comparison between different treatment modalities: A nationwide population-based cohort study in Taiwan. Transpl. Proc. 2014, 46, 339–341. [Google Scholar] [CrossRef] [PubMed]
- Tennankore, K.K.; Kim, S.J.; Baer, H.J.; Chan, C.T. Survival and hospitalization for intensive home hemodialysis compared with kidney transplantation. J. Am. Soc. Nephrol. 2014, 25, 2113–2120. [Google Scholar] [CrossRef] [PubMed]
- Storey, B.C.; Staplin, N.; Harper, C.H.; Haynes, R.; Winearls, C.G.; Goldacre, R.; Emberson, J.R.; Goldacre, M.J.; Baigent, C.; Landray, M.J.; et al. Declining comorbidity-adjusted mortality rates in English patients receiving maintenance renal replacement therapy. Kidney Int. 2018, 93, 1165–1174. [Google Scholar] [CrossRef] [PubMed]
- Wetmore, J.B.; Gilbertson, D.T.; Liu, J.; Collins, A.J. Improving Outcomes in Patients Receiving Dialysis: The Peer Kidney Care Initiative. Clin. J. Am. Soc. Nephrol. 2016, 11, 1297–1304. [Google Scholar] [CrossRef] [PubMed]
- van Walraven, C.; Manuel, D.G.; Knoll, G. Survival trends in ESRD patients compared with the general population in the United States. Am. J. Kidney Dis. 2014, 63, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Pippias, M.; Jager, K.J.; Kramer, A.; Leivestad, T.; Sanchez, M.B.; Caskey, F.J.; Collart, F.; Couchoud, C.; Dekker, F.W.; Finne, P.; et al. The changing trends and outcomes in renal replacement therapy: Data from the ERA-EDTA Registry. Nephrol. Dial. Transpl. 2016, 31, 831–841. [Google Scholar] [CrossRef] [PubMed]
- Roberts, M.A.; Polkinghorne, K.R.; McDonald, S.P.; Ierino, F.L. Secular trends in cardiovascular mortality rates of patients receiving dialysis compared with the general population. Am. J. Kidney Dis. 2011, 58, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Deb, S.; Austin, P.C.; Tu, J.V.; Ko, D.T.; Mazer, C.D.; Kiss, A.; Fremes, S.E. A Review of Propensity-Score Methods and Their Use in Cardiovascular Research. Can. J. Cardiol. 2016, 32, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.M.; Chuang, Y.W.; Yu, M.C.; Chen, C.H.; Yang, C.K.; Huang, S.T.; Lin, C.L.; Shu, K.H.; Kao, C.H. Risk of cancer in patients with polycystic kidney disease: A propensity-score matched analysis of a nationwide, population-based cohort study. Lancet Oncol. 2016, 17, 1419–1425. [Google Scholar] [CrossRef]
- Huang, C.C.; Cheng, K.F.; Wu, H.D. Survival analysis: Comparing peritoneal dialysis and hemodialysis in Taiwan. Perit. Dial. Int. 2008, 28 (Suppl. 3), S15–S20. [Google Scholar] [PubMed]
- Wu, P.H.; Lin, Y.T.; Lee, T.C.; Lin, M.Y.; Kuo, M.C.; Chiu, Y.W.; Hwang, S.J.; Chen, H.C. Predicting mortality of incident dialysis patients in Taiwan—A longitudinal population-based study. PLoS ONE 2013, 8, e61930. [Google Scholar] [CrossRef] [PubMed]
- Silbernagel, G.; Genser, B.; Drechsler, C.; Scharnagl, H.; Grammer, T.B.; Stojakovic, T.; Krane, V.; Ritz, E.; Wanner, C.; März, W. HDL cholesterol, apolipoproteins, and cardiovascular risk in hemodialysis patients. J. Am. Soc. Nephrol. 2015, 26, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Neale, J.; Smith, A.C. Cardiovascular risk factors following renal transplant. World J. Transpl. 2015, 5, 183–195. [Google Scholar] [CrossRef] [PubMed]
