Diagnostic Value of Uric Acid/Albumin Ratio and Platelet Indices in Predicting Hypervascularization in the Placenta Accreta Spectrum: A Comparative Retrospective Analysis
Abstract
1. Introduction
2. Materials and Methods
Statistical Analysis
3. Results
4. Discussion
Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AUC | Area under the curve |
| BMI | Body mass index |
| FIGO | International Federation of Gynecology and Obstetrics |
| EW-AIP | European Working Group on Abnormally Invasive Placenta |
| GFR | Glomerular filtration rate |
| MPV | Mean platelet volume |
| NICU | Neonatal intensive care unit |
| PAS | Placenta accreta spectrum |
| PDW | Platelet distribution width |
| P-LCR | Platelet large cell ratio |
| PPH | Postpartum hemorrhage |
| ROC | Receiver operating characteristic |
| SDF-1α | Stromal cell-derived factor-1 alpha |
| UAR | Uric acid/albumin ratio |
| VEGF | Vascular endothelial growth factor |
| APGAR | Appearance, pulse, grimace, activity, respiration |
References
- Liu, X.; Wang, Y.; Wu, Y.; Zeng, J.; Yuan, X.; Tong, C.; Qi, H. What we know about placenta accreta spectrum (PAS). Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 259, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Hecht, J.L.; Baergen, R.; Ernst, L.M.; Katzman, P.J.; Jacques, S.M.; Jauniaux, E.; Khong, T.Y.; Metlay, L.A.; Poder, L.; Qureshi, F.; et al. Classification and reporting guidelines for the pathology diagnosis of placenta accreta spectrum (PAS) disorders: Recommendations from an expert panel. Mod. Pathol. 2020, 33, 2382–2396. [Google Scholar] [CrossRef] [PubMed]
- Einerson, B.D.; Gilner, J.B.; Zuckerwise, L.C. Placenta Accreta Spectrum. Obstet. Gynecol. 2023, 142, 31–50. [Google Scholar] [CrossRef] [PubMed]
- Jauniaux, E.; D’Antonio, F.; Bhide, A.; Prefumo, F.; Silver, R.M.; Hussein, A.M.; Shainker, S.A.; Chantraine, F.; Alfirevic, Z.; Panel, D.C.E. Modified Delphi study of ultrasound signs associated with placenta accreta spectrum. Ultrasound Obstet. Gynecol. 2023, 61, 518–525. [Google Scholar] [CrossRef]
- Jauniaux, E.; Jurkovic, D.; Hussein, A.M.; Burton, G.J. New insights into the etiopathology of placenta accreta spectrum. Am. J. Obstet. Gynecol. 2022, 227, 384–391. [Google Scholar] [CrossRef]
- Collins, S.L.; Ashcroft, A.; Braun, T.; Calda, P.; Langhoff-Roos, J.; Morel, O.; Stefanovic, V.; Tutschek, B.; Chantraine, F.; on behalf of the European Working Group on Abnormally Invasive Placenta (EW-AIP). Proposal for standardized ultrasound descriptors of abnormally invasive placenta (AIP). Ultrasound Obstet. Gynecol. 2015, 47, 271–275. [Google Scholar] [CrossRef]
