The Efficacy of Prone Single-Position Lateral Lumbar Interbody Fusion for Symptomatic Cranial Adjacent Segment Degeneration
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
2.2. Clinical and Radiological Assessment
2.3. Statistical Analyses
2.4. Surgical Technique
3. Results
3.1. Patient Demographics and Operative Characteristics
3.2. Clinical Outcomes
3.3. Radiological Outcomes
3.4. Complications
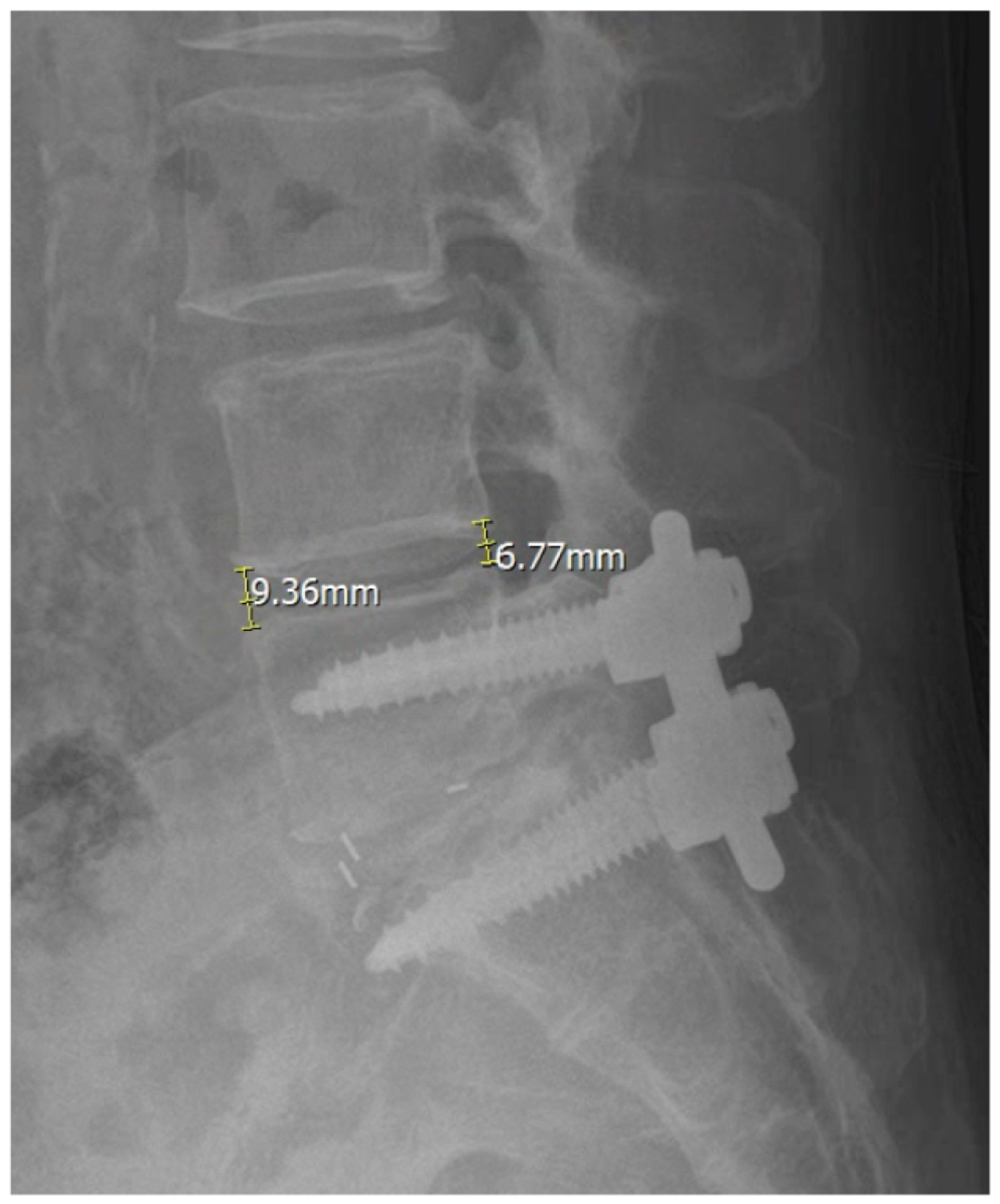
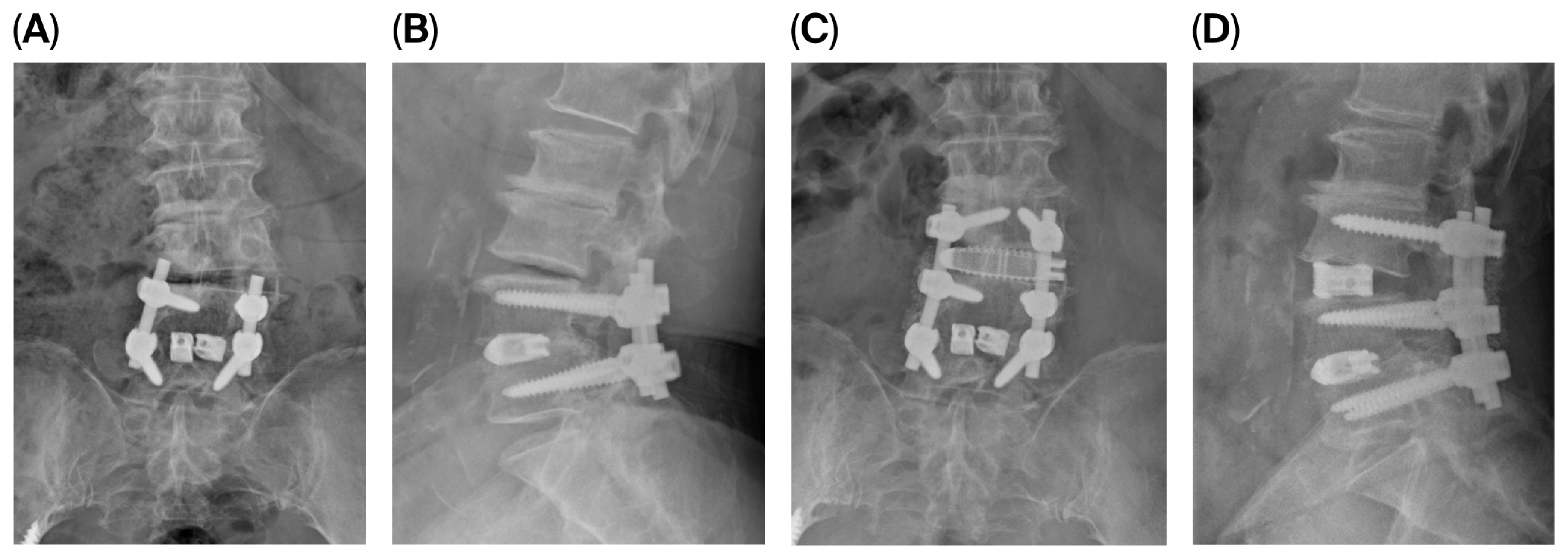
3.5. Illustrative Case
4. Discussion
4.1. Rationale for Single-Position Surgery and Its Clinical Significance
4.2. Advantages of the Prone Single-Position Approach
4.3. Complication Profile in the Context of the Existing Literature
4.4. Anatomical Implications of Prone Positioning
4.5. Technical Considerations for Safe Execution
4.6. Variations in Surgical Technique: Prone Transpsoas vs. Prone Pre-Psoas Corridor
4.7. Study Limitations
4.8. Clinical Implications and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Lee, J.C.; Choi, S.W. Adjacent Segment Pathology After Lumbar Spinal Fusion. Asian Spine J. 2015, 9, 807–817. [Google Scholar] [CrossRef]
- Park, P.; Garton, H.J.; Gala, V.C.; Hoff, J.T.; McGillicuddy, J.E. Adjacent segment disease after lumbar or lumbosacral fusion: Review of the literature. Spine (Phila Pa 1976) 2004, 29, 1938–1944. [Google Scholar]
- Wang, T.; Ding, W. Risk factors for adjacent segment degeneration after posterior lumbar fusion surgery in treatment for degenerative lumbar disorders: A meta-analysis. J. Orthop. Surg. Res. 2020, 15, 582. [Google Scholar] [CrossRef]
- Khan, M.H.; Rihn, J.; Steele, G.; Davis, R.; Donaldson, W.F.; Kang, J.D.; Lee, J.Y. Postoperative management protocol for incidental dural tears during degenerative lumbar spine surgery: A review of 3,183 consecutive degenerative lumbar cases. Spine (Phila Pa 1976) 2006, 31, 2609–2613. [Google Scholar]
- Tafazal, S.I.; Sell, P.J. Incidental durotomy in lumbar spine surgery: Incidence and management. Eur. Spine J. 2005, 14, 287–290. [Google Scholar]
- Du, P.Z.; Singh, G.; Smith, S.; Yoo, J. Association between paraspinal muscle quality and surgery for adjacent segment disease. N. Am. Spine Soc. J. 2025, 21, 100594. [Google Scholar] [CrossRef] [PubMed]
