Propensity Score-Matched Analysis of the Survival Benefit from Kidney Transplantation in Patients with End-Stage Renal Disease
Abstract
:1. Introduction
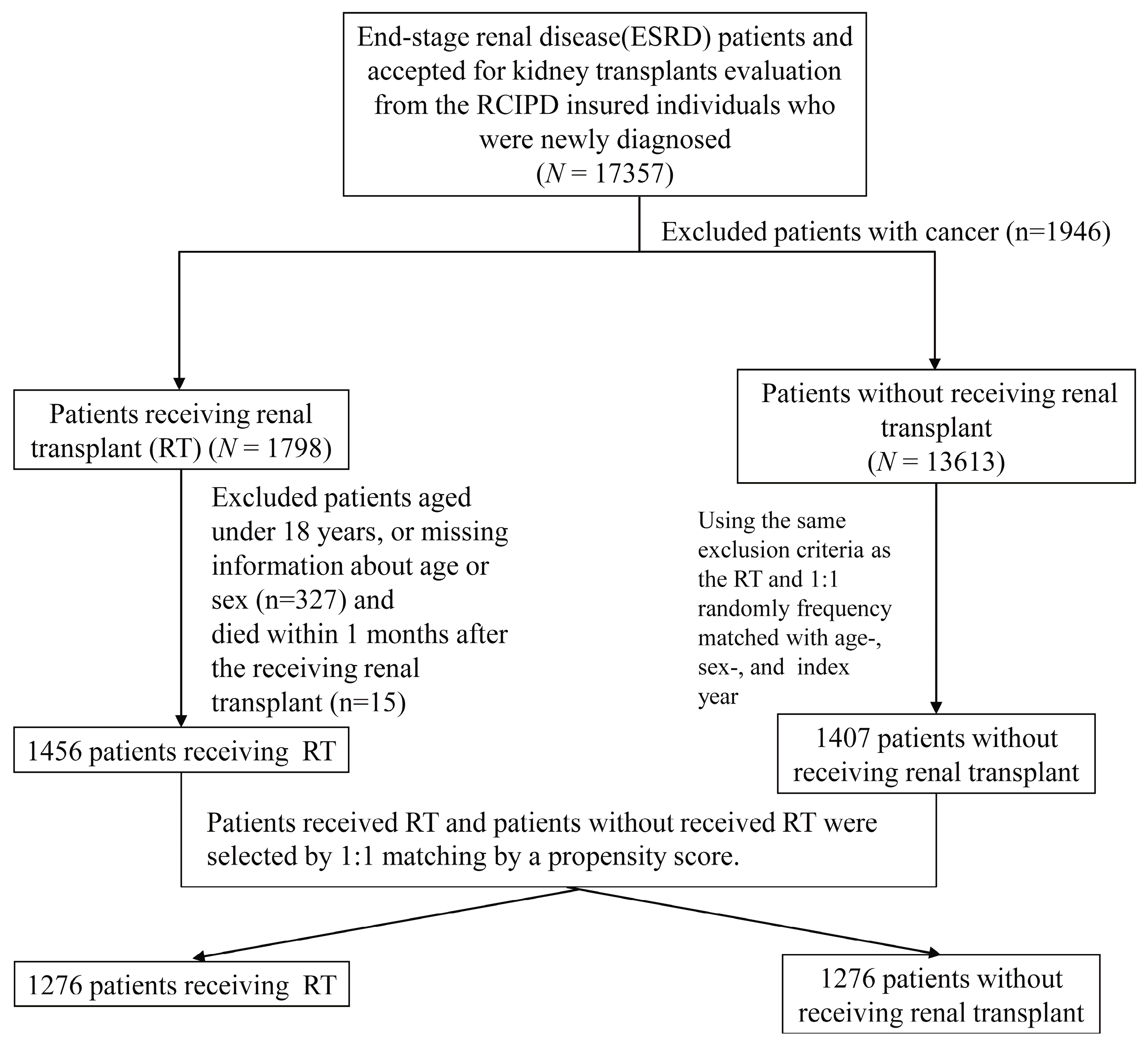
2. Materials and Methods
2.1. Data Source
2.2. Study Enrollees
2.3. Statistical Analysis
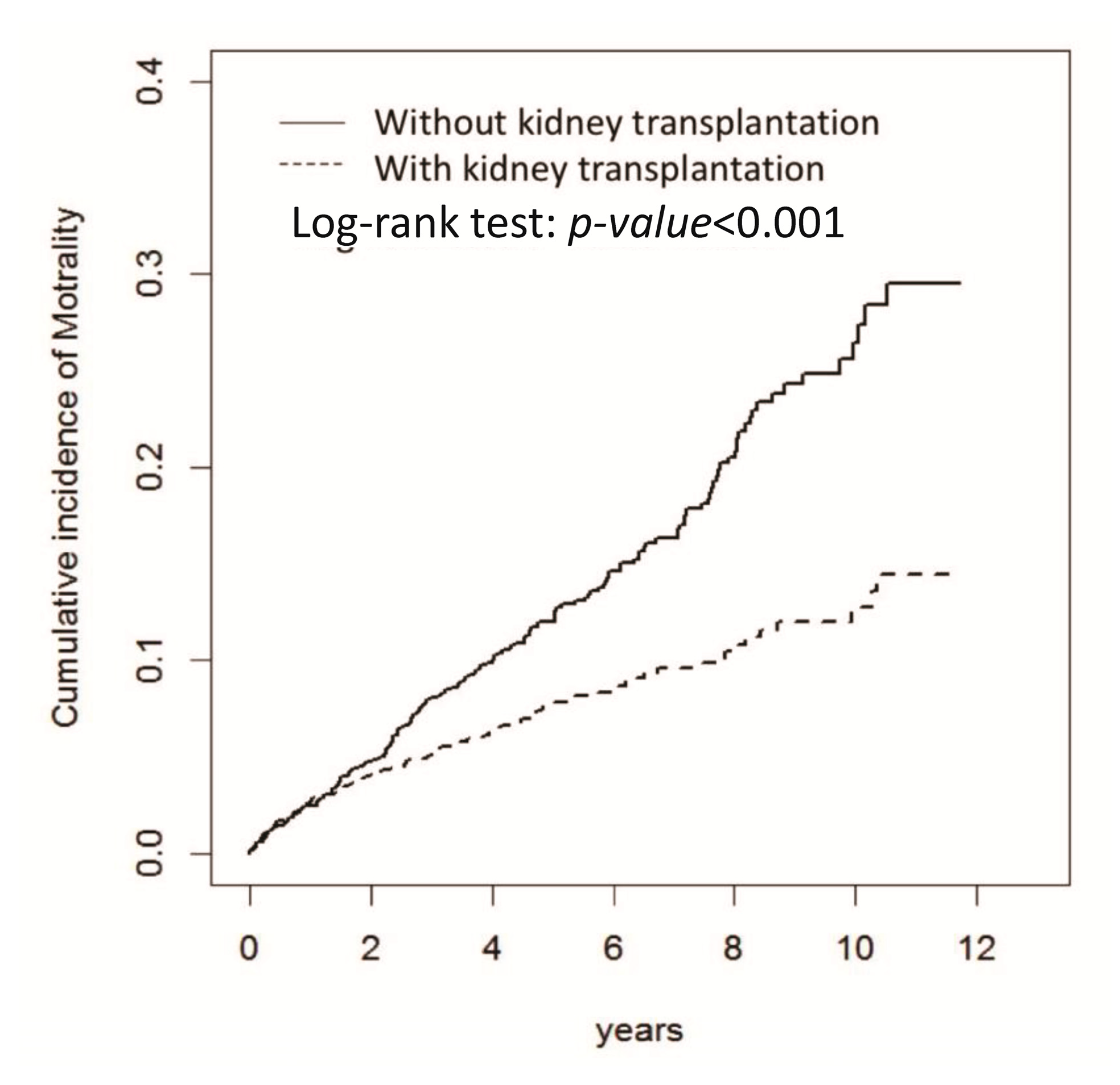
3. Results
4. Discussion
5. Conclusions
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Jager, K.J.; Fraser, S.D.S. The ascending rank of chronic kidney disease in the global burden of disease study. Nephrol. Dial. Transpl. 2017, 32, ii121–ii128. [Google Scholar] [CrossRef] [PubMed]
- Schnuelle, P.; Lorenz, D.; Trede, M.; Van Der Woude, F.J. Impact of renal cadaveric transplantation on survival in end-stage renal failure: Evidence for reduced mortality risk compared with hemodialysis during long-term follow-up. J. Am. Soc. Nephrol. 1998, 9, 2135–2141. [Google Scholar] [PubMed]
- Pascual, J.; Zamora, J.; Pirsch, J.D. A systematic review of kidney transplantation from expanded criteria donors. Am. J. Kidney Dis. 2008, 52, 553–586. [Google Scholar] [CrossRef] [PubMed]
- Merion, R.M.; Ashby, V.B.; Wolfe, R.A.; Distant, D.A.; Hulbert-Shearon, T.E.; Metzger, R.A.; Ojo, A.O.; Port, F.K. Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA 2005, 294, 2726–2733. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J.B.; Eddinger, K.C.; Locke, J.E.; Forde, K.A.; Reese, P.P.; Sawinski, D.L. Survival Benefit of Transplantation with a Deceased Diabetic Donor Kidney Compared with Remaining on the Waitlist. Clin. J. Am. Soc. Nephrol. 2017, 12, 974–982. [Google Scholar] [CrossRef] [PubMed]
- Jay, C.L.; Washburn, K.; Dean, P.G.; Helmick, R.A.; Pugh, J.A.; Stegall, M.D. Survival Benefit in Older Patients Associated with Earlier Transplant with High KDPI Kidneys. Transplantation 2017, 101, 867–872. [Google Scholar] [CrossRef] [PubMed]