- Oflar, E.; Karabulut, D.; Yıldız, C.; Sinoplu, H.A.; Dönmez, E.; Koyuncu, A.; Özcan, S.; Çağlar, N.T. The uric acid/albumin ratio might be a better indicator for predicting repeat revascularization in young patients with acute coronary syndrome: Beyond inflammatory biomarkers. PLoS ONE 2024, 19, e0306178. [Google Scholar] [CrossRef]
- Toprak, K.; Yılmaz, R.; Kaplangoray, M.; Memioğlu, T.; İnAnır, M.; Akyol, S.; Özen, K.; Biçer, A.; Demirbağ, R. Comparison of the effect of uric acid/albumin ratio on coronary colleteral circulation with other inflammation-based markers in stable coronary artery disease patients. Perfusion 2023, 39, 1440–1452. [Google Scholar] [CrossRef]
- Yin, R.; Ye, Z.; You, H.; Wu, Y.; Chen, W.; Jiang, T. Elevated uric acid/albumin ratio as a predictor of poor coronary collateral circulation development in patients with non-ST segment elevation myocardial infarction. Clin. Cardiol. 2024, 47, e24215. [Google Scholar] [CrossRef]
- Yalcinkaya, D.; Karacali, K.; Ilhan, B.C.; Yarlioglues, M. Relation Between Serum Uric Acid to Albumin Ratio and Severity of Chronic Coronary Artery Disease. Angiology 2023, 75, 386–393. [Google Scholar] [CrossRef]
- Zhang, X.-J.; Hou, A.-J.; Luan, B.; Wang, C.-F.; Li, J.-J. Uric acid to albumin ratio as a novel predictor for coronary slow flow phenomenon in patients with chronic coronary syndrome and non-obstructive coronary arteries. BMC Cardiovasc. Disord. 2024, 24, 358. [Google Scholar] [CrossRef] [PubMed]
- Gökdeniz, H.G.; Bayramoglu, N.T.; Taysi, S. Investigation of Nrf2-Keap-1 pathway, Sestrin 2 and oxidative stress markers in serum of patients with placenta Accreata spectrum. Eur. J. Obstet. Gynecol. Reprod. Biol. 2024, 302, 211–215. [Google Scholar] [CrossRef] [PubMed]
- Roweth, H.G.; Battinelli, E.M. Platelets and (Lymph)angiogenesis. Cold Spring Harb. Perspect. Med. 2022, 13, a041174. [Google Scholar] [CrossRef]
- Italiano, J.E., Jr.; Richardson, J.L.; Patel-Hett, S.; Battinelli, E.; Zaslavsky, A.; Short, S.; Ryeom, S.; Folkman, J.; Klement, G.L. Angiogenesis is regulated by a novel mechanism: Pro- and antiangiogenic proteins are organized into separate platelet α granules and differentially released. Blood 2008, 111, 1227–1233. [Google Scholar] [CrossRef] [PubMed]