- Ramphul, R.; Fernandez, M.; Firoozi, S.; Kaski, J.C.; Sharma, R.; Banerjee, D. Assessing cardiovascular risk in chronic kidney disease patients prior to kidney transplantation: Clinical usefulness of a standardised cardiovascular assessment protocol. BMC Nephrol. 2018, 19, 2. [Google Scholar] [CrossRef] [PubMed]
- Helantera, I.; Salmela, K.; Kyllonen, L.; Koskinen, P.; Gronhagen-Riska, C.; Finne, P. Pretransplant dialysis duration and risk of death after kidney transplantation in the current era. Transplantation 2014, 98, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Haller, M.C.; Kainz, A.; Baer, H.; Oberbauer, R. Dialysis Vintage and Outcomes after Kidney Transplantation: A Retrospective Cohort Study. Clin. J. Am. Soc. Nephrol. 2017, 12, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Mokos, I.; Basic-Jukic, N.; Kastelan, Z.; Kes, P.; Pasini, J. Influence of long-term dialysis treatment on operative complications after renal transplantation. Transpl. Proc. 2010, 42, 2531–2533. [Google Scholar] [CrossRef] [PubMed]
- Batabyal, P.; Chapman, J.R.; Wong, G.; Craig, J.C.; Tong, A. Clinical practice guidelines on wait-listing for kidney transplantation: Consistent and equitable? Transplantation 2012, 94, 703–713. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.W.; Herzig, K.; Purdie, D.; Brown, A.M.; Rigby, R.J.; Nicol, D.L.; Hawley, C.M. A comparison of the effects of dialysis and renal transplantation on the survival of older uremic patients. Transplantation 2000, 69, 794–799. [Google Scholar] [CrossRef] [PubMed]
- Knoll, G.; Cockfield, S.; Blydt-Hansen, T.; Baran, D.; Kiberd, B.; Landsberg, D.; Rush, D.; Cole, E. Kidney Transplant Working Group of the Canadian Society of Transplantation. Canadian Society of Transplantation consensus guidelines on eligibility for kidney transplantation. CMAJ 2005, 173, 1181–1184. [Google Scholar] [CrossRef] [PubMed]
- Grams, M.E.; Massie, A.B.; Schold, J.D.; Chen, B.P.; Segev, D.L. Trends in the inactive kidney transplant waitlist and implications for candidate survival. Am. J. Transpl. 2013, 13, 1012–1018. [Google Scholar] [CrossRef] [PubMed]
- Grams, M.E.; Massie, A.B.; Coresh, J.; Segev, D.L. Trends in the timing of pre-emptive kidney transplantation. J. Am. Soc. Nephrol. 2011, 22, 1615–1620. [Google Scholar] [CrossRef] [PubMed]
| Age and Gender Matched | Propensity Score Matched | |||||
|---|---|---|---|---|---|---|
| Variable | Kidney Transplantation | p-Value | Kidney Transplantation | Standardized Differences | ||
| No | Yes | No | Yes | |||
| N = 1407 | N = 1456 | N = 1276 | N = 1276 | |||
| Age, year | 0.34 | |||||
| ≤34 | 319 (22.7) | 364 (25.0) | 293 (23.0) | 310 (24.3) | 0.03 | |
| 35–49 | 668 (47.5) | 670 (46.0) | 618 (48.4) | 578 (45.3) | 0.06 | |
| ≥50 | 420 (29.9) | 422 (29.0) | 365 (28.6) | 388 (30.4) | 0.04 | |
