Paroxysmal Atrial Fibrillation in Liver Diseases: Epidemiology and Possible Pathophysiological Mechanisms
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Data Collection
2.3. Statistical Analysis
2.4. Literature Review
3. Results
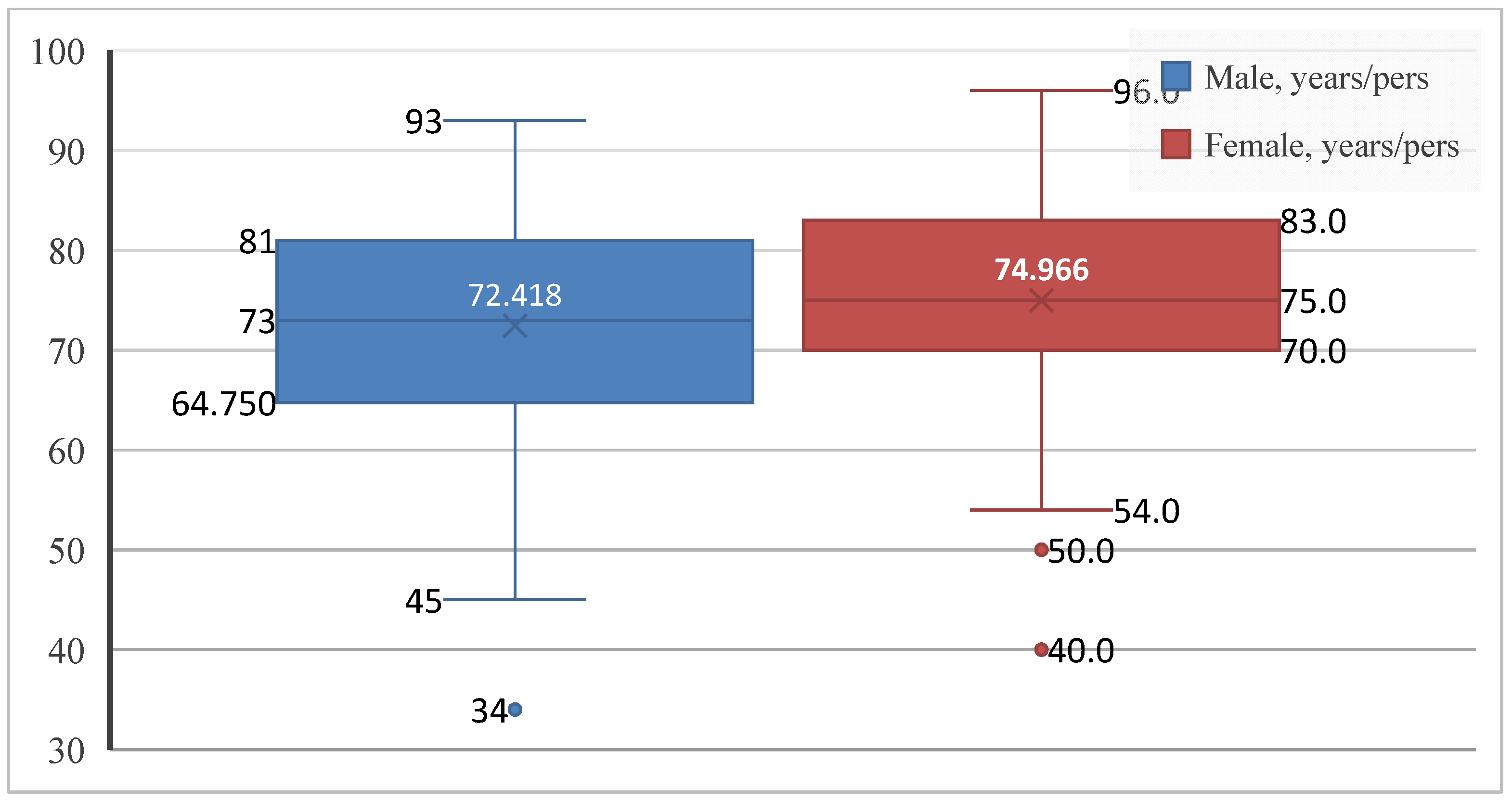
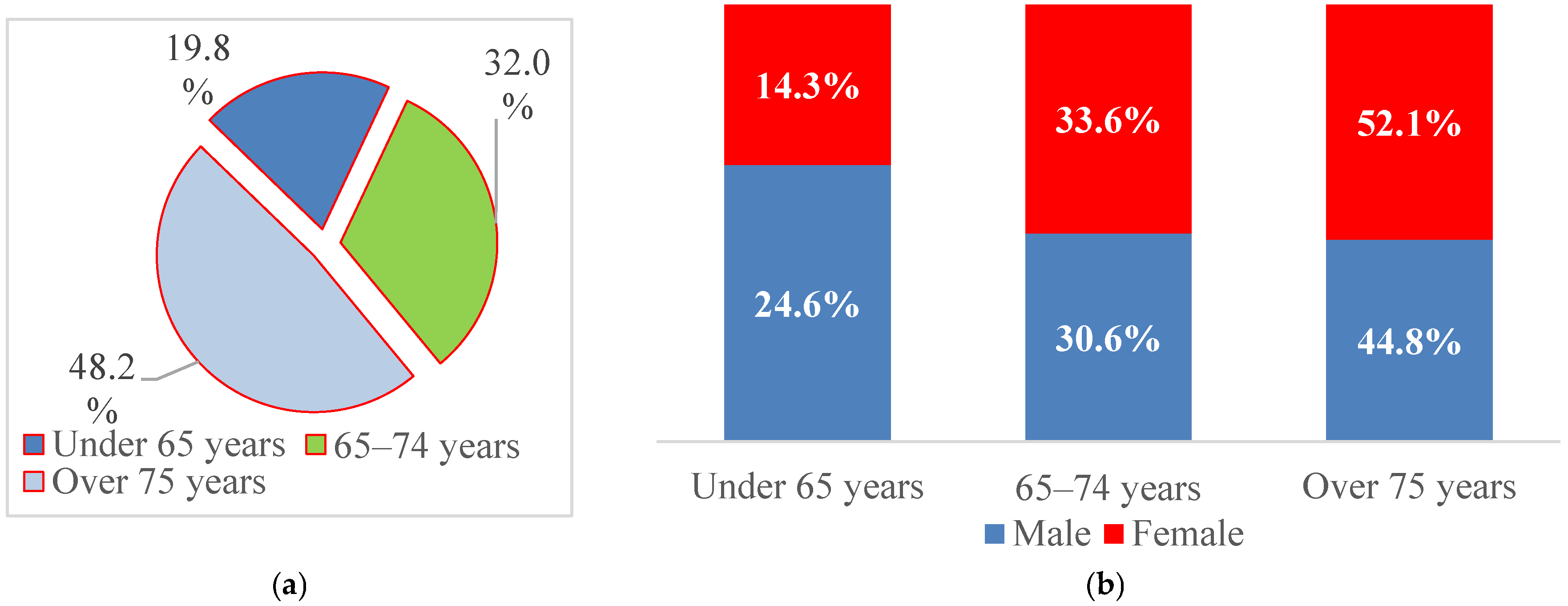
3.1. Demographic Characteristics
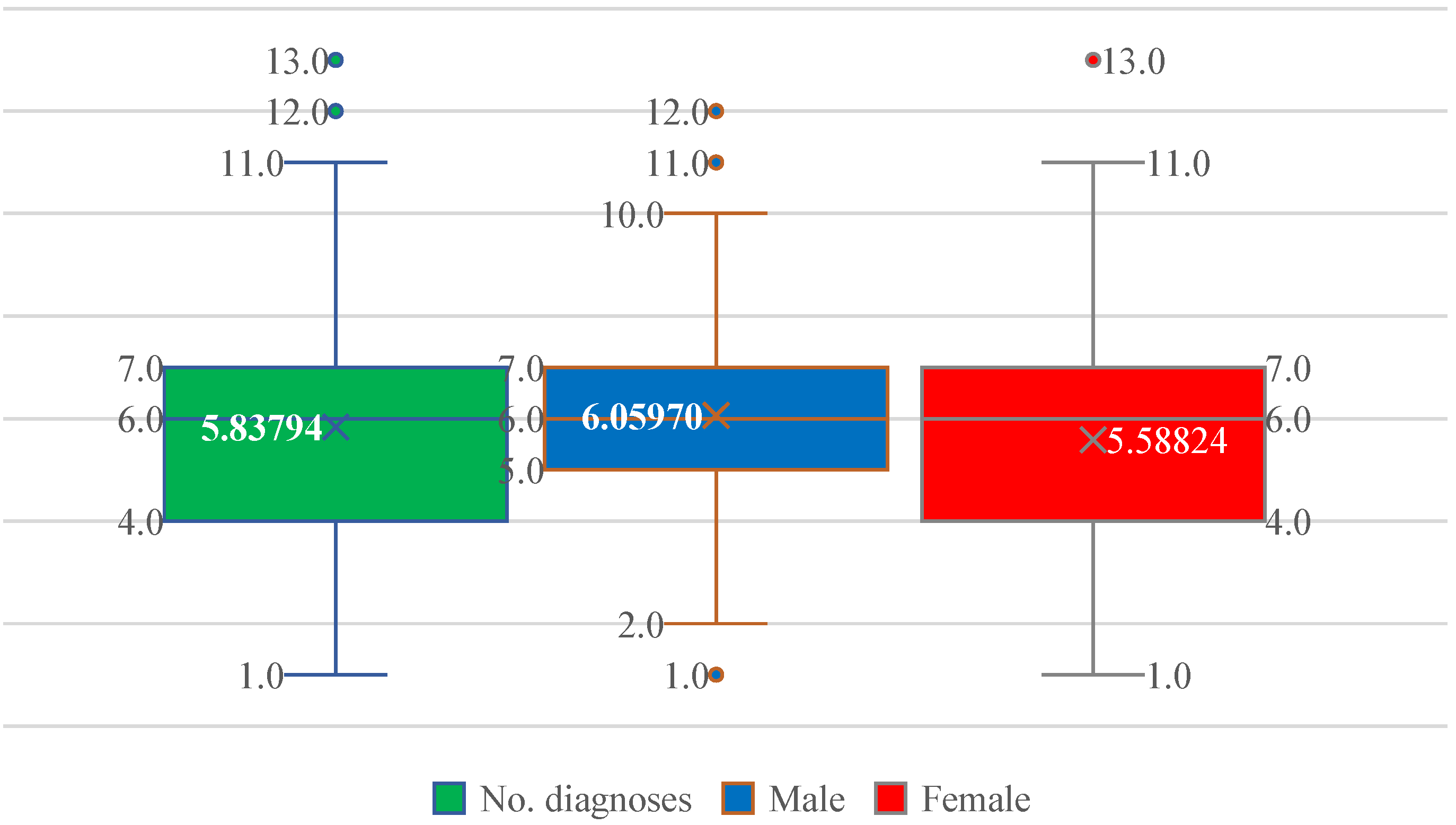
3.2. Comorbidity Burden
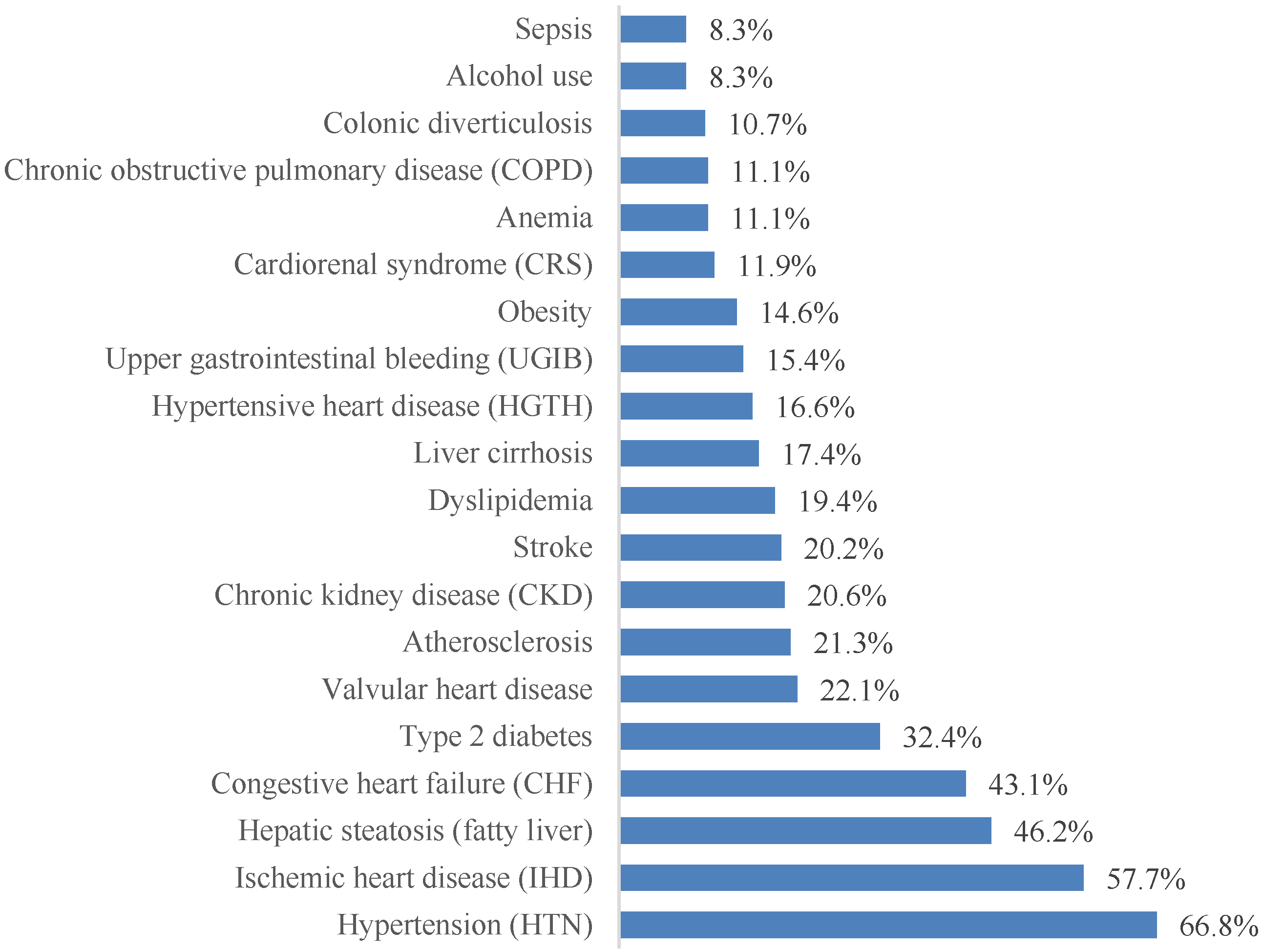
3.3. Spectrum of Comorbidities
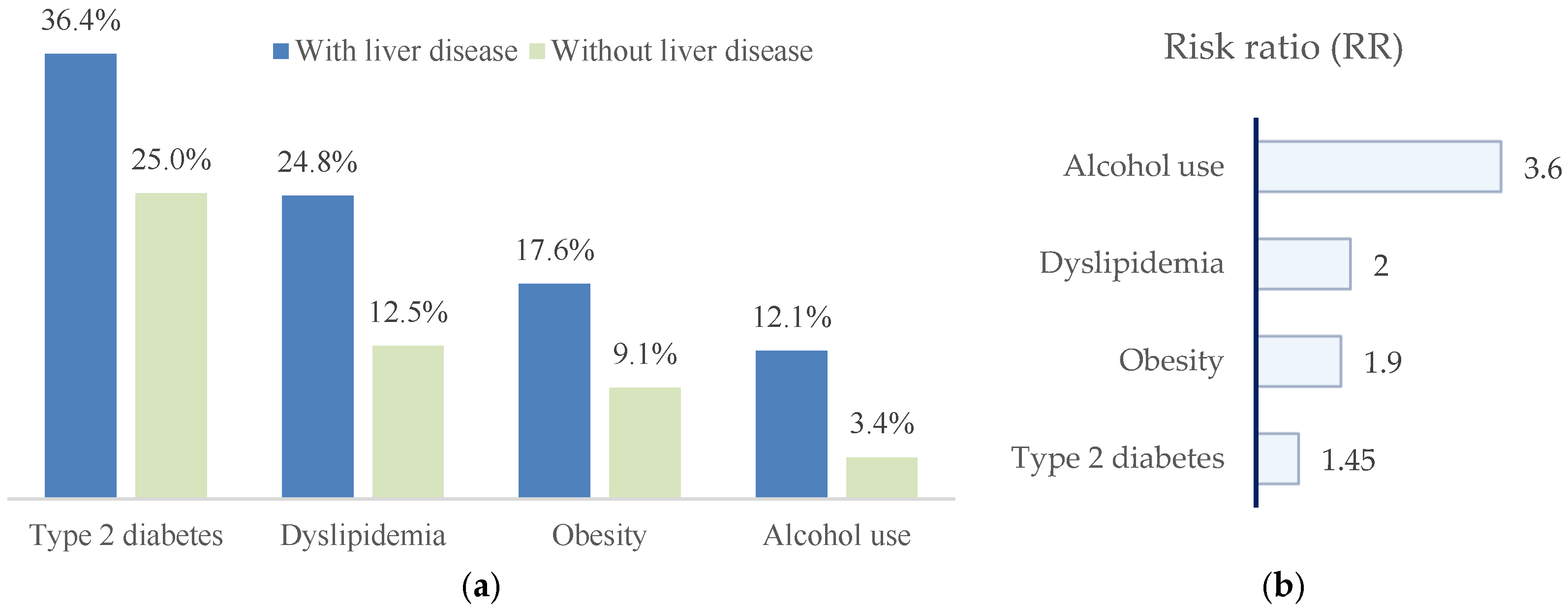
3.4. Liver Pathology in Patients with Paroxysmal AF
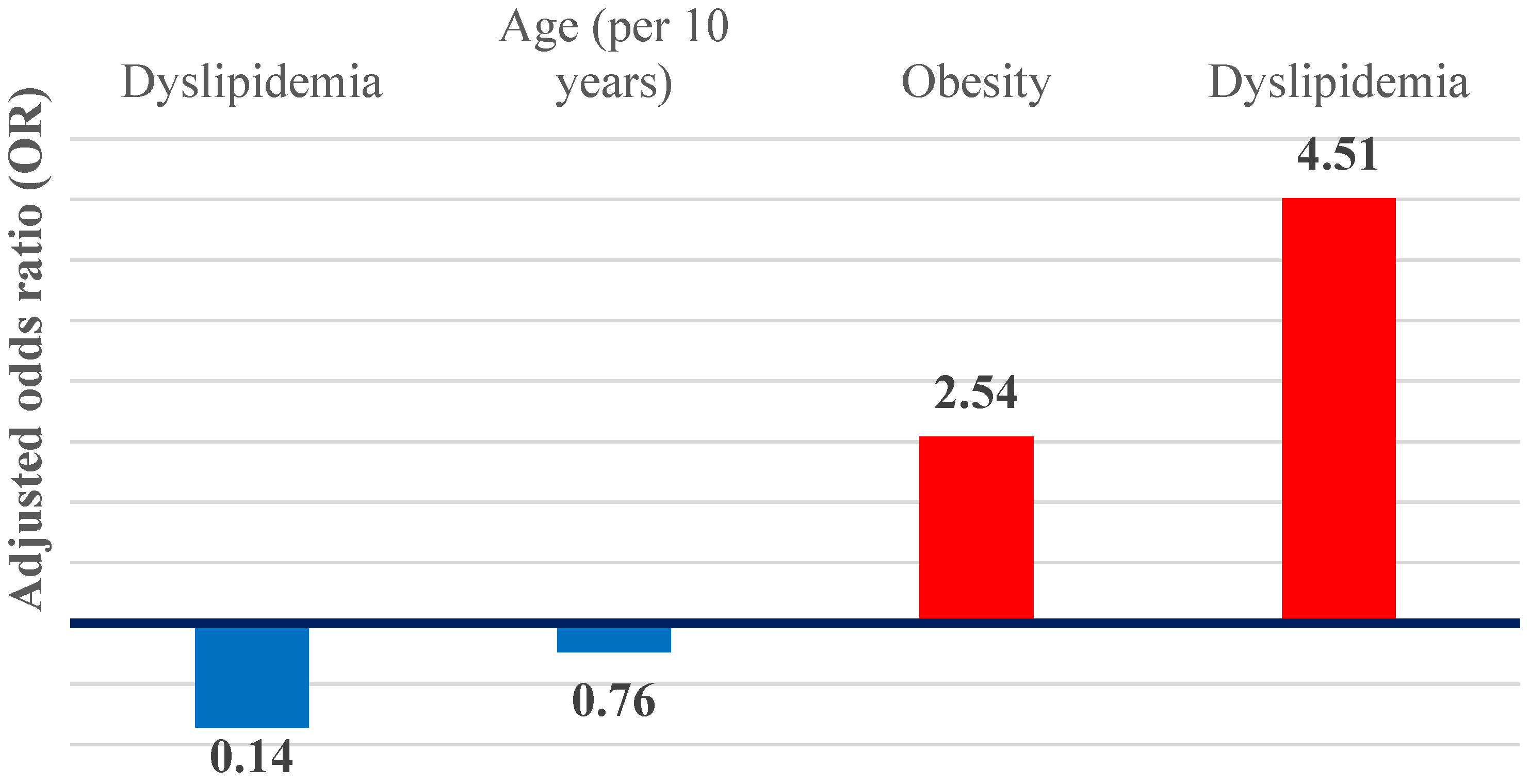
3.5. Independent Predictors and Hepatic Phenotypes
3.6. Serum Biomarker Profiles Across Hepatic Phenotypes
4. Discussion
- A.
- Metabolic–steatosis phenotype
- B.
- Cirrhotic phenotype (lipid paradox)
Study Design Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| AF | Atrial fibrillation |
| AI | Artificial intelligence |
| ALT | Alanine aminotransferase |
| AST | Aspartate aminotransferase |
| BMI | Body mass index |
| BP | Blood pressure |