- Faraji, A.; Akbarzadeh-Jahromi, M.; Bahrami, S.; Gharamani, S.; Shahraki, H.R.; Kasraeian, M.; Vafaei, H.; Zare, M.; Asadi, N. Predictive value of vascular endothelial growth factor and placenta growth factor for placenta accreta spectrum. J. Obstet. Gynaecol. 2021, 42, 900–905. [Google Scholar] [CrossRef]
- Wojtukiewicz, M.Z.; Sierko, E.; Hempel, D.; Tucker, S.C.; Honn, K.V. Platelets and cancer angiogenesis nexus. Cancer Metastasis Rev. 2017, 36, 249–262. [Google Scholar] [CrossRef]
- Cali, G.; Forlani, F.; Lees, C.; Timor-Tritsch, I.; Palacios-Jaraquemada, J.; Dall’Asta, A.; Bhide, A.; Flacco, M.E.; Manzoli, L.; Labate, F.; et al. Prenatal ultrasound staging system for placenta accreta spectrum disorders. Ultrasound Obstet. Gynecol. 2019, 53, 752–760. [Google Scholar] [CrossRef]
- Jauniaux, E.; Ayres-De-Campos, D.; Langhoff-Roos, J.; Fox, K.A.; Collins, S.; FIGO Placenta Accreta Diagnosis and Management Expert Consensus Panel. FIGO classification for the clinical diagnosis of placenta accreta spectrum disorders. Int. J. Gynecol. Obstet. 2019, 146, 20–24. [Google Scholar] [CrossRef]
- Jansen, C.H.J.R.; van Dijk, C.E.; Kleinrouweler, C.E.; Holzscherer, J.J.; Smits, A.C.; Limpens, J.C.E.J.M.; Kazemier, B.M.; van Leeuwen, E.; Pajkrt, E. Risk of preterm birth for placenta previa or low-lying placenta and possible preventive interventions: A systematic review and meta-analysis. Front. Endocrinol. 2022, 13, 921220. [Google Scholar] [CrossRef]
- Zhu, Y.; Hu, Y.; Huang, T.; Zhang, Y.; Li, Z.; Luo, C.; Luo, Y.; Yuan, H.; Hisatome, I.; Yamamoto, T.; et al. High uric acid directly inhibits insulin signalling and induces insulin resistance. Biochem. Biophys. Res. Commun. 2014, 447, 707–714. [Google Scholar] [CrossRef]
- Ramos, G.K.; Goldfarb, D.S. Update on Uric Acid and the Kidney. Curr. Rheumatol. Rep. 2022, 24, 132–138. [Google Scholar] [CrossRef] [PubMed]
- de Oliveira, E.P.; Burini, R.C. High plasma uric acid concentration: Causes and consequences. Diabetol. Metab. Syndr. 2012, 4, 12. [Google Scholar] [CrossRef] [PubMed]
- Du, L.; Zong, Y.; Li, H.; Wang, Q.; Xie, L.; Yang, B.; Pang, Y.; Zhang, C.; Zhong, Z.; Gao, J. Hyperuricemia and its related diseases: Mechanisms and advances in therapy. Signal Transduct. Target. Ther. 2024, 9, 212. [Google Scholar] [CrossRef]
- Wang, G.; Li, G.; Wang, P.; Zang, M.; Pu, J. The uric acid to albumin ratio predicts all-cause and cardiovascular mortality among U.S. adults: Results from the National Health and Nutrition Examination Survey 2003–2018. Int. J. Med. Sci. 2025, 22, 2277–2288. [Google Scholar] [CrossRef] [PubMed]