- Teixeira, J.P.; Combs, S.A.; Teitelbaum, I. Peritoneal dialysis: Update on patient survival. Clin. Nephrol. 2015, 83, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Rigoni, M.; Torri, E.; Nollo, G.; Zarantonello, D.; Laudon, A.; Sottini, L.; Guarrera, G.M.; Brunori, G. Survival and time-to-transplantation of peritoneal dialysis versus hemodialysis for end-stage renal disease patients: Competing-risks regression model in a single Italian center experience. J. Nephrol. 2017, 30, 441–447. [Google Scholar] [CrossRef] [PubMed]
- Wu, M.J.; Lo, Y.C.; Lan, J.L.; Yu, T.M.; Shu, K.H.; Chen, D.Y.; Ho, H.C.; Lin, C.H.; Chang, S.N. Outcome of lupus nephritis after entering into end-stage renal disease and comparison between different treatment modalities: A nationwide population-based cohort study in Taiwan. Transpl. Proc. 2014, 46, 339–341. [Google Scholar] [CrossRef] [PubMed]
- Tennankore, K.K.; Kim, S.J.; Baer, H.J.; Chan, C.T. Survival and hospitalization for intensive home hemodialysis compared with kidney transplantation. J. Am. Soc. Nephrol. 2014, 25, 2113–2120. [Google Scholar] [CrossRef] [PubMed]
- Storey, B.C.; Staplin, N.; Harper, C.H.; Haynes, R.; Winearls, C.G.; Goldacre, R.; Emberson, J.R.; Goldacre, M.J.; Baigent, C.; Landray, M.J.; et al. Declining comorbidity-adjusted mortality rates in English patients receiving maintenance renal replacement therapy. Kidney Int. 2018, 93, 1165–1174. [Google Scholar] [CrossRef] [PubMed]
- Wetmore, J.B.; Gilbertson, D.T.; Liu, J.; Collins, A.J. Improving Outcomes in Patients Receiving Dialysis: The Peer Kidney Care Initiative. Clin. J. Am. Soc. Nephrol. 2016, 11, 1297–1304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- van Walraven, C.; Manuel, D.G.; Knoll, G. Survival trends in ESRD patients compared with the general population in the United States. Am. J. Kidney Dis. 2014, 63, 491–499. [Google Scholar] [CrossRef] [PubMed]
- Pippias, M.; Jager, K.J.; Kramer, A.; Leivestad, T.; Sanchez, M.B.; Caskey, F.J.; Collart, F.; Couchoud, C.; Dekker, F.W.; Finne, P.; et al. The changing trends and outcomes in renal replacement therapy: Data from the ERA-EDTA Registry. Nephrol. Dial. Transpl. 2016, 31, 831–841. [Google Scholar] [CrossRef] [PubMed]