| CHA2DS2-VASc | Stroke risk score (Congestive heart failure, Hypertension, Age ≥ 75, Diabetes, Stroke/TIA, Vascular disease, Age 65–74, Sex category) |
| CI | Confidence interval |
| COPD | Chronic obstructive pulmonary disease |
| COVID-19 | Coronavirus disease 2019 |
| CT | Computed tomography |
| DRG | Diagnosis-Related Group |
| EPV | Events per variable |
| FIB-4 | Fibrosis-4 index |
| FLI | Fatty liver index |
| GERD | Gastroesophageal reflux disease |
| HDL-C | High-density lipoprotein cholesterol |
| IL | Illinois (in the affiliation “Chicago, IL, USA”) |
| MASH | Metabolic dysfunction-associated steatohepatitis |
| MASLD | Metabolic dysfunction-associated steatotic liver disease |
| MeSH | Medical Subject Headings |
| MRI | Magnetic resonance imaging |
| NAFLD | Nonalcoholic fatty liver disease |
| NLRP3 | NLR family pyrin domain containing 3 (inflammasome) |
| OR | Odds ratio |
| p | p value |
| RR | Risk ratio |
| SPSS | Statistical Package for the Social Sciences |
| TNF-α | Tumor necrosis factor alpha |
| USA | United States of America |
| α | Alpha (significance level) |
| χ2 | Chi-square (test) |
References