- Weng, H.; Li, H.; Zhang, Z.; Zhang, Y.; Xi, L.; Zhang, D.; Deng, C.; Wang, D.; Chen, R.; Chen, G.; et al. Association between uric acid and risk of venous thromboembolism in East Asian populations: A cohort and Mendelian randomization study. Lancet Reg. Health West. Pac. 2023, 39, 100848. [Google Scholar] [CrossRef]
- Misiani, R.; Marchesi, D.; Tiraboschi, G.; Gualanãris, L.; Pagnf, R.; Goglio, A.; Amuso, G.; Muratore, D.; Bertuletti, P.; Massazza, M. Urinary albumin excretion in normal pregnancy and pregnancy-induced hypertension. Nephron 1991, 59, 416–422. [Google Scholar] [CrossRef]
- Riis, J.L.; Cook, S.H.; Letourneau, N.; Campbell, T.; Granger, D.A.; Giesbrecht, G.F. Characterizing and Evaluating Diurnal Salivary Uric Acid Across Pregnancy Among Healthy Women. Front. Endocrinol. 2022, 13, 813564. [Google Scholar] [CrossRef]
- Montague, S.J.; Lim, Y.J.; Lee, W.M.; Gardiner, E.E. Imaging Platelet Processes and Function—Current and Emerging Approaches for Imaging in vitro and in vivo. Front. Immunol. 2020, 11, 78. [Google Scholar] [CrossRef]
- Patel-Lippmann, K.K.; Planz, V.B.; Phillips, C.H.; Ohlendorf, J.M.; Zuckerwise, L.C.; Moshiri, M. Placenta Accreta Spectrum Disorders: Update and Pictorial Review of the SAR-ESUR Joint Consensus Statement for MRI. RadioGraphics 2023, 43, e220090. [Google Scholar] [CrossRef]
- Romeo, V.; Sarno, L.; Volpe, A.; Ginocchio, M.I.; Esposito, R.; Mainenti, P.P.; Petretta, M.; Liuzzi, R.; D’aRmiento, M.; Martinelli, P.; et al. US and MR imaging findings to detect placental adhesion spectrum (PAS) in patients with placenta previa: A comparative systematic study. Abdom. Imaging 2019, 44, 3398–3407. [Google Scholar] [CrossRef]
- Liu, Q.; Zhou, W.; Yan, Z.; Li, D.; Lou, T.; Yuan, Y.; Rong, P.; Feng, Z. Development and validation of MRI-based scoring models for predicting placental invasiveness in high-risk women for placenta accreta spectrum. Eur. Radiol. 2023, 34, 957–969. [Google Scholar] [CrossRef]
- Çakır, B.T.; Aktemur, G.; Karabay, G.; Şeyhanlı, Z.; Çetin, S.; Filiz, A.A.; Tonyalı, N.V.; Çağlar, A.T. Evaluation of platelet indices and inflammation markers in preeclampsia. J. Clin. Med. 2025, 14, 1406. [Google Scholar] [CrossRef]
- Jauniaux, E.; Collins, S.; Burton, G.J. Placenta accreta spectrum: Pathophysiology and evidence-based anatomy for prenatal ultrasound imaging. Am. J. Obstet. Gynecol. 2018, 218, 75–87. [Google Scholar] [CrossRef]