- Roberts, M.A.; Polkinghorne, K.R.; McDonald, S.P.; Ierino, F.L. Secular trends in cardiovascular mortality rates of patients receiving dialysis compared with the general population. Am. J. Kidney Dis. 2011, 58, 64–72. [Google Scholar] [CrossRef] [PubMed]
- Deb, S.; Austin, P.C.; Tu, J.V.; Ko, D.T.; Mazer, C.D.; Kiss, A.; Fremes, S.E. A Review of Propensity-Score Methods and Their Use in Cardiovascular Research. Can. J. Cardiol. 2016, 32, 259–265. [Google Scholar] [CrossRef] [PubMed]
- Yu, T.M.; Chuang, Y.W.; Yu, M.C.; Chen, C.H.; Yang, C.K.; Huang, S.T.; Lin, C.L.; Shu, K.H.; Kao, C.H. Risk of cancer in patients with polycystic kidney disease: A propensity-score matched analysis of a nationwide, population-based cohort study. Lancet Oncol. 2016, 17, 1419–1425. [Google Scholar] [CrossRef]
- Huang, C.C.; Cheng, K.F.; Wu, H.D. Survival analysis: Comparing peritoneal dialysis and hemodialysis in Taiwan. Perit. Dial. Int. 2008, 28 (Suppl. 3), S15–S20. [Google Scholar] [PubMed]
- Wu, P.H.; Lin, Y.T.; Lee, T.C.; Lin, M.Y.; Kuo, M.C.; Chiu, Y.W.; Hwang, S.J.; Chen, H.C. Predicting mortality of incident dialysis patients in Taiwan—A longitudinal population-based study. PLoS ONE 2013, 8, e61930. [Google Scholar] [CrossRef] [PubMed]
- Silbernagel, G.; Genser, B.; Drechsler, C.; Scharnagl, H.; Grammer, T.B.; Stojakovic, T.; Krane, V.; Ritz, E.; Wanner, C.; März, W. HDL cholesterol, apolipoproteins, and cardiovascular risk in hemodialysis patients. J. Am. Soc. Nephrol. 2015, 26, 484–492. [Google Scholar] [CrossRef] [PubMed]
- Neale, J.; Smith, A.C. Cardiovascular risk factors following renal transplant. World J. Transpl. 2015, 5, 183–195. [Google Scholar] [CrossRef] [PubMed]
- Ramphul, R.; Fernandez, M.; Firoozi, S.; Kaski, J.C.; Sharma, R.; Banerjee, D. Assessing cardiovascular risk in chronic kidney disease patients prior to kidney transplantation: Clinical usefulness of a standardised cardiovascular assessment protocol. BMC Nephrol. 2018, 19, 2. [Google Scholar] [CrossRef] [PubMed]
- Helantera, I.; Salmela, K.; Kyllonen, L.; Koskinen, P.; Gronhagen-Riska, C.; Finne, P. Pretransplant dialysis duration and risk of death after kidney transplantation in the current era. Transplantation 2014, 98, 458–464. [Google Scholar] [CrossRef] [PubMed]