- Ohlrogge, A.H.; Brederecke, J.; Schnabel, R.B. Global Burden of Atrial Fibrillation and Flutter by National Income: Results from the Global Burden of Disease 2019 Database. J. Am. Heart Assoc. 2023, 12, e030438. [Google Scholar] [CrossRef]
- Van Gelder, I.C.; Rienstra, M.; Bunting, K.V.; Casado-Arroyo, R.; Caso, V.; Crijns, H.J.G.M.; De Potter, T.J.R.; Dwight, J.; Guasti, L.; Hanke, T.; et al. 2024 ESC Guidelines for the management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS). Eur. Heart J. 2024, 45, 3314–3414, Correction in Eur. Heart J. 2025, 46, 4349. https://doi.org/10.1093/eurheartj/ehaf306. [Google Scholar] [CrossRef]
- Joglar, J.A.; Chung, M.K.; Armbruster, A.L.; Benjamin, E.J.; Chyou, J.Y.; Cronin, E.M.; Deswal, A.; Eckhardt, L.L.; Goldberger, Z.D.; Gopinathannair, R.; et al. 2023 ACC/AHA/ACCP/HRS Guideline for the Diagnosis and Management of Atrial Fibrillation: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. J. Am. Coll. Cardiol. 2024, 83, 109–279. [Google Scholar] [CrossRef] [PubMed]
- Olshansky, B.; Arora, R.K. Mechanisms of Atrial Fibrillation. Available online: https://www.uptodate.com/contents/mechanisms-of-atrial-fibrillation (accessed on 8 July 2025).