- Jin, C.; Xie, M.; He, L.; Xu, W.; Han, W.; Liang, W.; Qian, Y. Oblique lumbar interbody fusion for adjacent segment disease after posterior lumbar fusion: A case-controlled study. J. Orthop. Surg. Res. 2019, 14, 216. [Google Scholar] [CrossRef]
- Zhang, B.; Hu, Y.; Kong, Q.; Feng, P.; Liu, J.; Ma, J. Comparison of Oblique Lumbar Interbody Fusion Combined with Posterior Decompression (OLIF-PD) and Posterior Lumbar Interbody Fusion (PLIF) in the Treatment of Adjacent Segmental Disease(ASD). J. Pers. Med. 2023, 13, 368. [Google Scholar] [CrossRef] [PubMed]
- Jung, J.; Lee, S.; Cho, D.C.; Han, I.B.; Kim, C.H.; Lee, Y.S.; Kim, K.T. Usefulness of Oblique Lumbar Interbody Fusion as Revision Surgery: Comparison of Clinical and Radiological Outcomes Between Primary and Revision Surgery. World Neurosurg. 2021, 149, e1067–e1076. [Google Scholar] [CrossRef] [PubMed]
- Buckland, A.J.; Proctor, D.J.; Thomas, J.A.; Protopsaltis, T.S.; Ashayeri, K.; Braly, B.A. Single-Position Prone Lateral Lumbar Interbody Fusion Increases Operative Efficiency and Maintains Safety in Revision Lumbar Spinal Fusion. Spine (Phila Pa 1976) 2024, 49, E19–E24. [Google Scholar]
- Rohde, M.; Echevarria, A.; Carrier, R.; Zinner, M.; Ngan, A.; Verma, R. Prone Single Position Approach to Lateral Lumbar Interbody Fusion: Systematic Review and Meta-Analysis. Int. J. Spine Surg. 2024, 18, 408–417. [Google Scholar] [CrossRef]
- Fujibayashi, S.; Takemoto, M.; Izeki, M.; Takahashi, Y.; Nakayama, T.; Neo, M. Does the formation of vertebral endplate cysts predict nonunion after lumbar interbody fusion? Spine (Phila Pa 1976) 2012, 37, E1197–E1202. [Google Scholar]
- Williams, A.L.; Gornet, M.F.; Burkus, J.K. CT evaluation of lumbar interbody fusion: Current concepts. AJNR Am. J. Neuroradiol. 2005, 26, 2057–2066. [Google Scholar] [PubMed]
- Mills, E.S.; Treloar, J.; Idowu, O.; Shelby, T.; Alluri, R.K.; Hah, R.J. Single position lumbar fusion: A systematic review and meta-analysis. Spine J. 2022, 22, 429–443. [Google Scholar] [CrossRef]
- Ziino, C.; Konopka, J.A.; Ajiboye, R.M.; Ledesma, J.B.; Koltsov, J.C.B.; Cheng, I. Single position versus lateral-then-prone positioning for lateral interbody fusion and pedicle screw fixation. J. Spine Surg. 2018, 4, 717–724. [Google Scholar]