- Haller, M.C.; Kainz, A.; Baer, H.; Oberbauer, R. Dialysis Vintage and Outcomes after Kidney Transplantation: A Retrospective Cohort Study. Clin. J. Am. Soc. Nephrol. 2017, 12, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Mokos, I.; Basic-Jukic, N.; Kastelan, Z.; Kes, P.; Pasini, J. Influence of long-term dialysis treatment on operative complications after renal transplantation. Transpl. Proc. 2010, 42, 2531–2533. [Google Scholar] [CrossRef] [PubMed]
- Batabyal, P.; Chapman, J.R.; Wong, G.; Craig, J.C.; Tong, A. Clinical practice guidelines on wait-listing for kidney transplantation: Consistent and equitable? Transplantation 2012, 94, 703–713. [Google Scholar] [CrossRef] [PubMed]
- Johnson, D.W.; Herzig, K.; Purdie, D.; Brown, A.M.; Rigby, R.J.; Nicol, D.L.; Hawley, C.M. A comparison of the effects of dialysis and renal transplantation on the survival of older uremic patients. Transplantation 2000, 69, 794–799. [Google Scholar] [CrossRef] [PubMed]
- Knoll, G.; Cockfield, S.; Blydt-Hansen, T.; Baran, D.; Kiberd, B.; Landsberg, D.; Rush, D.; Cole, E. Kidney Transplant Working Group of the Canadian Society of Transplantation. Canadian Society of Transplantation consensus guidelines on eligibility for kidney transplantation. CMAJ 2005, 173, 1181–1184. [Google Scholar] [CrossRef] [PubMed]
- Grams, M.E.; Massie, A.B.; Schold, J.D.; Chen, B.P.; Segev, D.L. Trends in the inactive kidney transplant waitlist and implications for candidate survival. Am. J. Transpl. 2013, 13, 1012–1018. [Google Scholar] [CrossRef] [PubMed]
- Grams, M.E.; Massie, A.B.; Coresh, J.; Segev, D.L. Trends in the timing of pre-emptive kidney transplantation. J. Am. Soc. Nephrol. 2011, 22, 1615–1620. [Google Scholar] [CrossRef] [PubMed]
| Age and Gender Matched | Propensity Score Matched | |||||
|---|---|---|---|---|---|---|
| Variable | Kidney Transplantation | p-Value | Kidney Transplantation | Standardized Differences | ||
| No | Yes | No | Yes | |||
| N = 1407 | N = 1456 | N = 1276 | N = 1276 | |||