- Gorenek, B.; Pelliccia, A.; Benjamin, E.J.; Boriani, G.; Crijns, H.J.; Fogel, R.I.; Van Gelder, I.C.; Halle, M.; Kudaiberdieva, G.; Lane, D.A.; et al. European Heart Rhythm Association (EHRA)/European Association of Cardiovascular Prevention and Rehabilitation (EACPR) position paper on how to prevent atrial fibrillation endorsed by the Heart Rhythm Society (HRS) and Asia Pacific Heart Rhythm Society (APHRS). Europace 2017, 19, 190–225. [Google Scholar] [CrossRef] [PubMed]
- Pierucci, N.; Mariani, M.V.; Iannetti, G.; Maffei, L.; Coluccio, A.; Laviola, D.; Palombi, M.; Trivigno, S.; Spadafora, L.; Chourda, E.; et al. Atrial cardiomyopathy: New pathophysiological and clinical aspects. Minerva Cardiol. Angiol. 2025, in press. [Google Scholar] [CrossRef] [PubMed]
- Bharaj, I.S.; Brar, A.S.; Kahlon, J.; Singh, A.; Hotwani, P.; Kumar, V.; Sohal, A.; Batta, A. Metabolic-dysfunction associated steatotic liver disease and atrial fibrillation: A review of pathogenesis. World J. Cardiol. 2025, 17, 106147. [Google Scholar] [CrossRef]
- Silberberg, A.; Tan, M.K.; Yan, A.T.; Angaran, P.; Dorian, P.; Bucci, C.; Gregoire, J.C.; Bell, A.D.; Gladstone, D.J.; Green, M.S.; et al. Use of Evidence-Based Therapy for Cardiovascular Risk Factors in Canadian Outpatients with Atrial Fibrillation: From the Facilitating Review and Education to Optimize Stroke Prevention in Atrial Fibrillation (FREEDOM AF) and Co-ordinated National Network to Engage Physicians in the Care and Treatment of Patients with Atrial Fibrillation (CONNECT AF). Am. J. Cardiol. 2017, 120, 582–587. [Google Scholar] [CrossRef]
- Danpanichkul, P.; Suparan, K.; Dutta, P.; Kaeosri, C.; Sukphutanan, B.; Pang, Y.; Kulthamrongsri, N.; Jaisa-Aad, M.; Ng, C.H.; Teng, M.; et al. Disparities in metabolic dysfunction-associated steatotic liver disease and cardiometabolic conditions in low and lower middle-income countries: A systematic analysis from the global burden of disease study 2019. Metabolism 2024, 158, 155958. [Google Scholar] [CrossRef]
- Chang, W.H.; Mueller, S.H.; Chung, S.C.; Foster, G.R.; Lai, A.G. Increased burden of cardiovascular disease in people with liver disease: Unequal geographical variations, risk factors and excess years of life lost. J. Transl. Med. 2022, 20, 2. [Google Scholar] [CrossRef]
- Ramadan, M.S.; Russo, V.; Nigro, G.; Durante-Mangoni, E.; Zampino, R. Interplay between Heart Disease and Metabolic Steatosis: A Contemporary Perspective. J. Clin. Med. 2021, 10, 1569. [Google Scholar] [CrossRef]
- Eslam, M.; Newsome, P.N.; Sarin, S.K.; Anstee, Q.M.; Targher, G.; Romero-Gomez, M.; Zelber-Sagi, S.; Wong, V.W.-S.; Dufour, J.-F.; Schattenberg, J.M.; et al. A new definition for metabolic dysfunction-associated fatty liver disease: An international expert consensus statement. J. Hepatol. 2020, 73, 202–209. [Google Scholar] [CrossRef]
- Zhou, B.G.; Ju, S.Y.; Mei, Y.Z.; Jiang, X.; Wang, M.; Zheng, A.-J.; Ding, Y.-B. A systematic review and meta-analysis of cohort studies on the potential association between NAFLD/MAFLD and risk of incident atrial fibrillation. Front. Endocrinol. 2023, 14, 1160532. [Google Scholar] [CrossRef] [PubMed]
- Israelsen, M.; Francque, S.; Tsochatzis, E.A.; Krag, A. Steatotic liver disease. Lancet 2024, 404, 1761–1778. [Google Scholar] [CrossRef] [PubMed]
- Tokushige, K.; Ikejima, K.; Ono, M.; Eguchi, Y.; Kamada, Y.; Itoh, Y.; Akuta, N.; Yoneda, M.; Iwasa, M.; Yoneda, M.; et al. Evidence-based clinical practice guidelines for nonalcoholic fatty liver disease/nonalcoholic steatohepatitis 2020. J. Gastroenterol. 2021, 56, 951–963. [Google Scholar] [CrossRef] [PubMed]
- Rinella, M.E.; Lazarus, J.V.; Ratziu, V.; Francque, S.M.; Sanyal, A.J.; Kanwal, F.; Romero, D.; Abdelmalek, M.F.; Anstee, Q.M.; Arab, J.P.; et al. A multisociety Delphi consensus statement on new fatty liver disease nomenclature. J. Hepatol. 2023, 79, 1542–1556. [Google Scholar] [CrossRef]
- Long, M.T.; Noureddin, M.; Lim, J.K. AGA Clinical Practice Update: Diagnosis and Management of Nonalcoholic Fatty Liver Disease in Lean Individuals: Expert Review. Gastroenterology 2022, 163, 764–774.e1. [Google Scholar] [CrossRef]
- Targher, G.; Valenti, L.; Byrne, C.D. Metabolic Dysfunction-Associated Steatotic Liver Disease. N. Engl. J. Med. 2025, 393, 683–698. [Google Scholar] [CrossRef]
- Cusi, K.; Abdelmalek, M.F.; Apovian, C.M.; Balapattabi, K.; Bannuru, R.R.; Barb, D.; Bardsley, J.K.; Beverly, E.A.; Corbin, K.D.; ElSayed, N.A.; et al. Metabolic Dysfunction-Associated Steatotic Liver Disease (MASLD) in People with Diabetes: The Need for Screening and Early Intervention. A Consensus Report of the American Diabetes Association. Diabetes Care 2025, 48, 1057–1082. [Google Scholar] [CrossRef]
- Rinella, M.E.; Neuschwander-Tetri, B.A.; Siddiqui, M.S.; Abdelmalek, M.F.; Caldwell, S.; Barb, D.; Kleiner, D.E.; Loomba, R. AASLD Practice Guidance on the clinical assessment and management of nonalcoholic fatty liver disease. Hepatology 2023, 77, 1797–1835. [Google Scholar] [CrossRef]
- Lip, G.Y.; Nieuwlaat, R.; Pisters, R.; Lane, D.A.; Crijns, H.J. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor-based approach: The euro heart survey on atrial fibrillation. Chest 2010, 137, 263–272. [Google Scholar] [CrossRef]
- Hindricks, G.; Potpara, T.; Dagres, N.; Arbelo, E.; Bax, J.J.; Blomström-Lundqvist, C.; Boriani, G.; Castella, M.; Dan, G.A.; Dilaveris, P.E.; et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio-Thoracic Surgery (EACTS): The Task Force for the diagnosis and management of atrial fibrillation of the European Society of Cardiology (ESC) Developed with the special contribution of the European Heart Rhythm Association (EHRA) of the ESC. Eur. Heart J. 2021, 42, 373–498. [Google Scholar] [CrossRef]
- Peduzzi, P.; Concato, J.; Kemper, E.; Holford, T.R.; Feinstein, A.R. A simulation study of the number of events per variable in logistic regression analysis. J. Clin. Epidemiol. 1996, 49, 1373–1379. [Google Scholar] [CrossRef] [PubMed]