- Lee, S.K.; Lee, S.H.; Song, K.S.; Park, B.M.; Lim, S.Y.; Jang, G.; Lee, B.S.; Moon, S.H.; Lee, H.M. Lumbar Lordosis of Spinal Stenosis Patients During Intraoperative Prone Positioning. Clin. Orthop. Surg. 2016, 8, 65–70. [Google Scholar] [CrossRef]
- Amaral, R.; Daher, M.T.; Pratali, R.; Arnoni, D.; Pokorny, G.; Rodrigues, R.; Batista, M.; Fortuna, P.P.; Pimenta, L.; Herrero, C.; et al. The Effect of Patient Position on Psoas Morphology and in Lumbar Lordosis. World Neurosurg. 2021, 153, e131–e140. [Google Scholar] [CrossRef] [PubMed]
- Lykissas, M.G.; Aichmair, A.; Hughes, A.P.; Sama, A.A.; Lebl, D.R.; Taher, F.; Du, J.Y.; Cammisa, F.P.; Girardi, F.P. Nerve injury after lateral lumbar interbody fusion: A review of 919 treated levels with identification of risk factors. Spine J. 2014, 14, 749–758. [Google Scholar] [CrossRef] [PubMed]
- Sofianos, D.A.; Briseno, M.R.; Abrams, J.; Patel, A.A. Complications of the lateral transpsoas approach for lumbar interbody arthrodesis: A case series and literature review. Clin. Orthop. Relat. Res. 2012, 470, 1621–1632. [Google Scholar] [CrossRef]
- Salzmann, S.N.; Shue, J.; Hughes, A.P. Lateral Lumbar Interbody Fusion-Outcomes and Complications. Curr. Rev. Musculoskelet. Med. 2017, 10, 539–546. [Google Scholar]
- Sadrameli, S.S.; Davidov, V.; Huang, M.; Lee, J.J.; Ramesh, S.; Guerrero, J.R.; Wong, M.S.; Boghani, Z.; Ordonez, A.; Barber, S.M.; et al. Complications associated with L4-5 anterior retroperitoneal trans-psoas interbody fusion: A single institution series. J. Spine Surg. 2020, 6, 562–571. [Google Scholar]
- Wellington, I.J.; Antonacci, C.L.; Chaudhary, C.; Coskun, E.; Cote, M.P.; Singh, H.; Mallozzi, S.S.; Moss, I.L. Early Clinical Outcomes of the Prone Transpsoas Lumbar Interbody Fusion Technique. Int. J. Spine Surg. 2023, 17, 112–121. [Google Scholar] [CrossRef]
- Farber, S.H.; Valenzuela Cecchi, B.; O’Neill, L.K.; Chapple, K.M.; Zhou, J.J.; Alan, N.; Gooldy, T.C.; DiDomenico, J.D.; Snyder, L.A.; Turner, J.D.; et al. Complications associated with single-position prone lateral lumbar interbody fusion: A systematic review and pooled analysis. J. Neurosurg. Spine 2023, 39, 380–386. [Google Scholar]
- Smajic, S.; Konieczny, M.; Kabir, K.; Scrofani, R.; Migliorini, F.; Dracic, A. Influence of prone, supine, and lateral positions during spine surgery on vascular, abdominal, and postural anatomy: A comprehensive review and Bayesian meta-analysis. Eur. J. Med. Res. 2025, 30, 932. [Google Scholar] [CrossRef]