| Age, year | 0.34 | |||||
| ≤34 | 319 (22.7) | 364 (25.0) | 293 (23.0) | 310 (24.3) | 0.03 | |
| 35–49 | 668 (47.5) | 670 (46.0) | 618 (48.4) | 578 (45.3) | 0.06 | |
| ≥50 | 420 (29.9) | 422 (29.0) | 365 (28.6) | 388 (30.4) | 0.04 | |
| Mean ± SD † | 43.6 (10.7) | 43.1 (11.0) | 0.25 | 43.3 (10.6) | 43.5 (11.1) | 0.01 |
| Sex | 0.96 | |||||
| Female | 727 (51.7) | 751 (51.6) | 648 (50.8) | 649 (50.9) | 0.002 | |
| Male | 680 (48.3) | 705 (48.4) | 628 (49.2) | 627 (49.1) | 0.002 | |
| Comorbidity | ||||||
| Hypertension | 1145 (81.4) | 1252 (86.0) | <0.001 | 1060 (83.1) | 1072 (84.0) | 0.025 |
| Hyperlipidemia | 433 (30.8) | 462 (31.7) | 0.58 | 373 (29.2) | 390 (30.6) | 0.029 |
| Diabetes | 178 (12.7) | 182 (12.5) | 0.9.00 | 152 (11.9) | 160 (12.5) | 0.019 |
| Coronary artery disease | 410 (29.1) | 298 (20.5) | <0.001 | 306 (24.0) | 298 (23.4) | 0.015 |
| Atrial fibrillation | 21 (1.49) | 17 (1.17) | 0.45 | 20 (1.57) | 17 (1.33) | 0.020 |
| Heart disease | 469 (33.3) | 391 (26.9) | <0.001 | 380 (29.8) | 389 (30.5) | 0.015 |
| Hepatitis B | 105 (7.46) | 121 (8.31) | 0.40 | 99 (7.76) | 107 (8.39) | 0.023 |
| Hepatitis C | 98 (6.97) | 106 (7.28) | 0.74 | 85 (6.66) | 92 (7.21) | 0.022 |
| Peripheral vessel disease | 33 (2.35) | 26 (1.79) | 0.29 | 24 (1.88) | 26 (2.04) | 0.022 |
| Age and Gender Matched | Propensity Score Matched | |||
|---|---|---|---|---|
| Kidney Transplantation | Kidney Transplantation | |||
| No | Yes | No | Yes | |
| (N = 1407) | (N = 1456) | (N = 1276) | (N = 1276) | |
| Person-years | 7060 | 7733 | 6388 | 6561 |
| Follow-up time (years, mean ± SD) | 5.02 ± 2.96 | 5.31 ± 3.07 | 5.01 ± 2.94 | 5.14 ± 3.04 |
| Mortality | ||||
| Event | 207 | 113 | 179 | 101 |
| Rate # | 2.93 | 1.46 | 2.80 | 1.54 |
| cHR (95% CI) | 1 (Reference) | 0.50 (0.40, 0.63) *** | 1 (Reference) | 0.59 (0.44, 0.78) *** |
| aHR † (95% CI) | 1 (Reference) | 0.51 (0.41, 0.64) *** | ||
| Propensity Score Matched | |||||||
|---|---|---|---|---|---|---|---|
| Variables | Event | PY | Rate # | Event | PY | Rate # | HR (95% CI) |
| Kidney Transplantation | |||||||