| Mean ± SD † | 43.6 (10.7) | 43.1 (11.0) | 0.25 | 43.3 (10.6) | 43.5 (11.1) | 0.01 |
| Sex | 0.96 | |||||
| Female | 727 (51.7) | 751 (51.6) | 648 (50.8) | 649 (50.9) | 0.002 | |
| Male | 680 (48.3) | 705 (48.4) | 628 (49.2) | 627 (49.1) | 0.002 | |
| Comorbidity | ||||||
| Hypertension | 1145 (81.4) | 1252 (86.0) | <0.001 | 1060 (83.1) | 1072 (84.0) | 0.025 |
| Hyperlipidemia | 433 (30.8) | 462 (31.7) | 0.58 | 373 (29.2) | 390 (30.6) | 0.029 |
| Diabetes | 178 (12.7) | 182 (12.5) | 0.9.00 | 152 (11.9) | 160 (12.5) | 0.019 |
| Coronary artery disease | 410 (29.1) | 298 (20.5) | <0.001 | 306 (24.0) | 298 (23.4) | 0.015 |
| Atrial fibrillation | 21 (1.49) | 17 (1.17) | 0.45 | 20 (1.57) | 17 (1.33) | 0.020 |
| Heart disease | 469 (33.3) | 391 (26.9) | <0.001 | 380 (29.8) | 389 (30.5) | 0.015 |
| Hepatitis B | 105 (7.46) | 121 (8.31) | 0.40 | 99 (7.76) | 107 (8.39) | 0.023 |
| Hepatitis C | 98 (6.97) | 106 (7.28) | 0.74 | 85 (6.66) | 92 (7.21) | 0.022 |
| Peripheral vessel disease | 33 (2.35) | 26 (1.79) | 0.29 | 24 (1.88) | 26 (2.04) | 0.022 |
| Age and Gender Matched | Propensity Score Matched | |||
|---|---|---|---|---|
| Kidney Transplantation | Kidney Transplantation | |||
| No | Yes | No | Yes | |
| (N = 1407) | (N = 1456) | (N = 1276) | (N = 1276) | |
| Person-years | 7060 | 7733 | 6388 | 6561 |
| Follow-up time (years, mean ± SD) | 5.02 ± 2.96 | 5.31 ± 3.07 | 5.01 ± 2.94 | 5.14 ± 3.04 |
| Mortality | ||||
| Event | 207 | 113 | 179 | 101 |
| Rate # | 2.93 | 1.46 | 2.80 | 1.54 |
| cHR (95% CI) | 1 (Reference) | 0.50 (0.40, 0.63) *** | 1 (Reference) | 0.59 (0.44, 0.78) *** |
| aHR † (95% CI) | 1 (Reference) | 0.51 (0.41, 0.64) *** | ||
| Propensity Score Matched | |||||||
|---|---|---|---|---|---|---|---|
| Variables | Event | PY | Rate # | Event | PY | Rate # | HR (95% CI) |
| Kidney Transplantation | |||||||
| No | Yes | ||||||
| Age, years | |||||||
| ≤34 | 33 | 1645 | 2.01 | 18 | 1815 | 0.99 | 0.67 (0.30, 1.48) |
| 35–49 | 77 | 3310 | 2.33 | 44 | 3185 | 1.38 | 0.58 (0.33, 1.04) |
| ≥50 | 69 | 1433 | 4.82 | 39 | 1560 | 2.50 | 0.64 (0.33, 1.24) |
| Sex | |||||||
| Female | 80 | 3427 | 2.33 | 44 | 3474 | 1.27 | 0.58 (0.36, 0.95) * |
| Male | 99 | 2960 | 3.34 | 57 | 3087 | 1.85 | 0.64 (0.42, 0.99) * |
| Comorbid | |||||||
| Hypertension | |||||||
| No | 21 | 1332 | 1.58 | 18 | 1263 | 1.42 | 0.87 (0.41, 1.82) |
| Yes | 158 | 5055 | 3.13 | 83 | 5298 | 1.57 | 0.49 (0.36, 0.68) *** |
| Hyperlipidemia | |||||||
| No | 122 | 4802 | 2.54 | 69 | 4866 | 1.42 | 0.63 (0.44, 0.91) * |
| Yes | 57 | 1585 | 3.60 | 32 | 1695 | 1.89 | 0.55 (0.31, 0.97) * |
| Diabetes | |||||||
| No | 130 | 5796 | 2.24 | 81 | 5944 | 1.36 | 0.62 (0.44, 0.88) ** |
| Yes | 49 | 592 | 8.28 | 20 | 617 | 3.24 | 0.06 (0.01, 0.42) ** |
| Coronary artery disease | |||||||
| No | 108 | 4999 | 2.16 | 69 | 5185 | 1.33 | 0.66 (0.46, 0.93) * |
| Yes | 71 | 1389 | 5.11 | 32 | 1376 | 2.33 | 0.36 (0.21, 0.64) *** |
| Atrial fibrillation | |||||||
| No | 175 | 6312 | 2.77 | 98 | 6485 | 1.51 | 0.58 (0.44, 0.78) *** |