- Vittinghoff, E.; McCulloch, C.E. Relaxing the rule of ten events per variable in logistic and Cox regression. Am. J. Epidemiol. 2007, 165, 710–718. [Google Scholar] [CrossRef] [PubMed]
- Cho, S.H.; Kim, G.; Lee, K.N.; Oh, R.; Kim, J.Y.; Jang, M.; Lee, Y.-B.; Jin, S.-M.; Hur, K.Y.; Han, K.; et al. Impact of steatotic liver disease categories on atrial fibrillation in type 2 diabetes: A nationwide study. Sci. Rep. 2025, 15, 11430. [Google Scholar] [CrossRef] [PubMed]
- Gong, H.; Liu, X.; Cheng, F. Relationship between non-alcoholic fatty liver disease and cardiac arrhythmia: A systematic review and meta-analysis. J. Int. Med. Res. 2021, 49, 3000605211047074. [Google Scholar] [CrossRef]
- Cai, X.; Zheng, S.; Liu, Y.; Zhang, Y.; Lu, J.; Huang, Y. Nonalcoholic fatty liver disease is associated with increased risk of atrial fibrillation. Liver Int. 2020, 40, 1594–1600. [Google Scholar] [CrossRef]
- Roh, J.H.; Lee, J.H.; Lee, H.; Yoon, Y.; Kim, M.; Kim, Y.; Park, G.; Park, J.; Seong, I. Association between non-alcoholic fatty liver disease and risk of new-onset atrial fibrillation in healthy adults. Liver Int. 2020, 40, 338–346. [Google Scholar] [CrossRef]
- Wijarnpreecha, K.; Boonpheng, B.; Thongprayoon, C.; Jaruvongvanich, V.; Ungprasert, P. The association between non-alcoholic fatty liver disease and atrial fibrillation: A meta-analysis. Clin. Res. Hepatol. Gastroenterol. 2017, 41, 525–532. [Google Scholar] [CrossRef]
- Käräjämäki, A.J.; Hukkanen, J.; Ukkola, O. The association of non-alcoholic fatty liver disease and atrial fibrillation: A review. Ann. Med. 2018, 50, 371–380. [Google Scholar] [CrossRef]
- Long, M.T.; Yin, X.; Larson, M.G.; Ellinor, P.T.; Lubitz, S.A.; McManus, D.D.; Magnani, J.W.; Staerk, L.; Ko, D.; Helm, R.H.; et al. Relations of Liver Fat with Prevalent and Incident Atrial Fibrillation in the Framingham Heart Study. J. Am. Heart Assoc. 2017, 6, e005227. [Google Scholar] [CrossRef]
- Argano, C. Editorial: Interactions between NAFLD and cardiac conduction, structure and function: Recent advances and treatments. Front. Endocrinol. 2023, 14, 1334227. [Google Scholar] [CrossRef] [PubMed]
- Minhas, A.M.; Usman, M.S.; Khan, M.S.; Fatima, K.; Mangi, M.A.; Illovsky, M.A. Link Between Non-Alcoholic Fatty Liver Disease and Atrial Fibrillation: A Systematic Review and Meta-Analysis. Cureus 2017, 9, e1142. [Google Scholar] [CrossRef] [PubMed]
- Alon, L.; Corica, B.; Raparelli, V.; Cangemi, R.; Basili, S.; Proietti, M.; Romiti, G.F. Risk of cardiovascular events in patients with non-alcoholic fatty liver disease: A systematic review and meta-analysis. Eur. J. Prev. Cardiol. 2022, 29, 938–946. [Google Scholar] [CrossRef] [PubMed]
- Bisaccia, G.; Ricci, F.; Khanji, M.Y.; Sorella, A.; Melchiorre, E.; Iannetti, G.; Galanti, K.; Mantini, C.; Pizzi, A.D.; Tana, C.; et al. Cardiovascular Morbidity and Mortality Related to Non-alcoholic Fatty Liver Disease: A Systematic Review and Meta-analysis. Curr. Probl. Cardiol. 2023, 48, 101643. [Google Scholar] [CrossRef]
- Tana, C.; Ballestri, S.; Ricci, F.; Di Vincenzo, A.; Ticinesi, A.; Gallina, S.; Giamberardino, M.A.; Cipollone, F.; Sutton, R.; Vettor, R.; et al. Cardiovascular Risk in Non-Alcoholic Fatty Liver Disease: Mechanisms and Therapeutic Implications. Int. J. Environ. Res. Public Health 2019, 16, 3104. [Google Scholar] [CrossRef]
- Mangi, M.A.; Rehman, H.; Minhas, A.M.; Rafique, M.; Bansal, V.; Constantin, J. Non-Alcoholic Fatty Liver Disease Association with Cardiac Arrhythmias. Cureus 2017, 9, e1165. [Google Scholar] [CrossRef]
- Ding, Y.H.; Ma, Y.; Qian, L.Y.; Xu, Q.; Wang, L.-H.; Huang, D.-S.; Zou, H. Linking atrial fibrillation with non-alcoholic fatty liver disease: Potential common therapeutic targets. Oncotarget 2017, 8, 60673–60683. [Google Scholar] [CrossRef]
- Zhou, Y.; Lai, C.; Peng, C.; Chen, M.; Li, B.; Wang, X.; Sun, J.; Sun, C. Nonalcoholic fatty liver disease as a predictor of atrial fibrillation: A systematic review and meta-analysis. Postepy Kardiol. Interwencyjnej 2017, 13, 250–257. [Google Scholar] [CrossRef]
- Kang, M.K.; Park, J.G.; Kim, M.C. Association between Atrial Fibrillation and Advanced Liver Fibrosis in Patients with Non-Alcoholic Fatty Liver Disease. Yonsei Med. J. 2020, 61, 860–867. [Google Scholar] [CrossRef]
- Park, H.E.; Lee, H.; Choi, S.Y.; Kim, H.S.; Chung, G.E. The risk of atrial fibrillation in patients with non-alcoholic fatty liver disease and a high hepatic fibrosis index. Sci. Rep. 2020, 10, 5023. [Google Scholar] [CrossRef]
- Cho, E.J.; Chung, G.E.; Yoo, J.J.; Cho, Y.; Na Lee, K.; Shin, D.W.; Kim, Y.J.; Yoon, J.-H.; Han, K.; Yu, S.J. Association of nonalcoholic fatty liver disease with new-onset atrial fibrillation stratified by age groups. Cardiovasc. Diabetol. 2024, 23, 340. [Google Scholar] [CrossRef] [PubMed]
- Choi, J.; Lee, S.R.; Choi, E.K.; Ahn, H.-J.; Kwon, S.; Park, S.-H.; Lee, H.; Chung, J.; Han, M.; Lee, S.-W.; et al. Non-alcoholic Fatty Liver Disease and the Risk of Incident Atrial Fibrillation in Young Adults: A Nationwide Population-Based Cohort Study. Front. Cardiovasc. Med. 2022, 9, 832023. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Byrne, C.D.; Benfari, G.; Bonapace, S.; Simon, T.G.; Targher, G. Risk of Heart Failure in Patients with Nonalcoholic Fatty Liver Disease: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2022, 79, 180–191. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Liu, J.; Zhou, F.; Li, H.; Zhang, X.-J.; She, Z.-G.; Lu, Z.; Cai, J.; Li, H. Nonalcoholic Fatty Liver Disease: An Emerging Driver of Cardiac Arrhythmia. Circ. Res. 2021, 128, 1747–1765. [Google Scholar] [CrossRef]
- Wang, L.; Zhang, Y.; Yu, B.; Zhao, J.; Zhang, W.; Fan, H.; Ren, Z.; Liang, B. The monocyte-to-high-density lipoprotein ratio is associated with the occurrence of atrial fibrillation among NAFLD patients: A propensity-matched analysis. Front. Endocrinol. 2023, 14, 1127425. [Google Scholar] [CrossRef]