| No | Yes | ||||||
| Age, years | |||||||
| ≤34 | 33 | 1645 | 2.01 | 18 | 1815 | 0.99 | 0.67 (0.30, 1.48) |
| 35–49 | 77 | 3310 | 2.33 | 44 | 3185 | 1.38 | 0.58 (0.33, 1.04) |
| ≥50 | 69 | 1433 | 4.82 | 39 | 1560 | 2.50 | 0.64 (0.33, 1.24) |
| Sex | |||||||
| Female | 80 | 3427 | 2.33 | 44 | 3474 | 1.27 | 0.58 (0.36, 0.95) * |
| Male | 99 | 2960 | 3.34 | 57 | 3087 | 1.85 | 0.64 (0.42, 0.99) * |
| Comorbid | |||||||
| Hypertension | |||||||
| No | 21 | 1332 | 1.58 | 18 | 1263 | 1.42 | 0.87 (0.41, 1.82) |
| Yes | 158 | 5055 | 3.13 | 83 | 5298 | 1.57 | 0.49 (0.36, 0.68) *** |
| Hyperlipidemia | |||||||
| No | 122 | 4802 | 2.54 | 69 | 4866 | 1.42 | 0.63 (0.44, 0.91) * |
| Yes | 57 | 1585 | 3.60 | 32 | 1695 | 1.89 | 0.55 (0.31, 0.97) * |
| Diabetes | |||||||
| No | 130 | 5796 | 2.24 | 81 | 5944 | 1.36 | 0.62 (0.44, 0.88) ** |
| Yes | 49 | 592 | 8.28 | 20 | 617 | 3.24 | 0.06 (0.01, 0.42) ** |
| Coronary artery disease | |||||||
| No | 108 | 4999 | 2.16 | 69 | 5185 | 1.33 | 0.66 (0.46, 0.93) * |
| Yes | 71 | 1389 | 5.11 | 32 | 1376 | 2.33 | 0.36 (0.21, 0.64) *** |
| Atrial fibrillation | |||||||
| No | 175 | 6312 | 2.77 | 98 | 6485 | 1.51 | 0.58 (0.44, 0.78) *** |
| Yes | 4 | 75 | 5.31 | 3 | 76 | 3.96 | - |
| Heart disease | |||||||
| No | 112 | 4727 | 2.37 | 59 | 4774 | 1.24 | 0.58 (0.41, 0.84) ** |
| Yes | 67 | 1660 | 4.04 | 42 | 1787 | 2.35 | 0.69 (0.43, 1.11) |
| Hepatitis B | |||||||
| No | 162 | 6037 | 2.68 | 92 | 6138 | 1.50 | 0.64 (0.47, 0.86) ** |
| Yes | 17 | 351 | 4.85 | 9 | 423 | 2.13 | 0.43 (0.11, 1.66) |
| Hepatitis C | |||||||
| No | 162 | 6022 | 2.69 | 92 | 6174 | 1.49 | 0.63 (0.46, 0.86) ** |
| Yes | 17 | 366 | 4.65 | 9 | 387 | 2.33 | 1.00 (0.20, 4.96) |
| Peripheral vessel disease | |||||||
| No | 177 | 6312 | 2.80 | 98 | 6493 | 1.51 | 0.58 (0.43, 0.77) *** |
| Yes | 2 | 75 | 2.65 | 3 | 68 | 4.42 | - |
| Follow-up period, years | |||||||
| ≤1 | 31 | 1248 | 2.48 | 34 | 1251 | 2.72 | 1.10 (0.67, 1.78) |
| >1, ≤2 | 27 | 1127 | 2.40 | 16 | 1130 | 1.42 | 0.64 (0.34, 1.20) |
| >2, ≤3 | 34 | 966 | 3.52 | 11 | 971 | 1.13 | 0.31 (0.14, 0.68) ** |