- American College of Obstetricians and Gynecologists; Society for Maternal-Fetal Medicine. Obstetric Care Consensus No. 7: Placenta Accreta Spectrum. Obstet. Gynecol. 2018, 132, e259–e275. [Google Scholar] [CrossRef]
- Toussia-Cohen, S.; Castel, E.; Friedrich, L.; Mor, N.; Ohayon, A.; Levin, G.; Meyer, R. Neonatal outcomes in pregnancies complicated by placenta accreta—A matched cohort study. Arch. Gynecol. Obstet. 2024, 310, 269–275. [Google Scholar] [CrossRef]

| Definition | Ultrasonographic Features | |
|---|---|---|
| PAS 0 | Placenta previa without hypervascularization | No abnormal placental findings; no evidence of abnormal vascularization on Doppler. |
| PAS 1 | Abnormal placental features without hypervascularization | At least two of: loss of clear zone, presence of placental lacunae, disruption of bladder wall, no hypervascularization. |
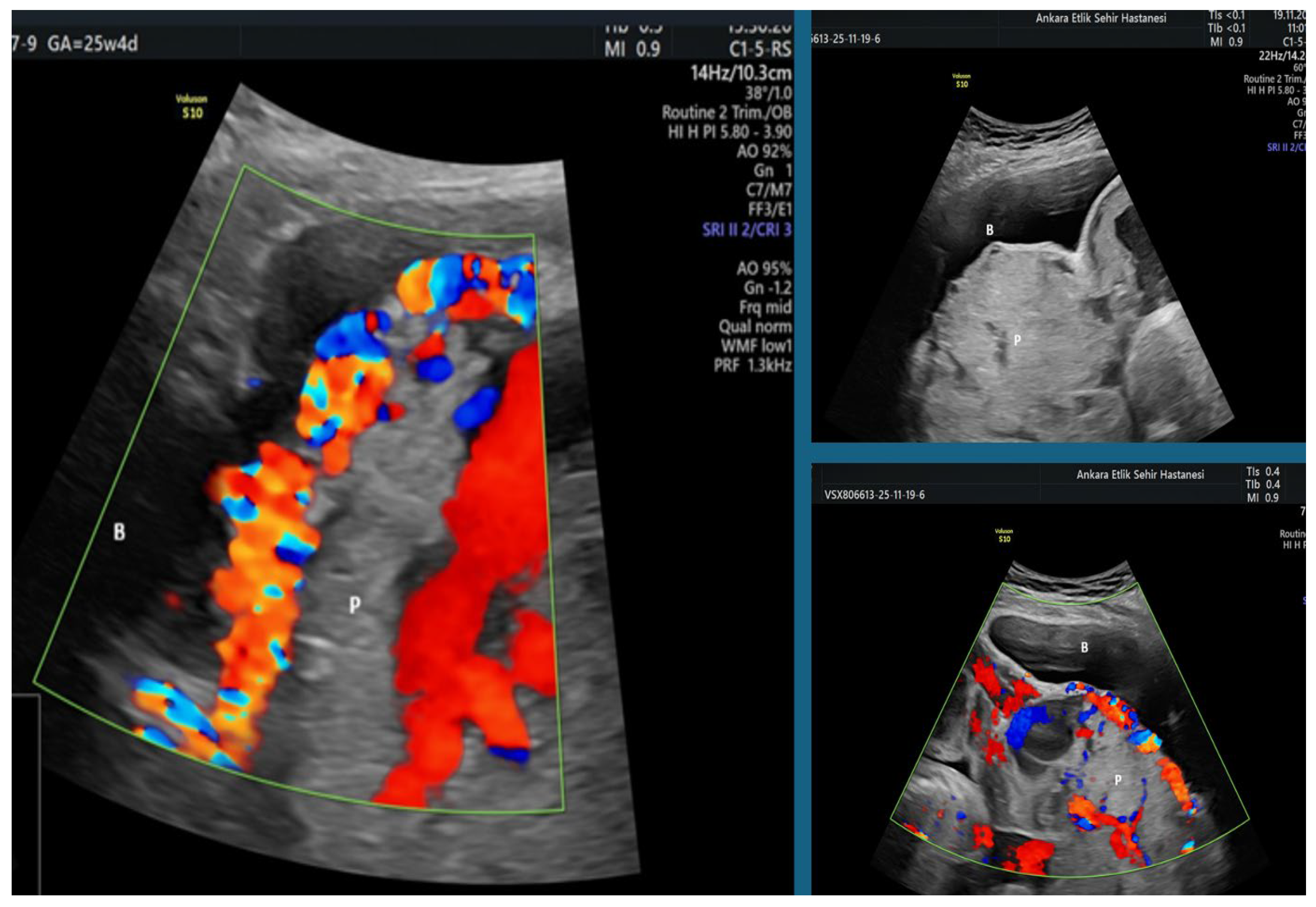
| PAS 2 | Uterovesical hypervascularization | PAS1 features plus increased vascularity between the uterus and bladder on Doppler imaging. |
| PAS 3 | Extensive parametrial vascularity | PAS1 or PAS2 features plus marked vascular extension into the parametrial region of the lower uterine segment. |
| G1 (n = 76) | G2 (n = 77) | G3 (n = 76) | p-Value | |
|---|---|---|---|---|
| Maternal age (year) Mean ± SD | 32.2 ± 5.1 | 33.0 ± 6.0 | 31 ± 4.9 | 0.158 a |
| BMI (kg/m2) Mean ± SD | 29.5 ± 4.2 | 27.7 ± 5.8 | 21 ± 4.8 | 0.07 a |
| Gravidity Median (min–max) | 4 (1–9) | 2 (1–9) | 2 (1–6) | <0.001 b,† |
| Parity Median (min–max) | 2 (0–7) | 1 (0–8) | 1 (0–4) | <0.001 b,‡ |
| Number of previous cesarean section Median (min–max) | 2 (0–5) | 0 (0–3) | 0 (0–3) | <0.001 b,§ |
| GW on ultrasound Median (min–max) | 32.0 (21.3–39.6) | 32.5 (16.2–38.1) | 39.0 (27.4–41.4) | <0.001 b,¶ |
| Smoking n (%) | 2 (22.6%) | 6 (8.0) | 1 (1.3) | 0.084 c |
| Additional disease n (%) | 19 (25) | 25 (32.5) | 0 (0) | <0.001 c,* |
| G1 (n = 76) | G2 (n = 77) | G3 (n = 76) | p-Value | |
|---|---|---|---|---|
| GW of delivery (week) Median (min–max) | 34.2 (23.4–39.6) | 35.6 (24.1–38.3) | 39.0 (27.5–42.0) | <0.001 a,† |
| Birth weight (g) Median (min–max) | 2480 (440–3760) | 2690 (490–3666) | 3205 (1420–4240) | <0.001 a,‡ |
| APGAR 1. min Median (min–max) | 8 (2–9) | 8 (1–9) | 9 (5–9) | <0.001 a,§ |
| APGAR 5. min Median (min–max) | 9 (4–10) | 9 (4–10) | 10 (7–10) | <0.001 a,¶ |
| NICU n (%) | 38 (50.0) | 23 (29.9) | 5 (6.6) | <0.001 b,* |
| G1 (n = 76) | G2 (n = 77) | G3 (n = 76) | p-Value | |
|---|---|---|---|---|