- Liu, G.; Zhang, Q.; Zhou, M.; Li, B.; Zhao, J.; Bai, R.; Song, X.; Qin, W.; Zhang, Y. Correlation between serum uric acid to high-density lipoprotein cholesterol ratio and atrial fibrillation in patients with NAFLD. PLoS ONE 2024, 19, e0305952. [Google Scholar] [CrossRef]
- Dimala, C.A.; Nso, N.; Wasserlauf, J.; Njei, B. Electrocardiographic abnormalities in patients with metabolic dysfunction-associated steatotic liver disease: A systematic review and meta-analysis. Curr. Probl. Cardiol. 2024, 49, 102580. [Google Scholar] [CrossRef]
- Decoin, R.; Butruille, L.; Defrancq, T.; Robert, J.; Destrait, N.; Coisne, A.; Aghezzaf, S.; Woitrain, E.; Gouda, Z.; Schino, S.; et al. High liver fibrosis scores in metabolic dysfunction-associated fatty liver disease patients are associated with adverse atrial remodeling and atrial fibrillation recurrence following catheter ablation. Front. Endocrinol. 2022, 13, 957245. [Google Scholar] [CrossRef]
- Ninni, S.; Algalarrondo, V.; Brette, F.; Lemesle, G.; Fauconnier, J. Groupe de Reflexion sur la Recherche Cardiovasculaire (GRRC). Left atrial cardiomyopathy: Pathophysiological insights, assessment methods and clinical implications. Arch. Cardiovasc. Dis. 2024, 117, 283–296. [Google Scholar] [CrossRef]
- Donnellan, E.; Cotter, T.G.; Wazni, O.M.; Elshazly, M.B.; Kochar, A.; Wilner, B.; Patel, D.; Kanj, M.; Hussein, A.; Baranowski, B.; et al. Impact of Nonalcoholic Fatty Liver Disease on Arrhythmia Recurrence Following Atrial Fibrillation Ablation. JACC Clin. Electrophysiol. 2020, 6, 1278–1287. [Google Scholar] [CrossRef]
- AlTurki, A.; Essebag, V. Atrial Fibrillation Ablation: Impact on Burden and Cardiovascular Outcomes. J. Clin. Med. 2025, 14, 2648. [Google Scholar] [CrossRef]
- Matteucci, A.; Russo, M.; Galeazzi, M.; Pandozi, C.; Bonanni, M.; Mariani, M.V.; Pierucci, N.; La Fazia, V.M.; Di Fusco, S.A.; Nardi, F.; et al. Impact of Ablation Energy Sources on Perceived Quality of Life and Symptom in Atrial Fibrillation Patients: A Comparative Study. J. Clin. Med. 2025, 14, 2741. [Google Scholar] [CrossRef] [PubMed]
- Mantovani, A.; Morandin, R.; Sani, E.; Fiorio, V.; Shtembari, E.; Bonapace, S.; Petta, S.; Polyzos, S.A.; Byrne, C.D.; Targher, G. MASLD Is Associated with an Increased Long-Term Risk of Atrial Fibrillation: An Updated Systematic Review and Meta-Analysis. Liver Int. 2025, 45, e16128. [Google Scholar] [CrossRef] [PubMed]
- Huang, J.K.; Lee, H.C. Emerging Evidence of Pathological Roles of Very-Low-Density Lipoprotein (VLDL). Int. J. Mol. Sci. 2022, 23, 4300. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Wang, T.; Song, J. A review regarding the article ‘Electrocardiographic abnormalities in patients with metabolic dysfunction-associated Steatotic liver disease: A systematic review and meta-analysis’. Curr. Probl. Cardiol. 2024, 49, 102626. [Google Scholar] [CrossRef]
- Simon, T.G.; Ebrahimi, F.; Roelstraete, B.; Hagström, H.; Sundström, J.; Ludvigsson, J.F. Incident cardiac arrhythmias associated with metabolic dysfunction-associated steatotic liver disease: A nationwide histology cohort study. Cardiovasc. Diabetol. 2023, 22, 343. [Google Scholar] [CrossRef]
- Cheung, J.; Cheung, B.M.; Yiu, K.H.; Tse, H.F.; Chan, Y.H. Role of metabolic dysfunction-associated fatty liver disease in atrial fibrillation and heart failure: Molecular and clinical aspects. Front. Cardiovasc. Med. 2025, 12, 1573841. [Google Scholar] [CrossRef]
- Driessen, S.; Francque, S.M.; Anker, S.D.; Cabezas, M.C.; Grobbee, D.E.; Tushuizen, M.E.; Holleboom, A.G. Metabolic dysfunction-associated steatotic liver disease and the heart. Hepatology 2023, 82, 487–503. [Google Scholar] [CrossRef]
- Ezeani, C.; Omaliko, C.; Al-Ajlouni, Y.A.; Njei, B. Mortality, Hepatic Decompensation, and Cardiovascular- and Renal-Related Outcomes in Lean Versus Non-lean Patients Hospitalized with Metabolic Dysfunction-Associated Steatohepatitis (MASH). Cureus 2024, 16, e60968. [Google Scholar] [CrossRef]
- Einarsson, G.; Thorleifsson, G.; Steinthorsdottir, V.; Zink, F.; Helgason, H.; Olafsdottir, T.; Rognvaldsson, S.; Tragante, V.; Ulfarsson, M.O.; Sveinbjornsson, G.; et al. Sequence variants associated with BMI affect disease risk through BMI itself. Nat. Commun. 2024, 15, 9335. [Google Scholar] [CrossRef]
- Lee, S.R.; Han, K.D.; Choi, E.K.; Oh, S.; Lip, G.Y.H. Nonalcoholic fatty liver disease and the risk of atrial fibrillation stratified by body mass index: A nationwide population-based study. Sci. Rep. 2021, 11, 3737. [Google Scholar] [CrossRef] [PubMed]
- Roca-Fernandez, A.; Banerjee, R.; Thomaides-Brears, H.; Telford, A.; Sanyal, A.; Neubauer, S.; Nichols, T.E.; Raman, B.; McCracken, C.; Petersen, S.E.; et al. Liver disease is a significant risk factor for cardiovascular outcomes—A UK Biobank study. J. Hepatol. 2023, 79, 1085–1095. [Google Scholar] [CrossRef] [PubMed]
- Estes, N.A.M.; Jain, S.K. Risk Factor Modification for Atrial Fibrillation: An Ounce of Prevention. JACC Clin. Electrophysiol. 2020, 6, 1288–1290. [Google Scholar] [CrossRef] [PubMed]
- Mairesse, G.H.; Moran, P.; Van Gelder, I.C.; Elsner, C.; Rosenqvist, M.; Mant, J.; Banerjee, A.; Gorenek, B.; Brachmann, J.; Varma, N.; et al. Screening for atrial fibrillation: A European Heart Rhythm Association (EHRA) consensus document endorsed by the Heart Rhythm Society (HRS), Asia Pacific Heart Rhythm Society (APHRS), and Sociedad Latinoamericana de Estimulación Cardíaca y Electrofisiología (SOLAECE). Europace 2017, 19, 1589–1623. [Google Scholar] [CrossRef]
- Chung, M.K.; Eckhardt, L.L.; Chen, L.Y.; Ahmed, H.M.; Gopinathannair, R.; Joglar, J.A.; Noseworthy, P.A.; Pack, Q.R.; Sanders, P.; Trulock, K.M.; et al. Lifestyle and Risk Factor Modification for Reduction of Atrial Fibrillation: A Scientific Statement from the American Heart Association. Circulation 2020, 141, e750–e772. [Google Scholar] [CrossRef]
- Huang, W.A.; Dunipace, E.A.; Sorg, J.M.; Vaseghi, M. Liver Disease as a Predictor of New-Onset Atrial Fibrillation. J. Am. Heart Assoc. 2018, 7, e008703. [Google Scholar] [CrossRef]