| >3, ≤4 | 16 | 802 | 2.00 | 11 | 807 | 1.36 | 0.54 (0.22, 1.35) |
| >4, ≤5 | 16 | 653 | 2.45 | 10 | 673 | 1.49 | 0.60 (0.22, 1.65) |
| >5 | 55 | 1591 | 3.46 | 19 | 1728 | 1.10 | 0.23 (0.10, 0.56) ** |
| Pre-Transplant Dialysis Duration (Years) | N | Event | PY | Rate # | cHR (95% CI) | aHR † (95% CI) |
|---|---|---|---|---|---|---|
| 0–1 (reference) | 101 | 5 | 468 | 1.07 | 1 (Reference) | 1 (Reference) |
| 1–3 | 325 | 22 | 1948 | 1.13 | 1.10 (0.42, 2.92) | 1.07 (0.40, 2.83) |
| 3–5 | 318 | 29 | 1727 | 1.68 | 1.62 (0.63, 4.18) | 1.39 (0.53, 3.62) |
| 5–7 | 252 | 21 | 1293 | 1.62 | 1.54 (0.58, 4.09) | 1.41 (0.53, 3.77) |
| >7 | 280 | 24 | 1124 | 2.13 | 1.94 (0.74, 5.08) | 1.65 (0.62, 4.36) |
| Variable | HR (95% CI) |
|---|---|
| Mortality | |
| Stratification adjusted on the propensity score 10 strata | 0.54 (0.43, 0.69) *** |
| Inverse probability of treatment weights | 0.55 (0.46, 0.65) *** |
| Covariate adjustment by using the propensity score | 0.54 (0.42, 0.69) *** |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, M.-J.; Yu, T.-M.; Lin, C.-L.; Kao, C.-H. Propensity Score-Matched Analysis of the Survival Benefit from Kidney Transplantation in Patients with End-Stage Renal Disease. J. Clin. Med. 2018, 7, 388. https://doi.org/10.3390/jcm7110388
Wu M-J, Yu T-M, Lin C-L, Kao C-H. Propensity Score-Matched Analysis of the Survival Benefit from Kidney Transplantation in Patients with End-Stage Renal Disease. Journal of Clinical Medicine. 2018; 7(11):388. https://doi.org/10.3390/jcm7110388
Chicago/Turabian StyleWu, Ming-Ju, Tung-Min Yu, Cheng-Li Lin, and Chia-Hung Kao. 2018. "Propensity Score-Matched Analysis of the Survival Benefit from Kidney Transplantation in Patients with End-Stage Renal Disease" Journal of Clinical Medicine 7, no. 11: 388. https://doi.org/10.3390/jcm7110388
APA StyleWu, M.-J., Yu, T.-M., Lin, C.-L., & Kao, C.-H. (2018). Propensity Score-Matched Analysis of the Survival Benefit from Kidney Transplantation in Patients with End-Stage Renal Disease. Journal of Clinical Medicine, 7(11), 388. https://doi.org/10.3390/jcm7110388