| Treatment, n (%) Hysterectomy Conservative | 37 (48.7) 39 (51.3) | 0 (0) 77 (100) | 0 (0) 76 (100) | <0.001 a,† |
| PPH, n (%) | 19 (25) | 13 (16.9) | 0 (0) | <0.001 a,‡ |
| Blood transfusion, n (%) | 39 (51.3) | 13 (16.9) | 1 (1.3) | <0.001 a,§ |
| Length of hospital stay (day) Median (min–max) | 4 (2–29) | 3 (2–7) | 2 (1–4) | <0.001 b,¶ |
| PAS 2–3 Groups (n = 38) | PAS 0–1 Groups (n = 115) | p-Value | |
|---|---|---|---|
| MPV fL Median (min–max) | 10.3 (8.8–13.0) | 10.7 (3–15.1) | 0.001 a |
| P-LCR % Median (min–max) | 27.7 (15.5–46.3) | 30.8 (11.1–54.5) | 0.057 a |
| PDW % Median (min–max) | 11.6 (8.9–18.10) | 12.7 (3–20.8) | 0.001 a |
| UAR Median (min–max) | 0.09 (0.05–0.17) | 0.10 (0.03–0.26) | 0.891 a |
| Cut-Off | Sensitivity (%) | Specificity (%) | AUC | %95 CI | p-Value | |
|---|---|---|---|---|---|---|
| MPV fL | 10.55 | 66% | 63% | 0.675 | 0.578–0.771 | 0.001 |
| PDW % | 12.35 | 66% | 60% | 0.683 | 0.585–0.782 | 0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license.
Share and Cite
Çayönü Kahraman, N.; Şeyhanlı, Z.; Karabay, G.; Aktemur, G.; Vanlı Tonyalı, N.; Akın, F.; Çağlar, A.T. Diagnostic Value of Uric Acid/Albumin Ratio and Platelet Indices in Predicting Hypervascularization in the Placenta Accreta Spectrum: A Comparative Retrospective Analysis. J. Clin. Med. 2026, 15, 99. https://doi.org/10.3390/jcm15010099
Çayönü Kahraman N, Şeyhanlı Z, Karabay G, Aktemur G, Vanlı Tonyalı N, Akın F, Çağlar AT. Diagnostic Value of Uric Acid/Albumin Ratio and Platelet Indices in Predicting Hypervascularization in the Placenta Accreta Spectrum: A Comparative Retrospective Analysis. Journal of Clinical Medicine. 2026; 15(1):99. https://doi.org/10.3390/jcm15010099
Chicago/Turabian StyleÇayönü Kahraman, Neval, Zeynep Şeyhanlı, Gülşan Karabay, Gizem Aktemur, Nazan Vanlı Tonyalı, Furkan Akın, and Ali Turhan Çağlar. 2026. "Diagnostic Value of Uric Acid/Albumin Ratio and Platelet Indices in Predicting Hypervascularization in the Placenta Accreta Spectrum: A Comparative Retrospective Analysis" Journal of Clinical Medicine 15, no. 1: 99. https://doi.org/10.3390/jcm15010099
APA StyleÇayönü Kahraman, N., Şeyhanlı, Z., Karabay, G., Aktemur, G., Vanlı Tonyalı, N., Akın, F., & Çağlar, A. T. (2026). Diagnostic Value of Uric Acid/Albumin Ratio and Platelet Indices in Predicting Hypervascularization in the Placenta Accreta Spectrum: A Comparative Retrospective Analysis. Journal of Clinical Medicine, 15(1), 99. https://doi.org/10.3390/jcm15010099