- Patel, H.M.; Fasani-Feldberg, G.; Patel, H. Prone position lateral interbody fusion—A narrative review. J. Spine Surg. 2023, 9, 331–341. [Google Scholar]
- Alluri, R.; Clark, N.; Sheha, E.; Shafi, K.; Geiselmann, M.; Kim, H.J.; Qureshi, S.; Dowdell, J. Location of the Femoral Nerve in the Lateral Decubitus Versus Prone Position. Glob. Spine J. 2023, 13, 1765–1770. [Google Scholar]
- McDermott, M.; Rogers, M.; Prior, R.; Michna, R.; Guiroy, A.; Asghar, J.; Patel, A. Single-Position Prone Lateral Lumbar Interbody Fusion Technique Guide: Surgical Tips and Tricks. Int. J. Spine Surg. 2024, 18, 110–116. [Google Scholar] [CrossRef]
- Farber, S.H.; Naeem, K.; Bhargava, M.; Porter, R.W. Single-position prone lateral transpsoas approach: Early experience and outcomes. J. Neurosurg. Spine 2022, 36, 358–365. [Google Scholar]
- Wu, T.; Yeo, Q.Y.; Oh, J.Y. Single position, prone oblique lateral interbody fusion (OLIF)-case illustration and technical considerations. J. Spine Surg. 2024, 10, 135–143. [Google Scholar] [PubMed]
- Hur, J.-W. Prone single position lateral interbody fusion for symptomatic cranial adjacent segment degeneration: Technical considerations and preliminary clinical outcomes. Spine J. 2025, 25, S154. [Google Scholar] [CrossRef]
| Pre | Post | |||
|---|---|---|---|---|
| Intraobserver | Interobserver | Intraobserver | Interobserver | |
| SVA | 0.887 | 0.814 | 0.908 | 0.832 |
| PT | 0.901 | 0.846 | 0.926 | 0.871 |
| LL | 0.918 | 0.874 | 0.94 | 0.892 |
| SL | 0.876 | 0.823 | 0.903 | 0.845 |
| Spondylolisthesis at the index level | 0.942 | 0.894 | 0.963 | 0.917 |
| ADH | 0.913 | 0.862 | 0.934 | 0.884 |
| PDH | 0.938 | 0.901 | 0.958 | 0.925 |
| Variables | |
|---|---|
| Numbers of patients | 30 |
| Age (years) | 64.1 ± 15.1 |
| BMI (kg/m2) | 27.2 ± 4.5 |
| Levels | |
| L2–3 | 4 |
| L3–4 | 16 |
| L4–5 | 10 |
| Operation time | 113.8 ± 26.6 |
| X-ray exposure | 29.5 ± 15.9 shots |
| EBL | 105.8 ± 69.3 |
| Preop | Postop (12 Mos) | p-Value | Δ | |
|---|---|---|---|---|
| VAS (back) | 8.0 ± 2.3 | 3.3 ± 1.7 | <0.001 * | 4.7 ± 1.2 |
| VAS (leg) | 8.6 ± 2.0 | 2.1 ± 2.4 | <0.001 * | 6.5 ± 2.2 |
| ODI | 39.0 ± 9.8 | 10.5 ± 10.2 | <0.001 * | 28.5 ± 11.0 |