| Yes | 4 | 75 | 5.31 | 3 | 76 | 3.96 | - |
| Heart disease | |||||||
| No | 112 | 4727 | 2.37 | 59 | 4774 | 1.24 | 0.58 (0.41, 0.84) ** |
| Yes | 67 | 1660 | 4.04 | 42 | 1787 | 2.35 | 0.69 (0.43, 1.11) |
| Hepatitis B | |||||||
| No | 162 | 6037 | 2.68 | 92 | 6138 | 1.50 | 0.64 (0.47, 0.86) ** |
| Yes | 17 | 351 | 4.85 | 9 | 423 | 2.13 | 0.43 (0.11, 1.66) |
| Hepatitis C | |||||||
| No | 162 | 6022 | 2.69 | 92 | 6174 | 1.49 | 0.63 (0.46, 0.86) ** |
| Yes | 17 | 366 | 4.65 | 9 | 387 | 2.33 | 1.00 (0.20, 4.96) |
| Peripheral vessel disease | |||||||
| No | 177 | 6312 | 2.80 | 98 | 6493 | 1.51 | 0.58 (0.43, 0.77) *** |
| Yes | 2 | 75 | 2.65 | 3 | 68 | 4.42 | - |
| Follow-up period, years | |||||||
| ≤1 | 31 | 1248 | 2.48 | 34 | 1251 | 2.72 | 1.10 (0.67, 1.78) |
| >1, ≤2 | 27 | 1127 | 2.40 | 16 | 1130 | 1.42 | 0.64 (0.34, 1.20) |
| >2, ≤3 | 34 | 966 | 3.52 | 11 | 971 | 1.13 | 0.31 (0.14, 0.68) ** |
| >3, ≤4 | 16 | 802 | 2.00 | 11 | 807 | 1.36 | 0.54 (0.22, 1.35) |
| >4, ≤5 | 16 | 653 | 2.45 | 10 | 673 | 1.49 | 0.60 (0.22, 1.65) |
| >5 | 55 | 1591 | 3.46 | 19 | 1728 | 1.10 | 0.23 (0.10, 0.56) ** |
| Pre-Transplant Dialysis Duration (Years) | N | Event | PY | Rate # | cHR (95% CI) | aHR † (95% CI) |
|---|---|---|---|---|---|---|
| 0–1 (reference) | 101 | 5 | 468 | 1.07 | 1 (Reference) | 1 (Reference) |
| 1–3 | 325 | 22 | 1948 | 1.13 | 1.10 (0.42, 2.92) | 1.07 (0.40, 2.83) |
| 3–5 | 318 | 29 | 1727 | 1.68 | 1.62 (0.63, 4.18) | 1.39 (0.53, 3.62) |
| 5–7 | 252 | 21 | 1293 | 1.62 | 1.54 (0.58, 4.09) | 1.41 (0.53, 3.77) |
| >7 | 280 | 24 | 1124 | 2.13 | 1.94 (0.74, 5.08) | 1.65 (0.62, 4.36) |
| Variable | HR (95% CI) |
|---|---|
| Mortality | |
| Stratification adjusted on the propensity score 10 strata | 0.54 (0.43, 0.69) *** |
| Inverse probability of treatment weights | 0.55 (0.46, 0.65) *** |
| Covariate adjustment by using the propensity score | 0.54 (0.42, 0.69) *** |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, M.-J.; Yu, T.-M.; Lin, C.-L.; Kao, C.-H. Propensity Score-Matched Analysis of the Survival Benefit from Kidney Transplantation in Patients with End-Stage Renal Disease. J. Clin. Med. 2018, 7, 388. https://doi.org/10.3390/jcm7110388
Wu M-J, Yu T-M, Lin C-L, Kao C-H. Propensity Score-Matched Analysis of the Survival Benefit from Kidney Transplantation in Patients with End-Stage Renal Disease. Journal of Clinical Medicine. 2018; 7(11):388. https://doi.org/10.3390/jcm7110388
Chicago/Turabian StyleWu, Ming-Ju, Tung-Min Yu, Cheng-Li Lin, and Chia-Hung Kao. 2018. "Propensity Score-Matched Analysis of the Survival Benefit from Kidney Transplantation in Patients with End-Stage Renal Disease" Journal of Clinical Medicine 7, no. 11: 388. https://doi.org/10.3390/jcm7110388
APA StyleWu, M.-J., Yu, T.-M., Lin, C.-L., & Kao, C.-H. (2018). Propensity Score-Matched Analysis of the Survival Benefit from Kidney Transplantation in Patients with End-Stage Renal Disease. Journal of Clinical Medicine, 7(11), 388. https://doi.org/10.3390/jcm7110388