- Darrat, Y.H.; Smer, A.; Elayi, C.S.; Morales, G.X.; Alqahtani, F.; Alkhouli, M.; Catanzaro, J.; Shah, J.; Salih, M. Mortality and morbidity in patients with atrial fibrillation and liver cirrhosis. World J. Cardiol. 2020, 12, 342–350. [Google Scholar] [CrossRef]
- Godtfredsen, S.J.; Kragholm, K.H.; Pareek, M. Atrial fibrillation in patients with liver disease: Recent advances. Kardiol. Pol. 2023, 81, 950–959. [Google Scholar] [CrossRef]
- Lee, H.; Choi, E.K.; Rhee, T.M.; Lee, S.; Lim, W.; Kang, S.; Han, K.; Cha, M.; Oh, S. Cirrhosis is a risk factor for atrial fibrillation: A nationwide, population-based study. Liver Int. 2017, 37, 1660–1667. [Google Scholar] [CrossRef]
- Chokesuwattanaskul, R.; Thongprayoon, C.; Bathini, T.; O’corragain, O.A.; Sharma, K.; Preechawat, S.; Wijarnpreecha, K.; Kröner, P.T.; Ungprasert, P.; Cheungpasitporn, W. Epidemiology of atrial fibrillation in patients with cirrhosis and clinical significance: A meta-analysis. Eur. J. Gastroenterol. Hepatol. 2019, 31, 514–519. [Google Scholar] [CrossRef]
- Han, H.; Qin, Y.; Yu, Y.; Wei, X.; Guo, H.; Ruan, Y.; Cao, Y.; He, J. Atrial fibrillation in hospitalized patients with end-stage liver disease: Temporal trends in prevalence and outcomes. Liver Int. 2020, 40, 674–684. [Google Scholar] [CrossRef]
- Adejumo, A.C.; Adejumo, K.L.; Akanbi, O.; Adegbala, O.M.; Alayo, Q.A.; Fijabi, D.O.; Ogundipe, O.A.; Almaddah, N.; Pani, L.; Adeboye, A. Predictors, burden and impact of cardiac arrhythmias among patients hospitalized with end-stage liver disease. Heart Lung 2020, 49, 73–79. [Google Scholar] [CrossRef]
- Mozos, I. Arrhythmia risk in liver cirrhosis. World J. Hepatol. 2015, 7, 662–672. [Google Scholar] [CrossRef] [PubMed]
- Mann, J.P.; Carter, P.; Armstrong, M.J.; Abdelaziz, H.K.; Uppal, H.; Patel, B.; Chandran, S.; More, R.; Newsome, P.N.; Potluri, R. Hospital admission with non-alcoholic fatty liver disease is associated with increased all-cause mortality independent of cardiovascular risk factors. PLoS ONE 2020, 15, e0241357. [Google Scholar] [CrossRef] [PubMed]
- Prenner, S.B.; Kumar, A.; Zhao, L.; Cvijic, M.E.; Basso, M.; Spires, T.; Li, Z.; Yarde, M.; Bhattacharya, P.; Zamani, P.; et al. Effect of Serum Albumin Levels in Patients with Heart Failure with Preserved Ejection Fraction (from the TOPCAT Trial). Am. J. Cardiol. 2020, 125, 575–582. [Google Scholar] [CrossRef] [PubMed]
- Lu, X.; Wang, Z.; Yang, L.; Yang, C.; Song, M. Risk Factors of Atrial Arrhythmia in Patients with Liver Cirrhosis: A Retrospective Study. Front. Cardiovasc. Med. 2021, 8, 704073. [Google Scholar] [CrossRef]
- Luo, Y.; Wu, B.; Wu, Y.; Peng, L.; Li, Z.; Zhu, J.; Su, Z.; Liu, J.; Li, S.; Chong, Y. Atrial fibrillation increases inpatient and 4-year all-cause mortality in critically ill patients with liver cirrhosis. Ann. Transl. Med. 2021, 9, 1239. [Google Scholar] [CrossRef]
- Obi, M.F.; Reinberg Palmar, A.; Namireddy, V.; Campos, F.N.; Cho, H.J. The Liver-Heart Connection: A Literature Review of Liver Disease as a Risk Factor for Atrial Fibrillation. Cureus 2023, 15, e38536. [Google Scholar] [CrossRef]
- Violi, F.; Nocella, C.; Bartimoccia, S.; Castellani, V.; Carnevale, R.; Pignatelli, P.; Cammisotto, V. Gut dysbiosis-derived low-grade endotoxemia: A common basis for liver and cardiovascular disease. Kardiol. Pol. 2023, 81, 563–571. [Google Scholar] [CrossRef]
- Wu, H.H.L.; Rakisheva, A.; Ponnusamy, A.; Chinnadurai, R. Hepatocardiorenal syndrome in liver cirrhosis: Recognition of a new entity? World J. Gastroenterol. 2024, 30, 128–136. [Google Scholar] [CrossRef]
- van Kleef, L.A.; Lu, Z.; Ikram, M.A.; de Groot, N.M.S.; Kavousi, M.; de Knegt, R.J. Liver stiffness not fatty liver disease is associated with atrial fibrillation: The Rotterdam study. J. Hepatol. 2022, 77, 931–938. [Google Scholar] [CrossRef] [PubMed]
- Ikram, M.A.; Kieboom, B.C.T.; Brouwer, W.P.; Brusselle, G.; Chaker, L.; Ghanbari, M.; Goedegebure, A.; Ikram, M.K.; Kavousi, M.; de Knegt, R.J.; et al. The Rotterdam Study. Design update and major findings between 2020 and 2024. Eur. J. Epidemiol. 2024, 39, 183–206. [Google Scholar] [CrossRef] [PubMed]
- Saito, Y.; Okumura, Y.; Nagashima, K.; Fukamachi, D.; Yokoyama, K.; Matsumoto, N.; Tachibana, E.; Kuronuma, K.; Oiwa, K.; Matsumoto, M.; et al. Impact of the Fibrosis-4 Index on Risk Stratification of Cardiovascular Events and Mortality in Patients with Atrial Fibrillation: Findings from a Japanese Multicenter Registry. J. Clin. Med. 2020, 9, 584. [Google Scholar] [CrossRef]
- Boeckmans, J.; Michel, M.; Gieswinkel, A.; Tüscher, O.; Konstantinides, S.V.; König, J.; Münzel, T.; Lackner, K.J.; Kerahrodi, J.G.; Schuster, A.K.; et al. Inflammation in liver fibrosis and atrial fibrillation: A prospective population-based proteomic study. JHEP Rep. 2024, 6, 101171. [Google Scholar] [CrossRef] [PubMed]
- Chu, Y.; Yu, F.; Wu, Y.; Yang, J.; Shi, J.; Ye, T.; Han, D.; Wang, X. Identification of genes and key pathways underlying the pathophysiological association between nonalcoholic fatty liver disease and atrial fibrillation. BMC Med. Genom. 2022, 15, 150. [Google Scholar] [CrossRef]
- Roberts, J.D.; Chalazan, B.; Andrade, J.G.; Macle, L.; Nattel, S.; Tadros, R. Clinical Genetic Testing for Atrial Fibrillation: Are We There Yet? Can. J. Cardiol. 2024, 40, 540–553. [Google Scholar] [CrossRef]
- Long, M.T.; Ko, D.; Arnold, L.M.; Trinquart, L.; Sherer, J.A.; Keppel, S.-S.; Benjamin, E.J.; Helm, R.H. Gastrointestinal and liver diseases and atrial fibrillation: A review of the literature. Therap. Adv. Gastroenterol. 2019, 12, 1756284819832237. [Google Scholar] [CrossRef]
- Huang, W.; Xu, S.; Zhou, H.; Ji, W.; Chen, Y. Global association of incidence between atrial fibrillation and the major gastrointestinal cancers: An analysis based on the 2019 Global burden of disease study. Heliyon 2024, 10, e29929. [Google Scholar] [CrossRef]
- Mehta, A.; Bath, A.; Ahmed, M.U.; Kalavakunta, J.K. Rare and unusual presentation of gastrocardiac syndrome. BMJ Case Rep. 2020, 13, e236910. [Google Scholar] [CrossRef]