| SVA (cm) | 3.6 ± 4.5 | 3.5 ± 4.3 | 0.84 | 0.1 ± 2.1 |
| PT (°) | 21.8 ± 7.4 | 21.3 ± 7.0 | 0.41 | 0.5 ± 3.2 |
| LL (°) | 37.8 ± 9.6 | 44.1 ± 5.7 | <0.001 * | 6.3 ± 3.9 |
| SL (°) | 11.2 ± 6.4 | 16.3 ± 5.2 | <0.001 * | 5.1 ± 1.2 |
| Spondylolisthesis at the index level (mm) | 6.8 ± 3.4 | 2.4 ± 2.8 | <0.001 * | 4.4 ± 3.7 |
| ADH (mm) | 5.1 ± 2.2 | 13.2 ± 2.6 | <0.001 * | 8.1 ± 2.2 |
| PDH (mm) | 4.7 ± 2.0 | 11.0 ± 2.3 | <0.001 * | 6.3 ± 1.2 |
| Complication Type | Severity | No. of Patients (%) | Progress |
|---|---|---|---|
| Transient neurological symptoms | Minor | 5 (16.7%) | - |
| - Thigh numbness | 3 (10.0%) | Recovered without intervention (immediate or POD 1 onset; improved by 3 months) | |
| - Hip flexion weakness | 2 (6.7%) | Fully resolved (immediate onset; POD 6 and POD 18) | |
| Intraoperative cage subsidence | Minor | 1 (3.3%) | Managed intraoperatively |
| Vascular injury | Major | 0 | - |
| Permanent neurological deficit | Major | 0 | - |
| Dural tear | Major | 0 | - |
| Infection or wound complication | Major | 0 | - |
| Total complication rate | 6 (20.0%) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2026 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Kim, D.H.; Kim, S.D.; Hur, J.-W.; Kim, J.Y.; Hong, J.T. The Efficacy of Prone Single-Position Lateral Lumbar Interbody Fusion for Symptomatic Cranial Adjacent Segment Degeneration. J. Clin. Med. 2026, 15, 895. https://doi.org/10.3390/jcm15020895
Kim DH, Kim SD, Hur J-W, Kim JY, Hong JT. The Efficacy of Prone Single-Position Lateral Lumbar Interbody Fusion for Symptomatic Cranial Adjacent Segment Degeneration. Journal of Clinical Medicine. 2026; 15(2):895. https://doi.org/10.3390/jcm15020895
Chicago/Turabian StyleKim, Dong Hun, Sang Don Kim, Jung-Woo Hur, Jin Young Kim, and Jae Taek Hong. 2026. "The Efficacy of Prone Single-Position Lateral Lumbar Interbody Fusion for Symptomatic Cranial Adjacent Segment Degeneration" Journal of Clinical Medicine 15, no. 2: 895. https://doi.org/10.3390/jcm15020895
APA StyleKim, D. H., Kim, S. D., Hur, J.-W., Kim, J. Y., & Hong, J. T. (2026). The Efficacy of Prone Single-Position Lateral Lumbar Interbody Fusion for Symptomatic Cranial Adjacent Segment Degeneration. Journal of Clinical Medicine, 15(2), 895. https://doi.org/10.3390/jcm15020895