- Mohamed, A.; Ochoa Crespo, D.; Kaur, G.; Ashraf, I.; Peck, M.M.; Maram, R.; Malik, B.H. Gastroesophageal Reflux and Its Association with Atrial Fibrillation: A Traditional Review. Cureus 2020, 12, e10387. [Google Scholar] [CrossRef]
- Williams, E.G.; Alissa, M.; Alsugoor, M.H.; Albakri, G.S.; Altamimi, A.A.; Alabdullateef, A.A.; Almansour, N.M.; Aldakheel, F.M.; Alessa, S.; Marber, M. Integrative approaches to atrial fibrillation prevention and management: Leveraging gut health for improved cardiovascular outcomes in the aging population. Curr. Probl. Cardiol. 2025, 50, 102952. [Google Scholar] [CrossRef] [PubMed]
- Attia, Z.I.; Noseworthy, P.A.; Lopez-Jimenez, F.; Asirvatham, S.J.; Deshmukh, A.J.; Gersh, B.J.; Carter, R.E.; Yao, X.; Rabinstein, A.A.; Erickson, B.J.; et al. An artificial intelligence-enabled ECG algorithm for the identification of patients with atrial fibrillation during sinus rhythm: A retrospective analysis of outcome prediction. Lancet 2019, 394, 861–867. [Google Scholar] [CrossRef]
- Attia, Z.I.; Kapa, S.; Lopez-Jimenez, F.; McKie, P.M.; Ladewig, D.J.; Satam, G.; Pellikka, P.A.; Enriquez-Sarano, M.; Noseworthy, P.A.; Munger, T.M.; et al. Screening for cardiac contractile dysfunction using an artificial intelligence-enabled electrocardiogram. Nat. Med. 2019, 25, 70–74. [Google Scholar] [CrossRef] [PubMed]
- Johnson, K.W.; Torres Soto, J.; Glicksberg, B.S.; Shameer, K.; Miotto, R.; Ali, M.; Ashley, E.; Dudley, J.T. Artificial Intelligence in Cardiology. J. Am. Coll. Cardiol. 2018, 71, 2668–2679. [Google Scholar] [CrossRef] [PubMed]
- Hannun, A.Y.; Rajpurkar, P.; Haghpanahi, M.; Tison, G.H.; Bourn, C.; Turakhia, M.P.; Ng, A.Y. Cardiologist-level arrhythmia detection and classification in ambulatory electrocardiograms using a deep neural network. Nat. Med. 2019, 25, 65–69. [Google Scholar] [CrossRef]
- Karakasis, P.; Theofilis, P.; Sagris, M.; Pamporis, K.; Stachteas, P.; Sidiropoulos, G.; Vlachakis, P.K.; Patoulias, D.; Antoniadis, A.P.; Fragakis, N. Artificial Intelligence in Atrial Fibrillation: From Early Detection to Precision Therapy. J. Clin. Med. 2025, 14, 2627. [Google Scholar] [CrossRef]
- Capisizu, A.; Zamfirescu, A.; Aurelian, S.M.; Dina, I. Results of prevalence study regarding comorbidities for various patients. Rom. Stat. Rev. 2013, 61, 75–87. [Google Scholar]
- Omer, S.; Zara, O.; Iacobescu, C.; Dina, I. Partial splenic embolization for hypersplenism in cirrhotic patients. A case series. J. Gastrointestin Liver Dis. 2014, 23, 215–218. [Google Scholar] [CrossRef]
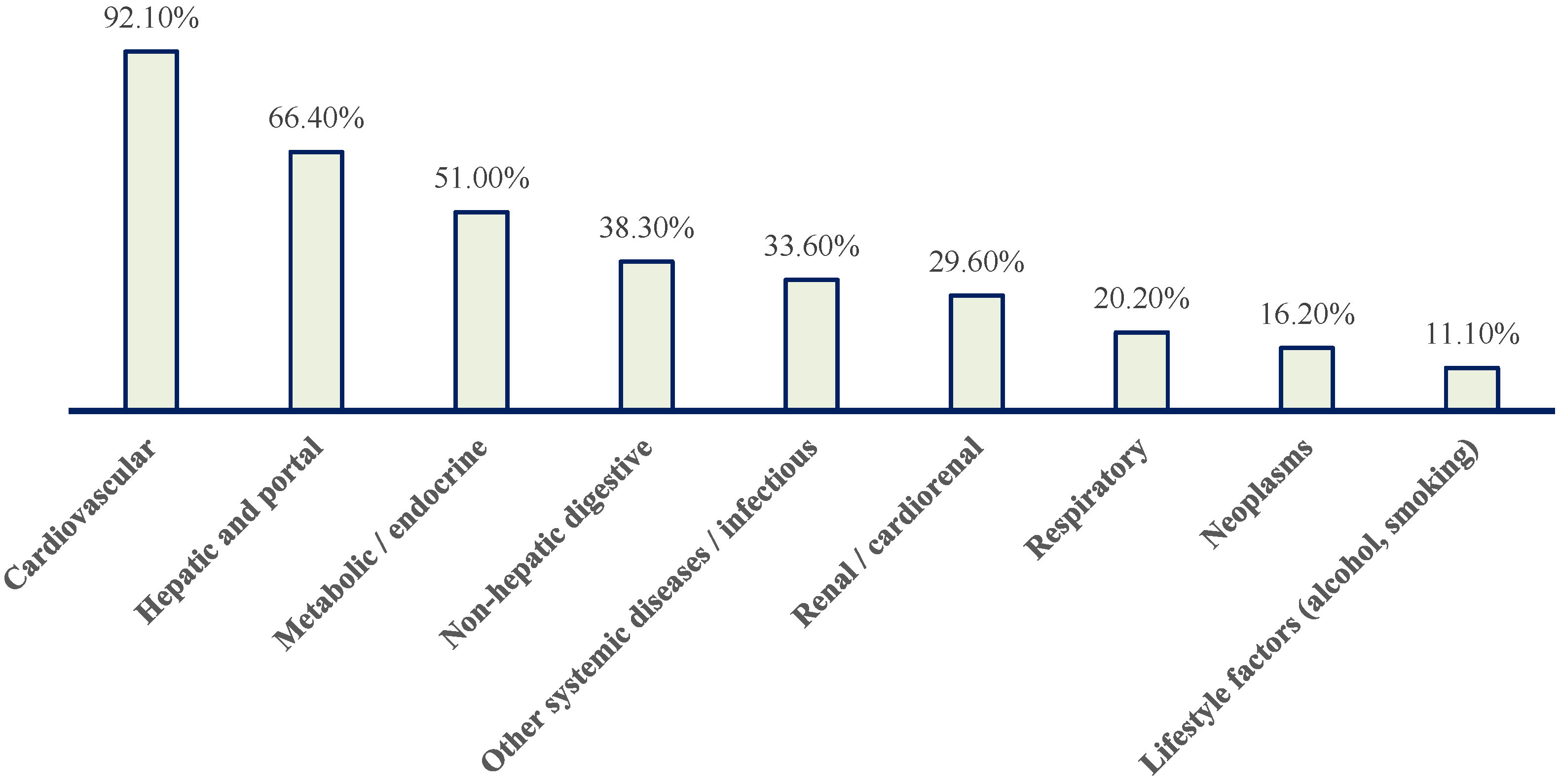
| Comorbidity Category | Included Conditions |
|---|---|
| Cardiovascular | Arterial hypertension, coronary artery disease, chronic heart failure, valvular heart disease, stroke, conduction disorders, pacemaker implantation |
| Hepatic and portal | Hepatic steatosis, liver cirrhosis, chronic liver failure, ascites, esophageal varices, primary and secondary liver tumors |
| Metabolic/endocrine | Type 2 diabetes mellitus, dyslipidemia, obesity, hypothyroidism |
| Non-hepatic digestive | Gastroesophageal reflux disease, diverticulosis, gastrointestinal bleeding, colonic polyps |
| Renal | Chronic kidney disease, benign renal tumors |
| Respiratory | Chronic obstructive pulmonary disease, asthma, pulmonary fibrosis, obstructive sleep apnea |
| Neoplastic | Digestive, pulmonary, urological, breast, thyroid, hematological malignancies |
| Other systemic/infectious | Anemia, sepsis, COVID-19, autoimmune disorders |
| Lifestyle factors | Alcohol consumption, smoking |
| Parameter | No Liver Disease | Hepatic Steatosis | Advanced Liver Disease/Cirrhosis | p (Kruskal–Wallis) |
|---|---|---|---|---|
| ALT (U/L) | 18.20 [10.00–34.90], N = 31 | 22.20 [16.30–43.20], N = 45 | 26.60 [14.07–41.35], N = 22 | 0.39681 |
| AST (U/L) | 19.10 [13.60–45.95], N = 31 | 23.00 [18.00–30.95], N = 47 | 31.70 [20.80–79.00], N = 21 | 0.02153 |
| Albumin | 3.64 [2.81–4.03], N = 16 | 3.76 [3.44–4.36], N = 30 | 3.23 [2.54–3.79], N = 18 | 0.01052 |
| Total bilirubin | 0.44 [0.33–0.62], N = 35 | 0.67 [0.40–0.86], N = 50 | 0.95 [0.56–1.83], N = 21 | 0.00177 |
| Alkaline phosphatase (ALP) | 77.00 [53.50–92.00], N = 18 | 66.00 [56.00–97.00], N = 35 | 100.00 [74.50–115.25], N = 14 | 0.02532 |
| Cholesterol | 138.40 [120.90–158.20], N = 29 | 177.00 [132.55–207.80], N = 40 | 115.85 [80.70–153.90], N = 20 | 0.00118 |
| Triglycerides | 104.95 [66.92–145.25], N = 24 | 95.75 [78.58–150.18], N = 36 | 87.80 [62.32–103.95], N = 18 | 0.30758 |
| INR | 1.34 [1.12–2.09], N = 32 | 1.12 [1.04–1.20], N = 50 | 1.61 [1.28–2.47], N = 26 | 0.00001 |
| Platelets (/µL) | 242,500 [190,500–327,750], N = 38 | 239,000 [193,500–317,250], N = 54 | 166,000 [106,500–252,500], N = 27 | 0.00318 |
| Hemoglobin | 9.00 [6.72–12.65], N = 39 | 12.70 [10.08–14.00], N = 54 | 10.70 [8.85–12.45], N = 27 | 0.00154 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Bălăceanu, L.A.; Grigore, C.; Bălăceanu-Gurău, B.; Gurău, C.-D.; Grigorescu, I.V.; Dina, I. Paroxysmal Atrial Fibrillation in Liver Diseases: Epidemiology and Possible Pathophysiological Mechanisms. J. Clin. Med. 2026, 15, 1156. https://doi.org/10.3390/jcm15031156
Bălăceanu LA, Grigore C, Bălăceanu-Gurău B, Gurău C-D, Grigorescu IV, Dina I. Paroxysmal Atrial Fibrillation in Liver Diseases: Epidemiology and Possible Pathophysiological Mechanisms. Journal of Clinical Medicine. 2026; 15(3):1156. https://doi.org/10.3390/jcm15031156
Chicago/Turabian StyleBălăceanu, Lavinia Alice, Cristiana Grigore, Beatrice Bălăceanu-Gurău, Cristian-Dorin Gurău, Ioana Valeria Grigorescu, and Ion Dina. 2026. "Paroxysmal Atrial Fibrillation in Liver Diseases: Epidemiology and Possible Pathophysiological Mechanisms" Journal of Clinical Medicine 15, no. 3: 1156. https://doi.org/10.3390/jcm15031156
APA StyleBălăceanu, L. A., Grigore, C., Bălăceanu-Gurău, B., Gurău, C.-D., Grigorescu, I. V., & Dina, I. (2026). Paroxysmal Atrial Fibrillation in Liver Diseases: Epidemiology and Possible Pathophysiological Mechanisms. Journal of Clinical Medicine, 15(3), 1156. https://doi.org/10.3390/jcm15031156






